Abstract
Purpose
The aim of this study was to assess the kinematics of arthritic knees prior to TKA. The hypothesis was that the arthritic knee follows distinct patterns with regard to deformity in coronal plane as it flexes from extended position.
Method
Data from 585 consecutive arthritic knees that had undergone TKA using two non-image-based navigation systems were included in the study. Coronal plane alignment given by the femoro-tibial mechanical angle (FTMA) was recorded in extension, 30°, 60°, 90° and maximum flexion prior to making any bony cuts or ligamentous releases.
Results
Complete data were available for 512 (87.5 %) of arthritic knees. It was found that pre-implant arthritic knees behaved in different distinct patterns from full extension to 90° flexion. These patterns in FTMA from extension through to 90° of flexion were classified into 4 major types (1, 2, 3, and 4) and 8 subgroups (1A, 1B, 2A, 2B, 3, 4A, 4B, 4C) for varus and valgus knees. Beyond 90° of flexion, there were no distinct or consistent patterns. There were differences between varus and valgus knee deformities not only in overall numbers (73.8 % varus vs. 21.1 % valgus) but also in kinematic behaviour. Only 14.1 % of total knees had a consistent deformity (Type 1A) which remained the same throughout the range of flexion. 14.1 % knees actually become opposite deformity as the knee flexes; thus, varus becomes valgus and valgus becomes varus as the knee flexes (Type 3 and 4C).
Conclusion
This study has observed and categorised distinct patterns which arthritic knees follow in the coronal plane as it flexes. This dynamic change during flexion will have bearing on collateral releases that are traditionally done based on deformity in extension or 90° flexion mainly. This may be the underlying cause of flexion instability especially for Types 3 and 4C knees if collateral soft tissue release is done based on deformity in extension. Full significance of this remains unknown and will need further investigation.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The evaluation of preoperative knee deformity remains fundamental in total knee arthroplasty (TKA); bone cuts and soft tissue can be adjusted to produce optimum outcomes as malalignment and instability are two of the most frequent causes of TKA failure [3, 28]. Varus and valgus knee deformity has been traditionally defined as coronal deformity in extended position of the knee. Long-leg radiographs including the hip, knee, and ankle (HKA radiographs) in extension are still regularly used to measure preoperative leg alignment [19]. Nevertheless, the inaccuracy of long-leg radiographs is well documented in the literature and is still subject to controversy [4, 25, 32].
With the advent of computer-assisted surgery (CAS), it has become possible to study knee alignment and kinematics for each individual patient as they undergo knee surgery. This technology allows for the real-time evaluation of coronal alignment during the surgical procedure [2]. It also allows for the dynamic kinematic measurement of coronal alignment through the full range of knee flexion [12]. Siston et al. [29] showed that knees with valgus and varus deformities had different behaviour during flexion. Therefore, while radiographs evaluate the static alignment of lower limbs in standing or supine position and label knee alignment as neutral, varus, or valgus depending on the deviation of leg in coronal plane in extension, CAS evaluates dynamic FTMA (femoro-tibial mechanical alignment) through the full range of movement from extension to flexion (dynamic mechanical alignment).
During total knee arthroplasty, the release of soft tissues may be performed according to radiographic and clinical assessment: the medial anatomical structures for varus and lateral structures for valgus deformities [22]. Other studies have shown that navigation helps improve soft tissue management, tailoring soft tissue releases to the individual patient following computer-assisted kinematic measurements [10, 17, 24]. The ability to measure coronal alignment throughout the range of motion may offer the opportunity to further personalise the soft tissue management of TKA patients. Indeed, the traditional approach to TKA surgery is based on the assumption that the coronal deformity remains the same throughout flexion as it is in extension.
Study questions were as follows: (1) Do the arthritic knees follow certain patterns in dynamic coronal alignment? (2) Are certain patterns in kinematic behaviour more prevalent than others? This study classifies the dynamic alignment patterns of the arthritic knees as it moves from extension to flexion.
Materials and methods
The Golden Jubilee National Hospital research ethics board was approached, and it was determined that ethical approval was not required for this study. Therefore, the study was carried out as an audit under the clinical governance of our institution. A consecutive series of patients undergoing TKA for knee arthritis were included. They were under the care of three consultants who use computer navigation routinely in their standard TKA practice. There were no exclusion criteria for any of the patients who underwent TKA with computer-assisted navigation.
A total of 585 arthritic knees (KD 227, FP 199, JB 159) were included in the study. These included 326 (55.7 %) females and 259 (44.3 %) males with a mean age of 68.9 years (range 42 to 92). The left knee was involved in 296 (50.6 %) cases. Long-leg radiographs (HKA) were measured pre-op using Moreland protocol [21].
