Abstract
Composite restorations have shown excellent survival rates on anterior and posterior teeth, with secondary caries, tooth/restoration fracture and aesthetic demand being the main reasons for failures. Due to materials improvements overtime, current materials’ properties have revelated a minor influence on the survival of composites in clinical studies. When hybrid or nanohybrid composites are used, low AFR could be expected. Thus, patient-related factors and operators are fundamental to be considered on restoration longevity. Invasive behavior toward restoration replacement results in a decrease in the survival of restoration . Restorations should be carried out in a health promotion environment, emphasizing preventive practices. The adoption of healthy behaviors by patients will consequently led to “healthy” restorations, increasing the longevity of treatments. The adoption of minimally invasive dentistry for the management of deteriorated restorations, such as refurbishment or repair restorations, should be considered in routine practice. In this way, dentists should react less in front of small defects of restorations, indicating replacements only when other alternatives are not plausible.
This chapter explains long-term survival and reasons for the failure of composite restorations, including all correlated factors.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Composite resin restorations have been the first choice by clinicians and patients for direct anterior [1] and posterior restorations [2] mainly due to optical characteristics, high longevity, adhesive properties, and preservation of sound tooth structure [3, 4]. Resin composite restorations have presented a lower annual failure rate (AFR) ranging from 1 to 3% in posterior teeth and 1–5% in anterior teeth [5]. Recent publications have shown that this material can be used to rehabilitate severely worn teeth with acceptable clinical success, with AFR ranging from 0.4% for microhybrid composites to 26.3% for microfilled materials [6]. Similarly, a network meta-analysis found an AFR of 2.2% for use in large posterior restorations [7].
The main reasons for failure in posterior restorations, both in adults [8] and children [9], are fractures and secondary caries. It has been discussed that material properties had a minor effect on longevity. At the same time, clinical-related factors (such as the position of the tooth in the tooth arc and dental type), the operator (age, country of qualification, and employment status), patient (caries risk, bruxing habits, parafunction, esthetic demand), and socioeconomic status might play essential roles in the longevity of composites [10]. Tooth structure or composite fractures are important factors for restorations failure, while esthetic demands could account for restoration replacement in anterior teeth [11].
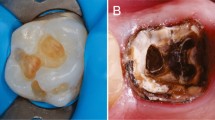
To improve dental restorations’ longevity and under a minimally invasive dentistry philosophy, repair has been proposed as an interesting strategy over the replacement, avoiding the repetitive restorative cycle [12]. Removal of the sound dental structure occurs when the complete restoration is replaced. When the restoration needing replacement is near the vital pulp tissue, the risk of pulp exposure is elevated and can result in unnecessary endodontic treatments [13, 14]. Therefore, resin restorations can be repaired when a considerable part of restoration presents good condition to be maintained. Repair of defective restorations has exhibited good clinical performance, increasing dental restorations’ longevity (Fig. 10.1) [10, 15] and displaying better cost-effectiveness than replacement [16]. In this chapter, we will discuss the longevity of esthetic composite restorations, the reasons for failure, and exploring the repair of defective restorations as a treatment option to the replacement.
Clinical phenotypes of resin composite restorations in posterior teeth after at least two decades of clinical service. In (a) and (b), the restorations show typical signs of aging including loss of anatomical form, surface and marginal staining, color instability, and wear. In (c), restorations were repaired and still presented good clinical performance after several years in the mouth. In (d), restorations were repaired and subjected to polishing, which removed the extrinsic staining and improved appearance. (Photography courtesy of Dr. Paullo Rodolpho)
10.1 Expectation vs. Reality
Resin composites have undergone constant development, becoming the most used direct restorative material [2], mainly because of their esthetic properties, preservation of tooth structure, and the high success rates [3, 17]. Considering the results from clinical studies about the longevity of composite restorations, clinicians frequently expect a longevity of more than 20 years for their restorations. However, despite the excellent results showed in the literature, dentists should be aware that different aspects involving themselves, the tooth/cavity, and the patient can interfere with the durability of a restorations. The understanding of these factors can help professionals to predict better the probability of failure of a given restoration.
A vast number of systematic reviews have been published in recent literature presenting the AFR/success rate (SR) of resin composites [10, 11, 18,19,20,21,22,23,24,25,26,27,28] (Table 10.1). In general, the systematic reviews have presented similar results: AFR ranging from 1 to 3% in posterior teeth and from 1 to 5% in anterior teeth [5]. The AFR increases when endodontic treated teeth are investigated: ranging from 2 to 12.4% [10]. It is important to highlight that several systematic reviews are based exclusively on prospective clinical trials, including low-risk patients. On the other hand, practice-based studies have displayed AFR higher when patients with high risk are included [8, 35]. In 11 Dutch general practices, a Practice-Based Study evaluated 31,472 restorations observed an AFR of 7.8% at 2 years [35]. A similar practice-based retrospective study that assessed the survival of resin composite restorations in posterior teeth found that 30% of the restorations failed, of which 82% were found in patients with high-risk factors, being secondary caries the main reason for failure [8].
The expectation of longevity is often determined by empirical criteria or measures, such as the average age of a failed restoration. There are several factors associated with restorative failures that are important to be evaluated for each clinical situation and can more accurately predict the longevity of restorations. The clinician’s expectations should be based on the assessment of risk factors, which may help a more accurate estimate. Thus, when the restoration is placed on a patient with risk factors (sometimes more than one) it is expected that the durability of this restoration may be less than average observed. On the other hand, when few risk factors are found clinically, greater longevity can be expected. To predict better the likelihood of restoration failure and make the expectation closer to reality, we need to discuss the main factors associated with the failure of composite materials.
10.1.1 Long-Term Survival and Reasons for Failures
Data on composite resin restorations’ survival have been widely explored for posterior teeth, while data of anterior teeth is more limited in the literature [11]. The main reasons for failure in posterior restorations seem to be secondary caries and the fracture of teeth/restorations [3, 26, 27] (Table 10.2). When high-risk patients are included, secondary caries commonly is reported as the main reason for restoration failure [8, 35, 51]. Fractures are frequently linked with premature or long-term (fatigue of material) failures, while caries is related to long-term follow-ups [52].
Fracture and esthetic demand have been reported as the main failure reasons for anterior esthetic restoration. Indeed, when the anterior restoration is placed for an esthetic reason, the likelihood main reason for failure will be related to esthetics (such as color match, anatomical form, or surface stain) [11]. Although direct comparisons between anterior and posterior restorations are not appropriate, in general, anterior restorations behave differently from posterior restorations, presenting reduced failures for “loss of restoration” or caries. At the same time, esthetic appearance plays a prominent role in the patient’s desire to have a restoration replaced.
10.1.1.1 Dental Caries
Secondary caries are reported to be the main reason for restoration’s failure. By definition, secondary or recurrent caries are “lesions at the margins of existing restorations” or “caries associated with restorations or sealants” (CARS) [53, 54]. It is important to note that restoring a tooth is not the definitive treatment for caries disease—but it may be a part of the treatment. To be clear, it is necessary to control all the etiological factors that are causing the disease [55]. The understanding of the causal factors for caries development and their respective control is necessary. As it is well-established, caries is a sugar-biofilm-dependent disease, and epidemiological studies have shown that sugar consumption in the life course is associated with caries lesions [56, 57]. In addition to diet, fluoride consumption, hygiene habits, socioeconomic factors, among others, are essential to be investigated and influence restoration’s survival through secondary caries failures. Considering these aspects, it is possible to treat caries disease properly, preventing the occurrence of secondary caries.
