Abstract
Purpose
Medial release during total knee arthroplasty (TKA) is used to correct ligament imbalance in knees with varus deformity. However, questions remain on whether residual ligament imbalance would be related to inferior clinical results. The purposes of the present study were to measure the intraoperative joint gap and to evaluate the effect of intraoperative soft tissue condition on the new Knee Society Score (KSS 2011) at 2-year follow-up, without the maneuver of additional medial release to correct the asymmetrical gap balance.
Methods
Varus–valgus gap angle and joint gap were measured using a tensor device without medial release for 100 knees with preoperative varus deformity. The knees were categorized according to the varus–valgus gap angle and the laxity. The preoperative and postoperative clinical outcomes using KSS 2011 were compared between the groups.
Results
The average varus–valgus angles had a residual imbalance of 2.8° varus and 1.3° varus in extension and flexion, respectively. In comparison, according to varus–valgus joint gap angle and knee laxity in extension and flexion, no significant differences were found in postoperative range of motion and subscale of KSS 2011 among the groups.
Conclusion
Intraoperative asymmetrical joint gap and physiological laxity do not affect early clinical results after TKA.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Achieving proper soft tissue balance is one of the important factors for successful total knee arthroplasty (TKA) [18]. Generally, an additional procedure is used to correct imbalance of the medial and lateral joint gap in knee extension and flexion, which is believed to improve clinical outcomes and durability. Release of the medial structure has been performed frequently when the medial joint gap is tighter than the lateral joint gap in the knees with varus deformity. For mild varus knees, release of the deep medial collateral ligament (MCL) and posteromedial capsule is usually sufficient [4, 12, 33]. In the severe varus knee with increased lateral laxity, the superficial MCL is often released to acquire equal medial–lateral gap [11]. Various methods of medial release have been reported, in which functional ligament balancing including the release of the anterior and posterior oblique portions of MCL is necessary in up to 80% of patients with severe varus deformity in the mechanical alignment technique [3, 6, 35].
However, medial release has risks for causing medial instability. In previous cadaveric studies, extensive MCL release reduced tibial internal rotation during knee flexion [15]. In a fluoroscopic analysis, laxity of the MCL induced abnormal anterior motion of the femur in deep knee flexion [21]. On the contrary, lateral laxity does not seem to worsen clinical results, and a certain amount of lateral laxity may be necessary to have medial pivot motion as well as good range of motion to represent ligament balance in normal knees [14, 24, 28], although asymmetric lateral flexion instability can cause significant problems to the patient such as limited flexion and anterior knee pain [25]. Some studies evaluated soft tissue condition in osteoarthritic knees, and reported that soft tissue on the medial side did not have contracture, but lateral laxity increased in the varus knees [26, 31]. It seems unnecessary to extensively release ligaments on the not-contracted medial side to match the loose lateral side for varus knees. Concerning the coronal alignment, functional knee phenotypes in the female and male population are investigated, in which functional knee phenotypes enable a simple, but detailed assessment of a patient’s individual anatomy and thereby could be a helpful tool to individualize the approach to TKA [8]. Further, in a biomechanical study, no condylar lift-off was detected in a neutrally aligned TKA, even if the lateral laxity was excessive [13]. Therefore, lateral laxity can be left without medial release if the varus–valgus imbalance existed, aiming for the neutral alignment.
In the present study, clinical outcomes were evaluated without additional medial release for consecutive TKA with preoperative varus deformity, even if lateral laxity was observed during surgery. The purposes of the present study were to measure the varus–valgus gap angle and laxity in extension and flexion using a tensor device during consecutive TKA, and to evaluate whether good clinical outcomes using the new Knee Society Score (KSS 2011) were achieved at 2-year follow-up, without the maneuver of additional medial release to correct the asymmetrical gap balance. The first hypothesis was that the ligament balance during TKA is kept in varus extension and flexion without extensive medial release. The second hypothesis was that residual asymmetrical joint gap does not affect clinical outcomes including range of motion and subscale of KSS 2011 after TKA for the knee with preoperative varus deformity.
