Abstract
Purpose
During total knee arthroplasty (TKA), an orthopaedic surgeon is focused on soft-tissue balance in extension (0°) and in flexion (90°). Patients with instability problems of the knee often report a feeling of instability during daily life activities, at around 30° knee flexion. There are no reference values available for knee laxity of healthy subjects in mid-flexion (30°) and flexion (90°) for comparison with the TKA population. Therefore, the aim was to quantify varus and valgus knee laxity in extension, mid-flexion and flexion in the asymptomatic native knee.
Methods
In 40 healthy volunteers matched for age, gender and BMI with the TKA-population, varus and valgus knee laxity in extension (0°), mid-flexion (30°) and flexion (90°) was measured on low-dose radiographs. For each subject, one randomly selected knee was stressed in extension, mid-flexion and flexion (with 15 Nm) using a stress device.
Results
Varus laxity in mid-flexion was higher than in extension and flexion (p < 0.01). Valgus laxity tended to be highest in mid-flexion laxity; however, no differences in knee laxity between flexion angles were seen (n.s.). Varus knee laxity in extension was higher in females than in males (p < 0.05).
Conclusions
Mid-flexion laxity in the native knee is more prominent on the lateral side of the knee, while the medial side is more stable and constrained. Varus knee laxity in extension was shown to be higher in females than in males.
Level of evidence
Prognostic Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During total knee arthroplasty (TKA) surgery, important knee joint stabilizers, such as the menisci and, in posterior stabilized (PS) TKA, the cruciate ligaments, are removed [1]. The collateral ligaments remain intact and are recognised to be the primary passive knee stabilisers in the coronal plane [2, 3]. In order to restore the stability of the replaced knee, it is important to know how tight or loose a knee should be implanted to achieve optimal tension of the collateral ligaments [4].
Intra-operatively, knee laxity is difficult to quantify; the orthopaedic surgeon is mainly focused on soft-tissue balance in extension (0°) and in flexion (90°), to achieve proper kinematics and stability [1, 4]. In that case, knee laxity in the mid-flexion range (15°–60°) is frequently not taken into account [1]. Moreover, the anatomy of the lateral and medial knee compartments differ; therefore, it makes sense to determine varus and valgus laxity separately [2].
Mid-flexion laxity is experienced by patients as impairment in performing daily life activities when the knee is regularly loaded in mid-flexion (around 30°) [5]. Therefore, mid-flexion stability is considered of major importance for a good functional outcome after TKA [1, 6].
To date, there are no in vivo reference values of knee laxity in mid-flexion (30°) and flexion (90°) available for equally aged asymptomatic knees to compare with those of the TKA population (Table 1). Previously, cadaveric studies measuring mid-flexion laxity on the lateral and medial sides of the knee [1, 7, 8] and a study measuring knee laxity in healthy older volunteers [9] have been published. Additionally, varus-valgus knee laxity is related to functional ability [10]. Reference values of clinical and functional performance in asymptomatic knees have not been published before.
The goal was to explore and describe the reference values for varus and valgus knee laxity in mid-flexion, flexion and extension, in healthy older subjects. In addition, reference values for clinical performance and knee function will be retrieved. Providing reference values helps to improve understanding of the envelope of laxity in the native knee and will subsequently help orthopaedic surgeons in clinical practice to restore stability in the osteoarthritic knee.
Materials and methods
This cross-sectional study was performed at the Sint Maartenskliniek Nijmegen, The Netherlands. 40 subjects [average age 62.7 (SD 5.8) years, 13 males, 27 females] were recruited through social media advertisement and an advertisement in the waiting room of our orthopaedic clinic. All 40 subjects completed the study protocol. Subjects aged 50–75 with no (diagnosed) osteo- or rheumatoid arthritis, no history of knee (ligament) injury or knee complaints and able to walk for at least one hour were included. Considering the heterogeneity of the TKA population, two or three clusters (Table 2) per relevant characteristic were created [age, gender and body mass index (BMI)], based on the characteristics of the patients who underwent a primary TKA in 2014 in our hospital. Clusters were created to reflect the heterogeneity of the population and not to measure differences between subjects within the different clusters. Recruitment continued until the number of subjects for every cluster in Table 2 was reached. Subjects with a hip arthrodesis or hip prosthesis, BMI > 35, knee flexion < 90°, treatment for osteoporosis, visually observable varus or valgus leg alignment were not recruited. For each subject, one randomly selected knee was included in the study (20 left and 20 right knees). A computer-generated randomization list was used to select an equal number of left and right knees.
