Abstract
Purpose
To achieve a higher level of satisfaction in patients having undergone Total Knee Arthroplasty (TKA), a more personalized approach has been discussed recently. It can be assumed that a more profound knowledge of bony morphology and ligamentous situation would be beneficial. While CT/MRI can give 3D information on bone morphology, the understanding of the ligamentous situation in different flexion angles is still incomplete. In this study, the dynamic gap widths of a large number of varus knees were assessed in various flexion angles, to find out whether all varus knees behave similar or have more individual soft tissue patterns. Additionally, it was investigated whether the amount of varus deformity or other patient factors have an effect on joint gap widths.
Methods
A series of 1000 consecutive TKA patients, including their CAS data and patient records were analyzed. Joint gap widths in multiple flexion angles (0°, 30°, 60°, 90°) were measured in mm and differences between the joint gaps were compared. A “standard” varus knee was defined as follows: (1) Lateral extension gap greater than medial, (2) lateral flexion gap greater than medial, and (3) flexion gap greater than extension gap. The percentage of fulfillment was tested for each and all criteria. To measure the influence of varus deformity on gap width difference, three subgroups were formed based on the deformity. Data were analyzed at 0°, 30°, 60° and 90° flexion. The effect of patient factors (gender, BMI, age) on gap sizes was tested by performing subgroup analyses.
Results
Only 444 of 680 (65%) patients met all three varus knee criteria. The lateral extension gap (4.1 mm) was significantly larger than the medial extension gap (0.6 mm) in 657 (97%) patients and the gap difference highly correlated with the amount of varus deformity (r2 = 0.62). In all flexion positions, however, no correlation between gap differences and varus deformity existed. Women had significantly larger extension and flexion gaps. Age and BMI showed no significant effect on gap widths.
Conclusion
Varus knees show a large inter-individual variability regarding gap widths and gap differences. The amount of varus deformity correlates highly with the medio-lateral gap difference in extension, but not in any flexion angle. As varus knees are not all alike, a uniform surgical technique will not treat all varus knees adequately and the individual gap sizes need to be analyzed and addressed accordingly with an individualized balancing technique. Which final balancing goal should be achieved needs to be analyzed in future studies.
Level of evidence
Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several studies have shown that about 20% of patients are dissatisfied after total knee arthroplasty (TKA) [1, 2]. Several patient-related, but also surgery- and implant-related factors play an important role in this multifactorial issue [3,4,5,6,7].
More recently, individual reconstruction of the knee has also been considered a relevant factor in improving patient outcome [8,9,10,11]. To achieve anatomical reconstruction, both, individual bone and soft tissue anatomy should be analyzed quantitatively with a higher level of accuracy. Hirschmann et al. [12] have shown that by analyzing the bony anatomy, it is possible to differentiate between 43 morpho-types of the knee, but the anatomical reconstruction of the knee should also include the individual ligamentous frame. Therefore, quantitative assessment of soft tissue structures is equally important [13,14,15,16]. However, in daily practice, pre-operative information is mainly based on subjective, qualitative assessments. Intra-operatively, the use of modern CAS/robotic software has proven to be the best method to obtain quantitative information on gap widths [14, 17,18,19,20,21]. Using these techniques, dynamic stress tests of the ligaments at all clinically relevant flexion angles are possible, and Mehliß et al. [22] demonstrated a high intra- and inter-observer reliability with a short learning curve for CAS.
It has to be assumed that a varus knee is not a homogeneous entity, neither from the soft tissue envelope nor from the bony side. The latter has been confirmed by previous studies [23,24,25]. For the soft tissues, Deep et al. [26] described a large variability of gap sizes from extension to flexion in their CAS analysis and developed a gap-based classification within the varus knee group. Some authors [27,28,29,30,31] have described that a typical varus knee has larger lateral gap sizes in extension and in flexion compared to the medial side. This increase in gap difference between medial and lateral sides has been shown to be particularly pronounced in severe varus deformities. The flexion gap being larger than the extension gap has been described as another criterion of varus knees [32]. However, it is unclear in which percentage each of these three criteria is met in varus knees. This information would be very helpful for individual soft tissue envelope restoration.