The failure to interrupt the caries disease can contribute to the failure of the restoration [58]. After 18 years, a retrospective study found that 68.4% of failures were due to secondary caries [59]. Posterior restorations placed in children with high DMFT index displayed a high risk to fail [60], corroborating with a systematic review that observed caries as the main reason for the failure of posterior restoration in primary teeth, independently of restorative material [9]. On the other hand, considering anterior composite restorations in permanent teeth, caries has a low contribution in failures in a systematic review [11], probably due to a low incidence of caries in the anterior region compared to posterior teeth. Practice-based studies have already corroborated these findings [37, 61, 62].
10.1.1.2 Fracture
Tooth/restoration fracture has been highlighted as the main reason for failure in anterior teeth. In a systematic review that evaluated the longevity of anterior restoration, the fracture (tooth/restoration) was the most common reason for failure among all studies [11], with rates varying from 25 to 100% of all failures observed in the included studies.
Bruxism of parafunctional habits probably plays a significant role in the fracture of the tooth or restorations via tooth-restoration complex fatigue, resulting in a fracture as a long-term outcome. In addition to the complex etiopathogenic mechanisms of bruxism, which hinder its correct diagnosis, in general, studies do not use reliable instruments for their assessment. Also, quite often, studies excluded bruxism patients. Restorations performed in participants with severe tooth wear presented negative findings when compared to participants without bruxism habits in a clinical study with patients with severe tooth wear [63]. Indeed, when restorations are placed in individuals presenting bruxism symptoms, more failures due to fracture could occur [64]. In a practice-based study, when patients showed “occlusal-stress,” there was a 2.6-fold risk of failure than in individuals with “no risk” [8].
10.1.1.3 Esthetic Demand
Modern society has increased the demand for esthetics [65]. Especially the anterior teeth must be well-aligned and white, which impacts the oral health-related quality of life [66]. The high visibility and the importance of the smile’s appearance expose the anterior restorations to a greater risk of undergoing interventions due to esthetic demands. In this region, small marginal pigmentations observed with the natural degradation of the hybrid layer or small natural changes in color or shape resulting from the natural aging of composites can result in early interventions in these restorations. Especially in patients who exhibit a high esthetic demand. Unlike the posterior region, where color changes appear to be less important [49]. It is clear that these changes are linked to factors related to patients and may depend on cultural and contextual factors of these individuals, which are incredibly subjective.
Upper front teeth restorations exhibited a higher risk for failure when compared with lower front teeth, especially in young patients [37]. Color alterations, marginal mismatch, and surface staining are some of the motifs for patients to require replacement of their veneer restorations [67]. However, for posterior teeth, the esthetic demand is a less important factor to some patients. When evaluating restorations after 27 years in clinical service, the ones carried out with chemical-cured resin composite (which presents accelerate deterioration of color match linked to the non-color stable initiators of the peroxide-initiated curing mechanism) were 59% non-acceptable to the researchers who evaluated these restorations, while only 6.3% of light-cured materials were classified as non-acceptable. However, these restorations were not classified as a failure because no patients requested replacement of non-acceptable color restoration, which were in function [49].
10.1.2 Factors Involved in Esthetic Restorations Failure
Whereas most of the attention in the clinical studies in restorative dentistry is given to the restoration’s longevity and the failure causes, it is of utmost importance to study all the factors affecting the restoration’s failure. I this context, even if most clinicians give quite some importance to the dental material and dental techniques, factors related to the characteristics of the patient, operator, and tooth are critical in assessing the long-term survival of restorations [10]. Also, population studies found that socioeconomic and demographic factors influenced the choice of restorative materials, the patients’ risk status, and, consequently, the longevity of the dental restorations [58].
10.1.2.1 Tooth Factors
Restoration survival depends on several clinical-related factors for their longevity, including the tooth position in the dental ark, tooth type, cavity size, previous endodontic treatment, and substrate type [3, 10, 27].
Restorations in premolars have shown better survival results than those placed in molars, and the explanations are related to higher masticatory forces observed in the molar region [8, 10, 38, 68,69,70]. After 10 years, general practitioners’ restorations have a hazard ratio of 2.3 to fail in molar than premolar [36]. Similar results have been reported in other studies [8, 10, 38, 68,69,70]. After 27 years, class II restorations in molars presented a failure risk almost 5 higher than premolars [49]. However, some studies did not find significant differences [45, 71]. For restoration in anterior teeth, failures were more frequent in upper central incisors and upper canines, when evaluating both children and adults in a practice-based study [37].
The increase in the number of surfaces involved in the restorations has been associated with a higher risk of failure [10, 36, 38, 72]. Posterior restorations fail 3.3 times more often in teeth with fewer than 2 remaining walls than those with 4 [73]. For premolars, each surface included in the restoration introduces a hazard risk of 1.5, while for molars, the risk is 1.24 [27]. Opdam et al. [38] estimate that each restored surface’s addition leads to an increased 40% risk of failure. Similarly, it was reported that every extra missing wall increases the failure risk from 30 to 40% [74]. Thus, class II restorations present a higher risk than Class I. Also, class III restorations tend to fail less than other anterior restorations types [11]. Collares et al. [37] observed a high-risk of failure in anterior restorations with three or more involved surfaces (Class IV) than class III restoration, highlighting that restoration size is an important predictor of failure risk also in anterior teeth.
Glass ionomer cement sandwich-type restorations are frequently used to perform indirect pulp protection in deep caries lesions. Using a GIC liner or base under composite resin restorations has shown divergent results in the literature. In several studies, the use of an intermediate GIC liner negatively influenced the restorations’ survival, resulting in more fracture of composite resin [10, 27, 38, 75, 76]. An AFR of 3.8% was observed for class II restorations with glass ionomer bases while observing an AFR of 1.4% for restorations without a base material [38]. In opposite, other studies observed no effect on restoration longevity when using GIC liners [44, 68, 77]. The thickness and type of glass ionomer cement used could explain the different results observed [10, 44]. Therefore, there is no consensus in the literature about the influence of GIC under composite restorations.
The endodontic treatment represents a challenging situation for restoration longevity in both anterior and posterior teeth. The significant loss of dental structure in these teeth could be related to the main reason for reducing the success rate. A 13-year clinical trial comparing restorations in vital and endodontic treated teeth observed AFR of 0.08 and 1.78%, respectively [40]. An AFR of 4.9% was observed in vital teeth and 9.8% in non-vital teeth in evaluating anterior composite veneers. Veneers made in non-vital teeth had a higher risk of failure (HR 2.78; 95% CI 1.02–7.56) over time compared to those made in vital teeth [39].
The selective carious tissue removal of soft dentine has also been discussed. It is important to consider that selective caries removal decreases the risk of pulp exposition [41] and can improve the longevity of restorations [42]. A 5-years randomized trial observed that selective caries removal to soft dentin in deep caries did not affect the restoration survival when compared to stepwise excavation [43]. A systematic review observed that selective caries removal have similar results in restoration longevity than stepwise excavation and result in fewer pulp complications [42]. Similar results were observed in a multicenter clinical trial considering primary posterior teeth. The longevity of restorations was similar between non-selective and selective carious tissue removal over 33 months [78]; but a systematic review with a limited number of included articles with a high risk of bias have observed that—in primary teeth—selective caries removal decrease the restoration longevity [79]. Thus, for primary teeth, no definitive conclusion about the influence of selective caries removal on restoration longevity can be performed.