Measurements
Varus and valgus knee laxity
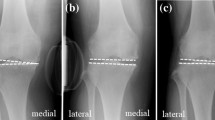
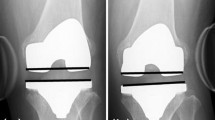
Varus and valgus laxity of the knee in extension (0°), mid-flexion (30°) and flexion (90°) was assessed on radiographs with the use of a custom-made stress device to stress the knee (Fig. 1). Knee laxity was defined as the joint opening under standardized applied moment. The assessments were similar to the method published by Heesterbeek et al. [9]. During the stress radiographs, the subject was in a supine position on a table with the lower leg on a platform with the knee consecutively extended (but unlocked), flexed in 30° and flexed in 90°, with the leg muscles relaxed. The foot was placed in an ankle–foot orthosis. To minimize femur movement when applying torques to the knee, the upper leg was strapped on a thigh support on the medial and lateral sides just proximal to the femoral epicondyles. With the use of 50 N on a pulley 0.30 m distally from the joint line, an external moment of 15 Nm was applied at the knee joint laterally and medially, resulting in varus and valgus stress, respectively. An external moment of 15 Nm was gradually applied to the knee in a standardized way, so that the subject could have continuously relaxed muscles. Under stress, low-dose radiographs (Multidiagnost Eleva, Philips, Best, The Netherlands) were obtained in the anteroposterior view. For each subject, nine low-dose radiographs were made with varus, valgus and no stress (neutral situation) applied, under fluoroscopic guidance with the roentgen ray direction parallel to the tibia joint surface, centred on the middle of the femorotibial joint space.
Varus and valgus knee laxity calculation
The angle between a tangent line on the femur condyles and a line through the deepest tibial joint surfaces was measured on the varus stress, valgus stress and neutral radiographs (Fig. 2). The measurement tool within the radiographic database program (Volume Vision within IntelliSpace PACS Enterprise version 4.4, Philips, Foster City, United States) was used, and measurements were made to the nearest 0.1°. Varus laxity was defined as the difference between the varus stress situation and the neutral situation and valgus laxity, as the difference between the valgus stress situation and the neutral situation [9]. The measurements were performed by a single person (MtM). Duplicates of 25% of the measurements were performed by a second rater (PH), to calculate inter-rater reproducibility. Intra-rater reproducibility was measured with an interval of 4 weeks. Four difficult measurements caused by low-quality radiographs were discussed and scored by consensus of the two raters. For two subjects, the radiographs in 90° flexion were considered to be of insufficient quality, making measurements impossible. These measurements were withdrawn from the data set. Inter- and intra-rater comparisons showed adequate reproducibility for measuring varus and valgus laxity in extension, mid-flexion and flexion in healthy subjects (95% prediction limits (Bland and Altman)) (Table 3). The repeatability of varus-valgus laxity measurements was investigated earlier by Heesterbeek et al. [9] and showed values ranging between 0.6° and 0.9°.
Clinical performance and knee function
Clinical performance and knee function were measured to adequately describe the study population and to obtain reference values for these parameters. Knee function was scored with the Knee Society Scoring System (KSS), including subscales for clinical score (100 points) and function score (100 points), where a higher score indicates a better outcome [23]. Passive range of motion of the knee, part of the KSS, was measured with a long-arm goniometer by the researcher. The Tegner activity score was used to grade activity based on work and sports activities on an activity level scale of 0–10, with level 10 indicating competitive sports (national elite) [24]. Finally, anterior and posterior translation of the tibia in 20°, 30° and 90° was measured using the rolimeter (aircast Europa GmbH Neubeuern, Germany).
