Abstract
Purpose
It has been hypothesized that under-correction of a preoperative varus deformity may be more natural and improve outcomes after total knee arthroplasty (TKA). This study’s purpose was to assess the impact of hip-knee-ankle (HKA) alignment and joint line obliquity on TKA outcomes for the varus knee.
Methods
All patients with a preoperative varus deformity received both preoperative and postoperative standing, full-length radiographs from which two independent observers performed radiographic measurements including the HKA axis and mechanical medial proximal tibial angle (mMPTA). Patients were categorized based on their HKA into neutral (0° ± 3°), mild varus (−6° to −3°), severe varus (≤ −6°), and valgus (>3°) cohorts, and separately categorized based on their mMPTA into neutral (90° ± 2°), mild varus (86°–88°), severe varus (<86°), and valgus (>92°) cohorts.
Results
Two hundred and fifty-six patients (mean age 63.8 ± 9.0 years, BMI 33.0 ± 6.2 kg/m2, follow-up 1.3 ± 0.6 years) were included. There was no difference in the postoperative SF-12 physical component, mental component, Oxford knee, Forgotten Joint Score, or incremental improvement in scores based on the postoperative alignment category for either the HKA or mMPTA. There was no correlation between the magnitude of change in HKA (r = 0.03–0.1) and mMPTA (r = 0.02–0.1) from preoperatively to postoperatively with clinical outcomes.
Conclusions
In patients undergoing TKA for a preoperative varus deformity, a specific postoperative HKA or mMPTA alignment category was not associated with improved outcomes. Therefore, categorization of optimal postoperative alignment after TKA may not be possible as static, coronal alignment is just one of many variables that can impact clinical outcomes. Future investigations focusing on the combination of static images with dynamic examinations and ligamentous balancing may shed further insight into the controversy and importance of coronal alignment following TKA.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite its long-term survivorship and clinical success, it has been reported that 15–30% of patients remain “dissatisfied” following primary total knee arthroplasty (TKA) [5, 24, 27]. Furthermore, a substantial percentage of patients report persistent symptoms including pain, stiffness, and noise following total knee arthroplasty [22, 27].
Traditionally, the success of TKA has been accepted to be dependent on achieving a neutral lower extremity mechanical hip-knee-ankle (HKA) axis within 3° of neutral and tibial and femoral component positions perpendicular to the mechanical axis in the coronal plane [4, 6, 7, 19, 30]. However, recent studies have challenged the importance of a neutral postoperative alignment on outcomes following TKA [3, 11, 13, 14, 26]. Parratte et al. in a review of 398 TKAs demonstrated no improvement in the fifteen-year implant survival rate in patients with or without a postoperative HKA axis within 0° ± 3°, questioning the utility of defining alignment as a dichotomous variable [26]. Recently, Van Lommel et al. retrospectively reviewed a cohort of 132 patients with a preoperative varus alignment and noted patients to have improved functional outcome scores and equivalent implant survivorship if their overall HKA alignment was left in mild varus (between 3° and 6°) versus those corrected to neutral (0° ± 3°) [33]. Furthermore, the concept of the “kinematically aligned” TKA has been introduced, with the goal to align the angle and level of the distal and posterior joint lines of the femoral component and joint line of the tibial component to those of the native knee [13]. Mid-term results of the kinematic alignment technique have been encouraging [10–13].
Therefore, several recent reports have questioned the long-held tenet of targeting a neutral HKA alignment in TKA. However, the true impact of overall HKA alignment and joint line obliquity on outcomes following TKA requires further investigation. In addition, it remains unclear whether the overall HKA alignment or the orientation of the joint line has a greater impact on clinical outcomes. The purpose of this study is to assess the impact of overall HKA alignment and joint line obliquity on outcomes following TKA for patients with a preoperative varus deformity. Our hypothesis is that in patients with a preoperative varus alignment, under-correction of the varus deformity and implantation of the tibial component in slight varus will improve short-term functional outcomes.