10.1.2.2 Patients’ Related Factors
The focus of a vast number of clinical trials investigating the survival of restorations is limited to comparisons between technic or materials [80, 81] while patients-related factors are not investigated. The contribution to patient-related factors on restoration survival cannot be ignored [11, 27, 28]. When patients are not mainly selected for inclusion criteria in clinical trials, some studies have observed that failures are linked to certain participants, independently of restorative material used [82]. Similar results are observed in epidemiological studies where caries is the central factor in explaining the failure and replacement of dental restorations [83, 84]. Corroborating, a birth cohort study, observed that unsatisfactory restorations at 24 years were more prevalent in individuals that presented a high number of decayed teeth at 15 years [58].
Caries risk of patients has been associated with higher restorations failure. Restorations placed in the high-risk group showed a lower survival rate than the low-risk group after 5 and 12 years. Considering 12 years of evaluation, AFR was 4.2% in the high-risk group and 0.9% in the low caries risk group [45]. In a clinical trial, corroborating that after 30 years, 64% of restorations that failed due to secondary caries were observed in the high-risk group [71]. A review observed that caries risk was associated with decreased restoration survival, including amalgam and composite resin [28]. In a cohort study evaluating posterior restorations (composite or amalgam), it was observed that individuals who had a higher trajectory of caries during their life were more likely to present failed restorations in adult life [47]. In another cohort study, in children at the age 12, the chances of presenting unsatisfactory restorations were 5.3 higher in children at high-risk for untreated dental caries in the permanent dentition than children at low risk. If the parents have received orientation from professionals on preventing caries development in their offspring, the children exhibited a 91.0% less chance of having an unsatisfactory restoration than children whose parents never received information [46]. Decayed, missing, filled teeth-surfaces (DMFT-S) have been used to evaluate caries experience, even as the component D of DMFT. Also, the number of the previous restoration was used to access caries risk. However, the use of a cumulative indicator could overestimate the caries risk. Therefore, identifying high-caries risk patients when the restoration is placed may provide a reasonable estimate, such as the lesion activity assessment [85].
Bruxism and parafunctional habits have been reported as factors that overload the restorations and increases the likelihood of restoration/teeth failure due to fatigue. Fracture of restorations is frequently reported as the second main reason for restorations failure. Fracture is the main failure of patients with habits of grinding and clenching teeth [8]. 70% of the restoration’s fractures occurred in patients with the parafunctional habit in a long-term follow-up (30 years) [71]. Patients with bruxism were also associated with a 37-fold more failed restoration or catastrophic fracture occurred whether the teeth presented root canal treatment [40]. In a practice-based retrospective study that evaluated the survival of resin composite restorations in posterior teeth, individuals with high occlusal-stress displayed three times higher risk to failure than individuals with low occlusal-stress; moreover, individuals with occlusal-stress and caries risk showed a cumulative effect and eight times more failures than individuals no risk [8].
Instruments for assessing bruxism habits used in studies that evaluate restorative materials are not objective, and they do not present standardized cutoff points, which limit their inference [10]. The most recent International Consensus [86] proposed a system for evaluating bruxism, considering that possible bruxism during sleep is based only on the author’s report (report of patients), probable sleep bruxism (with clinical inspection such as the presence of tooth wear), and definitive sleep bruxism (based on instrumental assessment, such as polysomnographic). Furthermore, bruxism’s etiology is considered to be multifactorial, and several underlying mechanisms may play a role in triggering and perpetuating events [87].
Post-operative sensitivity was one of the causes of patient-related failures in the first clinical studies evaluating composite restorations; however, such aspect is not observed in modern studies, primarily due to the improvements in adhesive systems [88] and restorative technique [89]. Several studies have found that participant’s age significantly influences restoration longevity [37, 90, 91]. The explanations are directed to the influence of age in other co-variables like dental caries, patient cooperation, among others, and it is not recommended to be considered as an isolated factor [5]. Caries activity has been reported to be the more frequent reason for making a dental restoration in the young population. Consequently, these restorations would be subject to higher risk due to individual factors. A study that followed 4355 restorations placed by 115 dentists in the Public Dental Health Service in Denmark observed that posterior composite resin restorations placed in children presented more likely to fail than those placed in the adolescent group [90].
10.1.2.3 Socioeconomic Status
Limited studies have investigated the influence of socioeconomic variables and their influence on the longevity of composite restorations. Most studies evaluating the longevity of restorations are carried out in private dental clinics or are performed under high control in randomized clinical trials, excluding patients with high-caries risk [10]. Frequently only individuals with high socioeconomic status are included. However, the findings of studies that investigate the influence of socioeconomic status suggest that it influences dental restorations survival via dental caries. One study carried out in a birth cohort investigate the influence of socioeconomic trajectory in the life course and found more unsatisfactory restorations in the low trajectory group. Individuals who always lived in the poorest stratus presented more failures than those who lived in the wealthiest layer [58]. A more recent follow-up of this cohort reported that posterior restorations’ failures were significant associated with socioeconomic status at age 30, with a prevalence ratio of 2.21 (95% CI 1.19–4.09) in low-income tertile [47]. In the same way, a recent study assessing restorations performed in the Brazilian public oral health service found that people with lower access to public services presented lower survival rates of composite restorations [92]. A practice-based study also observed that restorations performed by clinicians located in the more deprived region presented higher AFR than those found in areas of medium and high socioeconomic status [48]. Some studies have corroborated with the discussion of the influence of socioeconomic and behavioral factor on the survival of composite resins [93,94,95,96].
10.1.2.4 Restorative Material
Although in vitro studies have found considerable differences between the properties of commercially available restorative materials [97, 98], these findings are limited in predicting the clinical behavior of restorations [76]. In fact, in vitro and clinical studies have presented contradictory evidence of direct restorations’ clinical performance in posterior teeth [24]. Perhaps differences observed in laboratory tests will take decades to be observed clinically [17]. Yet, the differences can be so minor in clinical outcomes that they may not be statistically significant [71]. For posterior teeth, a retrospective study with data from one dentist’s private clinical practice followed two types of composites for long periods. No differences in performances were observed 17 years; however, after 22 years of follow-up, midfilled (70 vol% inorganic filler loading) composite showed superior performance than minifilled (55 vol% inorganic filler loading) [17]. Similar tendencies were observed to anterior restorations: only after 10 years of follow-up significative differences between restorative composites were clinically observed [61].
Another study that retrospectively evaluated for up to 20 years the longevity of restorations placed by one operator under rubber dam isolation and patients with regular check-up visits did not find differences between the composites placed in posterior teeth [99]. Similarly, after 30 years of another controlled trial, no differences between composite resins placed with chemical-cured and light-cured resin composite were observed regarding survival rate. Thus, to compare the clinical survival of restorations is necessary long-term studies. Moreover, these studies’ results are with materials that were developed decades ago and are expected to be inferior to the composite resins recently developed.
A wide number of composite materials have been introduced in the market, and the clinical trials’ design to compare these new materials present few years of follow-up. The main modification in the inorganic formulation of composites was the introduction of nanofiller composites. These materials were created to provide superior polish and gloss retention. A randomized 10-years trial of class II nanohybrid and conventional hybrid resin composite observed an overall AFR of 1.9% and no significant difference between the composites [100]. In another study, the overall success rate was 100% after 6 years of clinical evaluation for nanohybrid and hybrid composite [101]. At 8 years, the success rate was 98.5%, with no differences observed between materials [102].