The Leg Extensor Power (LEP) rig (Queens Medical Centre, Nottingham, United Kingdom) was used to objectively assess knee power output and, indirectly, knee function, with high validity [25]. The LEP rig consists of a seat and footplate connected through a lever and chain to a flywheel. When the leg is extended, the footplate is pushed away from the body, thereby accelerating the flywheel and producing power. Subjects were encouraged to push their flexed leg from the starting position into full extension with maximal effort. This procedure was repeated five times for the study knee.
IRB approval
The hospital’s institutional review board and the Medical Ethical Review Board of Slotervaart and Reade (NL55385.048.15) approved the study protocol. All participants gave written informed consent.
Statistical analysis
No sample size was calculated because of the explorative nature of the study. Subject characteristics were summarized using descriptive statistics. Further, the Shapiro–Wilk test was used to test for a normal distribution. Stratified analyses were performed for males and females. Differences in varus and valgus laxity in extension, mid-flexion and flexion were assessed using ANOVA. The association between gender, age and BMI and varus-valgus laxity was investigated with a regression analysis. Pearson’s correlation coefficients (two-tailed) were calculated between varus and valgus laxity for extension, mid-flexion and flexion. Results were presented as mean (SD) with range and 95% CI. Clinical and functional variables were presented with median and ranges. Pearson’s correlation coefficients (parametric) and/or Spearman’s rho (non-parametric) were calculated between function scores and varus and valgus laxity, when appropriate. Student’s t test and the non-parametric Mann–Whitney U test were used to compare function scores between males and females. Data were analysed using STATA 13.0 (StataCorp, College Station, Texas). A p value of < 0.05 was considered statistically significant.
Results
Varus and valgus laxity data in extension, mid-flexion and flexion were all normally distributed, except for varus laxity in extension. Total varus and total valgus laxity were not normally distributed.
Varus and valgus knee laxity at various flexion angles
Varus laxity in mid-flexion was significantly higher than in extension and flexion (p < 0.001) (Table 3). Valgus laxity tended to be highest in mid-flexion; however, this was not statistically significant between flexion angles (n.s.).
Gender differences in varus and valgus knee laxity
When varus and valgus laxity were stratified by gender, we saw that mid-flexion varus laxity was significantly higher than in extension and flexion in both males and females (p < 0.002 and p < 0.001, respectively) (Fig. 3; Table 4). Valgus laxity was not significantly different between flexion angles in males and females (n.s.) (Fig. 4).
Box plots of varus knee laxity in extension, mid-flexion and flexion, stratified by gender (blue = male; red = female). Horizontal lines represent the median, the length of the box the 25th–75th percentile, the whiskers the 0–25th and 75–100th percentiles, dots represent the outliers. *Varus laxity in extension statistically significantly higher in females than in males (p < 0.05). **Varus laxity in mid-flexion statistically significantly higher than in extension (p < 0.01). ***Varus laxity in mid-flexion statistically significantly higher than in flexion (p < 0.01)
Pearson’s correlation coefficient (R) between varus and valgus laxity was − 0.19 in extension, − 0.10 in mid-flexion and 0.37 in flexion, indicating a low degree of correlation.
There was no statistical association between age, left or right knee or BMI and varus or valgus knee laxity in extension, mid-flexion and flexion, in males or females.
Clinical performance and knee function
Clinical performance and knee function scores were not correlated with varus-valgus knee laxity. Maximum power output was higher, and time to maximum power output was lower in males than in females (Table 5).
Discussion
The most important finding of the study was that mid-flexion laxity in the asymptomatic native knee was more prominent on the lateral side of the knee, whereas the medial side was more stable and constrained. Furthermore, varus knee laxity in extension was shown to differ between males and females. This is the first in vivo study reporting on mid-flexion laxity in the asymptomatic native knee.
The differences between findings for the medial and lateral sides can be explained by the characteristics of the medial and lateral collateral ligament complex [2]. The lateral side of the knee shows greater mobility because the axis of rotation is based in the medial compartment [2]. In contrast, the medial side of the knee is the more stable one [2].