Methods
This study was conducted to evaluate our hypotheses using consecutive primary TKAs performed with a single implant design, in which prospectively collected data were retrospectively analyzed. All surgeries and gap measurements using a tensor device were executed, and clinical outcomes were evaluated at 2-year follow-up for 100 knees. Inclusion criteria were primary TKA for medial osteoarthritis of the knee using a ceramic tri-condylar posterior-stabilized implant (Bi-Surface 5: Kyocera, Kyoto, Japan) [20, 22, 23]. 17 patients presenting any valgus deformity were excluded from this analysis. Informed consent was obtained from all patients. The study design was approved by the institutional ethics review boards, and all procedures performed were in accordance with the ethical standards of the institutional research committee. A total of 15 male and 85 female knees with an average age of 75.7 years [standard deviation (SD) = 6.9 years] were included for surgery. The average preoperative hip–knee–ankle (HKA) angle, based on the angles between a mechanical axis of the femur and the tibia, was 11.5° varus (SD = 5.2°, range 0.6° to 24.5° varus). Ten knees had HKA smaller than 5°. The average preoperative femoral mechanical angle (FMA, the medial angle between the femoral mechanical axis and a tangent to the distal femoral condyles) and tibial mechanical angle (TMA, the medial angle between the tibial mechanical axis and a tangent to the proximal tibial joint surface) were 88.7° varus (SD = 2.5°) and 83.3° varus (SD = 2.7°), respectively. The delta values of HKA, FMA, and TMA between preoperative and postoperative alignment were calculated. The postoperative decrease of the varus deformity was denoted as positive. The average height and weight were 151.7 cm (SD = 6.9 cm) and 61.4 kg (SD = 11.0 kg), respectively, and the mean body mass index was 26.6 (SD = 3.9). Regarding statistical power, a post hoc power analysis was conducted because the data were retrospectively analyzed, in which the present study had 80% power to detect a parameter estimate of 0.3.
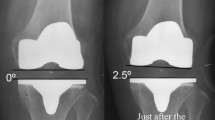
TKA was performed with mechanical alignment method in a uniform manner, and the goal of the coronal alignment was neutral alignment with the femoral and tibial components perpendicular to the respective mechanical axis. The medial parapatellar approach was used. The posterior cruciate ligament (PCL) was sacrificed, and the bone was cut using the following measured resection technique. The distal femur was cut perpendicular to its mechanical axis. Concerning the rotational alignment, the angle between the surgical epicondylar axis and the posterior condylar axis was measured preoperatively using a computed tomography. The cutting jig was set in accordance with the measured angle relative to the posterior condylar axis. The size of the femoral component was determined based on the antero-posterior length of the femur, which was independent of the flexion gap. Smaller size was chosen in between sizes. The tibia was cut perpendicular to the mechanical axis in the coronal plane. Approximately 10 mm of bone was resected from the most proximal part of the lateral tibial plateau. In the sagittal plane, the posterior slope was set to 5° relative to the tibial shaft. Rotational alignment of the tibial component was adjusted to the antero-posterior axis of the tibia (the Akagi line) [1]. Osteophytes on the medial side of the femur and tibia were removed. The patella was resurfaced for all knees.
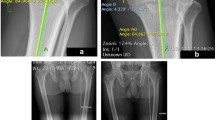
Regarding ligament balancing in extension, the deep layer of the MCL was released within 1 cm from the joint line for bone resection and osteophyte removal. No further extensive medial release was performed to acquire equal medio-lateral joint gap balance, even if lateral laxity was observed. The superficial layer of the MCL, semimembranosus, and posterior oblique ligament were not released. In flexion, gap imbalance was left uncorrected without additional ligament release or bony resection. After setting the femoral component trial, a tensor device was used to measure the joint gap at the center of the knee joint and the varus–valgus angle of the joint gap. The joint gap and the varus–valgus angle were measured applying a distraction force of 178 N with the knee in extension and 90° of flexion (Fig. 1). All components were fixed with Simplex bone cement (Stryker, Kalamazoo, MI, USA). The incision was closed with the knee in 100° of flexion.
