Abstract
Most surgeons believe that varus deformity leads to progressive tightness of the medial soft tissue envelope and laxity on the lateral side. It is, however, unclear at what stage of the deformity such ligament alterations occur, and whether these are the consequence of intrinsic alterations in the ligaments themselves, or rather due to extrinsic factors such as osteophytes, adhesions to the underlying bone, or other factors which may cause a tightening effect. Thirty-five varus knees that were scheduled for TKA were investigated. Ligament status was evaluated after temporary correction of alignment and removal of osteophytes, using varus/valgus testing with computer navigation technology. Knees with <10° varus deformity were easily correctable to neutral after correction of the extrinsic factors that could cause medial tightness, and these knees maintained normal mediolateral laxity during varus/valgus stress testing. When coronal plane deformity exceeded 10°, progressive shortening of the medial collateral ligament was noted, as well as progressive stretching of the lateral structures (P < 0.001). This study, therefore, demonstrates that the medial collateral structures become intrinsically shortened when preoperative varus deformity exceeds 10°. Likewise, the lateral soft tissues become stretched. None of these occur when the preoperative deformity is <10°.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restoration of neutral limb alignment and establishing an adequate soft tissue balance are two important criteria for obtaining a successful total knee arthroplasty (TKA).
In knees with minimal deformity, this can usually be achieved relatively easy using modern TKA instrumentation and a standardized surgical technique.
Knees with limited preoperative deformation are likely to have an unaltered soft tissue envelope, and therefore do not require corrective soft tissue work in most of the cases.
The situation may however be different in cases where the preoperative deformity is more important, since the deformity itself may have induced an abnormality in the soft tissue envelope around the knee [2, 11, 15–17, 25].
In the varus knee for example, many surgeons believe that progressive shortening or contraction of the soft tissue structures on the medial side may occur, whereas the lateral structures may become stretched [10, 12, 16, 17, 26].
Performing a TKA in this situation may therefore require some type of mediolateral soft tissue balancing in order to provide a stable soft tissue envelope with symmetric laxity both on the medial and lateral side [6, 10, 12, 18, 26–28].
Although it is generally believed that the development of medial tightness and lateral laxity is correlated with the severity of the arthritic deformity, little or no data exist on the question at which degree of deformity such alterations start to occur, and whether these alterations are the consequence of intrinsic changes in the ligaments themselves, or rather due to factors extrinsic to the ligament quality, such as the formation of osteophytes, adhesions to the underlying bone, or other factors that may cause a tightening effect. Our hypothesis was that such correlation between varus deformity and mediolateral ligament status exists and starts to occur after a certain degree of deformity. The purpose of the study was to examine this hypothesis.
Materials and methods
Thirty-five consecutive patients with varus malalignment that were scheduled for TKA were included in our study. Only patients with degenerative osteoarthritis were considered. Patients were included in the protocol when preoperative full leg standing radiographs demonstrated a mechanical varus alignment.
After consenting the patient to the study, standard femoral and tibial fiducial navigation pins were inserted for the navigation system (Vectorvision®, Brainlab, Munich, Germany) and a standard midline incision and medial arthrotomy for performing a total knee replacement was performed.
All necessary landmarks for identification of the mechanical axes and generation of the individualized 3D model of the patient’s anatomy were collected and stored into the system.
Once the degree of mechanical malalignment had been registered, all medial osteophytes on the femoral condyle and intercondylar notch were removed.
Next, the deep medial collateral ligament was carefully liberated form the underlying osteophytes on the medial tibia, and these were subsequently removed from anterior to posterior, while leaving any remnants of the medial meniscus untouched. The deep portion of the medial collateral ligament was therefore released from the underlying tibial bone up to 5 mm distal at maximum and using sharp dissection.
Specific attention was paid to remove of all reachable osteophytes, especially these on the most posterior aspect of both the femur and tibia. Both cruciate ligaments were left untouched, but hypertrophic patches of synovial fibrosis were removed when encountered.
Next, a specially developed intercalary shim with 0.5 mm increments in thickness was interposed into the medial tibiofemoral compartment until neutral mechanical alignment was obtained on the navigation screen (Fig. 1).
Graphical demonstration of steps 1 and 2 in the study; (1) recording of preoperative varus deformity using computer navigation technology, (2) after osteophyte removal a specially developed intercalary shim with 0.5 mm increments in thickness was interposed into the medial tibiofemoral compartment until neutral mechanical alignment was obtained on the navigation screen
Once neutral alignment was obtained, maximal manual varus-valgus stress was applied with the knee in extension and the shim still in situ, and the maximal mechanical axis deviation was recorded both for varus- as well as valgus-stress (Fig. 2).