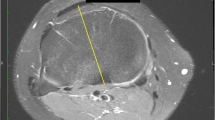
Two different validated CE Marked CT-free navigation systems were used, Orthopilot® (BBraun Aesculap, Tuttlingen, Germany) and Stryker (Stryker, Mahwah, New Jersey 07430, USA). Both systems are based on similar principles of hip, knee, and ankle centre acquisition via kinematic and anatomical landmark registration processes. Both systems used kinematic acquisition of the hip centre and anatomical acquisition of the knee and ankle centres. The Orthopilot® system in addition used kinematic acquisition of knee and ankle centres. From these data, the femoral and tibial mechanical axes are defined. The knee rotation axis taken in computer-assisted measurement is either the posterior condylar axis (PCA) for Orthopilot® or the mean of AP and transepicondylar axis for the Stryker system. Therefore, during knee flexion, the projected femoral mechanical axis onto the reference plane determines the varus and valgus angles (Fig. 1). The sagittal plane is formed perpendicular to the computed coronal plane. Thus, during knee flexion, the measurement of the FTMA in the coronal plane can be displayed for every degree of flexion (Fig. 2).
In Figs. 3, 4, 5, 6, 7, 8, 9, 10, and 11, the Y-axis shows the amount of flexion in the range of movement of knee at that point of time which shows the varus valgus on X-axis. X-axis shows the amount of varus or valgus in degrees at different points of degrees of flexion noted on y-axis.
After knee exposure, dynamic reference bases (DRB) with active tracker systems were fixed onto the femur and tibia. Surgical exposure of the joint was performed to allow the patient’s anatomy to be registered according to standard procedure. Minimal soft tissue dissection was carried out in order to collect appropriate kinematic and anatomical data of the knee. Coronal plane alignment given by the femoro-tibial mechanical angle (FTMA) was recorded in extension, 30°, 60°, 90° and maximum flexion before making any bony cuts or ligamentous releases. Klein’s protocol [14, 16] was used to assess each knee. One hand held the heel and the other was underneath the thigh. The knee was then flexed passively from extension to maximum flexion without influencing the knee’s natural kinematic behaviour. No varus or valgus stress was applied to record this part. The collected data were recorded and stored on a computer navigation file. Data for all patients were extracted from these navigation files into Microsoft Excel 2003 (Microsoft Corp, Redmond, WA, USA) and then used to assess the change in coronal alignment throughout the range of motion.
Classification: definitions
The coronal deformity with CAS was investigated and classified according to the following criteria:
The lower limb alignment in extension was used to decide whether the knee was in the neutral, varus, or valgus group. A deviation of more than 2° was taken to denote a change in coronal alignment (as the navigation system’s accuracy is within 1°). A knee would be classified as neutral if it remained within ±2° of 0° coronal alignment throughout the range of flexion. Different patterns observed were then classified (Table 1). Due to the possible effect of the tourniquet during knee flexion and no specific patterns observed in more than 90° flexion, measurements only up to 90° of flexion were used in the classification.
Statistical analysis
Once the variation in behaviour had been identified and classified, SPSS v 17.0 (IBM, Armonk, NY, USA) was used for tabulations and descriptive statistics.
Results
The computer navigation data were available for 512 (87.5 %) knees.
Classification: groups
It was found that pre-implant knees behaved in different distinct patterns from full extension to 90° flexion. Various patterns in FTMA from extension through to 90° of flexion were identified, giving a total of 4 types and 8 subtypes for both varus and valgus knees (Table 1).
Classification: prevalence
According to our classification, 26 (5.1 %) knees were neutral, 378 (73.8 %) knees were in varus, and 108 (21.1 %) knees were in valgus in full extension (Table 2). A consistent level of deformity (Type 1A) was present in only 72 (14.1 %) of knees, and the deformity became an opposite deformity (varus becomes valgus and vice versa) through flexion (Type 3 and Type 4C) in 72 (14.1 %) knees (Table 2; Fig. 3). In 50 % knees, the deformity reduced from its original extension deformity as the knee flexed. Frequency of different patterns is detailed in Table 2.
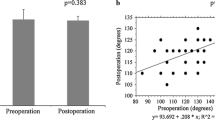
No correlation was found between the long-leg radiographic deformity type or severity to the pattern of knee deformity in flexion. So it was unpredictable from the radiographs as to what pattern the knee will follow when flexed.