Materials and methods
This study was a retrospective review of prospectively collected data performed at a single institution. Patients undergoing primary total knee arthroplasty between 2011 and 2015 were reviewed. Two fellowship-trained joint replacement surgeons performed all TKAs. Inclusion criteria were patients greater than 18 years of age with a history of osteoarthritis or rheumatoid arthritis that received a primary TKA, and had both preoperative and postoperative weight-bearing, standing, full-length hip-knee-ankle radiographs available for review. Exclusion criteria were a prior history of traumatic fracture to the ipsilateral femur, knee, or tibia, neuromuscular disorders, patients unable to stand for examination, the absence of adequate preoperative and postoperative HKA radiographs, and those with a preoperative HKA valgus alignment. The study population consisted only of patients with a preoperative varus HKA alignment. All patients received a TKA with the use of an intramedullary femoral and extramedullary tibial alignment guide to perform the distal femur and proximal tibia resections, respectively.
All patients received both a preoperative and postoperative weight-bearing, standing, full-length hip-knee-ankle radiograph using either a classic HKA roentgenogram taken on a long cassette or a 2-dimensional HKA image obtained using an EOS X-Ray Imaging Acquisition System (EOS Imaging Inc., Paris, France). Hip-knee-ankle roentgenograms were obtained using a 14 × 51 inch cassette centred at the knee joint, with the patellae facing forward and the legs in full extension. The EOS system was also used to acquire standing hip-to-ankle images in patients, but only the 2-dimensional image obtained was analysed as it corresponds to a standing full-length radiograph obtained using conventional radiography [31, 32]. The decision to obtain a classic HKA roentgenogram or EOS image was solely based on the clinic site at which the patient was seen, as the EOS system was only available at one of our outpatient clinic sites.
Two independent observers performed radiographic measurements. The femorotibial angle (FTA), mechanical lateral distal femoral angle (mLDFA), mechanical medial proximal tibial angle (mMPTA), and hip-knee-ankle (HKA) axis were measured for all preoperative and postoperative radiographs. The FTA was the angle between the anatomic femoral axis and the anatomic tibial axis. The anatomic femoral axis was defined as the line connecting the midpoint of the endosteal cortices of the femoral isthmus to the midpoint of the femur 10 cm proximal to the joint line. Similarly, the anatomic tibial axis was defined as the line connecting the midpoint of the midshaft of the tibia to the midpoint of the tibia 10 cm distal to the joint line [20, 28]. The mechanical femoral axis was defined as the line connecting the centre of the femoral head, as determined by a best-fit circle, and the midpoint of the widest dimension of the distal femur. The mechanical tibial axis was defined as the line connecting the centre of the tibial spines to the centre of the talus. The mMPTA was the medial angle between the mechanical tibial axis and the joint line of the proximal tibia. For the native knee, this was the line that connects the highest points of the medial and lateral tibial plateaus. After TKA, the joint line was set parallel to the inferior aspect of the tibial component’s metal tray. The mLDFA was defined as the lateral angle between the mechanical femoral axis and the joint line of the distal most aspects of the medial and lateral femoral condyles for both the native and replaced knees [23] (Fig. 1). The HKA was determined as the angle between the mechanical axes of the femur and tibia [2]. The HKA was expressed as a deviation from 0°, with varus assigned a negative value and valgus a positive value (Fig. 2). Lastly, the zone of the mechanical axis (ZMA) was measured for each patient postoperatively, which is the zone through which the line connecting the centre of the femoral head to the centre of the ankle passes when the tibial baseplate is divided into five equal zones as described by Kennedy and White [17]. For convention, zone 0 was considered medial to the tibial baseplate, and zone 6 lateral to the tibial baseplate, with zones 1 through 5 equally dividing the tibial baseplate from a medial to lateral direction (Fig. 3).
Baseline demographics including age (years), body mass index (BMI: kg/m2), and gender were recorded. SF-12 physical component (PCS) and mental component (MCS) [34], and Oxford knee scores [9] were obtained for each patient preoperatively and at the most recent follow-up visit. In addition, the Forgotten Joint Score [1] was recorded for patients at their most recent follow-up visit. This was an Institutional Review Board (IRB)-approved investigation (Washington University School of Medicine, St. Louis, Missouri, USA; IRB approval number 201101880).