A recent development in resin composite technology was the introduction of “bulk-fill” resin composites. Bulk-fill composites can be cured in up to 4 or 5 mm layers and include both low as high viscosity materials. A randomized clinical trial compared to class I and II restorations compared flowable bulk-filled resin composite (in increments up to 4 mm as needed to fill the cavity and 2 mm short of the occlusal cave surface with the occlusal part completed with nanohybrid resin composite) and resin composite-only placed in 2 mm increments. After 5 years of evaluation, bulk-filled presented an AFR of 1.1% and the resin composite-only restorations of 1.3%, with no significant differences detected between the materials [102].
Although the comparisons of direct and indirect composite restorations have similar performance and longevity [24], other factors related to the restorative technique have been reported to influence the clinical performance of composite materials. Adhesive systems are frequently evaluated in Class V restorations and also influenced the longevity of these restorations [103], even though, for anterior restorations, the degradation of the hybrid layer could affect more the esthetics, while such aspect seems not to be relevant for posterior composite restorations [88, 104, 105]. Regarding longevity or restorations, the gold standard dental adhesive technique is the use of a mild two-step, self-etch adhesive system with selective phosphoric acid enamel etching [50] and bevel are not indicated because they does not affect the clinical performance [34]. Moreover, the use of rubber dam isolation does not seem to affect the longevity of restorations, as long as it is applied effectively with cotton rolls and suction devices. Although some studies have observed better performances of restorations applied under rubber dam isolation [9, 34], the evidence shows that restorations placed using cotton rolls and suction device can also survive for long periods [49] and the use of appropriate suction device and working with the aid of a dental nurse are even more important for achieving good isolation from humidity in case rubber dam is not used.
10.1.2.5 Operator
Dentist-linked factors, such as operator skills, are considered important factors that influenced the survival of composite resin restorations [5]. Although a wide part of results is explained solely on the training level and accuracy of work, the decision-making process also can influence restoration survival and could combine as a complex process, ranging among clinicians according to co-variables, such as the type of practice, reimbursement system, competition environment among dentists, patients’ views and opinions, and cultural aspects.
The dentists are the ones who place the restorations, those who evaluate them, and, ultimately, decide when the restoration needs to be changed. Variability on diagnostic and decision-making has been elevated among dentists that frequently adopt an invasive approach to intervene in restorations, especially when they were performed by other professionals [13]. Invasive behavior toward restoration replacement results in a decrease in the survival of restoration. Chisini et al. [106] observed that the decision-making of dentists was influenced by patient skin color. Clinicians choose more to replace ill-adapted restoration in white patients while they decide not to intervene in restoration from dark-skinned individuals [106]. Dentists frequently choose to replace restorations with a small sign of marginal degradation or staining because they then confound with secondary caries. After 27 years of follow-up on posterior chemical-cured resin composite with the high color changed (classified as non-acceptable research evaluators) were maintained in function and classified as satisfactory to the patients [49]. Even secondary caries kept restricted in the enamel can be maintained and treated with non-operative treatments [107], and the repair can—preferably—choose if operative treatment is required.
Despite clinical studies with trained and calibrated operators maybe not observe significant associations between operator and success, practice-based studies have observed that age, country of qualification, and employment status of the operator could influence the survival of restoration [5]. Data from Washington dental service observed that restorations placed by efficient dentists survive almost 5 months more than restorations performed by inefficient dentists, and no differences between the restorations were observed when efficient dentists performed than [108]. Similarly, the longevity of restorations placed by more experienced clinicians was better than those placed for less experienced ones [109]. Restorations placed by the dentist with less practice workload presented a success rate of about twice than those slightly busy clinicians [110]. A geospatial analysis carried out in Canada observed more aggressive treatment choices were performed by dentists who feel under great competitive pressure and in low dentist density areas [111]. Therefore, all these issues and the differences in the decision-making process on judging restorations intensification the risk for replacement restorations and decrease the survival rates.
10.2 Repairing Esthetic Composite Restorations
Patients that changed the dentist have an increased chance to replace their restorations [93,94,95,96]. In fact, a cross-sectional study that included 194 dentists of the Dental Practice-Based Research Network observed that the decision to repair defective restoration instead to replace is influenced by who place the original one: clinicians are less demanding when evaluating their work [13]. The decision to replace a restoration relies on the dentist’s clinical expertise rather than on strict criteria. Thus, dentists adopt different approaches (repair or replacement) in cases of imperfect restorations [112], although the literature presents a consensus that, when possible, repaired restorations presents benefits and are more cost-effective than replacement [16].
10.2.1 Long-Term Survival and Reasons for Failures of Repaired Restorations
Replacement of a failed restoration is still one of the most frequent treatments performed in dental practice [113]. While most dentists state to perform repairs, and the vast majority of dental schools teach repairs, the proportion of truly repaired restorations is still very low [16]. A clinical trial assessed the longevity of repaired restorations and showed similar longevity than replaced restorations after 12 years of follow-up [15]. Repaired and replaced restorations presented similar behavior in marginal adaptation, marginal stain, teeth sensitivity, anatomic form, and luster parameter, although roughness was significative was significantly worse in the group of repaired restorations [15].
Casagrande et al. [114] estimated the reduction in AFR when repaired restorations were not considered as a “true failure” and observed that repair increases the longevity of direct posterior restorations. When repair was not considered as a failure, the survival of restoration changed from 83.1 (AFR = 3.6%) to 87.9% (ARF = 2.5%) at 5 years and from 65.9 (AFR = 4.1%) to 74.6% (AFR = 2.9%) at 10 years of follow-up. Reduction of AFR from 1.83 to 0.72% in composite resins repaired restorations after 12 years of follow-up was observed in another study [115]. A study that follows for 22 years posterior composite restorations performed by one dentist observed that a reduction from 1.9 to 0.7% on AFR when restorations repaired were not considered as failures [10, 17].
A study that evaluated 880 restorations placed in posterior and anterior teeth observed that repair increases the survival of restorations even after previous repairs or replacements [116]. A recent long-term practice-based clinical study carried out in a private dental practice followed class III and class IV for 15 years, and veneer restorations for 10 years. For class III and class IV restoration, AFR was 2.9%, and for veneers 9.2% when the repair was considered as failure. When repair was not considered as failure, class III and IV presented an AFR of 2.4% and veneers of 6.3% [117]. Thus, direct comparisons between the treatments (repair and replacement) presented comparable results.
In this way, secondary caries was the main reason for failure in both repaired and replaced restorations [15] while Opdam et al. [115] reported tooth fracture as the main reason for failure in the repaired restorations (41.1%) followed by dental caries (24.2%) [115]. These two reasons are the same observed for non-repaired restorations both in permanent [8, 10] and primary teeth [9].
10.2.2 Factors Involved in Repaired Restorations Failure
Regarding the main reasons for failures, studies have shown, in general, that the same factors known for non-repaired restorations seem to influence repaired restorations as well. Casagrande et al. [114] found that endodontic treatment, molar teeth, use of a prosthesis, and age were important risk factors for restoration failure. On the other hand, in one study, only sex was reported as associated as a risk factor to failure in repaired restorations, in which women presented a risk of failure twice higher when compared to men [115]. Cox regression analysis in a practice-based study found that class III and IV restorations placed in the upper jaw had a higher risk for failure compared to the lower jaw. Central incisors also had a higher failure risk for failed repaired restorations. Also, the type of composite influenced the survival rates [117]. The presence of endodontic treatment is a factor associated with a higher risk of failure for both repaired or replaced restorations [116].