The same postoperative rehabilitation programs were applied for all patients. Knee flexion exercises were continued in routine rehabilitation programs with physical therapists for one month. Following rehabilitation, patients were free to carry out deep flexion activities and were able to perform most activities without any restrictions, including deep knee flexion. Physical examination and knee scoring were conducted preoperatively and for 2 years postoperatively using the KSS 2011. Range of motion was passively measured with a long-arm goniometer in the supine position. In a previous study, intra-class correlation coefficient using a long-arm goniometer was 0.996 and 0.993 in inter-rater and intra-rater reliability, respectively, and the minimum significant difference was 10° [7]. Preoperative and postoperative examinations were performed by physical therapists that were independent from the surgeons performing the surgery.
To evaluate the effects of ligament imbalance, the knees were divided according to the intraoperative varus–valgus angle of the joint gap in knee extension and 90° of flexion independently. The balanced group consisted of knees with the varus–valgus angle of the joint gap being less than 3°. The varus imbalance group consisted of knees with the medio-lateral angle of the joint gap having 3°–6° of varus imbalance. The severe varus imbalance group consisted of knees with the varus–valgus angle of the joint gap being 6° and more. The valgus imbalance group consisted of knees with the medio-lateral angle of the joint gap having 3° and more of valgus imbalance, respectively.
To evaluate the effects of the joint laxity on clinical outcomes, the knees were divided according to the estimated laxity after implantation, which was calculated by subtracting the polyethylene thickness from the joint gap in extension and flexion. Grouping was performed with 2 mm gap increments, because previous clinical and biomechanical studies show that 2 mm increase in the joint gap has significant effect on clinical outcomes and knee kinematics and kinetics [9, 34]. In extension, the tight group consisted of knees with a laxity of − 2 mm and less. The moderate and loose group consisted of knees with the laxity of− 2 mm to 0 mm and more than 0 mm, respectively. In flexion, the tight group consisted of knees with the laxity of 0 mm and less. The moderate, loose, and over-loose group consisted of knees with the laxity of 0 mm to 2 mm, 2 mm to 4 mm, and more than 4 mm, respectively. To evaluate the accuracy of the measurement of the varus–valgus angle and the joint gap, measurement was conducted 5 times in extension and at 90° of flexion for six knees. The standard errors of the measurement of the varus–valgus angle were 0.1° and 0.2° in extension and flexion, respectively. Those of the joint gap were 0.2 mm and 0.1 mm.
All analyses were performed using JMP Pro software version 12.2.0 (SAS Institute Inc., Cary, NC). Clinical outcomes including preoperative and postoperative KSS 2011, range of motion, and alignment were compared between groups using either an ANOVA test or Wilcoxon signed rank test, whichever appropriate. Pearson correlation coefficients were calculated to determine the correlations. Post hoc analyses were conducted using the Tukey–Kramer method.
Results
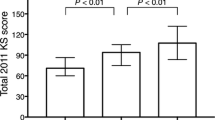
KSS 2011 scores except patient expectation were significantly improved postoperatively (Table 1). The average preoperative extension angle was significantly improved postoperatively, and preoperative flexion angle was maintained at 2 years after TKA. Regarding limb, femoral and tibial alignment, neutral alignment was achieved postoperatively. Preoperative alignment had no significant correlation with postoperative alignment in HKA (p = 0.166), FMA (p = 0.540), and TMA (p = 0.501) (Fig. 2).
The average residual varus–valgus imbalance was 2.8° (SD = 2.8°) varus in extension and 1.3° (SD = 4.0°) varus in flexion. The average varus–valgus angles were kept varus in extension and flexion, respectively (Fig. 3). The average extension gap was smaller than the flexion gap. The average extension and flexion gaps were 9.4 mm (SD = 2.5 mm) and 12.7 mm (SD = 2.8 mm), respectively. The average thickness of polyethylene insert was 10.0 mm (SD = 1.4 mm). The distribution of the laxity in flexion was more variable than in extension (Figs. 4, 5). Analyzing correlation with the alignment and the gap angle and joint laxity, the delta HKA angle had significant correlation with the joint gap angle, and the preoperative TMA and delta TMA had significant correlation with the laxity in extension (Table 2). Larger correction angle of limb alignment showed more varus joint gap in extension, and larger varus deformity and correction angle of the tibia showed more laxity in extension.
