Abstract
The aim of this study was to evaluate the fracture frequency and longevity of fractured class IV resin composite (RC), polyacid-modified resin composite (compomer; PMRC), and resin-modified glass ionomer cement (RMGIC) restorations in a longitudinal long-term follow-up. Eighty-five class IV RC (43: Pekafil), PMRC (24: Dyract (D), Hytac (H)), and RMGIC (18: Fuji II LC (F), Photac Fil (P)) restorations were placed in ongoing longitudinal follow-ups in 45 patients (mean age 54.5 years). The restorations were evaluated during 14 years by slightly modified USPHS criteria at yearly recalls especially for their fracture behavior. For all restorations, 36.5% were fractured, with a Kaplan–Meier (KM) estimate of 8.8 years (standard error (SE) 0.5, confidence interval (CI) 7.9–9.8). The number of fractures per material was 11 RC (25.6%; KM 9.9 years, CI 8.7–11.0), 13 PMRC (54.2%; D 66.6%; H 50.0%; KM 7.5 years, CI 5.8–9.2), and seven RMGIC (36.5%; F 22.2%, P 71.4%; KM 6.9 years, CI 7.9–9.8). Significant differences were seen between RC and PMRC (p = 0.043). A significant higher fracture rate was observed in teeth 12 + 22 compared to teeth 11 + 21. No significant differences were observed between male and female patients. Restorations in bruxing patients (45) showed 22 fractures (KM 8 years; CI 6.9–9.3) and in non-bruxing patients (39) nine fractures (KM 9.9 years, CI 8.7–11.1; p = 0.017). With regard to the longevity of the replaced failed restorations, for RC, the mean age was 4.5 years; for PMRC, 4.3 years; and for RMGIC, 3.3 years. It can be concluded that fracture was the main reason for failure of class IV restorations. An improved longevity was observed for class IV restorations compared to those presented in earlier studies. RC restorations showed the lowest failure frequency and the highest longevity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esthetic restorative materials have to simulate the natural tooth in color, texture, and translucency and should have adequate strength, wear, and sealing characteristics. Resin composites (RC) and conventional glass ionomer cements (GIC) have been the materials of choice for restoring anterior cavities since the early 1970s [6, 29]. During the early 1990s, new hybrid restorative materials, composed of elements of GIC and RC, were introduced. In the resin-modified glass ionomer cements (RMGIC), the addition of light- and/or self-curing resin components improved conventional glass ionomer cements by higher resistance to early moisture contact and desiccation and improved mechanical properties but with similar fluoride release [8, 17, 28]. Polyacid-modified resin composites (PMRC), commonly termed as compomers, contained modified GIC filler particles and methacrylate-based monomers containing carboxylate groups, which enabled a slow rate acid–base reaction to take place in the presence of water after free radical polymerization [5, 8]. They were introduced with some of the first marketed self-etching primers which infiltrated the demineralized tooth tissues with formation of a thin hybrid layer. The dissimilar fluoride release and mechanical and adhesive properties of these restorative materials may result in differences in durability.
Longevity of anterior restorations varied in earlier studies depending on restorative material and cavity class [4, 7, 9, 27]. Lucarotti et al. [16] reported that involvement of the incisal angle in incisors and canine teeth resulted in an associated reduction in median survival time. However, limited class evidence has been published concerning the longevity of the highly stressed class IV restorations. In contrast to class III and V restorations, loss of material has been reported as the major mode of failure [2, 10, 15, 25]. No evidence has been reported for the newer hybrid restorative materials. The hypothesis tested was that newer hybrid restoratives showed equal clinical fracture frequency in class IV cavities as resin composites. The aim of this study was to evaluate the fracture frequency of class IV restorations performed with different esthetic restorative systems in a prospective long time follow-up.