Discussion
The most important findings of the present study were as follows: (1) the arthritic knees follow certain patterns in dynamic coronal alignment; (2) certain patterns in kinematic behaviour are more prevalent than others as shown in (Table 2). This study classified the dynamic alignment patterns of the arthritic knees as it moves from extension to flexion (Table 1).
To the best of our knowledge, this is the largest series of arthritic knee deformity dynamic assessment with a comprehensive analysis and classification. There are differences between varus and valgus knee deformities not only in overall numbers (73.8 % varus vs. 21.1 % valgus) but also in kinematic behaviour; only 14.1 % of total knees have a consistent deformity (Type 1A) which remains the same throughout the range of flexion.
These distinct kinematic patterns may have an effect on soft tissue management during surgery. The traditional approach to TKA surgery is based on the assumption that the coronal deformity in extension will remain the same throughout flexion. This study confirms that this is the case only in 14.1 % of our patients. However, numerous studies have shown for instance that tightness in extension in a varus knee needs different management than tightness in flexion [22, 23, 31]. Additionally, valgus knees deserve distinct management depending on the reducibility of the deformity [5]. In this study, the deformity in 49.5 % of patients decreased while it reversed for 14.1 % of patients. If traditional releases were carried out in these knees, kinematics might have been made worse. This may be a factor responsible for flexion instability which is seen in some knees post-TKA. This will especially be applicable to Type 3 knees which is mainly a consequence of dysplastic condylar anatomy rather than soft tissue imbalance. Olcott et al. [23] found that any one method based on bony landmarks is responsible for at least 10 % of flexion asymmetry. Whiteside as well as Mihalko et al. have shown that balancing ligaments after a posterior femoral cut may create imbalance between flexion–extension [20, 31]. Colle et al. [7] also found that the knee functional flexion axis changes significantly in frontal plane, when they analysed extension to 120 degree kinematics from extension to passive flexion. Therefore, identifying knee kinematic patterns prior to making bone cuts or soft tissue releases may be useful in managing gaps in flexion and in extension during TKA.
Before considering the use of these data for any algorithm in the management of soft tissue release, it is important to understand the meaning of these dynamic coronal plane mechanical angles. Indeed, it has been established for many years that normal knee motion from extension to flexion shows a posterior move of the knee’s instant centre pathway. This move is related to rolling at the beginning of flexion and sliding at the end of femur to the tibial plateau [15]. The coupled motion is called screw-home mechanism combining motion in the sagittal plane (flexion/extension) and automatic rotation during flexion [1]. Computer-assisted navigation allows for the measurement of the femoral mechanical axis (between the centre of the hip and the centre of the knee) and the tibial mechanical axis (between the centre of the knee and the centre of the ankle). Therefore, during knee flexion, the recorded leg varus/valgus angles are a combination of the knee’s three-dimensional movements projected onto the femoral reference plane.
Arthritic knee kinematics and deformity are a result of a combination of bony anatomy, osteophytes, cartilage degeneration, soft tissue changes, and adhesions. It is difficult to evaluate the accountability of each isolated component in kinematic behaviour. Romero et al. [27] used a similar frame of reference to assess varus and valgus laxity using a loading apparatus displacing the tibia medially or laterally. This experiment showed that in extension neither external nor internal malrotation of the femoral component up to 6° had any effect on ligamentous stability. On the contrary, at 30° or 60° of knee flexion, a femoral component set at 6° for both internal and external rotation had an effect on varus/valgus laxity. Robkopf et al. [26] found they had to flex the femoral component to approximately 3° to balance the medial and lateral flexion and extension gaps. Traditionally even when using gap balancing technique, the soft tissue tension is measured in extension and 90° of flexion but misses the range between these measurements which may be of great significance in aetiology of the midflexion instability. Measuring pre-implant knee kinematics through the flexion may help improve our understanding of individual knee behaviour in the future. Release of medial or lateral collateral soft tissues, without an understanding of how the deformity behaves in flexion, may lead to worsening of kinematics. While this may correct the knee deformity in extension, it may make knee unstable in flexion. This will be especially applicable for Types 2, 3, and 4C knees where the deformity is reduced or reversed in flexion. Ghosh et al. [9] found in their cadaveric study of kinematic envelop of laxity there is a wide range of midflexion excursion in the knee. They also recommended evaluation of the knee kinematics to optimise the knee replacement outcomes [9]. Venkatesan et al. [30] noted in a critical analysis of computer navigation in TKR that it may be of value in complex deformity, revision surgery, and minimally invasive surgery.