In comparison, according to the varus–valgus joint gap angle in extension, no valgus imbalance group was found, and no significant differences in patient demographics, preoperative and postoperative clinical outcomes were observed among the groups except BMI and preoperative HKA angle (Table 3). In comparison, according to the varus–valgus joint gap angle in flexion, there were no significant differences in patient demographics, preoperative and postoperative clinical outcomes among the groups (Table 4).
In comparison, according to the knee laxity in extension, there were no significant differences in clinical outcomes among the groups (Table 5). In comparison, according to the knee laxity in flexion, preoperative patient expectation had significant difference between moderate and loose groups and between moderate and over loose groups. However, no significant differences were observed in postoperative clinical outcomes (Table 6).
Discussion
The most important findings of the present study were that asymmetrical varus–valgus balance at full extension and 90° of flexion had no effect on postoperative range of motion and the subscales of the KSS 2011 and that relatively large varus imbalance did not worsen clinical symptoms at 2 years after TKA.
In the present study, the same surgical technique was applied for consecutive knees with preoperative varus deformity, and the measurement of the varus–valgus gap angle and joint gap was performed in a uniform manner. Medial release was limited to the deep layer of the MCL even if the varus–valgus imbalance was observed with the aim of neutral coronal alignment. The average varus–valgus imbalance was 2.8° varus in extension and 1.3° varus in flexion. In terms of functional knee phenotype, mechanical alignment target was obtained postoperatively in most of the patients, whereas the preoperative alignment was variable [8].
So far, it is still under discussion whether varus–valgus imbalance affects clinical outcomes. A previous study measuring the joint gap with a tensor device revealed achieving equalized rectangular gaps at extension and flexion did not influence 2-year postoperative clinical outcomes [14]. In several reports, however, asymmetrical gap balance affected negatively the University of California, Los Angeles activity level at 4 months, the postoperative knee flexion at 1 year, and Western Ontario and McMaster Universities Arthritis Index (WOMAC) score at 34 months, although these studies did not separately evaluate the knees with varus and valgus imbalance [10, 16, 32]. In the present study, the effect on clinical outcomes was analyzed at 2 years using KSS 2011 for consecutive knees with preoperative varus deformity. In extension, the groups with the residual varus and severe varus imbalance during TKA showed no significant differences in clinical outcomes including range of motion and KSS 2011 in comparison with the balanced group. However, the effect of valgus imbalance was unclear, because no knee showed postoperative valgus imbalance. In flexion, the groups with residual valgus, varus, and severe varus imbalance also showed no significant differences in comparison with the balanced group, although valgus imbalance was correlated with poor postoperative outcomes in several studies [24, 32]. The findings of the present study suggest that the asymmetrical gap seems to have no relation with early postoperative knee function and patient satisfaction. However, further research should be conducted to evaluate long term durability for the knees with asymmetrical varus–valgus balance, because 2-year follow-up is too short to comment on wear and aseptic loosening.
Several reasons can be suggested why residual lateral laxity had no effect on postoperative outcomes. First, larger lateral laxity has been reported in normal knees [28, 30]. One study showed that the mean angle was 4.9° in varus stress and 2.4° in valgus stress in extension and that the mean angle was 4.8° in varus stress and 1.7° in valgus stress in flexion. Therefore, larger lateral laxity, which is seen in normal knees, did not cause patient discomfort. Second, several clinical studies after TKA support our findings. Favorable outcomes were reported for the patients with lateral laxity after TKA, in which lateral laxity was positively correlated with postoperative knee flexion angle [24]. On the contrary, medial laxity had negative effects on postoperative pain and functions [3]. In the kinematic analysis after TKA, medial laxity induced abnormal knee kinematics, whereas lateral laxity had little effects on knee kinematics [21]. Finally, in a computer simulation study, no lift-off motion was observed with excessive lateral laxity alone in a neutrally aligned TKA [13]. In the present study, neutral alignment was almost achieved postoperatively with 1.4° varus of HKA angle on average, whereas the residual varus–valgus imbalance was 2.8° varus in extension and 1.3° varus in flexion. Therefore, varus–valgus imbalance and lateral laxity during surgery may be acceptable for the varus knees if the postoperative neutral alignment is achieved.
