Abstract
Objectives
The aim was to conduct a meta-analysis of the randomized evidence to determine the relative merits of laparoscopic assisted (LADG) and open (ODG) distal gastrectomy for proven gastric cancer.
Data sources and review methods
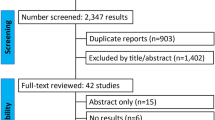
A search of the Medline, Embase, Science Citation Index, Current Contents, and PubMed databases identified all randomized clinical trials (RCTs) that compared LADG and OGD and were published in the English language between January 1990 and the end of June 2007. The meta-analysis was prepared in accordance with the Quality of Reporting of Meta-analyses (QUOROM) statement. The eight outcome variables analysed were operating time, blood loss, retrieval of lymph nodes, oral intake, hospital stay, postoperative complications, tumor recurrence, and mortality. Random effects meta-analyses were performed using odds ratios (OR) and weighted mean differences (WMD).
Results
Four trials were considered suitable for meta-analysis. A total of 82 patients underwent LADG and 80 had ODG. For only one of the eight outcomes, the summary point estimates favoured LADG over ODG; there was a significant reduction of 104.26 ml in intraoperative blood loss for LADG (WMD, −104.26, 95% confidence interval (CI) −189.01 to −19.51; p = 0.0159). There was however a 83.08 min longer duration of operating time for the LADG group compared with the ODG group (WMD 83.08, 95% CI 40.53 to 125.64; p = 0.0001) and significant reduction in lymph nodes harvesting of 4.34 lymph nodes in the LADG group (WMD −4.3, 95% CI −6.66 to −2.02; p = 0.0002). Other outcome variables such as time to commencement of oral intake (WMD −0.97, 95% CI −2.47 to 0.54; p = 0.2068), duration of hospital stay (WMD −3.32, 95% CI −7.69 to 1.05; p = 0.1365), rate of complications (OR 0.66, 95% CI 0.27 to 1.60; p = 0.3530), mortality rates (OR 0.94, 95% CI 0.21 to 4.19; p = 0.9363), and tumor recurrence (OR 1.08, 95% CI 0.42 to 2.79; p = 0.8806) were not found to be statistically significant for either group. However, for commencement of oral intake, duration of hospital stay, and complication rate, the trend was in favor of LADG.
Conclusion
LADG was associated with a significantly reduced rate of intraoperative blood loss, at the expense of significantly longer operating time and significantly reduced lymph node retrieval compared to its open counterpart. Mortality and tumor recurrence rates were similar between the two groups. Furthermore, time to commencement of oral intake, postprocedural discharge from hospital, and perioperative complication rate, although not significantly different between the two groups, did suggest a positive trend toward LADG. Based on this meta-analysis, the authors cannot recommend the routine use of LADG over ODG for the treatment of distal gastric cancer. However, significant limitations exist in the interpretation of this data due to the limited number of published randomised control trials, the small sample sizes to date, and the limited duration of follow up. Further large multicentre randomized controlled trials are required to delineate significantly quantifiable differences between the two groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Minimal access gastrointestinal surgery for gastric cancer in the form of laparoscopic distal gastrectomy was introduced 13 years ago by Japanese surgeons [1]. However, its wider acceptance as an alternative to an open approach remains a contentious issue. There could be a number of reasons for such slow acceptance, which include the complexity of the procedure especially the subsequent reconstruction of the alimentary tract and oncological adequacy and safety in terms of R0 resection, lymph nodes harvesting, and tumor recurrence at the trocar sites [2]. The other factor which may have slowed its progress is the extent of the associated lymph node dissection, an issue which is viewed differently by Japanese and Western surgeons [3–8]. However, recent years have also seen a tremendous advancement in the development of laparoscopic instruments which, coupled with increasing experience in the performance of complex laparoscopic gastrointestinal procedures, have led to the expansion of minimal access surgery for both benign and malignant gastric procedures.
Our aim therefore was to conduct an appraisal, based on a meta-analysis of pooled data from four available randomized clinical trials [9–12], to compare the laparoscopic and open methods of distal gastrectomy for gastric cancer with a view to providing some clarity on a number of issues considered to be controversial. This meta-analysis was prepared in accordance with the Quality of Reporting of Meta-analyses (QUOROM) statement [13].