10.2.3 Repairing Benefits Over Replacing Restorations
The comparison of the survival of replaced versus repaired restoration may be unfair. A repaired restoration is comprised mostly of the older and aged part of a restoration. It presents already signs of fatigue, differently from a replaced filling that is entirely new. Thus, a repaired and older restoration may fail before the replaced one. But even in this case, the survival of the original restoration is increased, and the removal of tooth tissue is postponed, which could be the main direct benefits. If the repaired restoration fails, the replacement is indicated and can be carried out without further problems. Repair is considered an approach of minimal intervention dentistry, being an alternative to easy, fast, and low-cost treatment [16]. The clinical time spent to replace a restoration is reported to be higher than the time required to repair the same restoration. Additionally, the repair of restoration seems to be more cost-effective than replacement, and thus repairs are drawn as an important strategy for public health services [16].
10.2.4 When Repairing Is Not a Solution?
Repair of defective restorations is not always possible. Like this, the Academy of Operative Dentistry European Section has indicated the restoration replacement when (a) restoration has unaccepted qualities (deterioration/secondary caries); (b) repair is contraindicated; (c) benefits of replacement are less than possible harm; (d) prospects for an acceptable clinical outcome are favorable; and (e) patient consents [118].
10.3 Replacing Esthetic Composite Restorations
As previously discussed, composites have shown considerable improvements since their introduction in the 1960s. Due to the improvement of the properties of the material, nowadays, most of the failures are related to factors related to the patient and the operator. When small changes in color, shape, or fractures are observed, repair should always be the first choice. However, in some situations where the remaining restoration is integrally degraded, replacement of the restoration can be indicated.
10.3.1 Restorations Do Not Last Forever
Composite resin restorations are materials that, like any other, present aging over time. The degradation of the hybrid layer and its respective pigmentation are the main surface changes in the medium term; together with small changes in surface roughness, they can be overcome with surface finishing and polishing. However, this marginal degradation or marginal staining cannot be mistakenly interpreted as secondary caries. Limited time is used to teach secondary caries diagnosis in dental schools and this fact could be a contributor for the lack of consensus among dentists regarding the interventions on restorative. Considering that criteria for repair/replacement are not clear among dentists, [118] suggest a shift from “in doubt, take it out” toward “as a last resort take it out” after considering monitoring, refurbishment, and repair as the first treatment options.
10.3.2 Aspects That Can Increase the Longevity of Esthetic Composite Restorations
Composite restorations have shown excellent survival rates on anterior and posterior teeth. Due to materials improvements overtime, current materials’ properties have revelated a minor influence on the survival of composites in clinical studies. When hybrid or nanohybrid composites are used, low AFR could be expected. To improve the longevity of these restorations, patient-related factors and operators are fundamental. Therefore, restorations should be carried out in a health promotion environment, emphasizing preventive practices. The adoption of healthy behaviors by patients will consequently led to “healthy” restorations, increasing the longevity of treatments. The adoption of minimally invasive dentistry for the management of deteriorated restorations, such as refurbishment or repair restorations, should be considered in routine practice. In this way, dentists should react less in front of small defects of restorations, indicating replacements only when other alternatives are not plausible.
References
Demarco FF, Baldissera RA, Madruga FC, Simoes RC, Lund RG, Correa MB, Cenci MS. Anterior composite restorations in clinical practice: findings from a survey with general dental practitioners. J Appl Oral Sci. 2013;21:497–504.
Nascimento GG, Correa MB, Opdam N, Demarco FF. Do clinical experience time and postgraduate training influence the choice of materials for posterior restorations? Results of a survey with Brazilian general dentists. Braz Dent J. 2013;24:642–6.
Manhart J, Chen H, Hamm G, Hickel R. Buonocore memorial lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent. 2004;29:481–508.
Maran BM, de Geus JL, Gutierrez MF, Heintze S, Tardem C, Barceleiro MO, Reis A, Loguercio AD. Nanofilled/nanohybrid and hybrid resin-based composite in patients with direct restorations in posterior teeth: a systematic review and meta-analysis. J Dent. 2020;99:103407.
Demarco FF, Collares K, Correa MB, Cenci MS, Moraes RR, Opdam NJ. Should my composite restorations last forever? Why are they failing? Braz Oral Res. 2017;31:e56.
Mesko ME, Sarkis-Onofre R, Cenci MS, Opdam NJ, Loomans B, Pereira-Cenci T. Rehabilitation of severely worn teeth: a systematic review. J Dent. 2016;48:9–15.
Vetromilla BM, Opdam NJ, Leida FL, Sarkis-Onofre R, Demarco FF, van der Loo MPJ, Cenci MS, Pereira-Cenci T. Treatment options for large posterior restorations: a systematic review and network meta-analysis. J Am Dent Assoc. 2020;151:614–24.
van de Sande FH, Opdam NJ, Rodolpho PA, Correa MB, Demarco FF, Cenci MS. Patient risk factors’ influence on survival of posterior composites. J Dent Res. 2013;92:78S–83S.
Chisini LA, Collares K, Cademartori MG, de Oliveira LJC, Conde MCM, Demarco FF, Correa MB. Restorations in primary teeth: a systematic review on survival and reasons for failures. Int J Paediatr Dent. 2018;28:123–39.
Demarco FF, Correa MB, Cenci MS, Moraes RR, Opdam NJ. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater. 2012;28:87–101.
Demarco FF, Collares K, Coelho-de-Souza FH, Correa MB, Cenci MS, Moraes RR, Opdam NJ. Anterior composite restorations: a systematic review on long-term survival and reasons for failure. Dent Mater. 2015;31:1214–24.
Elderton RJ. Restorations without conventional cavity preparations. Int Dent J. 1988;38:112–8.
Gordan VV, Riley J 3rd, Geraldeli S, Williams OD, Spoto JC 3rd, Gilbert GH, National Dental PCG. The decision to repair or replace a defective restoration is affected by who placed the original restoration: findings from the National Dental PBRN. J Dent. 2014;42:1528–34.
Kanzow P, Hoffmann R, Tschammler C, Kruppa J, Rodig T, Wiegand A. Attitudes, practice, and experience of German dentists regarding repair restorations. Clin Oral Investig. 2017;21:1087–93.
Estay J, Martin J, Viera V, Valdivieso J, Bersezio C, Vildosola P, Mjor IA, Andrade MF, Moraes RR, Moncada G, Gordan VV, Fernandez E. 12 Years of repair of amalgam and composite resins: a clinical study. Oper Dent. 2018;43:12–21.
Kanzow P, Wiegand A, Schwendicke F. Cost-effectiveness of repairing versus replacing composite or amalgam restorations. J Dent. 2016;54:41–7.
Da Rosa Rodolpho PA, Donassollo TA, Cenci MS, Loguercio AD, Moraes RR, Bronkhorst EM, Opdam NJ, Demarco FF. 22-Year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dent Mater. 2011;27:955–63.
Afrashtehfar KI, Ahmadi M, Emami E, Abi-Nader S, Tamimi F. Failure of single-unit restorations on root filled posterior teeth: a systematic review. Int Endod J. 2017a;50:951–66.
Afrashtehfar KI, Emami E, Ahmadi M, Eilayyan O, Abi-Nader S, Tamimi F. Failure rate of single-unit restorations on posterior vital teeth: a systematic review. J Prosthet Dent. 2017b;117:345–53.
Ahmed KE, Murbay S. Survival rates of anterior composites in managing tooth wear: systematic review. J Oral Rehabil. 2016;43:145–53.
Angeletaki F, Gkogkos A, Papazoglou E, Kloukos D. Direct versus indirect inlay/onlay composite restorations in posterior teeth. A systematic review and meta-analysis. J Dent. 2016;53:12–21.
Astvaldsdottir A, Dagerhamn J, van Dijken JW, Naimi-Akbar A, Sandborgh-Englund G, Tranaeus S, Nilsson M. Longevity of posterior resin composite restorations in adults—a systematic review. J Dent. 2015;43:934–54.