The joint gap during TKA has been known as one of important factors to influence postoperative range of motion. The intraoperative extension gap is correlated with the postoperative extension angle, in which tight component gap in extension causes postoperative flexion contracture [2, 27]. The intraoperative flexion gap is positively correlated with postoperative flexion angle [24, 29]. In the present study, the joint gap in extension and flexion was measured using a tensor device, and the comparison was made according to the laxity of the joint gap. Both joint gaps in extension and flexion were not correlated with the postoperative range of motion and KSS 2011. These results might be due to the limited range of joint gap during surgery within physiological lateral laxity or due to the limited number of each group.
Medial release is one of the essential steps toward the achievement of ligament balancing during TKA in patients with varus deformity. Several studies conduct extensive medial release up to complete detachment of MCL until the medial gap opens enough to balance the lateral gap. In these studies, the joint gap opening for knees with extensive medial release is similar, and knee kinematics and clinical outcomes are not altered in comparison with knees with minimal medial release [5, 17]. In the present study, 25 and 14 knees showed more than 6° of varus imbalance in extension and flexion, respectively. However, similar clinical outcomes were observed for knees with residual severe varus gap angle, although further studies are needed to evaluate the effect of residual ligament imbalance on long-term clinical outcomes and implant durability.
This study had several limitations. First, the number of patients in each group was relatively small, which can be underpowered to detect differences between groups, although the post hoc power analysis suggested adequate power. Moreover, only KSS scores were evaluated in the present study. Another patient reported outcome measure may be more responsive to these differences in knee balancing. Second, this study used a single posterior-stabilized implant design, and the results of this study might be specific to this specific TKA implant. Third, the measurements were made intraoperatively with a tensor with the trial components in place, and this might not reflect the final situation, since uneven cement mantle thickness and differences in intraoperative component positioning during cementation may affect the final gap. In addition, the gap angle and the joint gap were measured at full extension and 90° of flexion, but not in between. The condition at mid-flexion may affect clinical outcomes. Fourth, the number of the patients with extensive knee deformity of more than 20° was small. The results of the present study cannot be applied for the knees with severe varus deformity. Moreover, most of the knees included in the current study were of female patients, because consecutive TKA patients were recruited without any adjustment for sex. In previous clinical studies in Asian countries, female predominance among patients undergoing TKA is well documented [19, 20, 22]. Finally, the follow-up period was relatively short, and the effects of ligament imbalance during surgery were evaluated with clinical outcomes at 2 years after TKA. It was assumed that the ligament imbalance might cause functional disabilities and poor patient satisfaction in the short-term follow-up. Thus, the effects on clinical outcomes were analyzed for 2 years. However, ligament imbalance could have long-term effects on postoperative knee function, range of motion, patient satisfaction, and durability. Further studies are needed to evaluate the effect of residual ligament imbalance on the longevity of the implants.
Conclusions
Intraoperative asymmetrical joint gap and physiological laxity at full extension and 90° of flexion do not affect postoperative early clinical results after TKA, although mid-flexion stability is not evaluated, and the present study can be underpowered to detect differences due to the small number of each group. Medial release seems unnecessary for knees with preoperative varus deformity, and residual asymmetrical joint gap may be permitted during TKA.