Materials and methods
Randomized clinical trials of any size that compared LADG with ODG for gastric cancer, and were published in full in peer-reviewed journals in the English language between January 1990 and the end of June 2007, were included. Unpublished studies and abstracts presented at national and international meetings were excluded. Trials were identified by conducting a comprehensive search of Medline, Embase, Science Citation Index, Current Contents, and PubMed databases, using medical subject headings (MESH) ‘gastric cancer’, ‘gastrectomy’, ‘comparative study’, ‘prospective studies’, ‘randomized controlled trials’, ‘random allocation’, and ‘clinical trial’. A manual search of the bibliographies of relevant papers was also carried out to identify trials for possible inclusion. Data extraction and critical appraisal were carried out by three authors independently (BM, RB, MAM). Eight outcome variables were considered most suitable for analysis: operating time, blood loss, retrieval of lymph nodes, oral intake, hospital stay, postoperative complications, tumor recurrence, and mortality rate. The quality of the randomized clinical trials was assessed using Jadad’s scoring system [14] by the two authors (BM, RB) (Table 1).
Statistical analysis
Meta-analyses were performed using odds ratios (ORs) for binary and weighted mean differences (WMDs) for continuous outcome measures. The slightly amended estimator [15] of OR is used to avoid the computation of reciprocal of zeros among observed values in the calculation of the original OR. Random effects models by using the weighted method approach were used to combine the data and statistical heterogeneity was assessed using the χ 2 test [16]. A sensitivity analysis was carried out to assess the impact of study quality on the results, by excluding poor-quality studies (Jadad score 1). Funnel plots (Fig. 1) were constructed to detect publication bias in meta-analysis by plotting both size and precision (1/standard error) against the treatment effect (mean difference/log odds ratio) for each outcome variable [16–18]. Sixteen funnel plots are plotted for eight outcome variables. Eight of them are size-based funnel plots while another eight are standard-error-based funnel plots. For this meta-analysis, the number of points in the funnel plots (the number of studies) is small, i.e., four in each plot, therefore the detection of bias is limited [17, 19]. The funnel plots were produced to show (a) that the conclusion about the shape or visual interpretation may alter by plotting treatment effects against precision error instead of the sample size [16, 18] and (b) the limitation in the use of funnel plots to detect publication bias when the number of studies are small. All estimates were obtained using a computer program written in R, an open-source software (copyright 1998–2007 Kurt Hornik) [20]. All plots were obtained using a computer program written by means of S-PLUS 2000® (Insightful Corporation, Seattle, USA).
Results
A total of four randomized prospective clinical trials that included 162 distal gastrectomies (LADG 82, ODG 80) were considered suitable for meta-analysis. In general, the quality of the studies was poor on critical appraisal (mean quality score 2.7 of 5) (Table 1). This was because the method of randomization was not defined in every study, it was not possible to blind study participants and investigators for these procedures, and a description of withdrawals and dropouts was not always provided. This is not an uncommon feature amongst the surgical RCTs, and has been observed in many reviews and meta-analyses of surgical trials [21–23]. The pooled data (OR and WMD) for the eight outcomes are summarized in Table 2 and Figs. 2–9. As statistically significant heterogeneity was evident for the majority of outcome variables, random effects models were used to combine the data [24]. A total of 81 patients underwent LADG and 80 had ODG. For only one of the eight outcome variables, the summary point estimates favoured LADG over ODG; there was a significant reduction of 104.26 ml in intraoperative blood loss for LADG (WMD −104.26, 95% confidence interval (CI) −189.01 to −19.51; p = 0.0159). There was however a 83.08 min longer duration of operating time for the LADG group compared with the ODG group (WMD 83.08, 95% CI 40.53 to 125.64; p = 0.0001) and significant reduction in lymph nodes harvesting of 4.34 lymph nodes in the LADG group (WMD −4.3, 95% CI −6.66 to −2.02; p = 0.0002). Other outcome variables such as time to commencement of oral intake (WMD −0.97, 95% CI −2.47 to 0.54; p = 0.2068), duration of hospital stay for LADG (WMD −3.32, 95% CI −7.69 to 1.05; p = 0.1365), rate of complications (OR 0.66, 95% CI 0.27 to 1.60; p = 0.3530), mortality rates (OR 0.94, 95% CI 0.21 to 4.19; p = 0.9363), and tumor recurrence (OR 1.08, 95% CI 0.42 to 2.79; p = 0.8806) were not found to be statistically significant for either group. However, for commencement of oral intake, duration of hospital stay, and complication rate, the trend was in favor of LADG.