Varus knee laxity in extension was one degree higher in females than in males. Although this value was close to the limit of reproducibility, significant differences in knee laxity of the collateral ligaments between males and females have also been reported previously: these studies showed that females had more varus and valgus knee laxity than males [14,15,16]. Gender differences were also seen in functional outcomes, although clinical performance and knee function scores were not associated with the level of varus-valgus knee laxity in this study.
Our in vivo results approximate the in vivo knee laxities in extension and 70° flexion found in a previous study by Heesterbeek et al. [9] and by other authors [1, 7,8,9, 11,12,13, 17, 18, 20,21,22, 26, 27] (Table 1). Exact comparison of the results with findings from previous studies is complicated by heterogeneity in the methods used to stress the knee, the amount of load applied, the unit of measurement (e.g. millimetres vs degrees), differences between study populations (e.g. in vivo vs in vitro, young vs older subjects, cultural and anatomical differences) and differences in presentation of results (combined results vs varus and valgus laxity separately). While almost all studies also found a more stable medial side of the knee (Table 1), the majority of studies reported increases in laxities with increasing flexion angles (0°, 30° and 90°) [7, 8, 28] and observed higher laxities than the present results in extension, as well as in mid-flexion and flexion [1, 3, 7]. These differences in laxity are likely attributable to differences between the in vivo and in vitro knees [8, 18].
Due to technical improvements in the previously used custom-made stress device, it was possible to measure in vivo varus-valgus knee laxity in up to 90° flexion with low-dose radiographs. Although it was not always feasible to measure this parameter in exactly 90° flexion, even with the aforementioned technical improvements, the knees were substantially more flexed than the 70° reported by Heesterbeek et al. [9]. Unlike others, the present study found slightly more laxity in mid-flexion than in 90° flexion. Possibly, this was due to hip rotation during measurement in 90° flexion. Although the upper leg was strapped tightly on a thigh support, rotation was allowed when the knee was flexed at 90°. Incomplete hip rotation and subsequent unintentional muscular tensioning may have led to an underestimation of the actual laxity in 90° flexion. This is a known limitation of in vivo models [3], and it was attempted to prevent this by gradually increasing the load.
The present study has some additional limitations: the use of low-dose radiographs instead of normal radiographs resulted not only in a lower radiation dose for the subject but also in lower quality stress radiographs. Fortunately, the inter-rater analyses still showed adequate reproducibility for measuring varus-valgus knee laxity on low-dose radiographs. Furthermore, the sample size was a compromise between feasibility and ethical considerations. However, the sample size was large enough to explore varus and valgus knee laxity in asymptomatic native knees of a representative cohort.
How these findings could be translated to TKA remains an open question. Mid-flexion laxity on the medial side of the knee appears as an important issue: Aunan et al. found that functional outcome 1 year after TKA was negatively affected by increasing valgus laxity in extension and flexion [29]. Other studies also found the same negative correlation between valgus laxity and reduced postoperative knee function [8, 30, 31]. Laxity in 0° and 90° flexion can be influenced by a number of factors such as varus, valgus and rotational changes of the implants [19]. Also, joint line elevation causes mid-flexion laxity by shifting the centre of rotation of the medial condyle and subsequently changing the function of the medial collateral ligament [1, 18, 28, 32]. In addition, reduction of posterior condylar offset can also cause mid-flexion laxity [33]. In summary, knowing the envelope of laxity in the asymptomatic native knee can contribute to an optimal restoration of stability during TKA. However, it is still unresolved how varus laxity in 30° flexion can be controlled precisely during surgery. Perhaps new techniques such as robotic-assisted gap-balancing with sophisticated software that can predict knee laxity before femoral resections are performed have a place here [19].
Conclusion
Mid-flexion laxity in the asymptomatic native knee seems more prominent on the lateral side of the knee, while the medial side is more stable and constrained. Varus knee laxity in extension was higher in females than in males. These reference values for varus and valgus laxity in the native knee for the full range of motion provide an overview for orthopaedic surgeons that will help them to better understand the envelope of laxity.