Beck F, Lettner S, Graf A, Bitriol B, Dumitrescu N, Bauer P, Moritz A, Schedle A. Survival of direct resin restorations in posterior teeth within a 19-year period (1996–2015): a meta-analysis of prospective studies. Dent Mater. 2015;31:958–85.
da Veiga AM, Cunha AC, Ferreira DM, da Silva Fidalgo TK, Chianca TK, Reis KR, Maia LC. Longevity of direct and indirect resin composite restorations in permanent posterior teeth: a systematic review and meta-analysis. J Dent. 2016;54:1–12.
Heintze SD, Rousson V, Hickel R. Clinical effectiveness of direct anterior restorations—a meta-analysis. Dent Mater. 2015;31:481–95.
Moraschini V, Fai CK, Alto RM, Dos Santos GO. Amalgam and resin composite longevity of posterior restorations: a systematic review and meta-analysis. J Dent. 2015;43:1043–50.
Opdam NJ, van de Sande FH, Bronkhorst E, Cenci MS, Bottenberg P, Pallesen U, Gaengler P, Lindberg A, Huysmans MC, van Dijken JW. Longevity of posterior composite restorations: a systematic review and meta-analysis. J Dent Res. 2014;93:943–9.
van de Sande FH, Collares K, Correa MB, Cenci MS, Demarco FF, Opdam N. Restoration survival: revisiting patients’ risk factors through a systematic literature review. Oper Dent. 2016;41:S7–S26.
Arbildo-Vega HI, Lapinska B, Panda S, Lamas-Lara C, Khan AS, Lukomska-Szymanska M. Clinical effectiveness of bulk-fill and conventional resin composite restorations: systematic review and meta-analysis. Polymers (Basel). 2020;12:1786.
Veloso SRM, Lemos CAA, de Moraes SLD, Do Egito Vasconcelos BC, Pellizzer EP, de Melo Monteiro GQ. Clinical performance of bulk-fill and conventional resin composite restorations in posterior teeth: a systematic review and meta-analysis. Clin Oral Investig. 2019;23:221–33.
Azeem RA, Sureshbabu NM. Clinical performance of direct versus indirect composite restorations in posterior teeth: a systematic review. J Conserv Dent. 2018;21:2–9.
Rasines Alcaraz MG, Veitz-Keenan A, Sahrmann P, Schmidlin PR, Davis D, Iheozor-Ejiofor Z. Direct composite resin fillings versus amalgam fillings for permanent or adult posterior teeth. Cochrane Database Syst Rev. 2014;3:CD005620.
Fron Chabouis H, Smail Faugeron V, Attal JP. Clinical efficacy of composite versus ceramic inlays and onlays: a systematic review. Dent Mater. 2013;29:1209–18.
Heintze SD, Rousson V. Clinical effectiveness of direct class II restorations—a meta-analysis. J Adhes Dent. 2012;14:407–31.
Laske M, Opdam NJM, Bronkhorst EM, Braspenning JCC, Huysmans M. Risk factors for dental restoration survival: a practice-based study. J Dent Res. 2019;98:414–22.
Laske M, Opdam NJM, Bronkhorst EM, Braspenning JCC, Huysmans M. Ten-year survival of class II restorations placed by general practitioners. JDR Clin Trans Res. 2016b;1:292–9.
Collares K, Opdam NJM, Laske M, Bronkhorst EM, Demarco FF, Correa MB, Huysmans M. Longevity of anterior composite restorations in a general dental practice-based network. J Dent Res. 2017;96:1092–9.
Opdam NJ, Bronkhorst EM, Roeters JM, Loomans BA. Longevity and reasons for failure of sandwich and total-etch posterior composite resin restorations. J Adhes Dent. 2007;9:469–75.
Coelho-de-Souza FH, Goncalves DS, Sales MP, Erhardt MC, Correa MB, Opdam NJ, Demarco FF. Direct anterior composite veneers in vital and non-vital teeth: a retrospective clinical evaluation. J Dent. 2015;43:1330–6.
Lempel E, Lovasz BV, Bihari E, Krajczar K, Jeges S, Toth A, Szalma J. Long-term clinical evaluation of direct resin composite restorations in vital vs. endodontically treated posterior teeth—retrospective study up to 13 years. Dent Mater. 2019;35:1308–18.
Barros M, De Queiroz Rodrigues MI, Muniz F, Rodrigues LKA. Selective, stepwise, or nonselective removal of carious tissue: which technique offers lower risk for the treatment of dental caries in permanent teeth? A systematic review and meta-analysis. Clin Oral Investig. 2020;24:521–32.
Hoefler V, Nagaoka H, Miller CS. Long-term survival and vitality outcomes of permanent teeth following deep caries treatment with step-wise and partial-caries-removal: a systematic review. J Dent. 2016;54:25–32.
Jardim JJ, Mestrinho HD, Koppe B, de Paula LM, Alves LS, Yamaguti PM, Almeida JCF, Maltz M. Restorations after selective caries removal: 5-year randomized trial. J Dent. 2020;99:103416.
van de Sande FH, Rodolpho PA, Basso GR, Patias R, da Rosa QF, Demarco FF, Opdam NJ, Cenci MS. 18-Year survival of posterior composite resin restorations with and without glass ionomer cement as base. Dent Mater. 2015;31:669–75.
Opdam NJ, Bronkhorst EM, Loomans BA, Huysmans MC. A 12-Year survival of composite vs. amalgam restorations. J Dent Res. 2010;89:1063–7.
Cumerlato C, Demarco FF, Barros AJD, Peres MA, Peres KG, Morales Cascaes A, de Camargo MBJ, da Silva Dos Santos I, Matijasevich A, Correa MB. Reasons for direct restoration failure from childhood to adolescence: a birth cohort study. J Dent. 2019;89:103183.
Collares K, Opdam NJ, Peres KG, Peres MA, Horta BL, Demarco FF, Correa MB. Higher experience of caries and lower income trajectory influence the quality of restorations: a multilevel analysis in a birth cohort. J Dent. 2018;68:79–84.
Laske M, Opdam NJ, Bronkhorst EM, Braspenning JC, Huysmans MC. Longevity of direct restorations in Dutch dental practices. Descriptive study out of a practice based research network. J Dent. 2016a;46:12–7.
Pallesen U, van Dijken JW. A randomized controlled 27 years follow up of three resin composites in class II restorations. J Dent. 2015b;43:1547–58.
Van Meerbeek B, Peumans M, Poitevin A, Mine A, Van Ende A, Neves A, De Munck J. Relationship between bond-strength tests and clinical outcomes. Dent Mater. 2010;26:e100–21.
Montagner AF, Sande FHV, Muller C, Cenci MS, Susin AH. Survival, reasons for failure and clinical characteristics of anterior/posterior composites: 8-year findings. Braz Dent J. 2018;29:547–54.
Brunthaler A, Konig F, Lucas T, Sperr W, Schedle A. Longevity of direct resin composite restorations in posterior teeth. Clin Oral Investig. 2003;7:63–70.
Askar H, Krois J, Gostemeyer G, Bottenberg P, Zero D, Banerjee A, Schwendicke F. Secondary caries: what is it, and how it can be controlled, detected, and managed? Clin Oral Investig. 2020;24:1869–76.