Materials and methods
In longitudinal follow-ups of anterior restorations, 85 class IV restorations were placed between 1992 and 1997 with three anterior restorative materials: resin composite, polyacid-modified resin composite and resin-modified glass ionomer cement [5, 9]. Every patient in need of a class IV restoration during the study period was included and none was excluded. The participating dentists did not receive special operative training at the start of the study. The study was approved by the Regional Research Ethics Committee at the medical faculty. The restorations were placed in 45 patients, 23 women and 22 men, with mean age of 54.5 years (range 33–82) at the time of placement. The majority of the restorations were placed in the maxilla—38 in teeth 11 + 21 (RC 24, PMRC 12, RMGIC two), 38 in teeth 12 + 22 (RC 14, PMRC ten, RMGIC 14), and nine restorations in teeth 32–42 (RC five, PMRC two, RMGIC two). The materials investigated were: (1) a hybrid light-cured small filler particle resin composite Pekafil PLT (P; Bayer AG, Leverkussen, Germany; batch 1157G and 2068H, N = 43) placed in combination with Gluma or the Gluma 2000 system (Bayer AG) after total etching with phosphoric acid (N = 25) and oxalic acid (N = 18) respectively; (2) two one-paste PMRC: Dyract (D; DeTrey/Dentsply, Konstanz, Germany; N = 14) placed in combination with the PENTA containing self-etching primer PSA, and Hytac (H) placed in combination with the methacrylated phosphoric acid containing self-etching system OSB (ESPE, Seefeld, Germany; batch 29243, 30825; N = 10); (3) two RMGIC: a hand-mixed Fuji II LC (F; GC Corporation, Tokyo, Japan; batch 140661, 290261; N = 9) and a capsulated Photac Fil Quick (P), RMGIC (ESPE, Seefeld, Germany; batch 29243, 29550; N = 9) applied after cavity conditioning with polyacrylic acid.
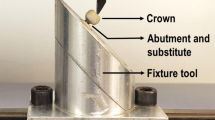
The restorative materials for the anterior cavities were randomly selected in the longitudinal studies and placed by three experienced dentists as part of their patient treatment. The class IV cavities of the PMRC and RMGIC were prepared with butt joint margins, while the enamel margins of the RC cavity were bevelled with a small 1–2-mm bevel. All cervical margins were placed in dentin. After color selection, the teeth were isolated with rubberdam or with cotton rolls and saliva suction device. The manufacturer’s directions were closely adhered to regarding cavity treatment and placement of the restorative materials. Adhesives were light-cured before placement of the restorative material. The RC cavities were filled incrementally. Each 2-mm restoration layer was light-cured for 40 s with a well-controlled visible light curing unit (Luxor, ICI, Macclefield, England, UK). In none of the restorations, except for one RC restoration, a Ca(OH)2 base was placed. The restorations were finished with fine diamond or carbide finishing burs to remove gross excess, followed by the Enhance finishing system and strips (DeTrey/Dentsply). The PMRC cavities were wetted for 15 s with PSA or OBS, after which the excess and solvent were removed by a gentle stream of air followed by a light cure of 20 s. A second layer of primer was applied equally. The PMRC materials were placed incrementally and each layer was light-cured for 40 s. The RMGICs were placed in bulk after cavity conditioning with the manufacturer’s polyacrylic acid for 15–20 s and light-cured for 40 s from both buccal and palatinal sides. In case of observed fracture of class IV restorations, and if indicated, the restoration was replaced by new class IV restorations of the same restorative material as the failed one.
Evaluation
All class IV restorations were evaluated yearly on occurrence of partial or total fracture during the follow-up with the last recall period during 2006, securing a minimum observation period of 8 years and the longest one of 14 years. The parameters were evaluated yearly with slightly modified USPHS criteria [12, 13]. The evaluations were performed by the calibrated operators and at regular intervals independent by other calibrated dentists followed by discussions in case of disagreement.
Statistical analysis
Data were processed in Statistical Package for the Social Sciences (SPSS, version 15.0). The characteristics of the restorations were described by descriptive statistics. Means and medians for survival times were tested with log rank and Breslow test. Kaplan–Meier (KM) was used to describe survival functions. The level of significance was set at p < 0.05.
Results
Ten restorations (four PMRC, three RC, three RMGIC), not evaluated during the whole period due to moving or death of the patients but still in place at the last registration before the drop out recall, were included in the survival analysis. All other restorations were evaluated yearly during the whole follow-up, at least 8 years and up to 14 years. Any restoration which had sustained a large chip fracture or bulk fracture was recorded as failure. Smaller chips not disturbing the function of the restoration were polished if necessary. No restoration was replaced because of non-acceptable color and marginal discoloration. Six class IV restorations (four RC, two PMRC) were repaired because of secondary cervical caries. Because the small size of the repairs, the risk for fracture was estimated as very low, and these restorations were continued to be evaluated in the follow-up. Three patients reported slight symptoms during biting forces during the first weeks after placement. None of the other participating patients reported post-operative sensitivity symptoms at the recalls.