Abbreviations
- TKA:
-
Total knee arthroplasty
- KSS:
-
Knee Society Score
- MCL:
-
Medial collateral ligament
- SD:
-
Standard deviation
- HKA:
-
Hip–knee–ankle
- FMA:
-
Femoral mechanical angle
- TMA:
-
Tibial mechanical angle
- WOMAC:
-
Western Ontario and McMaster Universities Arthritis Index
References
Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 420:213–219
Asano H, Muneta T, Sekiya I (2008) Soft tissue tension in extension in total knee arthroplasty affects postoperative knee extension and stability. Knee Surg Sports Traumatol Arthrosc 16:999–1003
Aunan E, Kibsgard TJ, Diep LM, Rohrl SM (2015) Intraoperative ligament laxity influences functional outcome 1 year after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23:1684–1692
Bottros J, Gad B, Krebs V, Barsoum WK (2006) Gap balancing in total knee arthroplasty. J Arthroplasty 21:11–15
Cho WS, Byun SE, Lee SJ, Yoon J (2015) Laxity after complete release of the medial collateral ligament in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23:1816–1823
Griffin FM, Insall JN, Scuderi GR (2000) Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty 15:970–973
Hancock GE, Hepworth T, Wembridge K (2018) Accuracy and reliability of knee goniometry methods. J Exp Orthop 5:46
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27:1394–1402
Ismailidis P, Kuster MS, Jost B, Giesinger K, Behrend H (2017) Clinical outcome of increased flexion gap after total knee arthroplasty. Can controlled gap imbalance improve knee flexion? Knee Surg Sports Traumatol Arthrosc 25:1705–1711
Jawhar A, Hutter K, Scharf HP (2016) Outcome in total knee arthroplasty with a medial-lateral balanced versus unbalanced gap. J Orthop Surg (Hong Kong) 24:298–301
Kim MW, Koh IJ, Kim JH, Jung JJ, In Y (2015) Efficacy and safety of a novel three-step medial release technique in varus total knee arthroplasty. J Arthroplasty 30:1542–1547
Koh HS, In Y (2013) Semimembranosus release as the second step of soft tissue balancing in varus total knee arthroplasty. J Arthroplasty 28:273–278
Kuriyama S, Ishikawa M, Nakamura S, Furu M, Ito H, Matsuda S (2016) No condylar lift-off occurs because of excessive lateral soft tissue laxity in neutrally aligned total knee arthroplasty: a computer simulation study. Knee Surg Sports Traumatol Arthrosc 24:2517–2524
Matsumoto T, Muratsu H, Kawakami Y, Takayama K, Ishida K, Matsushita T, Akisue T, Nishida K, Kuroda R, Kurosaka M (2014) Soft-tissue balancing in total knee arthroplasty: cruciate-retaining versus posterior-stabilised, and measured-resection versus gap technique. Int Orthop 38:531–537
Matsumoto T, Takayama K, Muratsu H, Matsushita T, Kuroda R, Kurosaka M (2015) Semimembranosus release reduces tibial internal rotation and flexion angle in cruciate-retaining total knee arthroplasty. J Arthroplasty 30:1537–1541
Meneghini RM, Ziemba-Davis MM, Lovro LR, Ireland PH, Damer BM (2016) Can Intraoperative sensors determine the "Target" ligament balance? Early outcomes in total knee arthroplasty. J Arthroplasty 31:2181–2187
Morcos MW, Lanting BA, Webster J, Howard JL, Bryant D, Teeter MG (2019) Effect of medial soft tissue releases during posterior-stabilized total knee arthroplasty on contact kinematics and patient-reported outcomes. J Arthroplasty 34:1110–1115
Moro-oka TA, Shiraishi H, Iwamoto Y, Banks SA (2010) Modified gap-balancing technique in total knee arthroplasty: evaluation of the post-operative coronal laxity. Knee Surg Sports Traumatol Arthrosc 18:375–380
Nakamura S, Ito H, Kobayashi M, Nakamura K, Toyoji U, Komistek RD, Nakamura T (2014) Are the long term results of a high-flex total knee replacement affected by the range of flexion? Int Orthop 38:761–766
Nakamura S, Ito H, Nakamura K, Kuriyama S, Furu M, Matsuda S (2017) Long-term durability of ceramic tri-condylar knee implants: a minimum 15-year follow-up. J Arthroplasty 32:1874–1879