These measurements were performed after partial closure of the arthrotomy, and were rounded off towards 0.5°. Based upon data available from literature, 1°–3° laxity under valgus stress, and 2°–4° under varus stress were considered normal [1, 8, 19, 20, 23].
In knees with a flexion contracture, the measurements were performed at maximal extension.
Once the data were obtained, the knee was opened again and a standard TKA was performed.
In all cases, the procedure and measurements were performed by the same surgeon (JB), who has an operative experience longer than 10 years in TKA.
Results
The average varus deformity of the studied cases was 8.7° (range 2°–18°). After correction to neutral alignment an average of 0.6° (range 3°–4°) of maximal laxity on valgus stress was noted, whereas an average of 4.1° (range 2°–8°) of maximal laxity on varus stress was measured.
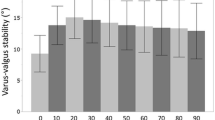
Figure 3 summarizes the measurements obtained under maximal varus and valgus stress as function of the preoperative deformity (positive indicates valgus, negative indicates varus).
For knees with a varus deformity of 10° or greater, a strong negative correlation was noted with maximal laxity on valgus stress (R 2 = 0.92, P < 0.001), and a strong positive correlation with maximal laxity on varus stress (R 2 = 0.80, P < 0.001).
No such correlation existed for knees with deformity smaller than 10° (R 2 < 0.01, P > 0.5).
Knees with preoperative varus deformity smaller than 10° had an average of 1.7° (range 1°–3°) laxity on maximal valgus stress, compared to −1.3° (range 1.5° to −4°) for knees with a varus deformity of 10° or greater (P < 0.001).
Knees with preoperative varus deformity of 10° or greater had an average of 5.8° (range 3.5°–8°) laxity on maximal varus stress calculated from the neutral mechanical alignment, compared to 3.1° (range 2°–7.5°) for knees with a varus deformity smaller than 10° (P < 0.001).
All knees with deformity smaller than 9° had laxity values on maximal varus and valgus stress that were in the normal range (1°–3° for valgus stress, 2°–4° for varus stress), whereas all of the knees with deformity more than 10° had greater than normal laxity on varus stress, and were on valgus stress tighter than normal in all of the cases studied.
Discussion
The most important finding of this study was that preoperative varus deformity is associated with changes in the collateral soft tissues as soon as the deformity reaches approximately 10°. Once such deformity is present, shortening of the medial collateral structures seems to occur, together with stretching on the lateral side. Knees with less severe deformity do not demonstrate such alterations in the surrounding soft tissue sleeve, and seem to have an unaltered soft tissue envelope comparable to the normal knee. Based upon our findings, it seems logical to conclude that intrinsic shortening of the medial soft tissues starts to occur when a varus deformity exceeds 10°, whereas no such alteration occurs in knees with less deformity.
Likewise, stretching of the lateral structures starts to occur at the same magnitude of deformity, approximately 10°. In knees with less varus deformity, no such stretching or elongation of the lateral structures could be noted based upon our measurements.
The findings from our study have some important implications.
First of all, our data suggest that ligament balancing should usually not be necessary in varus knees when the preoperative deformity is limited and smaller than 9° or 10°. These knees have a normal mediolateral soft tissue envelope without intrinsic shortening or stretching on either the medial or lateral side, and therefore should not require any soft tissue work in order to properly balance the joint during TKA. In such case a perfect soft tissue balance should indeed be achieved automatically, at least when the standard principles of matched resection are used, meaning that the surgeon aims at resecting the exact amount of bone that will be replaced by the implant (taken into consideration the eroded surface).
Second, our data also suggest that so-called ligament referenced TKA instrumentation systems can be safely used in varus knees as long as the deformity does not exceed 9° or 10°. Proponents of these systems, such as the LCS school, have traditionally determined the femoral component’s rotational position dependent to the proximal tibial cut (which is made first) and the collateral ligament tension [5, 7, 14, 30].
Several tensioning devices have been made available for this purpose, with or without the combination of an intra- or extramedullary femoral alignment system.
These ligament instrumentation systems are, however, primarily used with the knee in 90° of flexion, and since our data were recorded with the knee in extension only, it is unclear whether our findings are also valid with the knee in flexion.
This study also demonstrates however that in knees with greater deformity, the ligament status is no longer reliable for this purpose. Perfect restoration of correct soft tissue tension becomes therefore necessary in these cases in order to obtain a correct position of the femoral resection guide, and the surgeon should be aware of this. Practically speaking, this would usually indicate the necessity to perform a release of the tightened medial collateral structures until a balanced situation in equilibrium with the stretched lateral structures is achieved. Based upon our data, the surgeon can expect these measures to become proportional with the severity of the preoperative varus deformity.