This study used Klein’s assessment method to measure lower limb alignment through the range of motion [14]. There are some limitations in this method such as the difficulty in assessing heavy legs, the effect of tourniquet, and the degree of knee release as a result of exposure prior to measurements, although this was kept to a minimal and no bony cuts or ligamentous releases were attempted before recording. The computer-assisted technique is reliable and repeatable for measuring FTMA in extension [6, 13]. In flexion, FTMA was found to be less repeatable by Hauschild et al. [11]. They observed an increased tendency of intra-observer errors for those with less clinical experience. However, this study was carried out by experienced surgeons [18]. This is an attempt at classification of different patterns, which like any classification may have limitations. This can be strengthened by independent assessment from other institutions in the future. Another weakness may be that there were 3 different surgeons and 2 navigation systems. However, knee samples could vary between the two systems and may slightly change the figures, but still allowed the different patterns to be identified. This becomes a strength as well, as the patterns observed were similar for both the navigation systems and all the surgeons. Another limitation in our study can be that complete data were not available for all the patients (512/585). However, more than 500 patients had complete data sets available for all the parameters observed so this is a large and hopefully representative data set.
Clinical relevance of the study is in the assessment of the dynamic behaviour before making collateral soft tissue release. In Types 2, 3, and 4C knees, over release may lead to flexion instabilities. So one needs to be careful and do the collateral release in a controlled manner assessing its effect at each stage of release. While using gap balancing technique, the soft tissue tension is traditionally measured in extension and 90° of flexion but misses the flexion range between these measurements, which may be of significance in aetiology of the midflexion instability or post-operative satisfaction. Also the equality of tension/laxity on medial and lateral soft tissue/ligamentous structures in normal knees has recently been questioned as collateral laxity maybe different on medial and lateral sides [8]. Thus, rather than just assessing the gaps, the dynamic behaviour should also be assessed through the range of flexion. It is open to discussion if surgeons should be doing differential collateral releases in TKA surgery to address only part of the range of movement where it is needed, rather than doing medial or lateral collateral release as a whole, which may be unnecessary or make the kinematics worse. This will need further clinical evaluation.
Conclusion
This study has observed, defined, and classified definite patterns which arthritic knees follow in the coronal plane. The full significance of this is still unexplored, and more questions have been raised which need further evaluation.
References
Andriacchi TP, Stanwyck TS, Galante JO (1986) Knee biomechanics and total knee replacement. J Arthroplast 1:211–219
Austin MS, Ghanem E, Joshi A, Trappler R, Parvizi J, Hozack WJ (2008) The Assessment of intraoperative prosthetic knee range of motion using two methods. J Arthroplast 23:515–521
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE (2004) The Chitranjan Ranawat Award: tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34
Choi WC, Lee S, An JH, Kim D, Seong SC, Lee MC (2011) Plain radiograph fails to reflect the alignment and advantages of navigation in total knee arthroplasty. J Arthroplast 26:756–764
Clarke HD, Fuchs R, Scuderi GR, Scott WN, Insall JN (2005) Clinical results in valgus total knee arthroplasty with the “pie crust” technique of lateral soft tissue releases. J Arthroplast 20:1010–1014
Clarke JV, Wilson WT, Wearing SC, Picard F, Riches PE, Deakin AH (2012) Standardising the clinical assessment of coronal knee laxity. Proc Inst Mech Eng H 226:699–708
Colle F, Bruni D, Iacono F, Visani A, Zaffagnini S, Marcacci M, Lopomo N (2016) Changes in the orientation of knee functional flexion axis during passive flexion and extension movements in navigated total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24(8):2461–2469
Deep K (2014) Collateral ligament laxity in knees: what is normal? Clin Orthop Relat Res 472(11):3426–3431
Ghosh KM, Blain AP, Longstaff L, Rushton S, Amis AA, Deehan DJ (2014) Can we define envelope of laxity during navigated total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(8):1736–1743
Hakki S, Coleman S, Saleh K, Bilotta VJ, Hakki A (2009) Navigational predictors in determining the necessity for collateral ligament release in total knee replacement. J Bone Joint Surg Br 91:1178–1182