During the follow-up, a total of 31 fractures (35.3%) were observed (Fig. 1). The number of fractures per material was 11 of 43 restorations (25.6%) for RC, with a Kaplan–Meier estimate of 9.9 years (standard error (SE) 0.6, confidence interval 8.7–11.0); for PMRC, 13 of 24 restorations (54.2%; D 66.6%; H 50.0%), with a Kaplan–Meier estimate of 7.5 years (SE 0.9, confidence interval 5.8–9.2); and for RMGIC, seven of 18 restorations (36.5%; F 22.2%, P 71.4%), with a Kaplan–Meier estimate of 6.9 years (SE 0.9, confidence interval 7.9–9.8). For all restorations, 36.5% were fractured, with a Kaplan–Meier estimate of 8.8 years (SE 0.5, confidence interval 7.9–9.8). In the RC restorations, five fractures were observed in the oxalic acid (27.8%) and six in the phosphoric acid-etched cavities (24%). Significant differences were seen between RC and PMRC (p = 0.043). A significant higher fracture rate was observed in teeth 12 + 22 compared to teeth 11 and 21. No significant differences were observed between male and female patients.
Longevity of all restorations (fractured and non-fractured) was as follows: for RC, the mean was 9.1 years, median of 10 years; for PMRC, the mean was 6.7 years, median of 5 years; and for RMGIC, the mean was 6.1 years, median of 5 years. Longevity of the replaced failed restorations was as follows: for RC, the mean was 4.5 years, median of 3.5 years; for PMRC, the mean was 4.3 years, median of 3.5 years; and for RMGIC, the mean was 3.3 years, median of 3 years.
Restorations placed in bruxing patients (45) versus non-bruxing patients (39) showed 22 and nine fractures, respectively, with a Kaplan–Meier estimate for bruxing patients of 8 years (SE 0.66, confidence interval 6.9–9.3) and for non-bruxing patients an estimate of 9.9 years (SE 0.61, confidence interval 8.7–11.1; p = 0.017; Fig. 2).
Twenty-three of the fractured restorations were replaced by a new restoration. Thirteen of these fractured again during the follow-up with a mean of 2.9 years (range 1–8), median of 3 years. Ten of the 13 (77%) second-time fractured restorations were found in bruxing patients.
Discussion
General practitioners spend a significant part of their time to replace failed restorations. They have quite often little evidence for their choice of materials, placement technique, or when to change to new materials or techniques. A variety of new restorative materials and techniques have been introduced in operative dentistry during the last decades. New anterior adhesive restorations did show better durability compared to earlier ones in a few clinical follow-ups [4, 7, 9]. Despite an expected lower longevity of class IV restorations compared to class III and class V restorations, there is little evidence for their durability. Not at least because many studies did not differentiate between cavity classes [4, 12–14, 30].
In cross-sectional studies, frequently published in the literature after a model by Mjör [19], the longevity of replaced class IV restorations varied dramatically. Burke et al. [3] reported a mean longevity of 3.9 and 3.7 years for replaced class IV RC and GIC restorations, respectively, as recorded by vocational dental practitioners and their trainers in the UK. Browning and Dennison [2] showed that 36% of the replaced class IV restorations failed within 3 years and 50% within 5 years, as shown in questionnaires reported by general practitioners in the USA. Jokstad et al. [14] observed a median age of 7 years recorded by Swedish private practitioners. On the other hand, Smales and Hawthrone observed in a retrospective study in Australia a median age of 12.7 years [23]. They used casebook records of 20 private dentists which may decrease the reliability of the survival ages. In the present study, we reported a median longevity of replaced fractured class IV restorations of 3.5 years for RC and PMRC and 3 years for RMGIC.
Longitudinal evaluations will give more reliable durability figures by recording all placed restorations and not only replaced ones as in cross-sectional studies. However, the few longitudinal follow-ups of class IV RC restorations showed also a wide variation in longevity figures. Smales [21] reported a median age of 9.8 years for class III and 4.1 years for class IV RC restorations performed by staff members and students using a low viscosity enamel bonding resin. Duke et al. [10] showed after 1 year failure rates between 7% and 12.2% for three different RC placement techniques. Tyas [25] showed a cumulative failure rate of 26% for four RC after 3 years. Two microfilled resin composite materials showed far higher failure rates (40% and 42%) compared to the hybrid materials (5% and 9%). Smales and Gerke reported a 43% failure rate after 5 years [22]. A high failure rate of class IV restorations was also shown by Miller et al., however, based on very few restorations [18]. These figures can be compared with the present study observing a 35.3% fracture rate for all and 27.3% for RC restorations after up to 14 years.
The present and other published class IV RC studies indicate clearly that problems with loss of resin composite restorations due to fracture present the profession with a great challenge.