Another finding from our study is that so-called soft tissue guided knee arthroplasty could be possible in knees with an arthritic varus deformity up to 9° or 10°. The concept of soft tissue guided knee arthroplasty derives from the philosophy that the periarticular soft tissues function as an envelope for the joint, where the periarticular soft tissues work together with the osteoarticular configuration in balanced harmony. Using the soft tissues to guide the knee implant position three dimensionally throughout the whole range of motion is therefore an appealing concept, but may be questionable in case of deforming osteoarthritis with subsequent alterations in the soft tissues. Our study, however, demonstrates that soft tissue integrity is maintained in most cases until the deformity exceeds 10°, and that soft tissue guidance therefore could be used for TKA cases with less deformity.
Despite the fact that the findings of our study on the influence of coronal plane deformity on mediolateral ligament status are interesting to TKA surgeons, these data are new and to our knowledge no comparable material currently exists in literature on this matter.
One of the reasons for this is the absence of adequate measurement methods to quantify mediolateral laxity intraoperatively. Recently however, the use of latest generation computer navigation technology has made such evaluation possible. Modern navigation systems have an accuracy of 0.19° for rotations and 0.35 mm for translations, and can be used to measure the mediolateral joint line opening during varus and valgus stress testing, or any other laxity test [1, 3, 4, 17, 23, 24].
Normative laxity data that were obtained using computer navigation technology in normally aged, nonarthritic knees have been published in the past [1, 23].
The study we report here has been performed using the same technology, and despite the fact that this method has been validated, our study set-up has a number of limitations.
Manual stress testing was performed to assess mediolateral laxity, and despite the fact that such was performed by an experienced surgeon, some degree of variability in the forces exerted during testing can not be excluded. Also, all measurements were performed with the knee in full extension (0° flexion), but such was not possible in all cases. Cases with flexion contracture were analyzed with the knee in maximal extension. These were all knees with greater than 10° of varus deformity, which could be explained by potentially contracted posteromedial structures, as previously reported by Whiteside et al. [27].
This study also did not determine exactly the relative influence of the different extrinsic and intrinsic factors that theoretically could influence the soft tissue status [9, 13, 21, 22, 26–29]. Well-known extrinsic factors contributing to soft tissue tightness are the presence of osteophytes and hypertrophic synovial fibrosis, and none of these were quantitatively analysed with respect to their influence on the soft tissue sleeve.
Further research is therefore necessary in order to determine the relative importance of all these contributing factors. In our study the extrinsic factors were corrected by surgically removing them, which allowed us to determine the remaining influence of intrinsic factors. For surgeons this is important, since intrinsic factors are surgically only correctable by some type of lengthening or release procedure.
Despite these two weaknesses, the results of this study are valid and useful to the surgeon when dealing with the varus knee.
Conclusion
When a varus deformity exceeds 10°, the surgeon should be aware that the medial collateral structures become intrinsically shortened and the lateral soft tissues stretched. In knees with less severe deformity, no such alterations occur in the surrounding soft tissue sleeve.
References
Bellemans J, D’Hooghe P, Vandenneucker H, Van Damme G, Victor J (2006) Soft tissue balance in total knee arthroplasty: does stress relaxation occur perioperatively? Clin Orthop Relat Res 452:49–52
Brage ME, Draganich LF, Pottenger LA, Curan JJ (1994) Knee laxity in symptomatic osteoarthritis. Clin Orthop Relat Res 304:184–189
Broers H, Hemken H, Luhman T, Ritschl P (2002) Photogrammetric calibration of a C-arm X-ray system as a verification tool for orthopaedic navigation systems. ISPRS J Photogram Remote Sens 56:338–346
Chassat F, Lavallée S (1998) Experimental protocol of accuracy evaluation of 6-D localizers for computer-integrated surgery: application to four optical localizers. In: Wells WM, Colchester A, Delp S (eds) Lecture notes in computer science, vol 1496. Berlin, Germany: Springer-Verlag, pp 277–284