Whether the extent of varus deformity correlates with medial–lateral gap differences is not entirely clear. Matziolis et al. [33] showed in a smaller sample that in extension, there is a correlation between both parameters, which would allow planning the extent of release preoperatively based on coronal alignment. To date, it is unclear whether such a correlation also exists in flexion. However, this information would also be of great value for individual soft tissue balancing.
In this study, a group of 1000 patients was analyzed using a quantitative CAS technique. Based on the amount of varus deformity, patients were then divided into three subgroups. All knees were assessed for their medial and lateral gap sizes and differences in extension and 90° flexion and whether they met all three criteria of a “standard” varus knee: (1) lateral extension greater than medial; (2) lateral flexion gap greater than medial flexion gap; and (3) flexion gap greater than extension gap. The correlation between the extent of deformity and the gap differences was tested in extension and in flexion (30°, 60°, 90°). Additionally, the influence of various patient factors (gender, BMI, age) on gap sizes was analyzed.
The following hypotheses were made: (1) not all varus knees are alike and less than 80% meet all three criteria of a “standard” varus knee. (2) Medio-lateral gap differences correlate with the extent of varus deformity in extension and flexion. (3) Other patient factors (age, BMI, gender) have additional influence on gap sizes.
Materials and methods
Written consent of all patients for data collection was obtained prior to hospital entry. After communication with the local Ethics Committee (Bayerische Landesärztekammer), no IRB approval was required for this study as no specific data were obtained or modifications from standard treatment were performed. In the period between January 2017 and December 2018, 1000 consecutive patients who received TKA due to primary OA were prospectively selected for this study. Among the 1000 patients, 680 resulted as varus knee, 125 as valgus knee and 195 had neutral axis. Clinical data, radiographs and CAS data of each patient were stored and used for this analysis.
All patients were operated on by one of the two senior authors of this study (H.G.; W.S.). Surgery was performed in all cases with the use of a navigation system (Knee 3.1; Brainlab, Munich). Operating with CAS has been sufficiently studied and proven to have high precision for all obtained parameters [14, 18].
This system allows a dynamic stress testing of the collateral ligaments and during these procedures individual gap widths can be measured quantitatively. Stress testing was performed continuously from extension to maximal flexion as described by Mehliß et al. [22]. They were able to demonstrate that the stress test has a high intra- and inter-observer reliability (bias of deviation 0.09; 0.05) [22].
Data collection and analysis
At the beginning of surgery, after joint opening and palpation of the anatomical landmarks, the individual gap widths under varus and valgus stress testing were measured and stored.
This was performed before ACL or PCL resection, capsular release, or bone cutting. The patella was left in its natural position to minimize the influence of the extensor mechanism on the measurement of gap widths.
The width of a gap was defined as the minimum spatial distance between the most distal femoral point and the most proximal tibial point. The femoral points differed depending on the angle of flexion. While the most distal point was used for the extension gap, the most posterior point was used for flexion gap calculation. This calculation was performed fully automatic by the Knee3 software in 0.1 mm increments. Data were stored in 1° flexion increments in a single file for every patient.
The medial and lateral gap widths were measured continuously in mm and evaluated at 0°, 30°, 60°, and 90° flexion. The mean value of the extension and flexion gap was calculated by adding the values of the medial and lateral gap and dividing the sum by 2. To compare the extension gap with the flexion gap, the mean value of the flexion gap was subtracted from the mean value of the extension gap. A positive value indicates a larger extension gap, a negative value, a larger flexion gap. To analyze possible differences between medial and lateral gaps, we subtracted the lateral gap value from the medial one. A positive result means that the medial gap size is larger than the lateral one. A negative value indicates a larger lateral gap size.