Statistical analysis
To assess the impact of postoperative HKA alignment on clinical outcomes, patients were first divided into four groups based on their postoperative HKA alignment: neutral (HKA of 0° ± 3°), mild varus (−6° < HKA < −3°), severe varus (HKA ≤ −6°), and valgus (HKA >3°) [33]. Further analyses were performed dividing the “neutral” HKA cohort into varus/neutral (0° > HKA ≥ −3°) and valgus/neutral (0° < HKA ≤ 3°) subgroups, and also strictly comparing patients with a postoperative varus (HKA <0°) versus valgus (HKA >0°) alignment. Similarly, patients were also divided into four groups based on their postoperative tibial component alignment measured as the mMPTA: neutral (90° ± 2°), mild varus (86°–88°), severe varus (<86°), and valgus (>92°). Comparisons were also performed after categorizing patients based on their postoperative ZMA measurement. Baseline demographics and clinical outcomes measures were compared amongst the groups using χ 2 tests for categorical variables and non-parametric Kruskall–Wallis tests for continuous variables with a p value < 0.05 considered statistically significant. All tests were two sided. SAS 9.1 (SAS Institute Inc., Cary, NC, USA) was used for all statistical procedures.
Correlation coefficients were performed to compare radiographic measurements amongst the two independent observers and were graded using previously described semiquantitative criteria: excellent for 0.9 ≤ r ≤ 1, good for 0.7 ≤ r ≤ 0.89, fair/moderate for 0.5 ≤ r ≤ 0.69, low for 0.25 ≤ r ≤ 0.49, and poor for r ≤ 0.24 [21]. In addition, intra-observer correlation coefficients were calculated for each observer as they performed two measurements for each radiograph at a minimum of two weeks apart. Correlation coefficients were also used to assess if the difference between the preoperative and postoperative HKA (alignment correction), or preoperative and postoperative mMPTA (alteration of the joint line), was associated with clinical outcome scores. Lastly, to our knowledge the association between the postoperative HKA alignment and ZMA category has not been assessed, and thus their correlation was assessed.
A post hoc power analysis was performed to address the research question that under-correction of a varus deformity would improve postoperative clinical outcomes. It was determined that a sample size of 149 patients in a neutral postoperative alignment and 88 patients in a varus postoperative alignment would provide appropriate power (beta level = 0.80, alpha level = 0.05) to detect a five-point difference in the Oxford knee score at the most recent follow-up visit. A five-point difference in the Oxford knee score has been reported to be a minimal clinically important difference; thus, our study was adequately powered to detect this difference [8].
Results
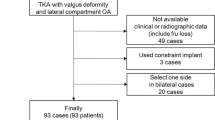
Three hundred thirty-one patients with both preoperative and postoperative HKA imaging were available for review. Of these patients, 256 (129 females, 127 males) had a preoperative varus alignment and were included for analysis (mean age 63.8 ± 9.0 years, mean BMI 33.0 ± 6.2 kg/m2). The mean preoperative and postoperative radiographic alignments are presented in Table 1. Both intra- and inter-observer correlations were good to excellent for all radiographic measurements (r = 0.87–0.96). At a mean follow-up of 1.3 ± 0.6 years, there was an improvement in the mean SF-12 PCS and Oxford knee scores for the entire cohort (Table 2).
To determine the impact of postoperative HKA alignment on clinical outcomes, patients were first divided into neutral (n = 149), mild varus (n = 60), severe varus (n = 28), and valgus (n = 19) cohorts (Table 3). As expected, postoperative radiographic measurements of the HKA, mMPTA, and mLDFA were different amongst the four cohorts (Table 4). There was no difference in the postoperative SF-12 PCS, SF-12 MCS, Oxford knee score, or Forgotten Joint Score amongst the four cohorts, or in the incremental difference in outcome scores from preoperatively to postoperatively amongst the four cohorts (n.s.; Table 5). However, patients in the severe varus cohort did have a significantly decreased postoperative SF-12 PCS score versus patients in the neutral cohort (p = 0.03), although no other inter-cohort differences were appreciated. After dividing the “neutral” cohort into those with a varus/neutral (0° > HKA ≥ −3°; n = 99) and valgus/neutral (0° < HKA ≤ 3°; n = 50) alignment, no differences were present in the preoperative or postoperative SF-12 PCS, SF-12 MCS, Oxford knee, or Forgotten Joint Scores when compared to the mild varus, severe varus, or valgus cohorts (n.s.). Lastly, no differences were present in the preoperative or postoperative SF-12 PCS, SF-12 MCS, Oxford knee, or Forgotten Joint Scores when comparing all patients with a postoperative varus (HKA < 0°; n = 184) versus valgus (HKA > 0°; n = 72) alignment (n.s.; Table 6).