Nakamura S, Ito H, Yoshitomi H, Kuriyama S, Komistek RD, Matsuda S (2015) Analysis of the flexion gap on in vivo knee kinematics using fluoroscopy. J Arthroplasty 30:1237–1242
Nakamura S, Kobayashi M, Ito H, Nakamura K, Ueo T, Nakamura T (2010) The Bi-Surface total knee arthroplasty: minimum 10-year follow-up study. Knee 17:274–278
Nakamura S, Sharma A, Ito H, Nakamura K, Zingde SM, Komistek RD (2015) Kinematic difference between various geometric centers and contact points for tri-condylar bi-surface knee system. J Arthroplasty 30:701–705
Nakano N, Matsumoto T, Muratsu H, Takayama K, Kuroda R, Kurosaka M (2016) Postoperative knee flexion angle is affected by lateral laxity in cruciate-retaining total knee arthroplasty. J Arthroplasty 31:401–405
Oh CS, Song EK, Seon JK, Ahn YS (2015) The effect of flexion balance on functional outcomes in cruciate-retaining total knee arthroplasty. Arch Orthop Trauma Surg 135:401–406
Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Iwamoto Y (2013) Lateral soft tissue laxity increases but medial laxity does not contract with varus deformity in total knee arthroplasty. Clin Orthop Relat Res 471:1334–1342
Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Mizu-Uchi H, Hamai S, Tashiro Y, Iwamoto Y (2014) Extension gap needs more than 1-mm laxity after implantation to avoid post-operative flexion contracture in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:3174–3180
Okazaki K, Miura H, Matsuda S, Takeuchi N, Mawatari T, Hashizume M, Iwamoto Y (2006) Asymmetry of mediolateral laxity of the normal knee. J Orthop Sci 11:264–266
Takayama K, Matsumoto T, Kubo S, Muratsu H, Ishida K, Matsushita T, Kurosaka M, Kuroda R (2012) Influence of intra-operative joint gaps on post-operative flexion angle in posterior cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:532–537
Tokuhara Y, Kadoya Y, Nakagawa S, Kobayashi A, Takaoka K (2004) The flexion gap in normal knees. An MRI study. J Bone Jt Surg Br 86:1133–1136
Tsubosaka M, Muratsu H, Takayama K, Miya H, Kuroda R, Matsumoto T (2018) Comparison of intraoperative soft tissue balance between cruciate-retaining and posterior-stabilized total knee arthroplasty performed by a newly developed medial preserving gap technique. J Arthroplasty 33:729–734
Tsukeoka T, Tsuneizumi Y, Yoshino K (2017) The rectangular flexion gap is associated with an increased knee flexion angle in a cruciate-sacrificing rotating platform mobile-bearing total knee arthroplasty. J Orthop Sci 22:313–317
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21:2325–2330
Watanabe M, Kuriyama S, Nakamura S, Nishitani K, Tanaka Y, Sekiguchi K, Ito H, Matsuda S (2019) Impact of intraoperative adjustment method for increased flexion gap on knee kinematics after posterior cruciate ligament-sacrificing total knee arthroplasty. Clin Biomech (Bristol, Avon) 63:85–94
Whiteside LA, Saeki K, Mihalko WM (2000) Functional medical ligament balancing in total knee arthroplasty. Clin Orthop Relat Res 380:45–57
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Funding
One or more authors (SN and SM) received research grant from Kyocera outside the submitted work.
Ethical approval
The study design was approved by the institutional ethics review boards, and all procedures performed were in accordance with the ethical standards of the institutional research committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tanaka, Y., Nakamura, S., Kuriyama, S. et al. Intraoperative physiological lateral laxity in extension and flexion for varus knees did not affect short-term clinical outcomes and patient satisfaction. Knee Surg Sports Traumatol Arthrosc 28, 3888–3898 (2020). https://doi.org/10.1007/s00167-020-05862-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-05862-4