This comparison was executed in extension and 90° flexion.
Coronal leg axis (HKA) was measured with the CAS system at the beginning and end of surgery. Pre-operative data were used to calculate the correlation between leg alignment and medio-lateral difference at different knee flexion angles.
To specify the effect of deformity on gap sizes, the entire varus group was divided into three subgroups based on HKA (I = 2–5°; II = 5–10°; III = > 10°). General patient data were collected, including BMI, age and sex and evaluating the influence each of these factors had on knee soft tissue situation.
Statistical analysis
Statistical analysis was performed using Microsoft Excel data analysis program. Data were summarized using descriptive statistics of mean and standard deviation. All data were tested for normal distribution.
Furthermore, mean values of gap widths and differences between the three subgroups were compared using the t test for independent samples. Differences between two groups were considered statistically significant if the p value was less than 0.05 in a two-tailed t test.
Pearson correlation test was used to test for correlation between coronal leg alignment and medial–lateral gap difference in extension and flexion (30°, 60°, 90°).
The data were further analyzed for sex-, age-, and BMI-related differences. For this purpose, age (< 55; 55–75; > 75) and BMI (< 25; 25–30; > 30) were grouped. The number of patients in each subgroup is shown in Table 3. For comparison of means between subgroups, the t test was used as previously described.
Results
The quantity, average HKA and different patient factors of all varus knees and the subgroups are presented in Table 1.
Gap widths
Different extension and flexion gap widths are presented in Table 2 using mean and standard deviation.
Comparison of gap sizes (Table 2)
Medial/lateral difference in extension
The mean lateral extension gap (4.1 mm) was significantly larger than the medial extension gap (0.6 mm; p < 0.001). 657 patients (97%) showed a larger lateral extension gap, 16 patients (2%) a larger medial extension gap, and seven (1%) patients showed equal medial and lateral extension gaps. Mean extension gap size was 2.3 ± 2.3 mm.
Subgroup analysis showed with increasing deformity a significantly increasing difference (subgroup I: 1.6 mm larger lateral extension gap (compared with medial extension gap); subgroup II: 3.8 mm larger; subgroup III: 6.7 mm larger).
Medial/lateral difference in flexion
The lateral flexion gap (5.5 ± 2.8 mm) was significantly larger than the medial flexion gap (3.0 ± 3.3 mm; p <0.001). In 583 patients (86%), the lateral flexion gap was larger than the medial, in 71 patients (10%), the medial was larger than the lateral, and in 26 (4%), both gaps were equal. The mean flexion gap size was 4.2 ± 2.8 mm.
With increasing deformity, the inter-gap difference became significantly larger (subgroup I: 1.7 mm larger lateral flexion gap; subgroup II: 2.8 mm larger; subgroup III: 4.1 mm larger).
Difference in flexion/extension gap
On average, the flexion gap was 1.9 mm larger than the extension gap (p < 0.0001) in varus knees. In 522 out of 680 knees (77%), the flexion gap was larger. In 144 knees (21%), the extension gap was larger than the flexion gap, and in 14 knees (2%), both gaps were equal.
Subgroup analysis showed no constant effect of deformity on flexion/extension gap differences (subgroup I: 2.2 mm larger flexion than extension gap; subgroup II: 1.8 mm; subgroup III: 2.0 mm larger). The differences between all subgroups were only significant between subgroup I and II, but not between subgroups I and III and II and III.
Criteria of varus knees
The criterion that was met the most (97%), was that the lateral extension gap was larger than the medial extension gap (3.5 mm). In 86%, the lateral flexion gap was larger than the medial flexion gap (2.5 mm). The criterion that was met at least (76%), was that the flexion gap was larger than the extension gap (1.9 mm). Only 65% of all knees fulfilled all three criteria, with no gender difference between male (65%) and female (66%).