Most of these studies used non-optimal dentin-bonding systems based on hydrophobic monomers. To our knowledge, no studies have been published evaluating the use of hydrophilic adhesive restorative systems in Class IV cavities. It is reasonable to believe that improvement in the retention of class IV restorations can be achieved with improvements in bonding and/or preparation techniques. The RC restorations showed a superior longevity compared to the other studied restoratives. Only the F RMGIC showed a comparable relative fracture frequency, however, unfortunately based on few restorations. Therefore, we reported the materials in each material group combined. In the present study, a hydrophilic bonding system was used in combination with the total etch technique for the RC. Eighty-two percent of the originally class IV RC restorations survived more than 10 years, which is a far higher survival rate as reported earlier. The results can be compared with those of Ferrari et al., where 7.5% of class IV resin composite restorations (Pekafil) needed replacement at 5 years [12].
Failure of class IV restorations due to loss of material or fracture is probably directly attributed to increased wear and incisal stresses. Incisal edge fractures contiguous class III restorations in anterior teeth were more frequently observed in bruxing patients [5, 7, 9]. The class IV restoration is subjected to great forces from opposing teeth, and the stress caused by parafunctional habits may further compromise the restoration [21]. It was therefore not surprising that we found significantly lower longevity of class IV restorations in bruxing patients versus non-bruxing ones.
Adhesive techniques have led away from the classic principles of cavity preparation to a more tissue-saving way of treatment. In earlier Cl IV RC investigations, pins and/or a lingual lock could be placed to aid retention [25]. The retention in our study was obtained by adhesive bond to the short enamel bevel and the inner dentin cavity walls. The RMGIC and PMRC were placed in butt joint cavities. Various RC preparation techniques have been recommended for anterior cavities such as butt joint margins, feather-edged margins, short and long bevel preparation, and chamfer preparation. No clinical evidence can be found in the literature for these different cavity margins in class IV cavities [1]. Longer enamel bevels have been suggested to give better color match and retention. However, Eid showed no significant differences in shear bond strength between a 2-mm 45° bevel, a 2-mm circumferential chamfer, and a stair step chamfer [11]. He indicated that it was not the adhesion between enamel and composite that failed, rather the cohesive strength within the restorative material.
No reports have been published about the use of PMRC and RMGIC in the class IV cavity. Despite the relative low number of PMRC and RMGIC restorations evaluated, better performance of RC restorations was clear. The hypothesis was therefore rejected. The higher failure rate of the PMRC restorations may be partly due to the non-optimal bonding of the materials self-etching primer to the enamel tooth tissues as observed earlier [7, 8]. At the introduction of the PMRC on the market, no phosphoric etching was recommended for enamel, and the non-bevelled PMRC cavities were treated only with the self-etching primers of the restorative systems which were not aggressive enough to perform suitable enamel etch patterns. A total etch with phosphoric acid was later recommended. It has been suggested that the fracture risk can be decreased by using materials with improved fracture toughness [15, 25]. Tyas [25] showed that microfilled RC had a faster and higher loss frequency than small particle hybrid resin composites. Lambrechts et al. [15] reported that 17 of 22 class IV fractures were found in microfine RC. Both the RC and PMRC in the present study can be defined as small filler particle materials. No large difference was observed between the two PMRC, but the difference between the two RMGIC materials was surprising. P showed the highest and F the lowest fracture rate. Improved retention of F to tooth tissues may be partly explained by the materials excellent adaptation as shown earlier by SEM replica technique [8].
Secondary caries have been indicated as the main reason of placement and replacement of most types of restorations [24]. The class IV restoration, however, seems to be an exception as indicated by the low rate of secondary caries observed in this and many other class IV studies [2, 20, 25, 26]. The short longevity reported of class IV restorations may partially explain their low caries activity.
Conclusion
Fracture was the main reason for failure of class IV restorations. An improved longevity was observed compared to earlier studies. Resin composites showed the lowest failure frequency and the highest longevity.
