Abstract
The MAPK/ERK/p38 are signal transduction pathways that couple intracellular responses to the external stimuli. Contrary to ERK protein which is part of the survival route, presence of p38 could have an impact on cell injury. Tolerance induced by ischemic preconditioning (IPC) is a phenomenon of tissue adaptation, which results in increased tolerance to lethal ischemia–reperfusion injury (IRI). Paper describes changes in MAPK protein pathways after brain IPC. Ischemia was induced by 4-vessels occlusion and rats were preconditioned by sub-lethal ischemia. Western blot and immunohistochemistry identified ERK/p38 proteins in injured areas. The highest level of the pERK was detected at 24 h in IPC groups. A contrary pattern of MAPK/p38 activation was observed in this group, where the lowest level of p38 was displayed at 24 h after ischemia. This suggests that the MAPK signal transduction might have a potential role in tissues response subjected to IRI and in the phenomenon of tolerance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischemia/reperfusion injury (IRI) is a third leading cause of death worldwide [1–4]. An enormous interest has therefore arisen to explore mechanisms capable of limiting brain damage [5]. IRI refers to the tissue damage caused when blood supply returns to tissue after a period of ischemia [3, 7, 8].
The ethiopathology of the IRI is complex. During ischemia, cells undergo rapid changes which lead to perturbations in signaling pathways and surface molecule expression [8–12].
Strategies interfering with programmed cell death (apoptosis) have been investigated in order to reduce cell death and thus, protect the graft from cell loss [13]. Multiple therapeutic trials are currently being conducted in animal models against brain damage, with recent breakthroughs [14] in rats, in rabbits, and in humans [8, 9].
Depending on stimulus intensity, that is not necessarily hypoxic or ischemic in nature, it can induce changes ranging to activation of endogenous protective mechanism known as ischemic tolerance. The extensively investigated ischemic preconditioning (IPC) is a powerful innate protection induced by local brief ischemic episodes that initiates tolerance to a subsequent, more sustained ischemia [1–5, 10–12, 14]. Previous results [1–4, 10–12] showed that, for full expression of tolerance, repeated stress is essential [14].
Within the last decade there has been an explosion of research documenting the roles of a variety of signaling molecules in IRI and IPC [5, 12, 14]. Mitogen-activated protein kinases (MAPKs) are a family of related serine/threonine kinases [15–17] and signal transduction mediators, that regulate a diverse array of cellular functions [17–19]. These MAPKs consist of four highly conserved subfamilies: the extracellular signal regulated kinases (ERK1/2, also referred to as p44/p42); the jun-NH2-terminal kinases 1/2 (JNK1/2, also designated as stress activated protein kinases or p54/p46); p38 MAPK; and ERK5 [5, 16–21]. ERKs regulate multiple functions, including cell growth, proliferation, differentiation and apoptosis [16, 19, 20, 22]. This pathway is activated by growth factors, oxidative stress, increases of intracellular Ca2 + levels and glutamate receptor stimulation, factors which are activated by IRI [17, 23]. MAPK/p38 (also known as stress-activated protein kinase2 family) [15, 23] mainly function as mediators of cellular stresses such as inflammation and apoptosis. It has been reported that the expression of ERK1/2 mRNA and protein is relatively high in the rat brain, especially in the hippocampus and nucleus accumbens [15, 16, 20]. Patophysiologically stressful stimuli, including seizure induction, ischemic insult, trauma, visceral pain and electroconvulsive shock have also been shown to rapidly activate MAPKs in various brain regions [15, 19, 20, 23, 27, 28]. It was detected, following focal cerebral ischemia in the rat, activation of both ERK and p38 MAPK, up to 24 h after ischemia [20]. In addition, it was reported that pERK immunoreactivity was changed in the gerbil hippocampus after transient forebrain ischemia [16]. Recent studies have shown that MEK/ERK-mediated signals play a major role in ischemia-induced apoptosis through regulation of Bax/Bcl-2/Bcl-xL expression [24]. A dual role of ERK in the regulation of survival and death via AIF (apoptosis inducting factor) has been also demonstrated [25, 26]. Phosphorylation of p38 MAPK during ischemia has been reported to occur in the tissues of rats, dogs and pigs [5, 6]. In regard to p38 MAPK, data agree on protection by p38 inhibition against focal ischemia induced infarct, neurological deficit and expression of inflammatory cytokines [15, 20]. Although many studies have been focused on determining the role of the MAPK/ERK and p38 cascades in different tissues [5, 6, 16], there are contradictory information about changes in pERK1/2 expression in the brains of rats during following ischemic preconditioning (IPC). Preconditioning, due to its unique mode of action affords an opportunity to examine protective signaling mechanism. The present study was designed to characterize the precise roles of p38 and pERK1/2 in IPC by using an in vivo model of global brain ischemia in rats.