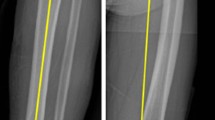
Correlation between leg alignment and medial–lateral gap size difference (Fig. 1)
The correlation between the coronal leg alignment and the medial–lateral gap difference in extension showed a high correlation of r2 = 0.62. This is documented in a constant increase of difference in extension: HKA 2° = 1.0 mm difference, HKA 5° = 2.6 mm, HKA 10° = 5.2 mm and HKA 15° = 7.8 mm.
At all flexion angles, this correlation was low r2 = 0.05 at 30°, to 0.11 at 60° to 0.16 at 90°.
Influence of patient demographics on gap size (Table 3)
Gender
Females showed significantly larger gaps of 0.5 mm in extension and flexion, demonstrating increased ligament laxity.
BMI
No differences between the different BMI groups were found for the extension gaps. Flexion gap was only significantly larger in patients with a BMI > 30 than in those between 25 and 30.
Age
In extension, younger patients (< 55 years) showed significantly lager gap sizes than the other subgroups. There was no significant difference between the latter groups or in any flexion position.
Discussion
The most important finding in this study was that varus OA knees show a large variability regarding their gap widths from extension to flexion. Although each of the three varus knee criteria was found to be significant in the overall group, only 65% of patients fulfilled all three of them. Second, the amount of varus deformity highly correlates with the differences of medial and lateral gap widths in extension; however, no correlation was found in any of the tested flexion angles. Third, women showed significantly larger gap sizes in extension and flexion compared to men, whereas other factors, such as BMI and age, had no significant influence.
Based on the fact that about 20% of patients are still dissatisfied after TKA, we need to reconsider our surgical approach to treat all varus knees as a homogeneous entity, with the same resection heights, the same alignment targets, and the same standard soft tissue release steps. It is likely that a more individualized approach might help to significantly reduce this in sometime soon [11, 34,35,36]. Some authors try to reconstruct the knee more anatomically with the tibia cut in constitutional varus [13, 37, 38]. Others attempt to restore the bony morphology of the femur first and then balance the tibia against the femur [39,40,41,42,43].
Valid quantitative data are needed for individual soft tissue envelope restoration. In this study, a dynamic CAS technique was used that has demonstrated adequate reproducibility [22]. A “standard” varus knee was described using three criteria, based on the literature [27, 30, 31]. While each criterion proved significant, only 65% of all knees met all three criteria.
It was demonstrated that varus knees generally (97%) had a significant extension gap difference, with the lateral gap being 2.3 mm larger. However, this difference is highly dependent on several factors, one of the most important being the extent of varus deformity. In a 2° varus deformity, we found a medial–lateral difference in extension of only 1.0 mm, in a 5° varus of 2.6 mm and in a 10° varus of 5.2 mm. This correlation is in agreement with Matziolis et al. [33]. However, the extent of gap difference in their study was only 0.35 mm per degree of varus, whereas in our study, it is 0.52 mm. This may be due to the smaller sample size studied by Matziolis et al. [33]. They noted that due to this correlation, it is possible to predict the amount of soft tissue release required to balance the knee in extension by pre-operatively measuring the HKA on long leg radiographs. This study was able to confirm the hypothesis. However, it should be noted that the amount of soft tissue release needed in midrange and flexion cannot be predicted with similar precision and individual intraoperative analysis is mandatory.
Other authors also found that the lateral extension gap is larger than the medial, but described the difference to be smaller. For example, Nowakowski et al. [44] described a difference of only 1.2 mm. They did not provide information on the extent of varus deformity. Matsumoto et al. [28] described the difference between medial and lateral extension gap to be 1.0 mm in knees with a varus deformity less than 10°, this difference increased to 2.7 mm in knees with a varus greater than 20°. Okamoto et al. [30] divided their knees into three groups depending on the extent of varus deformity and described a significantly larger lateral extension gap in knees with severe deformity compared to moderate or mild varus.