To determine the impact of postoperative mMPTA alignment on clinical outcomes, patients were divided into neutral (n = 181), mild varus (n = 44), severe varus (n = 6), and valgus (n = 25) cohorts (Table 7). There was no difference in the preoperative HKA, mMPTA, or mLDFA amongst the four cohorts. As expected, postoperative radiographic measurements of the HKA and mMPTA were different amongst the four cohorts, although there was no difference in the postoperative mLDFA.(Table 8). There was no difference in the postoperative SF-12 PCS, Oxford Knee Score, or Forgotten Joint Score amongst the four cohorts, or change from preoperatively to postoperatively in any clinical outcome score amongst the four cohorts (p value n.s., Table 9). The magnitude of change from preoperatively to postoperatively of both the HKA alignment (r = 0.03 to 0.1) and mMPTA (r = 0.02 to 0.1) did not correlate with an improvement in clinical outcome scores.
Categorization of patients based on their ZMA had a good to excellent degree of correlation with the HKA alignment measurement (r = 0.85). After categorization of patients based on their ZMA (1, n = 13; 2, n = 89; 3, n = 127; 4, n = 25; 5, n = 2), again no difference was appreciated in the preoperative or postoperative SF-12 PCS, SF-12 MCS, or Oxford Knee Scores (n.s.). There was also no difference in the postoperative Forgotten Joint Score or incremental improvement in clinical outcome scores between the five categories (r = 0.1 to 0.8).
Discussion
The most important finding of the presents study was that in patients undergoing TKA for a preoperative varus deformity, we could not identify a specific category of alignment based on the postoperative HKA or mMPTA that was associated with improved clinical outcomes. Thus, radiographic categorization of an optimal postoperative coronal alignment following TKA may not be possible.
With a growing population of patients undergoing total knee arthroplasty and the increased recognition that a substantial percentage of patients remain dissatisfied postoperatively, the optimal coronal alignment in TKA continues to be investigated [18]. Recent studies have questioned the long-held tenet of targeting a neutral HKA alignment in TKA and its impact on both implant survivorship and clinical outcomes, with several investigations hypothesizing a neutral alignment and perpendicular joint line to be unnatural for a subset of patients [2, 13]. The concept of constitutional varus has suggested that residual under-correction of a preoperative HKA varus alignment may lead to improved outcomes [33], while the kinematic alignment technique has emphasized the importance of restoration of a patient’s native joint line regardless of the final HKA alignment achieved [13]. Thus, questions remain regarding the relative impact of HKA and joint line alignment on clinical outcomes following TKA.
This study has several limitations that must be recognized prior to interpretation of its results. First, as this study was a retrospective review only, the presence of an association between postoperative alignment and clinical outcomes, and not necessarily causation, can be determined. Second, the number of patients who had both preoperative and postoperative standing, hip-knee-ankle imaging, and a preoperative varus deformity limited our overall cohort size. However, to our knowledge, the only prior investigation assessing the clinical impact of under-correction of HKA alignment included only 132 patients [33], and thus we were able to nearly double this cohort size. Third, as with all radiographic assessments of coronal plane alignment, it is known that rotational attitudes can affect standard measurements of limb alignment [16, 29]; thus, variability in lower extremity rotation during image acquisition could impact our results. However, a detailed uniform protocol was followed to obtain each image to minimize this variability, and we believe a standing hip-knee-ankle image remains the most reasonable image to measure functional HKA alignment. Lastly, mean follow-up of our study was 1.3 years and thus we cannot comment on the impact of HKA or joint line alignment on implant survivorship. However, this was not the purpose of this study as the goal was to assess clinical function based on alignment, and prior larger investigations have already recently reported on the impact of alignment on implant survivorship [26, 30 ].