References
Black J, Retief D, Lemons J (1983) Effect of cavity design on retention of class IV composite resin restorations. JADA 107:42–46
Browning WD, Dennison JB (1996) A survey of failure modes in composite resin restorations. Oper Dent 21:160–166
Burke FJ, Cheung SW, Mjör IA, Wilson NHF (1999) Restoration longevity and analysis of reasons for the placement and replacement of restorations provided by vocational dental practitioners and their trainers in the United Kingdom. Quintessence Int 30:234–242
Dijken van JWV (1987). Conventional, microfilled and hybrid composite resins: laboratory and class evaluations. Thesis, Umeå University, Sweden
van Dijken JWV (1999) Longevity of new hybrid restorative materials in class III cavities. Eur J Oral Sci 107:115–219
van Dijken JWV (1992) Three year evaluation of effects of surface conditioning on bonding of glass ionomer cement in cervical abrasion lesions. A three year class evaluation. Scand J Dent Res 100:133–135
van Dijken JWV (2001) Durability of new restorative materials in class III cavities. J Adhes Dent 3:65–70
van Dijken JWV, Hörstedt P (1997) In vivo enamel adaptation of a polyacid-modified resin composite (compomer) and a resin-modified glass ionomer cement. Clin Oral Invest 1:185–190
van Dijken JWV, Olofsson AL, Holm C (1999) Five year evaluation of class III composite resin restorations in cavities pre-treated with an oxalic- or a phosphoric acid conditioner. J Oral Rehabil 26:364–371
Duke ES, Robbins JW, Trevino D (1994) The clinical performance of a new adhesive resin system in class V and IV restorations. Compend Contin Educ Dent 15:852–862
Eid H (2002) Retention of composite resin restorations in class IV preparations. J Clin Pediatr Dent 26:251–256
Ferrari M, Bertelli E, Finger W (1993) A 5-year report on an enamel-dentin bonding agent and microfilled resin system. Quintessence Int 24:735–741
Geitel B, Kwiatkowski R, Zimmer S, Barthel CR, Roulet J-F, Jahn K-R (2004) Clinically controlled study on the quality of class III, IV, and V composite restorations after two years. J Adhes Dent 6:247–253
Jokstad A, Mjör IA, Qvist V (1994) The age of restorations in situ. Acta Odontol Scand 52:234–242
Lambrecht P, Ameye C, VanHerle G (1982) Conventional and microfilled composite resins. Part II. Chip fractures. J Prosthet Dent 48:527–537
Lucarotti PSK, Holder RL, Burke FJT (2005) Outcome of direct restorations placed within the general dental services in England and Wales (Part 1): variation by type of restoration and re-intervention. J Dent 33:805–815
Mathis RS, Ferracane JL (1989) Properties of a glass ionomer/resin composite hybrid material. Dent Mater 5:355–358
Millar BJ, Robinson PB, Inglis AT (1997) Clinical evaluation of an anterior hybrid composite resin over 8 years. Br Dent J 182:26–30
Mjör IA (1981) Placement and replacement of restorations. Oper Dent 6:49–54
Qvist V, Ström C (1993) 11-year assessment of class III resin restorations completed with two restorative procedures. Acta Odontol Scand 51:253–262
Smales RJ (1991) Effects of enamel-bonding, type of restoration, patient age and operator on the longevity of an anterior composite resin. Am J Dent 4:130–133
Smales RJ, Gerke DC (1992) Clinical evaluation of four anterior composite resins over five years. Dent Mater 8:246–51
Smales RJ, Hawthorne WS (1996) Long-term survival and cost-effectiveness of five dental restorative materials used in various classes of cavity preparations. Int Dent J 46:126–130
Sunnegårdh-Grönberg K, van Dijken JWV, Funegård U, Lindberg A, Nilsson M (2009) Selection of dental materials and longevity of replaced restorations in Public Dental Health clinics in northern Sweden. J Dent doi:10.1016/j.jdent.2009.04.010
Tyas MJ (1990) Correlation between fracture properties and clinical performance of composite resins in class IV cavities. Aust Dent J 35:46–49
Ulvestad H (1978) A 5-year evaluation of semipermanent composite resin crowns. Scand J Dent Res 86:163–168
van Noort R, Davis LG (1993) A prospective study of the survival of chemically activated anterior resin composite restorations in general dental practice: 5-year results. J Dent 21:209–215
Wilson AD (1990) Resin-modified glass ionomer cements. Int J Prosthodont 3:425–429
Wilson AD, Kent BE (1971) The glass ionomer cement, a new translucent cement for dentistry. J Appl Chem Biotechnol 21:313–319
Wilson NHF, Burke FJT, Mjör IA (1997) Reasons for placement and replacement of restorations of direct restorative materials by a selected group of practitioners in the United Kingdom. Quintessence Int 28:245–248
Acknowledgments
The support from the County Council of Västerbotten and the Swedish National Board of Welfare is gratefully acknowledged.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Dijken, J.W.V., Pallesen, U. Fracture frequency and longevity of fractured resin composite, polyacid-modified resin composite, and resin-modified glass ionomer cement class IV restorations: an up to 14 years of follow-up. Clin Oral Invest 14, 217–222 (2010). https://doi.org/10.1007/s00784-009-0287-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-009-0287-z