References
Victor J, Luyckx T (2018) Mid flexion instability. In: Scott WN (ed) Insall & Scott Surgery of the Knee, 6th edn. Elsevier, Philadelphia, pp 1740–1749
Hirschmann MT, Müller W (2015) Complex function of the knee joint: the current understanding of the knee. Knee Surg Sports Traumatol Arthrosc 23:2780–2788
Markolf KL, Mensch JS, Amstutz HC (1976) Stiffness and laxity of the knee—the contributions of the supporting structures. J Bone Jt Surg Am 58-A:583–594
Heesterbeek PJC, Jacobs WCH, Wymenga AB (2009) Effects of the balanced gap technique on femoral component rotation in TKA. Clin Orthop Relat Res 467:1015–1022
Hicks-Little CA, Peindl RD, Hubbard TJ, Scannell BP, Springer BD, Odum SM, Fehring TK, Cordova ML (2011) Lower extremity joint kinematics during stair climbing in knee osteoarthritis. Med Sci Sports Exerc 43:516–524
Ghosh KM, Blain AP, Longstaff L, Rushton S, Amis AA, Deehan DJ (2014) Can we define envelope of laxity during navigated knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 22:1736–1743
Van Damme G, Defoort K, Ducoulombier Y, Van Glabbeek F, Bellemans J, Victor J (2005) What should the surgeon aim for when performing computer- assisted total knee arthroplasty? J Bone Jt Surg Am 87-A:52–58
Roth JD, Howell SM, Hull ML (2015) Native knee laxities at 0°, 45, and 90° of flexion and their relationship to the goal of the gap-balancing alignment method of total knee arthroplasty. J Bone Jt Surg Am 97:1678–1684
Heesterbeek PJC, Verdonschot N, Wymenga AB (2008) In vivo knee laxity in flexion and extension: A radiographic study in 30 older healthy subjects. Knee 15:45–49
Van Der Esch M, Steultjens M, Knol DL, Dinant H, Dekker J (2006) Joint laxity and the relationship between muscle strength and functional ability in patients with osteoarthritis of the knee. Arthritis Care Res 55:953–959
Lewek MD, Rudolph KS, Snyder-Mackler LS (2004) Control of frontal plane knee laxity during gait in patients with medial compartment knee osteoarthritis. Osteoarthr Cartil 12:745–751
Okazaki K, Miura H, Matsuda S, Takeuchi N, Mawatari T, Hashizume M, Iwamoto Y (2006) Asymmetry of mediolateral laxity of the normal knee. J Orthop Sci 11:264–266
Tokuhara Y, Kadoya Y, Nakagawa S, Kobayashi A, Takaoka K (2004) The flexion gap in normal knees. J Bone Jt Surg 86:1133–1136
Shultz SJ, Shimokochi Y, Nguyen A, Schmitz RJ, Bruce D, Perrin DH (2007) Measurement of varus-valgus and internal-external rotational knee laxities in vivo—Part II: relationship with anterior-posterior and general joint laxity in males and females. J Orthop Res 25:989–996
Sharma L, Lou C, Felson DT, Dunlop DD, Kirwan-Mellis G, Hayes KW, Weinrach D, Buchanan TS (1999) Laxity in healthy and osteoarthritic knees. Arthritis Rheum 42:861–870
Deep K (2014) Collateral ligament laxity in knees: what is normal? Clin Orthop Relat Res 472:3426–3431
Hunt NC, Ghosh KM, Blain AP, Rushton SP, Longstaff LM, Deehan DJ (2015) No statistically significant kinematic difference found between a cruciate-retaining and posterior-stabilised Triathlon knee arthroplasty: a laboratory study involving eight cadavers examining soft-tissue laxity. Bone Joint J 97-B:642–648
Luyckx T, Vandenneucker H, Scheys L, Vereecke E, Victor A, Victor J (2018) Raising the joint line in TKA is associated with mid-flexion laxity: a study in cadaver knees. Clin Orthop Relat Res 476:601–611
Shalhoub S, Moschetti WE, Dabuzhsky L, Jevsevar DS, Keggi JM, Plaskos C (2018) Laxity profiles in the native and replaced knee-application to robotic-assisted gap-balancing total knee arthroplasty. J Arthroplasty 33:3043–3048