The optimal coronal alignment following TKA continues to be an evolving area of controversy. Historical studies on implant survivorship and design have led to the traditional targets of a neutral HKA axis, and tibial and femoral component positions perpendicular to their mechanical axes in the coronal plane [4, 15]. However, a number of these prior investigations utilized a short anteroposterior knee radiograph as a surrogate measure for mechanical alignment, which can be an inaccurate proxy for full-length HKA measurements [25]. Parratte et al. demonstrated no improvement in the 15-year implant survival rate in patients with or without a postoperative HKA axis within 0° ± 3°, questioning the utility of this traditional target [26]. Furthermore, the concept of constitutional varus at skeletal maturity has led to the hypothesis that under-correction of a varus HKA deformity may be more natural for patients undergoing TKA, while also limiting the degree of ligamentous release required. Van Lommel et al. demonstrated that in patients with a preoperative varus deformity, Knee Society Score (KSS) and Western Ontario and McMaster Universities Arthritis Index (WOMAC) were improved in patients with a mild varus HKA alignment (3° and 6°) without compromising implant survivorship [33]. However, limitations of this study were that there were only 46 TKAs in the mild varus and 75 TKAs in the neutral cohorts, and no measurements were performed assessing the alignment of the joint line itself. The present study did not corroborate these prior findings, as no differences were present in the postoperative or incremental improvement of outcome scores between patients categorized as neutral, mild varus, severe varus, or valgus based on their HKA axis. However, patients left in severe varus did have a significantly decreased postoperative SF-12 PCS versus patients in the neutral cohort. Further subgroup analyses of varus/neutral and valgus/neutral TKAs also failed to demonstrate an optimal category for postoperative alignment, and there was no correlation between the magnitude of change in the HKA and clinical outcomes. Thus, the potential for identifying an optimal category of HKA coronal alignment following TKA must be questioned.
The kinematic alignment technique has received increased attention and focuses on restoration of the patient’s native joint line via measured resections of the distal and posterior femur that equal the thickness of the femoral component to be implanted, after accounting for cartilage wear and kerf of the saw blade, [12]. Thus, this technique focuses solely on establishment of the joint line, with the resultant HKA alignment being secondary. In a prospective, randomized controlled trial of 44 TKAs receiving a kinematic alignment technique and 44 TKAs receiving a mechanical alignment technique, Dossett et al. found the femoral component to be in a mean of 2.1° more valgus and tibial component in 2.2° more varus than in the mechanically aligned cohort, but with no difference in the mean HKA alignment. Furthermore, patients in the kinematic alignment cohort demonstrated improved mean Oxford, KSS, and WOMAC scores at 2-year follow-up [10]. Thus, there is the potential that the presence of joint line obliquity could account for these improved outcomes. However, it is important to note that the kinematic alignment technique does not target a specific category of joint line alignment (i.e. 2° of tibial varus) and the joint line orientation can vary on a patient-specific basis. In an attempt to assess the impact of joint line obliquity on TKA outcomes, in this study patients were categorized based on their postoperative tibial component alignment. The present study did not see any difference in incremental improvement in outcome scores in those with a neutral, mild varus, severe varus, or valgus mMPTA postoperatively. Thus, the potential for identifying an optimal category for tibial component alignment following TKA must also be questioned. While postoperative alignment remains an important variable for implant survivorship following TKA, surgeons can use the information from this investigation to reinforce that coronal alignment remains just one aspect that impacts clinical outcomes, and attention should continue to be focused on appropriate ligamentous balancing, component rotation, and other surgical variables known to improve the success of TKA.
Conclusion
In this investigation of patients undergoing TKA for a preoperative varus deformity, a specific postoperative HKA or tibial alignment category could not be identified that was associated with improved outcomes. Therefore, our investigation questions whether it will be possible to identify an optimal category of HKA or mMPTA alignment following TKA as this remains just one of many variables that impact the clinical outcome. Future investigations focusing on the combination of static images with dynamic examinations and ligamentous balancing may shed further insight into the controversy and importance of coronal alignment following TKA.