Another criterion of varus knees was also confirmed: the lateral flexion gap was significantly larger (2.5 mm) than the medial one. This criterion was met in 86% of patients and is in agreement with many other studies [27, 45,46,47,48]. Tokuhara et al. [49] found that the lateral flexion gap was 4 mm larger than the medial one using an in vivo MRI technique. However, in this study, only 19% of knees had a lateral flexion gap greater than 4 mm. The majority of the patients showed a difference between 2 and 4 mm. This may be due to patient situation under which the data were obtained. While, our data were collected from anesthetized patients (general or spinal) in vivo MRI requires patients to be awake. Another explanation for the slightly larger difference could be the extent of deformity.
It was found that increasing varus deformity is associated with an increase in gap difference in flexion; while subgroup I showed a difference of only 1.7 mm, this rose to 4.4 mm in subgroup III. The effect is mainly due to decreasing medial gap widths and not so much to an increase in lateral values. Furthermore, the correlation between varus deformity and gap difference in flexion is very low. These results are in agreement with other studies that described a difference of 3° (3–4 mm depending on knee size) as physiological in OA knees [44, 47, 50]. McAuliffe et al. [46] described in their CAS study a difference of less than 2.5° in 91.6% of varus knees. They concluded that this small difference reflects the fact that coronal contractures are not present in varus knees at 90°. This result is not supported by the finding of this study that the reduction in medial values is more pronounced than the increase in lateral gap widths.
The third criterion of a “standard” varus knee being that the flexion gap is larger than the extension gap, was also found to be true. However, this criterion was met in only 77% of cases. Subgroup analysis showed no significant difference between groups, indicating that the extent of varus deformity did not affect this criterion. Shalhoub et al. [32] also found that the flexion gap was larger than the extension gap. Their difference was more than 3 mm, which is slightly larger than in our group (1.9 mm). Interestingly enough, they described a constant gap width from 20° to 90° flexion, which is not consistent with the findings in this study.
Deep et al. [51] described gender as a factor, with females having larger gap sizes. In our study, this finding was confirmed. The effect was evident in both extension and flexion, the difference however, being small (0.5 mm). Van der Esch et al. [52] measured a difference of 3° in OA patients, which again was larger in women. The higher value in their study is probably due to the fact that the measurement was made in 15° of flexion and thus stabilizing structures, such as the posterior capsule, are relaxed. Other authors found a similar effect in healthy control subjects [53, 54].
One limitation of our study is that the data were collected in a supine position in anesthetized patients. Although the number of patients examined in this study was very large, they were almost entirely Caucasian, and the extent of deformity was limited to less than 20°. Whether the changes in severe cases are similar to those we have described in knees between 2 and 15° varus can only be speculated upon.
The clinical relevance of this study is that it has been demonstrated quantitatively that varus knees should not be treated as a uniform entity as they have a large variability in gap widths at different joint positions. This implicates that a uniform surgical technique will address the majority but not all varus knees adequately.
Conclusion
It was shown that ligamentous knee morphology shows a high variability. The preoperative planning of releasing steps based on the amount of varus deformity is only possible in extension, because only in extension a high correlation between both factors exists. In all flexion angles, this cannot be predicted and is highly variable. Based on the results, a preoperative analysis of all gap sizes in the entire ROM is recommended for individual soft tissue management.