Values in the left panel are mean (standard deviation), mean difference (95% CI), weighted mean difference (95% CI), and weight. In the graph, squares indicate point estimates of treatment effect (mean difference, i.e., mean for LADG group of patients – mean for ODG group of patients) with the size of the squares representing the weight attributed to each study. The horizontal lines represent 95% confidence interval for means differences. The pooled estimate of operating time (min) is the weighted mean difference, obtained by combining all means differences using the inverse weighted method, and is represented by the diamond with the size of the diamond depicting the 95% confidence interval. Values to the left of the vertical line at zero favor LADG
Values in the left panel are mean (standard deviation), mean difference (95% CI), weighted mean difference (95% CI), and weight. In the graph, squares indicate point estimates of treatment effect (mean difference, i.e., mean for LADG group of patients – mean for ODG group of patients) with the size of the squares representing the weight attribute to each study. The horizontal lines represent 95% confidence interval for means differences. The pooled estimate of blood loss (ml) is the weighted mean difference, obtained by combining all means differences using the inverse weighted method, and is represented by the diamond with the size of the diamond depicting the 95% confidence interval. Values to the left of the vertical line at zero favor LADG
Values in the left panel are mean (standard deviation), mean difference (95% CI), weighted mean difference (95% CI), and weight. In the graph, squares indicate point estimates of treatment effect (mean difference, i.e., mean for LADG group of patients – mean for ODG group of patients) with the size of the squares representing the weight attribute to each study. The horizontal lines represent 95% confidence interval for means differences. The pooled estimate of lymph nodes harvested (units) is the weighted mean difference, obtained by combining all means differences using the inverse weighted method, and is represented by the diamond with the size of the diamond depicting the 95% confidence interval. Values to the left of the vertical line at zero favor ODG
Values in the left panel are mean (standard deviation), mean difference (95% CI), weighted mean difference (95% CI), and weight. In the graph, squares indicate point estimates of treatment effect (mean difference, i.e., mean for LADG group of patients – mean for ODG group of patients) with the size of the squares representing the weight attribute to each study. The horizontal lines represent 95% confidence interval for means differences. The pooled estimate of time to commencement of oral intake (days) is the weighted mean difference, obtained by combining all means differences using the inverse weighted method, and is represented by the diamond with the size of the diamond depicting the 95% confidence interval. Values to the left of the vertical line at zero favor LADG
Values in the left panel are mean (standard deviation), mean difference (95% CI), weighted mean difference (95% CI), and weight. In the graph, squares indicate point estimates of treatment effect (mean difference, i.e., mean for LADG group of patients – mean for ODG group of patients) with the size of the squares representing the weight attribute to each study. The horizontal lines represent 95% confidence interval for means differences. The pooled estimate of duration of hospital stay (days) is the weighted mean difference, obtained by combining all means differences using the inverse weighted method, and is represented by the diamond with the size of the diamond depicting the 95% confidence interval. Values to the left of the vertical line at zero favor LADG
In the graph, squares indicate point estimates of treatment effect (odds ratio for LADG over ODG groups) with the size of the squares representing the weight attribute to each study. The horizontal lines represent 95% confidence interval for odds ratio. The pooled estimate for complication rate is the pooled odds ratio obtained by combining all odds ratio of the four studies using the inverse weighted method and is represented by the diamond with the size of the diamond depicting the 95% confidence interval. Values to the left of the vertical line at 1 favor LADG
In the graph, squares indicate point estimates of treatment effect (odds ratio for LADG over ODG groups) with the size of the squares representing the weight attribute to each study. The horizontal lines represent 95% confidence interval for odds ratio. The pooled estimate for mortality rate is the pooled odds ratio obtained by combining all odds ratio of the four studies using the inverse weighted method and is represented by the diamond with the size of the diamond depicting the 95% confidence interval. Values to the left of the vertical line at 1 favor LADG
In the graph, squares indicate point estimates of treatment effect (odds ratio for LADG over ODG groups) with the size of the squares representing the weight attribute to each study. The horizontal lines represent 95% confidence interval for odds ratio. The pooled estimate for tumor recurrence is the pooled odds ratio obtained by combining all odds ratio of the four studies using the inverse weighted method and is represented by the diamond with the size of the diamond depicting the 95% confidence interval. Values to the left of the vertical line at 1 favour LADG
Discussion
The proponents of LADG argue that the procedure is superior to ODG because it is associated with less postoperative pain, reduced perioperative blood loss, quicker return to gastrointestinal function, faster hospital discharge, earlier return to work and unrestricted physical activity, and better cosmetic result [2]. Opponents, however, argue that there is a higher incidence of major intra- and postoperative complications because of the complexity of the procedure and absence of tactile sensation, substantially greater costs, much longer anaesthetic and operating time, decreased numbers of lymph nodes harvesting essential for oncological adequacy, insufficient surgical resection margins, and potential for cancer reimplantation at trocar sites [2]. Furthermore, long-term consequences are unknown. This controversy has encouraged a number of investigators [9–12] to initiate randomized clinical trials in an attempt to address some of these issues. However all these comparative trials have recruited a limited number of patients to date and the long-term follow-up is not available. To clarify some of these issues, we undertook the present meta-analysis, concentrating on eight treatment variables that could be analyzed objectively. To our knowledge no meta-analyses or a systematic review on this subject has been undertaken or published.