Experimental Procedure
Ischemia–Reperfusion and Ischemic Preconditioning (IPC)
Animal studies were performed under a protocol approved by the State Veterinary and Food Department of the Slovak Republic. Adult male Wistar rats (mean body weight 320 g, total n = 60) used for the experiments were housed in a menagerie under standard conditions with a temperature of 22 ± 2 °C, and periodical variation in daylight at 12 h intervals. Food and water were provided ad libitum. Global forebrain ischemia was induced by the standard 4-vessel occlusion model [11, 29, 30]. Briefly on day 1, both vertebral arteries were irreversibly occluded for 10 min by thermo coagulation through the alar foramina after anesthesia with 2.5 % halothane in a mixture of oxygen/nitrous oxide (30/70 %). There was no visible influence on the animals. On day 2, both common carotid arteries were occluded for 15 min by small atraumatic clips under anesthesia with 2.5 % halothane in a mixture of oxygen/nitrous oxide (30/70 %). Two minutes before carotid occlusion, the halothane was removed from the mixture. Normothermic conditions (37 °C) were monitored by a microthermistor placed in the ear. Temperature was maintained using a homoeothermic blanket. Sham control animals (C, n = 5) were prepared in the same way without carotid occlusion. The rats then underwent 15 min ischemia (Isch, n = 5), followed by 1, 3 and 24 h of reperfusion (from IR-15 Isch to IR-72 h, respectively, each group n = 5). Criteria for forebrain ischemia were: loss of the righting reflex, mydriasis, and paw extension. The rats that became unresponsive and lost the righting reflex during bilateral carotid artery occlusion and showed no seizures during and after ischemia were used for the experiment. Only such animals are considered to have met the criteria for adequate ischemia [10]. All rats used reached the criteria for global forebrain ischemia and were divided into groups for the experiments mentioned above in the same way (C, IPC-15 Isch, IPC-1 h, IPC-3 h, IPC-24 h and IPC-72 h, in each group n = 5). IPC was induced by 5 min of sub-lethal ischemia followed by 2 days of reperfusion. The rats then underwent lethal ischemia for 15 min as above, followed by 1, 3, 24 or 72 h of reperfusion. After ischemia and particular time of reperfusion, animals were sacrificed by decapitation and brains were dissected and processed immediately. Control animals for both the naive ischemia and the preconditioned ischemia groups underwent the same procedure except for carotid occlusion.
Preparation of Whole Forebrain Homogenates
Rat brains were homogenized in 10 mmol/l Hepes/KOH pH 7.4, 0.32 mol/l sucrose, 0.1 mmol/l phenylmethylsulfonyl fluoride and protease inhibitor cocktail solution (Roche). The homogenate was centrifuged for 10 min at 1.500 g. The pellet was discarded and the supernatant was centrifuged for 45 min at 100,000 g. The final pellet was resuspended in 10 mmol/l Hepes/KOH pH 7.4, 0.32 mol/l sucrose and stored at −80 °C until use.