Hauschild O, Konstantinidis L, Strohm PC, Niemeyer P, Suedkamp NP, Helwig P (2009) Reliability of leg alignment using the OrthoPilot system depends on knee position: a cadaveric study. Knee Surg Sports Traumatol Arthrosc 17:1143–1151
Hüfner T, Meller R, Kendoff D, Zeichen J, Zelle BA, Fu FH, Krettek C (2005) The role of navigation in knee surgery and evaluation of three-dimensional knee kinematics. Oper Tech Orthop 15:64–69
Jenny JY, Boeri C, Picard F, Leitner F (2004) Reproducibility of intra-operative measurement of the mechanical axes of the lower limb during total knee replacement with a non-image-based navigation system. Comput Aided Surg 9:161–165
Klein GR, Restrepo C, Hozack WJ (2006) The effect of knee component design changes on range of motion evaluation in vivo by a computerized navigation system. J Arthroplast 21:623–627
Komistek RD, Dennis DA, Mahfouz M (2003) In vivo fluoroscopic analysis of the normal human knee. Clin Orthop Relat Res 410:69–81
Lee DC, Kim DH, Scott RD, Suthers K (1998) Intraoperative flexion against gravity as an indication of ultimate range of motion in individual cases after total knee arthroplasty. J Arthroplast 13:500–503
Lüring C, Hüfner T, Perlick L, Bäthis H, Krettek C, Grifka J (2005) Soft tissue management in knees with varus deformity. Computer-assisted sequential medial ligament release. Orthopade 34:1118–1124
McDonald DA, Siegmeth R, Deakin AH, Kinninmonth AW, Scott NB (2012) An enhanced recovery programme for primary total knee arthroplasty in the United Kingdom-follow up at one year. Knee 19:525–529
McGrory JE, Trousdale RT, Pagnano MW, Nigbur M (2002) Preoperative hip to ankle radiographs in total knee arthroplasty. Clin Orthop Relat Res 404:196–202
Mihalko WM, Saleh KJ, Krackow KA, Whiteside LA (2009) Soft-tissue balancing during total knee arthroplasty in the varus knee. J Am Acad Orthop Surg 17:766–774
Moreland JR, Bassett LW, Hanker GJ (1987) Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am 69:745–749
Munzinger UK, Keblish PA, Boldt JG (2004) Operating technique. In: Knee Primary, Munzinger UK, Boldt JG, Keblish PA (eds) Primary knee arthroplasty. Springer, Berlin, pp 139–228
Olcott CW, Scott RD (2000) A comparison of 4 intraoperative methods to determine femoral component rotation during total knee arthroplasty. J Arthroplast 15:22–26
Picard F, Deakin AH, Clarke IV, Dillon JM, Kinninmonth AW (2007) A quantitative method of effective soft tissue management for varus knees in total knee replacement surgery using navigational techniques. Proc Inst Mech Eng H 221:763–772
Rauh MA, Boyle J, Mihalko WM, Phillips MJ, Bayers-Thering M, Krackow KA (2007) Reliability of measuring long-standing lower extremity radiographs. Orthopedics 30:299–303
RoBkopf J, Singh PK, Wolf P, Strauch M, Graichen H (2014) Influence of intentional femoral component flexion in navigated TKA on gap balance and sagittal anatomy. Knee Surg Sports Traumatol Arthrosc 22(3):687–693
Romero J, Duronio JF, Sohrabi A, Alexander N, MacWilliams BA, Jones LC, Hungerford DS (2002) Varus and valgus flexion laxity of total knee alignment methods in loaded cadaveric knees. Clin Orthop Relat Res 394:243–253
Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jocaby SM (2002) Insall Award Paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res 404:7–13
Siston RA, Giori NJ, Goodman SB, Delp SL (2006) Intraoperative passive kinematics of osteoarthritic knees before and after total knee arthroplasty. J Orthop Res 24:1607–1614
Venkatesan M, Mahadevan D, Ashford RU (2013) Computer-assisted navigation in knee arthroplasty: a critical appraisal. J Knee Surg 26(5):357–361
Whiteside LA (1999) Selective ligament release in total knee arthroplasty of the knee in valgus. Clin Orthop Relat Res 367:130–140
Yaffe MA, Koo SS, Stulberg DS (2008) Radiographic and navigation measurements of TKA limb alignment do not correlate. Clin Orthop Relat Res 466:2736–2744
Acknowledgments
We thank Guillaume Picard for his help in preparing and formatting the manuscript for publication. We thank Dr Angela Deakin for her help with paper and statistics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Authors declare that they do not have a direct conflict of interest in the authorship and publication of this contribution.
Funding
There is no funding source.
Ethical approval
The study was carried out as an audit under the clinical governance of our institution.
Informed consent
Informed consent was obtained from all participants included in the study.
Rights and permissions
About this article
Cite this article
Deep, K., Picard, F. & Baines, J. Dynamic knee behaviour: does the knee deformity change as it is flexed—an assessment and classification with computer navigation. Knee Surg Sports Traumatol Arthrosc 24, 3575–3583 (2016). https://doi.org/10.1007/s00167-016-4338-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4338-0