Machiulskiene V, Campus G, Carvalho JC, Dige I, Ekstrand KR, Jablonski-Momeni A, Maltz M, Manton DJ, Martignon S, Martinez-Mier EA, Pitts NB, Schulte AG, Splieth CH, Tenuta LMA, Ferreira Zandona A, Nyvad B. Terminology of Dental Caries and Dental Caries Management: consensus report of a workshop organized by ORCA and Cariology Research Group of IADR. Caries Res. 2020;54:7–14.
Sheiham A. Dietary effects on dental diseases. Public Health Nutr. 2001;4:569–91.
Moynihan PJ, Kelly SA. Effect on caries of restricting sugars intake: systematic review to inform WHO guidelines. J Dent Res. 2014;93:8–18.
Peres MA, Sheiham A, Liu P, Demarco FF, Silva AE, Assuncao MC, Menezes AM, Barros FC, Peres KG. Sugar consumption and changes in dental caries from childhood to adolescence. J Dent Res. 2016;95:388–94.
Correa MB, Peres MA, Peres KG, Horta BL, Barros AJ, Demarco FF. Do socioeconomic determinants affect the quality of posterior dental restorations? A multilevel approach. J Dent. 2013;41:960–7.
Alonso V, Darriba IL, Caserio M. Retrospective evaluation of posterior composite resin sandwich restorations with Herculite XRV: 18-year findings. Quintessence Int. 2017;48:93–101.
Trachtenberg F, Maserejian NN, Tavares M, Soncini JA, Hayes C. Extent of tooth decay in the mouth and increased need for replacement of dental restorations: the New England Children’s amalgam trial. Pediatr Dent. 2008;30:388–92.
Baldissera RA, Correa MB, Schuch HS, Collares K, Nascimento GG, Jardim PS, Moraes RR, Opdam NJ, Demarco FF. Are there universal restorative composites for anterior and posterior teeth? J Dent. 2013;41:1027–35.
van Dijken JW, Pallesen U. Fracture frequency and longevity of fractured resin composite, polyacid-modified resin composite, and resin-modified glass ionomer cement class IV restorations: an up to 14 years of follow-up. Clin Oral Investig. 2010;14:217–22.
Bartlett D, Sundaram G. An up to 3-year randomized clinical study comparing indirect and direct resin composites used to restore worn posterior teeth. Int J Prosthodont. 2006;19:613–7.
Hamburger JT, Opdam NJ, Bronkhorst EM, Kreulen CM, Roeters JJ, Huysmans MC. Clinical performance of direct composite restorations for treatment of severe tooth wear. J Adhes Dent. 2011;13:585–93.
Silva FBD, Chisini LA, Demarco FF, Horta BL, Correa MB. Desire for tooth bleaching and treatment performed in Brazilian adults: findings from a birth cohort. Braz Oral Res. 2018;32:e12.
Goettems ML, Fernandez MDS, Donassollo TA, Henn Donassollo S, Demarco FF. Impact of tooth bleaching on oral health-related quality of life in adults: a triple-blind randomised clinical trial. J Dent. 2021;105:103564.
Alonso V, Caserio M. A clinical study of direct composite full-coverage crowns: long-term results. Oper Dent. 2012;37:432–41.
Lindberg A, van Dijken JW, Lindberg M. Nine-year evaluation of a polyacid-modified resin composite/resin composite open sandwich technique in class II cavities. J Dent. 2007;35:124–9.
Pallesen U, van Dijken JW, Halken J, Hallonsten AL, Hoigaard R. Longevity of posterior resin composite restorations in permanent teeth in public dental health service: a prospective 8 years follow up. J Dent. 2013;41:297–306.
van Dijken JW, Pallesen U. Eight-year randomized clinical evaluation of class II nanohybrid resin composite restorations bonded with a one-step self-etch or a two-step etch-and-rinse adhesive. Clin Oral Investig. 2015;19:1371–9.
Pallesen U, van Dijken JW. A randomized controlled 30 years follow up of three conventional resin composites in class II restorations. Dent Mater. 2015a;31:1232–44.
Lempel E, Toth A, Fabian T, Krajczar K, Szalma J. Retrospective evaluation of posterior direct composite restorations: 10-year findings. Dent Mater. 2015;31:115–22.
Tobi H, Kreulen CM, Vondeling H, van Amerongen WE. Cost-effectiveness of composite resins and amalgam in the replacement of amalgam class II restorations. Community Dent Oral Epidemiol. 1999;27:137–43.
Smales RJ, Webster DA. Restoration deterioration related to later failure. Oper Dent. 1993;18:130–7.
Andersson-Wenckert IE, van Dijken JW, Kieri C. Durability of extensive class II open-sandwich restorations with a resin-modified glass ionomer cement after 6 years. Am J Dent. 2004;17:43–50.
da Rosa Rodolpho PA, Cenci MS, Donassollo TA, Loguercio AD, Demarco FF. A clinical evaluation of posterior composite restorations: 17-year findings. J Dent. 2006;34:427–35.
van Dijken JW. Durability of resin composite restorations in high C-factor cavities: a 12-year follow-up. J Dent. 2010;38:469–74.
Pereira JT, Knorst JK, Ardenghi TM, Piva F, Imparato JCP, Olegario IC, Hermoza RAM, Armas-Vega ADC, de Araujo FB. Pulp vitality and longevity of adhesive restorations are not affected by selective carious removal: a multicenter clinical trial. Caries Res. 2021;55:55–62.
Pedrotti D, Cavalheiro CP, Casagrande L, de Araujo FB, Pettorossi Imparato JC, de Oliveira RR, Lenzi TL. Does selective carious tissue removal of soft dentin increase the restorative failure risk in primary teeth? Systematic review and meta-analysis. J Am Dent Assoc. 2019;150:582–90.
Shi L, Wang X, Zhao Q, Zhang Y, Zhang L, Ren Y, Chen Z. Evaluation of packable and conventional hybrid resin composites in class I restorations: three-year results of a randomized, double-blind and controlled clinical trial. Oper Dent. 2010;35:11–9.
Yazici AR, Ustunkol I, Ozgunaltay G, Dayangac B. Three-year clinical evaluation of different restorative resins in class I restorations. Oper Dent. 2014;39:248–55.
van Dijken JW. Direct resin composite inlays/onlays: an 11 year follow-up. J Dent. 2000;28:299–306.
Burke FJ, Cheung SW, Mjor IA, Wilson NH. Restoration longevity and analysis of reasons for the placement and replacement of restorations provided by vocational dental practitioners and their trainers in the United Kingdom. Quintessence Int. 1999;30:234–42.
Sunnegardh-Gronberg K, van Dijken JW, Funegard U, Lindberg A, Nilsson M. Selection of dental materials and longevity of replaced restorations in public dental health clinics in northern Sweden. J Dent. 2009;37:673–8.
Maltz M, Leal FL, Wagner MB, Zenkner J, Brusius CD, Alves LS. Can we diagnose a patient’s caries activity based on lesion activity assessment? Findings from a cohort study. Caries Res. 2020;54:218–25.
Lobbezoo F, Ahlberg J, Raphael KG, Wetselaar P, Glaros AG, Kato T, Santiago V, Winocur E, De Laat A, De Leeuw R, Koyano K, Lavigne GJ, Svensson P, Manfredini D. International consensus on the assessment of bruxism: report of a work in progress. J Oral Rehabil. 2018;45:837–44.
Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008;35:476–94.
Perdigao J, Dutra-Correa M, Castilhos N, Carmo AR, Anauate-Netto C, Cordeiro HJ, Amore R, Lewgoy HR. One-year clinical performance of self-etch adhesives in posterior restorations. Am J Dent. 2007;20:125–33.