References
Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW (2017) Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthoplasty 32:3854–3860
Kahlenberg CA, Nwachukwu BU, McLawhorn AS, Cross MB, Cornell CN, Padgett DE (2018) Patient satisfaction after total knee replacement: a systematic review. HSS J 14(2):192–201
Canovas F, Dagneaux L (2018) Quality of life after total knee arthroplasty. Orthop Traumatol Surg Res 104:41–46
Choi YJ, Ra HJ (2016) Patient satisfaction after total knee arthroplasty. Knee Surg Relat Res 28(1):1–15
Hossain FS, Konan S, Patel S, Rodriguez-Merchan EC, Haddad FS (2015) The assessment of outcome after total knee arthroplasty: are we there yet? Bone Joint J 97-B:3–9
Nam D, Nunley RM, Barrack RL (2014) Patient dissatisfaction following total knee replacement: a growing concern? Bone Joint J 96-B:96–100
Smith AF, Eccles CJ, Bhimani SJ, Denehy KM, Bhimani RB, Smith LS, Malkani AL (2021) Improved patient satisfaction following robotic-assisted total knee arthroplasty. J Knee Surg 34(7):730–738
Almaawi AM, Hutt JRB, Masse V, Lavigne M, Vendittoli PA (2017) The impact of mechanical and restricted kinematic alignment on knee anatomy in total knee arthroplasty. J Arthoplasty 32:2133–2140
Hirschmann MT, Müller W (2015) Complex function of the knee joint: the current understanding of the knee. Knee Surg Sports Traumatol Arthrosc 23:2780–2788
Kim K, Kim J, Lee D, Lim S, Eom J (2019) The accuracy of alignment determined by patient-specific instrumentation system in total knee arthroplasty. Knee Surg Relat Res 31(1):19–24
Rivière C, Iranpour F, Auvinet E, Howell S, Vendittoli PA, Cobb J, Parratte S (2017) Alignment options for total knee arthroplasty: a systematic review. Orthop Traumatol Surg Res 103(7):1047–1056
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27(5):1394–1402
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470:45–53
Confalonieri N, Biazzo A (2019) Computer-assisted surgery in total knee replacement: advantages, surgical procedure and review of the literature. Acta Biomed 90(1):16–23
Lee DH, Park JH, Song DI, Padhy D, Jeong WK, Han SB (2010) Accuracy of soft tissue balancing in TKA: comparison between navigation-assisted gap balancing and conventional measured resection. Knee Surg Sports Traumatol Arthrosc 18:381–387
Moon YW, Kim HJ, Ahn HS, Park CD, Lee DH (2016) Comparison of soft tissue balancing, femoral component rotation, and joint line change between the gap balancing and measured resection techniques in primary total knee arthroplasty: a meta-analysis. Medicine (Baltimore). https://doi.org/10.1097/MD.0000000000005006
Bagaria V, Sadigale OS, Pawar PP, Bashyal RK, Achalare A, Poduval M (2020) Robotic-assisted knee arthroplasty (RAKA): the technique, the technology and the transition. Indian J Orthop 54(6):745–756
Deep K, Shankar S, Mahendra A (2017) Computer assisted navigation in total knee and hip arthroplasty. SICOT J. https://doi.org/10.1051/sicotj/2017034
Hannan R, Free M, Arora V, Harle R, Harvie P (2020) Accuracy of computer navigation in total knee arthroplasty: a prospective computed tomography-based study. Med Eng Phys 79:52–59
Pertusson G, Fenstad AM, Gothesen O, Dyrhovden GS, Hallan G, Röhrl SM, Aamodt A, Furnes O (2018) Computer-assisted compared with conventional total knee replacement: a multicenter parallel-group randomized controlled trial. J Bone Joint Surg Am 100(15):1265–1274
van der List JP, Chawla H, Joskowicz L, Pearle AD (2016) Current state of computer navigation and robotics in unicompartmental and total knee arthroplasty: a systematic review with meta-analysis. Knee Surg Sports Traumatol Arthrosc 24(11):3482–3495
Mehliß V, Leira MS, Olaizola AS, Scior W, Graichen H (2019) Proven accuracy for a new dynamic gap measurement in navigated TKA. Knee Surg Sports Traumatol Arthrosc 27:1189–1195