Dennis DA (2008) Measured resection: an outdated technique in total knee arthroplasty. Orthopedics 31:943–944
Faris PM, Herbst SA, Ritter MA, Keating EM (1992) The effect of preoperative knee deformity on the initial results of cruciate-retaining total knee arthroplasty. J Arthroplasty 7:527–530
Fehring TK (2000) Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res 380:72–79
Heesterbeek PJ, Verdonschot N, Wymenga AB (2008) In vivo knee laxity in flexion and extension: a radiographic study in 30 older healthy subjects. Knee 15:45–49
Hildebrand KA, Zhang M, Germscheid NM, Wang C, Hart DA (2008) Cellular, matrix, and growth factor components of the joint capsule are modified early in the process of posttraumatic contracture formation in a rabbit model. Acta Orthop 79:116–125
Krackow K, Mihalko W (1999) The effect of medial release on flexion and extension gaps in cadaveric knees: implications for soft tissue balancing in total knee arthroplasty. Am J Knee Surg 12:222–228
Lewek MD, Rudolph KS, Snyder-Mackler L (2004) Control of frontal plane knee laxity during gait in patients with medial compartment knee osteoarthritis. Osteoarthr Cartil 12:745–751
Mihalko W, Miller C, Krackow K (2000) Total knee arthroplasty ligament balancing and gap kinematics with posterior cruciate ligament retention and sacrifice. Am J Orthop 29:610–616
Moriyama H, Yoshimura O, Kawamata S, Takemoto H, Saka Y, Tobimatsu Y (2007) Alteration of knee joint connective tissues during contracture formation in spastic rats after an experimentally induced spinal cord injury. Connect Tissue Res 48:180–187
Romero J, Duronio J, Sohrabi A, Alexander N, MacWilliams B, Jones L, Hungerford D (2002) Varus and valgus flexion laxity of total knee alignment methods in loaded cadaveric knees. Clin Orthop Relat Res 394:243–253
Rudolph KS, Schmitt LC, Lewek MD (2007) Age-related changes in strength, joint laxity, and walking parameters: are they related to knee osteoarthritis? Phys Ther 87:1422–1432
Sharma L, Lou C, Felson D, Dunlop D, Kirwan-Mellis G, Hayes KW, Weinrach D, Buchanan TS (1999) Laxity in healthy and osteoarthritic knees. Osteoarthr Rheum 42:861–870
Siston R, Goodman S, Delp S, Giori N (2007) Coronal plane stability before and after total knee arthroplasty. Clin Orthop Relat Res 463:43–49
Teeny S, Krackow K, Hungerford D, Jones M (1991) Primary total knee arthroplasty in patients with severe varus deformity. A comparative study. Clin Orthop Relat Res 273:19–31
Tokuhara Y, Kadoya Y, Nakagawa S, Kobayashi A, Takaoka K (2004) The flexion gap in normal knees. An MRI study. J Bone Joint Surg Br 86:1133–1136
Tokuhara Y, Kadoya Y, Kanekasu K, Kondo M, Kobayashi A, Takaoka K (2006) Evaluation of the flexion gap by axial radiography of the distal femur. J Bone Joint Surg Br 88:1327–1330
Trudel G, Jabi M, Uhthoff HK (1998) Intraarticular tissue proliferation after immobility: methods of assessment and preliminary results in rat knee joints. J Rheumatol 25:945–950
Trudel G, Seki M, Uhthoff HK (2000) Synovial adhesions are more important than pannus proliferation in the pathogenesis of knee joint contracture after immobilization: an experimental investigation in the rat. J Rheumatol 27:351–357
Van Damme G, Defoort K, Ducoulombier Y, Van Glabbeek F, Bellemans J, Victor J (2005) What should the surgeon aim for when performing computer-assisted total knee arthroplasty. J Bone Joint Surg 87A:52–58
Victor J, Hoste D (2004) Image-based computer-assisted total knee arthroplasty leads to lower variability in coronal alignment. Clin Orthop Relat Res 428:131–139
Wada M, Imura S, Baba H, Shimada S (1996) Knee laxity in patients with osteoarthritis and rheumatoid arthritis. Br J Rheumatol 35:560–563
Whiteside L (1995) Ligament release and bone grafting in total knee arthroplasty of the varus knee. Orthopedics 18:117–122
Whiteside L (2002) Soft tissue balancing: the knee. J Arthroplasty 17(Suppl 1):23–27
Whiteside L, Saeki K, Mihalko W (2000) Functional medial ligament balancing in total knee arthroplasty. Clin Orthop Relat Res 380:45–57
Witvrouw E, Danneels L, Thijs Y, Cambier D, Bellemans J (2009) Does soccer participation lead to genu varum? Knee Surg Sports Traumatol Arthrosc 17:422–427
Wyss T, Schuster A, Christen B, Wehrli U (2008) Tension controlled ligament balanced total knee arthroplasty: 5 year results of a soft tissue orientated surgical technique. Arch Orthop Trauma Surg 128:129–135
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bellemans, J., Vandenneucker, H., Vanlauwe, J. et al. The influence of coronal plane deformity on mediolateral ligament status: an observational study in varus knees. Knee Surg Sports Traumatol Arthrosc 18, 152–156 (2010). https://doi.org/10.1007/s00167-009-0903-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-009-0903-0