Perdigao J, Geraldeli S, Hodges JS. Total-etch versus self-etch adhesive: effect on postoperative sensitivity. J Am Dent Assoc. 2003;134:1621–9.
Pallesen U, van Dijken JW, Halken J, Hallonsten AL, Hoigaard R. A prospective 8-year follow-up of posterior resin composite restorations in permanent teeth of children and adolescents in public dental health service: reasons for replacement. Clin Oral Investig. 2014;18:819–27.
Soncini JA, Maserejian NN, Trachtenberg F, Tavares M, Hayes C. The longevity of amalgam versus compomer/composite restorations in posterior primary and permanent teeth: findings from the New England Children’s amalgam trial. J Am Dent Assoc. 2007;138:763–72.
da Silva Pereira RA, da Silva GR, Barcelos LM, Cavalcanti K, Herval AM, Ardenghi TM, Soares CJ. Practice-based analysis of direct posterior dental restorations performed in a public health service: retrospective long-term survival in Brazil. PLoS One. 2020;15:e0243288.
Burke FJ, Lucarotti PS, Holder R. Outcome of direct restorations placed within the general dental services in England and Wales (part 4): influence of time and place. J Dent. 2005a;33:837–47.
Burke FJ, Lucarotti PS, Holder RL. Outcome of direct restorations placed within the general dental services in England and Wales (part 2): variation by patients’ characteristics. J Dent. 2005b;33:817–26.
Lucarotti PS, Holder RL, Burke FJ. Outcome of direct restorations placed within the general dental services in England and Wales (part 3): variation by dentist factors. J Dent. 2005a;33:827–35.
Lucarotti PS, Holder RL, Burke FJ. Outcome of direct restorations placed within the general dental services in England and Wales (part 1): variation by type of restoration and re-intervention. J Dent. 2005b;33:805–15.
Borba M, Della Bona A, Cecchetti D. Flexural strength and hardness of direct and indirect composites. Braz Oral Res. 2009;23:5–10.
Koytchev E, Yamaguchi S, Shin-No Y, Suzaki N, Okamoto M, Imazato S, Datcheva M, Hayashi M. Comprehensive micro-mechanical characterization of experimental direct core build-up resin composites with different amounts of filler contents. Dent Mater J. 2019;38:743–9.
Borgia E, Baron R, Borgia JL. Quality and survival of direct light-activated composite resin restorations in posterior teeth: a 5- to 20-year retrospective longitudinal study. J Prosthodont. 2019;28:e195–203.
van Dijken JW, Pallesen U. A randomized 10-year prospective follow-up of class II nanohybrid and conventional hybrid resin composite restorations. J Adhes Dent. 2014;16:585–92.
Kramer N, Garcia-Godoy F, Reinelt C, Feilzer AJ, Frankenberger R. Nanohybrid vs. fine hybrid composite in extended class II cavities after six years. Dent Mater. 2011;27:455–64.
Frankenberger R, Reinelt C, Kramer N. Nanohybrid vs. fine hybrid composite in extended class II cavities: 8-year results. Clin Oral Investig. 2014;18:125–37.
Matos TP, Gutierrez MF, Hanzen TA, Malaquias P, de Paula AM, de Souza JJ, Hass V, Fernandez E, Reis A, Loguercio AD. A 18-Month clinical evaluation of a copper-containing universal adhesive in non-carious cervical lesions: a double-blind, randomized controlled trial. J Dent. 2019;90:103219.
Opdam NJ, Feilzer AJ, Roeters JJ, Smale I. Class I occlusal composite resin restorations: in vivo post-operative sensitivity, wall adaptation, and microleakage. Am J Dent. 1998a;11:229–34.
Opdam NJ, Roeters FJ, Feilzer AJ, Verdonschot EH. Marginal integrity and postoperative sensitivity in class 2 resin composite restorations in vivo. J Dent. 1998b;26:555–62.
Chisini LA, Noronha TG, Ramos EC, Dos Santos-Junior RB, Sampaio KH, Faria ESAL, Correa MB. Does the skin color of patients influence the treatment decision-making of dentists? A randomized questionnaire-based study. Clin Oral Investig. 2019;23:1023–30.
Schwendicke F, Splieth C, Breschi L, Banerjee A, Fontana M, Paris S, Burrow MF, Crombie F, Page LF, Gaton-Hernandez P, Giacaman R, Gugnani N, Hickel R, Jordan RA, Leal S, Lo E, Tassery H, Thomson WM, Manton DJ. When to intervene in the caries process? An expert Delphi consensus statement. Clin Oral Investig. 2019;23:3691–703.
Coppola MN, Ozcan YA, Bogacki R. Evaluation of performance of dental providers on posterior restorations: does experience matter? A data envelopment analysis (DEA) approach. J Med Syst. 2003;27:445–56.
Opdam NJ, Loomans BA, Roeters FJ, Bronkhorst EM. Five-year clinical performance of posterior resin composite restorations placed by dental students. J Dent. 2004;32:379–83.
McCracken MS, Gordan VV, Litaker MS, Funkhouser E, Fellows JL, Shamp DG, Qvist V, Meral JS, Gilbert GH, National Dental Practice-Based Research Network Collaborative G. A 24-month evaluation of amalgam and resin-based composite restorations: findings from the National Dental Practice-Based Research Network. J Am Dent Assoc. 2013;144:583–93.
Ghoneim A, Yu B, Lawrence HP, Glogauer M, Shankardass K, Quinonez C. Does competition affect the clinical decision-making of dentists? A geospatial analysis. Community Dent Oral Epidemiol. 2020;48:152–62.
Heaven TJ, Gordan VV, Litaker MS, Fellows JL, Brad Rindal D, Firestone AR, Gilbert GH, National Dental PCG. Agreement among dentists’ restorative treatment planning thresholds for primary occlusal caries, primary proximal caries, and existing restorations: findings from the National Dental Practice-Based Research Network. J Dent. 2013;41:718–25.
Mjor IA, Shen C, Eliasson ST, Richter S. Placement and replacement of restorations in general dental practice in Iceland. Oper Dent. 2002;27:117–23.
Casagrande L, Laske M, Bronkhorst EM, Huysmans M, Opdam NJM. Repair may increase survival of direct posterior restorations—a practice based study. J Dent. 2017;64:30–6.
Opdam NJ, Bronkhorst EM, Loomans BA, Huysmans MC. Longevity of repaired restorations: a practice based study. J Dent. 2012;40:829–35.
Kanzow P, Wiegand A. Retrospective analysis on the repair vs. replacement of composite restorations. Dent Mater. 2020;36:108–18.
van de Sande FH, Moraes RR, Elias RV, Montagner AF, Rodolpho PA, Demarco FF, Cenci MS. Is composite repair suitable for anterior restorations? A long-term practice-based clinical study. Clin Oral Investig. 2019;23:2795–803.
Wilson N, Lynch CD, Brunton PA, Hickel R, Meyer-Lueckel H, Gurgan S, Pallesen U, Shearer AC, Tarle Z, Cotti E, Vanherle G, Opdam N. Criteria for the replacement of restorations: Academy of Operative Dentistry European Section. Oper Dent. 2016;41:S48–57.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Demarco, F.F., Chisini, L.A., Correa, M.B., Cenci, M.S., de Moraes, R.R. (2022). Longevity of Resin Composite Restorations. In: Oliveira, D. (eds) Color Science and Shade Selection in Operative Dentistry. Springer, Cham. https://doi.org/10.1007/978-3-030-99173-9_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-99173-9_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-99172-2
Online ISBN: 978-3-030-99173-9
eBook Packages: MedicineMedicine (R0)