Western Blot Analysis (WB)
Brains from sham control, ischemic and preischemic animals were homogenized and resolved by sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE). After Western blotting (Trans blot SD semi-dry transfer cell, Bio-rad) blots on nitrocellulose membrane were probed with rat polyclonal antibodies against p38 (sc-7149, 1:300, Santa Cruz Biotechnology) as well as with mouse monoclonal antibodies against pERK1/2 (sc-7383, 1:500, Santa Cruz Biotechnology) at room temperature for 3 h. After being washed with 0.05% phosphate-buffered saline (PBS)-Tween, the membranes were incubated with a goat anti-mouse (pERK1/2; sc-2005, 1:000, Santa Cruz Biotechnology) and goat anti-rabbit (sc-2040, 1:1,000, Santa Cruz Biotechnology) secondary antibodies conjugated with horseradish peroxidase for 1 h and washed again with PBS-Tween. Finally, the membranes were developed with a SuperSignal West Pico Chemiluminescence Substrate (ECL system from Pierce, #34080) and detected by Molecular Imager Gel Doc XR System (Bio-Rad) as described in [31]. We analyzed three animals per experimental group. To reduce differences among animals, sample loading on SDS-PAGE and variability due to ECL detection, Western blots were performed for each reperfusion time point per animal at least four times.
Protein Determination
Protein was measured by using bovine serum albumin as a standard as described in [31].
Immunohistochemistry
The animals (n = 3 per group) were anesthetized with 2.5 % halothane in a mixture of oxygen/nitrous oxide (30/70 %) and perfused transcardially with 0.1 M phosphate-buffered saline (PBS, pH 7.4) followed by 4 % paraformaldehyde in 0.1 M PBS (pH 7.4). The brains were removed and postfixed with the same solution for 24 h at 4 °C. The tissues were cryoprotected by infiltration with 30 % sucrose for the next 24 h at 4 °C. The brain tissues were then frozen and sectioned with a cryostat at 30 μm, and the sections were mounted into silanised glass. Sections were permeabilized with 0.1 % Triton X-100, preblocked with 10 % BSA for 60 min. Primary antibodies used are mentioned previously. The tissue sections were incubated O/N at 4 °C in primary antibody diluted in the blocking solution. Detection was performed using goat-anti-mouse FITC (sc-2010, Santa Cruz Biotechnology) and goat-anti-rabbit- TR (sc-2780, Santa Cruz Biotechnology)-conjugated secondary antibodies. Sections were mounted in Vectashield mounting medium containing 4′,6-diamidino-2-phenylindole (CA 94010, Vector Laboratories) according to standard protocols. No immunoreactivity was detected in the absence of the primary antibodies.
Fluoro-Jade B Staining
Fluoro-Jade B was used as a marker of neurons undergoing degeneration. The sections mounted on the silanized glass were heated at 50 °C for at least half an hour before staining. The slides were immersed in absolute alcohol for 3 min, for 1 min in 70 % alcohol and for 1 min in distilled water. Then the slides were transferred to the solution of 0.06 % potassium permanganate for 15 min and rinsed in distilled water for 2 min. After 30 min in the staining solution, 3 × 1 min rinses in distilled water followed. The slides were dried at room temperature, cleared by xylene and cover slipped with Fluoromont according to standard protocols.
Data Analysis
Images of p38, pERK and Fluoro-Jade B immunoreactivity in the PtA and CA1 region of rat brain of each animal were captured with an OLYMPUS fluoview FV10i confocal microscope. The brightness and contrast of each image file was uniformly calibrated using Adobe Photoshop version 2.4.1, followed by analysis using Image-Pro Plus 6.0 software. Values of background staining were obtained and subtracted from the immunoreactive intensities. All results were presented as mean ± SEM ANOVA and Student–Neuman–Keuls tests were used when control, IR and IPC groups were compared. The results from Western blot analysis were normalized to control which represents 100 %. A value of p < 0.05 was considered to be statistically significant.
Results
Acute Histologic Damage in the CA1 Sector of the Hippocampus After IRI and IPC
Fluoro-Jade B
As a sign of neuronal degeneration tissue slices were stained with Fluoro-Jade B at 72 h after IRI and at 72 h after IPC. 90 times higher amount of positive degenerating neurons was found in the hippocampus (47.7 ± 5.3; p < 0.001) in the IR group in comparison to the control animals, located mostly in the pyramidal cell layer of the CA1 subfield (Fig. 1b, b*). In extrahippocampal regions (layers III–VI of the cortex) damage appeared to be less detected in the density of labeled neurons. In contrast, the distribution of degenerating neurons in the IPC group was less in the CA1 sector (Fig. 1c, c*) compared to IR group. The number of Fluoro-Jade B+ cells was 58.6 times higher (19.3 ± 1.3; p < 0.01) in comparison to the control groups, whereas there was no positive labeling in control animals. We demonstrated that IPC initiates adaptation of brain tissue to lethal injury by the significant decrease of density FluoroJade-B+ neurons at 72 h after IPC to 246.7 ± 4.1 % (p < 0.01) in comparison to its IR group (Fig. 4), which suggests survival of vulnerable neurons. Fifteen minutes of ischemia with following 72 h reperfusion is able to kill roughly 75–80 % CA1 neurons in hippocampus (Fig. 1b) with minimal changes in the cortex. As it can be seen in Fig. 1c, surprisingly, preconditioning, though effective in CA1, is able to decrease the number of Fluoro Jade B positive neurons in CA1 region of hippocampus six times and completely prevent neurodegeneration in the cortex (Figs. 2, 3).