All the trials reported the duration of operation. The meta-analysis revealed statistically significant longer operating time for LADG than for ODG (Fig. 2). This has important implications for both patients and the healthcare providers. Longer operations expose patients to a protracted anaesthesia, which may increase the morbidity and even mortality rates especially in older patients with comorbidities. The vast majority of patients in these four RCTs were in their late fifties or early sixties with concomitant comorbidities including cardiopulmonary issues, diabetes, etc. Longer operating and anaesthesia times also increase the direct cost of the procedure. Even with experience, the operating time for LADG has remained substantially longer to date. Without exception, all the RCTs (Fig. 2) have clearly shown longer operating time for LADG by the authors who are considered experienced upper gastrointestinal (GI) and laparoscopic surgeons. The longer operating time for LADG may in part reflect an early learning curve, as this is a relatively new procedure. Furthermore, the operating time for LADG also includes the time for setting up laparoscopic equipments. Other reasons include lack of tactile sensation, the complexity of procedure, the postresectional reconstruction of gastrointestinal tract, and the extent of lymphadenectomy performed, at least by Japanese surgeons.
Regarding intraoperative blood loss, three out of four RCTs [9, 10, 12] (Fig. 3) have shown decreased blood loss for LADG compared to ODG. This translates into decreased transfusion requirement in the perioperative period with its inherent risk of acute or late adverse effects such as acute lung injury, volume overload, hypothermia, graft versus host disease, and immunomodulatory effects to name but a few. The last of these side-effect is especially important in cancer patients as a number of studies and a meta-analysis has suggested a significant deleterious transfusion effect in all cancer sites, except for breast [25, 26]. Furthermore, the blood transfusion economics has not been addressed in any of these studies. A multicentre study on blood transfusion cost performed in 1991 [27] revealed the average hospital cost per unit transfused was $155, which would be far higher now. It is therefore evident from this meta-analysis that LADG has biological, immunological, and economical benefits for the patient and the health care system by reducing perioperative transfusion needs.
Concerning oncological adequacy for lymph node harvesting, the number of lymph nodes retrieved laparoscopically in all these RCTs were sufficient (Fig. 4) in terms of the global standard for adequate staging, emphasizing the oncological capability of laparoscopic gastric procedures [2]. In fact, in none of the RCTs did lymph nodes retrieval for the two procedures show any significant statistical difference. However, when the results were pooled (Fig. 4), there was a statistically significant reduction in lymph node harvesting for LADG compared to ODG, which may translate into an overall survival disadvantage for patients having LADG. As the long-term results for the majority of these trials have not been published, this assumption is difficult to corroborate.