Hirschmann MT, Hess S, Behrend H, Amsler F, Leclercq V, Moser LB (2019) Phenotyping of hip-knee-ankle angle in young non-osteoarthritic knees provides better understanding of native alignment variability. Knee Surg Sports Traumatol Arthrosc 27:1378–1384
Moser LB, Hess S, Amsler F, Behrend H, Hirschmann MT (2019) Native non-osteoarthritic knees have a highly variable coronal alignment: a systematic review. Knee Surg Sports Traumatol Arthrosc 27:1359–1367
Thienpont E, Parvizi J (2016) A new classification for the varus knee. J Arthroplasty 31:2156–2160
Deep K, Picard F, Baines J (2016) Dynamic knee behaviour: does the knee deformity change as it is flexed-an assessment and classification with computer navigation. Knee Surg Sports Traumatol Arthrosc 24:3575–3583
Bellemans J, Vandenneucker H, Vanlauwe J, Victor J (2010) The influence of coronal plane deformity on mediolateral ligament status: an observational study in varus knees. Knee Surg Sports Traumatol Arthrosc 18:152–156
Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kurosaka M, Kuroda R (2011) The influence of preoperative deformity on intraoperative soft tissue balance in posterior-stabilized total knee arthroplasty. J Arthroplasty 26:1291–1298
Meloni MC, Hoedemaeker RW, Violante B, Mazzola C (2014) Soft tissue balancing in total knee arthroplasty. Joints 2:37–40
Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Iwamoto Y (2013) Lateral soft tissue laxity increases but medial laxity does not contract with varus deformity in total knee arthroplasty. Clin Orthop Relat Res 471:1334–1342
Tanaka Y, Nakamura S, Kuriyama S, Nishitani K, Ito H, Lyman S, Matsuda S (2020) Intraoperative physiological lateral laxity in extension and flexion for varus knees did not affect short-term clinical outcomes and patient satisfaction. Knee Surg Sports Traumatol Arthrosc 28:3888–3898
Shalhoub S, Moschetti WE, Dabuzhsky L, Jevsevar DS, Keggi JM, Plaskos C (2018) Laxity profiles in the native and replaced knee-application to robotic-assisted gap-balancing total knee arthroplasty. J Arthroplasty 33(9):3043–3048
Matziolis G, Matziolis D, Perka C (2012) Pre-operative frontal plane malalignment predicts the extension gap asymmetry in knee osteoarthritis. Int Orthop 36:79–82
Hirschmann MT, Karlsson J, Becker R (2018) Hot topic: alignment in total knee arthroplasty-systematic versus more individualised alignment strategies. Knee Surg Sports Traumatol Arthrosc 26(6):1587–1588
Jaffe WL, Dundon JM, Camus T (2018) Alignment and balance methods in total knee arthroplasty. J Am Acad Orthop Surg 26(20):709–716
Karachalios T, Komnos GA (2020) Individualized surgery in primary total knee arthroplasty. EFORT Open Rev 5:663–671
MacDessi SJ, Griffiths-Jones W, Chen DB, Griffiths-Jones S, Wood JA, Diwan AD, Harris IA (2020) Restoring the constitutional alignment with a restrictive kinematic protocol improves quantitative soft-tissue balance in total knee arthroplasty: a randomized controlled trial. Bone Joint J 102-B(1):117–124
Victor JM, Bassens D, Bellemans J, Gürsu S, Dhollander AA, Verdonk P (2014) Constitutional varus does not affect joint line orientation in the coronal plane. Clin Orthop Relat Res 472(1):98–104
Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML (2013) Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res 471:1000–1007
Howell SM, Hull ML (2012) Kinematic alignment in total knee arthroplasty. In: Scott WN, Insall SK (eds) Surgery of the knee. Elsevier, Philadelphia, pp 1255–1268
Hutt JR, LeBlanc MA, Massé V, Lavigne M, Vendittoli PA (2016) Kinematic TKA using navigation: surgical technique and initial results. Orthop Traumatol Surg Res 102:99–104