References
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 27(430–436):e1
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470:45–53
Bellemans J (2011) Neutral mechanical alignment: a requirement for successful TKA: opposes. Orthopedics 34:e507–e509
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE (2004) Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Chao EY, Neluheni EV, Hsu RW, Paley D (1994) Biomechanics of malalignment. Orthop Clin North Am 25:379–386
Choong PF, Dowsey MM, Stoney JD (2009) Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty 24:560–569
Clement ND, MacDonald D, Simpson AH (2014) The minimal clinically important difference in the Oxford knee score and short form 12 score after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:1933–1939
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 80:63–69
Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG (2014) A randomised controlled trial of kinematically and mechanically aligned total knee replacements: Two-year clinical results. Bone Joint J 96-B:907–913
Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG (2012) Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics 35:e160–e169
Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML (2013) Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res 471:1000–1007
Howell SM, Papadopoulos S, Kuznik KT, Hull ML (2013) Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc 21:2271–2280
Howell SM, Hodapp EE, Vernace JV, Hull ML, Meade TD (2012) Are undesirable contact kinematics minimized after kinematically aligned total knee arthroplasty? An intersurgeon analysis of consecutive patients. Knee Surg Sports Traumatol Arthrosc 21(10):2281–2287
Jeffery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Joint Surg Br 73:709–714
Jiang CC, Insall JN (1989) Effect of rotation on the axial alignment of the femur. Pitfalls in the use of femoral intramedullary guides in total knee arthroplasty. Clin Orthop Relat Res 248:50–56
Kennedy WR, White RP (1987) Unicompartmental arthroplasty of the knee. Postoperative alignment and its influence on overall results. Clin Orthop Relat Res 221:278–285
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89:780–785
Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R (2009) Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty 24:570–578
Moreland JR, Bassett LW, Hanker GJ (1987) Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am 69:745–749
Munro BH (1997) Correlation. In: Statistical methods for healthcare research, 3rd edn. Lippincott-Raven, pp 224–245
Nam D, Berend ME, Nunley RM, Della Valle CJ, Berend KR, Lombardi AV, Barrack RL (2016) Residual symptoms and function after unicompartmental and total knee arthroplasty: comparable to normative controls? J Arthroplasty 31(10):2161–2166
Nam D, Maher PA, Robles A, McLawhorn AS, Mayman DJ (2013) Variability in the relationship between the distal femoral mechanical and anatomical axes in patients undergoing primary total knee arthroplasty. J Arthroplasty 28(5):798–801
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The john insall award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43
Park A, Stambough JB, Nunley RM, Barrack RL, Nam D (2015) The inadequacy of short knee radiographs in evaluating coronal alignment after total knee arthroplasty. J Arthroplasty 31(4):878–882
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92:2143–2149
Parvizi J, Nunley RM, Berend KR, Lombardi AV, Ruh EL, Clohisy JC, Hamilton WG, DellaValle CJ, Barrack RL (2014) High level of residual symptoms in young patients after total knee arthroplasty. Clin Orthop Relat Res 472(1):133–137.
Petersen TL, Engh GA (1988) Radiographic assessment of knee alignment after total knee arthroplasty. J Arthroplasty 3:67–72
Radtke K, Becher C, Noll Y, Ostermeier S (2010) Effect of limb rotation on radiographic alignment in total knee arthroplasties. Arch Orthop Trauma Surg 130:451–457
Ritter MA, Faris PM, Keating EM, Meding JB (1994) Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res 299:153–156
Than P, Szuper K, Somoskeoy S, Warta V, Illes T (2012) Geometrical values of the normal and arthritic hip and knee detected with the EOS imaging system. Int Orthop 36:1291–1297
Thelen P, Delin C, Folinais D, Radier C (2012) Evaluation of a new low-dose biplanar system to assess lower-limb alignment in 3D: a phantom study. Skeletal Radiol 41:1287–1293
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21(10):2325–2330
Ware JE, Kosinski M, Keller SD (1996) A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest directly related to the content of this study. One author (DN) is a paid consultant of Acelity Inc., Smith and Nephew Inc., and ZimmerBiomet Inc. He also is on the surgeon advisory board and has stock options in OrthAlign Inc.. A second author (RLB) is a paid consultant of Stryker Inc. and receives research support from Stryker INc., Wright Medical Inc., Smith and Nephew Inc., and Mobile Compression Systems Inc.
Ethical approval
Appropriate institutional review board approval was obtained for this study.
Informed consent
All patients participating in this investigation signed informed consent to be part of our institution’s joint replacement repository.
Rights and permissions
About this article
Cite this article
Rames, R.D., Mathison, M., Meyer, Z. et al. No impact of under-correction and joint line obliquity on clinical outcomes of total knee arthroplasty for the varus knee. Knee Surg Sports Traumatol Arthrosc 26, 1506–1514 (2018). https://doi.org/10.1007/s00167-017-4507-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4507-9