The debate concerning the merits and risks of extended lymph node clearance during gastrectomy for cancer remains a contentious issue. A number of authors still feel that clinical benefit from extended lymphadenectomy for gastric cancer has no proven benefit and may even be counterproductive. A large retrospective study from Finland [28] analyzing 223 patients (D1 = 114, D2 = 109) undergoing curative gastrectomy found the surgical complication to be statistically higher for D2 cohort (33% versus 16.8%), although hospital mortality was similar between the two groups. Furthermore D2 lymphadenectomy was associated with longer postoperative hospital stay, operating time, blood loss and increased need for blood transfusions. A large Japanese multicentre RCT [29] consisting of 523 patients once again showed higher morbidity for the extended (D2) surgery compared to the D1 group (28.1% versus 20.9%) for curative gastric cancer. This difference however did not reach statistical significance. Nonetheless, the authors felt that extended (D2) surgery can be added without increasing major surgical complications in this setting. Yet another RCT from The Netherlands [30] analyzing 711 patients (D1 = 380, D2 = 331) has shown a significantly higher morbidity and mortality for the D2 group (25% versus 43% and 4% versus 10%, respectively) without affecting the 5-year survival rate. The Cochrane review [31] has shown no survival benefit for extended lymph node dissection but showed increased postoperative mortality and morbidity. Miura et al. [32] performed a critical reappraisal from the viewpoint of lymph node retrieval and found that laparoscopic D2 resection harvested sufficient numbers of nodes for adequate tumor–node–metastasis (TNM) classification in 86% of cases. However, a significantly greater number of lymph nodes were harvested by the open method. They concluded that the extent of lymphadenectomy achieved by current laparoscopic procedures approaches the global standard for accurate staging, although performing extended resection laparoscopically as recommended in Japan remains a challenge and is a time-consuming process. The authors therefore suggested that laparoscopic gastrectomy is only justified for more advanced disease under the setting of clinical trials.
Except for Kitano et al. [9], all the other RCTs [10–12] showed early resumption of oral intake by the patients undergoing LADG (Fig. 5). The pooled data showed a positive trend for LADG, however this did not reach statistical significance. Three out of the four trials [9, 11, 12] which reported on postoperative recovery of gastrointestinal function (passage of first flatus) showed that patients in all these trials have a quicker return of their gastrointestinal function following LADG and in two of these trials, this difference was significant [9, 12]. Quicker return of gastrointestinal function has a direct impact on early resumption of diet which is shown in these trials and this allows early discharge with economical benefits.
Three out of four RCTs [10–12] showed a trend towards earlier discharge from hospital after LADG (Fig. 6). Pooling the data from these trials failed to show any difference in the discharge data for these two procedures, although the trend favoured LADG (Table 2). Early discharge is associated with lower medical direct, non-medical direct, and indirect costs than conventional inpatient care. Cost savings per patient can therefore be significant. Furthermore, early discharge also has a positive effect on pressure on hospital beds, which in certain countries have decreased due to restructuring of health services with a direct impact on elective admissions. It is entirely possible that larger RCTs may show that LADG indeed has a clear-cut advantage over ODG in terms of hospital discharge. We eagerly await any such data.
None of the present trials have provided comparative data on patients returned to normal activity following LADG and ODG. However, all the RCTs have shown that the frequency, dose, and duration of analgesia requirement for LADG have been lower in the perioperative period. This is most likely due to the absence of a large abdominal incision in LADG. Two of the four RCTs [9, 10] have shown significantly early ambulation in their patients undergoing LADG. All these findings translate into a quicker return of biological functions, early hospital discharge, and quicker return to normal activities. Obviously an objective assessment would be ideal using one of the health profile questionnaires which measures physical, mental, or emotional problems or limitations in patients’ daily life in the immediate and late perioperative periods. This may have a major repercussion for both employers and society in general.
As far as the complication rate of these two procedures is concerned, the present analysis showed a higher incidence of perioperative complications after ODG (Fig. 7). However this did not reach statistical significance when compared to LADG. Because laparoscopic surgery avoids a large abdominal incision, this decreases the incidence of postoperative pain, which in turn decreases the incidence of atelectasis, hypoventilation, pneumonia, and coronary ischaemia. A number of RCTs and observational studies have shown that laparoscopic procedures are associated with less suppression of FVC and FEV1 compared to their open counterpart [33–36]. In all the RCTs of LADG versus ODG, the authors have observed more cardiorespiratory complications following ODG compared to LADG. Also the incidence of wound infection is higher for the open cohort because of the larger incision size. It is well known that reducing the number of complications should produce significant savings with an equal or better health outcome. The laparoscopic gastric procedure in this meta-analysis has shown 34% reduction in the relative odds of complications, which although not statistically significant certainly translates into better outcome for the patient and the health care system.