Lee YS, Howell SM, Won YY, Lee OS, Lee SH, Vahedi H, Teo SH (2017) Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:3467–3479
Matsumoto T, Takayama K, Ishida K, Kuroda Y, Tsubosaka M, Muratsu H, Hayashi S, Hashimoto S, Matsushita T, Niikura T, Kuroda R (2013) Intraoperative soft tissue balance/kinematics and clinical evaluation of modified kinematically versus mechanically aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21:2338–2345
Nowakowski AM, Majewski M, Müller-Gerbl M, Valderrabano V (2012) Measurement of knee joint gaps without bone resection: “physiologic” extension and flexion gaps in total knee arthroplasty are asymmetric and unequal and anterior and posterior cruciate ligament resections produce different gap changes. J Orthop Res 30:522–527
Jenny JY (2010) Coronal plane knee laxity measurement: is computer-assisted navigation useful? Orthop Traumatol Surg Res 96:583–588
McAuliffe MJ, Roe J, Garg G, Whitehouse SL, Crawford R (2017) The varus osteoarthritic knee has no coronal contractures in 90 degrees of flexion. J Bone Joint Surg Am 30:1678–1684
Okazaki K, Miura H, Matsuda S, Takeuchi N, Mawatari T, Hashizume M, Iwamoto Y (2006) Asymmetry of mediolateral laxity of the normal knee. J Orthop Sci 11:264–266
Roth JD, Howell SM, Hull ML (2015) Native knee laxities at 0°, 45°, and 90° of flexion and their relationship to the goal of the gap-balancing alignment method of total knee arthroplasty. J Bone Joint Surg Am 97:1678–1684
Tokuhara Y, Kadoya Y, Nakagawa S, Kobayashi A, Takaoka K (2004) The flexion gap in normal knees. An MRI study. J Bone Joint Surg Br 86(8):1133–1136
Matsuda S, Ito H (2015) Ligament balancing in total knee arthroplasty—medial stabilizing technique. Asia Pac J Sports Med Arthrosc Rehabil Technol 2:108–113
Deep K (2014) Collateral ligament laxity in knees: what is normal? Clin Orthop Relat Res 472:3426–3431
van der Esch M, Steultjens MP, Lems WF, Dekker J (2007) Gender difference in varus-valgus laxity in osteoarthritis of the knee. J Rheumatol 36:157–159
Sharma L, Lou C, Felson DT, Dunlop DD, Kirwan-Mellis G, Hayes KW, Weinrach D, Buchanan TS (1999) Laxity in healthy and osteoarthritic knees. Arthritis Rheum 42:861–870
Te Molder MEM, Wymenga AB, Heesterbeek PJC (2019) Mid-flexion laxity in the asymptomatic native knee is predominantly present on the lateral side. Knee Surg Sports Traumatol Arthrosc 27(11):3614–3625
Funding
No grants or other funding were received for this study.
Author information
Authors and Affiliations
Contributions
HG conceived and planned the study. HG and WS planned and performed operations. LK and KE contributed to the processing and analysis of the data. HG took the lead in writing the manuscript. KE and MH were responsible for corrections and revisions. All authors provided critical feedback and helped design the study, analyze the data, and write the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Each author (Heiko Graichen, Kreangsak Lekkreusuwan, Kim Eller, Thomas Grau, Michael T. Hirschmann, Wolfgang Scior) confirms that he or she has no commercial affiliations that could constitute a conflict of interest in connection with the submitted article.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and its later amendments. Our evaluations were written exclusively in anonymized form and applicable data protection regulations were observed.
Informed consent
Written consent of all patients for data collection was obtained prior to Hospital entry.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Graichen, H., Lekkreusuwan, K., Eller, K. et al. A single type of varus knee does not exist: morphotyping and gap analysis in varus OA. Knee Surg Sports Traumatol Arthrosc 30, 2600–2608 (2022). https://doi.org/10.1007/s00167-021-06688-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06688-4