Delport H, Labey L, De Corte R, Innocenti B, Vander J, Bellemans J (2013) Collateral ligament strains during knee joint laxity evaluation before and after TKA. J Clin Biomech 28:777–782
Manning WA, Ghosh K, Blain A, Longstaff L, Deehan DJ (2017) Tibiofemoral forces for the native and post-arthroplasty knee: relationship to maximal laxity through a functional arc of motion. Knee Surg Sports Traumatol Arthrosc 25:1669–1677
Hall RK, Ewing JA, Beal MD, Manning DW, Siston RA (2018) Medially-stabilized total knee arthroplasty does not alter knee laxity and balance in cadaveric knees. J Orthop Res. https://doi.org/10.1002/jor.24181
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR (2009) The reliability, validity, and responsiveness of the lysholm score and tegner activity scale for anterior cruciate ligament injuries of the knee. Am J Sports Med 37:890–897
Bassey EJ, Fiatarone MA, O’Neill EF, Kelly M, Evans WJ, Lipsitz LA (1992) Leg extensor power and functional performance in very old men and women. Clin Sci (London Engl 1979) 82:321–327
Halewood C, Traynor A, Bellemans J, Victor J, Amis AA (2015) Anteroposterior laxity after bicruciate-retaining total knee arthroplasty is closer to the native knee than ACL-resecting TKA: a biomechanical cadaver study. J Arthroplasty 30:2315–2319
Stoddard JE, Deehan DJ, Bull AMJ, McCaskie AW, Amis AA (2013) The kinematics and stability of single-radius versus multi-radius femoral components related to mid-range instability after TKA. J Orthop Res 31:53–58
Martin JW, Whiteside LA (1990) The influence of joint line position on knee stability after condylar knee arthroplasty. Clin Orthop Relat Res 259:146–156
Aunan E, Kibsgård TJ, Diep LM, Röhrl SM (2015) Intraoperative ligament laxity influences functional outcome 1 year after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23:1684–1692
Seah RB, Yeo SJ, Chin PL, Yew AKS, Chong HC, Lo NN (2014) Evaluation of medial-lateral stability and functional outcome following total knee arthroplasty: results of a single hospital joint registry. J Arthroplasty 29:2276–2279
Tsukiyama H, Kuriyama S, Kobayashi M, Nakamura S, Furu M, Ito H, Matsuda S (2017) Medial rather than lateral knee instability correlates with inferior patient satisfaction and knee function after total knee arthroplasty. Knee 24:1478–1484
Cross MB, Nam D, Plaskos C, Sherman SL, Lyman S, Pearle AD, Mayman DJ (2012) Recutting the distal femur to increase maximal knee extension during TKA causes coronal plane laxity in mid-flexion. Knee 19:875–879
Matziolis G, Brodt S, Windisch C, Roehner E (2017) Changes of posterior condylar offset results in midflexion instability in single-radius total knee arthroplasty. Knee Arthroplast 137:713–717
Acknowledgements
The authors wish to thank the radiology department of the Sint Maartenskliniek for taking the stress radiographs and Albert van Houten, for his comments.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors created the concept and design of the study. MtM managed the acquisition of data. MtM and PH analysed the data and wrote the draft of the full manuscript. All authors critically revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The hospital’s investigational review board and the Medical Ethical Review Board of Slotervaart and Reade (NL55385.048.15) approved the study protocol.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
te Molder, M.E.M., Wymenga, A.B. & Heesterbeek, P.J.C. Mid-flexion laxity in the asymptomatic native knee is predominantly present on the lateral side. Knee Surg Sports Traumatol Arthrosc 27, 3614–3625 (2019). https://doi.org/10.1007/s00167-019-05474-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05474-7