Lastly, there was no significant difference in mortality rate (Fig. 8) and tumor recurrence (Fig. 9) between the two procedures. There could be a number of explanations for such parity. First of all the number of patients in all these RCTs are relatively small, which may have masked the true difference in mortality rate. Secondly, the follow-up data is short and therefore the real difference in tumor recurrence may not be apparent presently. Once the data from these trials is matured, one will be able to obtain a clearer picture on these outcomes variables.
Conclusion
The present meta-analysis included a total of 162 distal gastrectomies for cancer, the largest body of information so far available for the comparison of LADG and ODG in the English-language literature. Laparoscopic gastrectomy was associated with significantly decreased blood loss and positive trends towards fewer postoperative complications, quicker commencement of oral intake, earlier hospital discharge, and early mobilization with decreased requirement for analgesia, but at the expense of a significantly longer operating time and fewer lymph nodes retrieval. Based on these data the authors feel the clear-cut benefits of LADG over ODG are rather limited and its widespread adaptation cannot be recommended. However, significant limitations exist in the interpretation of this data due to the limited number of published randomized control trials, the small sample sizes to date, and the limited duration of follow-up. Further large multicentre randomized controlled trials are required to delineate significantly quantifiable differences between the two groups. Nonetheless, it may be concluded that LADG is a safe and effective alternative to ODG and is justifiable under the setting of clinical trials.
References
Kitano S, Iso Y, Moriyama M (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4:146–8
Shehzad K, Mohiuddin K, Nizami S, Sharma H, Khan IM, Memon B, Memon MA (2007) Current status of minimal access surgery for gastric cancer. Surg Oncol 16:85–98
Kajitani T (1981) The general rules for the gastric cancer study in surgery and pathology. Japanese research for gastric cancer. Jpn J Surg 11:127–139
Japanese Gastric Cancer Association (2001) The guidelines for the treatment of gastric cancer. Kachara Co, Tokyo
Maruyama K, Gunven P, Okabayashi K (1987) Lymph node metastases of gastric cancer: general pattern in 1931 patients. Ann Surg 210:596–602
Maruyama K, Okabayashi K, Kinoshita T (1987) Progress in gastric cancer surgery in Japan in Japan and its limits of radicality. Word J Surg 11:418–425
Noguchi Y, Imada T, Matsumoto A (1986) Radical surgery for gastric cancer: a review of the Japanese experience. Cancer 64:2053–2062
Cuschieri A, Weeden S, Fieldig J (1999) Patient survival after D1 and D2 resections for gastric cancer: long term results of MRC randomized surgical trials. Br J Cancer 79:1522–1530
Kitano S, Shiraishi N, Fujii K, Yasuda K, Inomata M, Adachi Y (2002) A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery 131:S306–S311
Huscher CGS, Mingoli A, Sgarzini G, Sansonetti A, Di Paola M, Rcher A, Ponzano C (2005) Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five year results of a randomized prospective trial. Ann Surg 241:232–237
Lee JH, Han HS, Lee JH (2005) A prospective randomized study comparing open vs laparoscopy-assisted distal gastrectomy in early gastric cancer: early results. Surg Endosc 19:168–173
Hayashi H, Ochiai T, Shimada H, Gunji Y (2005) Prospective randomized study of open versus laparoscopy-assisted distal gastrectomy with extraperigastric lymph node dissection for early gastric cancer. Surg Endosc 19:1172–1176
Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF (1999) Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of reporting of meta-analyses. Lancet 354:1896–1900
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12
Agresti A (2002) Categorical data analysis, 2nd edn. Wiley, Canada, pp 1–734
Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F (2000) Methods for meta-analysis in medical research. Wiley, England, pp 1–346
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. Br Med J 315:629–634
Tang JL, Liu JLY (2000) Misleading funnel plot for detection of bias in meta-analysis. J Clin Epidemiol 53:477–484
Span J, Carière E, Croockewitt S, Smits P (2006) Publication bias, effects on the assessment of Rosiglitasone. Proc Dutch Soc Clin Pharmacol Biopharm Meet, April 2006. Br J Clin Pharmacol 62:732
Hornik K. The R FAQ. Version 2.6.2007-10-22. ISBN 3-900051-08-9. http://www.cran.r-project.org/doc/FAQ/R-FAQ.html. Accessed 16 February 2008
Solomon MJ, Laxamana A, Devore L, McLeod RS (1994) Randomized controlled trials in surgery. Surgery 115:707–712
McLeod RS, Wright JG, Solomon MJ, Hu X, Walters BC. Lossing A (1996) Randomized controlled trials in surgery: issues and problems. Surgery 119:483–486
Horton R (1996) Surgical research or comic opera: questions, but few answers. Lancet 347:984–985
Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F (2000) Methods for meta-analysis in medical research. Wiley, Chichester
Dellinger EP, Anaya DA (2004) Infectious and immunologic consequences of blood transfusion. Crit Care 8 Suppl 2:S18–S23
Vamvakas EC (1995) Perioperative blood transfusion and cancer recurrence: meta-analysis for explanation. Transfusion 35:760–768
Forbes JM, Anderson MD, Anderson GF, Bleecker GC, Rossi EC, Moss GS (1991) Blood transfusion costs: a multicenter study. Transfusion 31:318–323
Danielson H, Kokkola A, Kiviluoto T, Siren J, Louhimo J, Kivilaakso E, Puolakkainen P (2007) Clinical outcome afer D1 vs D2-3 gastrectomy for treatment of gastric cancer. Scand J Surg 96:35–40
Sano T, Sasako M, Yamamoto S, Nashimoto A, Kurita A, Hiratsuka M, Tsujinaka T, Kinoshita T, Arai K, Yamamura Y, Okajima K (2004) Gastric cancer surgery: morbidity and mortality resuls from a prospective randomized controlled trial comparing D2 and extended paraaortic lymphadenectomy – Japan Clinical Oncology Group study 9501. J Clin Oncol 22:2767–2773
Bonenkamp JJ, Hermans J, Sasako M, van de Velde CJ, Welvaart K, Songun I, Meyer S, Plukker JT, Van Elk P, Obertp H, Gouma DJ, van Lanschot JJ, Taat CW, de Graaf PW, von Meyenfeldt MF, Tilanus H, Dutch Gastric Cancer Group (1999) Extended lymph-node dissection for gastric cancer. N Engl J Med 340:908–914
McCulloch P, Nita ME, Kazi H, Gama-Rodrigues J (2004) Extended versus limited lymph nodes dissection technique for adenocarcinoma of the stomach. Cochrane Database Syst Rev 18:CD001964
Miura S, Kodera Y, Fujiwara M, Ito S, Mochizuki Y, Yamamura Y, Hibi K, Ito K, Akiyama S, Nakao A (2004) Laparoscopy-assisted distal gastrectomy with systemic lymph node dissection: a critical reappraisal from the viewpoint of lymph node retrieval. J Am Coll Surg 198:933–938
Schauer PR, Luna J, Ghiatas AA, Glen ME, Warren JM, Sirinek KR (1993) Pulmonary function after laparoscopic cholecystectomy. Surgery 114:389–399
McMahon AJ, Baxter JN, Kenney G, O’Dwyer PJ (1993) Ventilatory and blood gas change during laparoscopic and open cholecystectomy. Br J Surg 80:1252–1254
Frazee RC, Roberts JW, Okeson GC, Symmonds RE, Snyder SK, Hendricks JC, Smith RW (1991) Open versus laparoscopic cholecystectomy: a comparison of postoperative pulmonary function. Ann Surg 213:651–654
Schwenk W, Bohm B, Muller JM (1998) Postoperative pain and fatigue after laparoscopic or conventional colorectal resections: a prospective randomized trial. Surg Endosc 12:1131–1136
Acknowledgements
Authors’ contributions: MAM was responsible for the concept and design of this meta-analysis. Furthermore he takes responsibility for the integrity of the work as a whole, from inception to published article. MAM, RB and BM were responsible for acquisition and interpretation of the data. SK and RMY were involved in analyzing and interpretation of the data in depth from the statistical point of view.
All authors were involved in drafting the manuscript and revising it critically for important intellectual content and have given final approval of the version to be published. Furthermore all authors have participated sufficiently in the work to take public responsibility for its content.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Memon, M.A., Khan, S., Yunus, R.M. et al. Meta-analysis of laparoscopic and open distal gastrectomy for gastric carcinoma. Surg Endosc 22, 1781–1789 (2008). https://doi.org/10.1007/s00464-008-9925-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-9925-9