Representative fluorescence micrographs show Fluoro-Jade B-labeled cells in the CA1 area of hippocampus after IR and IPC. Control (a), IR- 72 h rep (b), IPC-72 h rep (c), detail of IR-72 h rep (b*) and detail of IPC-72 h rep (c*). The arrow heads indicate numbers of fluorescent cells in the CA1 area and arrows show morphological changed neurons. The line shows the CA1 area of the hippocampus. CC corpus callosum. Bar 50 μm
Immunohistochemistry for p38 in the PtA (parietal association cortex; [46]) area of rat forebrain in IR and IPC groups. C (a′), IR-15 Isch (b′), IR-1 h rep (c′), IR-3 h rep (d′), IR-24 h rep (e′); IPC-15 Isch (f′), IPC-1 h rep (g′), IPC-3 h rep (h′) and IPC-24 h rep (i′). Arrows indicate cytoplasmatic labeling of p38 positive neuronal cells. Bar 50 μm
Immunohistochemistry for pERK1/2 in the PtA area of rat forebrain in IR and IPC groups. C (a″), IR-15 Isch (b″), IR-1 h rep (c″), IR-3 h rep (d″), IR-24 h rep (e″); IPC-15 Isch (f″), IPC-1 h rep (g″), IPC-3 h rep (h″) and IPC-24 h rep (i″). Arrows indicate cytoplasmatic labeling of pERK positive neuronal cells. Bar 50 μm
Fluoro-Jade B positive neuronal cells in the CA1 area of rat hippocampus in control and after 72 h reperfusion without IPC and 72 h reperfusion with IPC. Comparison between control groups 15 min ischemia following 72 h reperfusion or 5 min preischemia following 15 min ischemia and 72 h reperfusion, respectively. Results are presented as mean ± SEM for n = 5, normalized to control levels. **p < 0.01 and ***p < 0.001 mean statistically significant different as compared to controls. ++ p < 0.01 signify statistically significant different between IR and IPC animals in the same time points
Neuronal Damage in the Cortical Neurons After IRI and IPC
We first analyze p38 and pERK1/2 proteins by Western blot analysis.
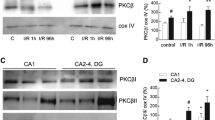
Western Blot
This analysis clearly detected the protein level in an injured area from sham-operated controls and from animals after IRI. In the IR group, the level of p38 protein in comparison to controls was not changed 15 min after ischemia (Fig. 5). The protein level of p38 increased in a time-dependent manner. We detected a non-statistically significant increase after 1 h of reperfusion with maximal level at 24 h after reperfusion (Fig. 5), however the changes in comparison to the controls were not statistically significant. IPC had a detectable influence on the protein level of p38 in the corresponding IRI period. IPC initiated an early response to the injury by the decrease of p38 already at 1 h of reperfusion, anyhow the alterations in comparison to the controls were not statistically significant. The expression level remained lower also at later reperfusion periods. After 24 h of reperfusion, the protein level reached 49 % (p < 0.05) in comparison to the controls. We ascertained a statistically significant decrease of p38 protein level to 53 % (p < 0.01) at 3 h after reperfusion when compared IR and IPC and to 36 % (p < 0.01) at 24 h after reperfusion when compared IR and IPC groups, respectively.
Protein levels of p38 in the cortex homogenates of rat brain after 15 min ischemia and 1, 3 and 24 h reperfusion with/without IPC. Comparison between control groups with lethal ischemia and 1, 3 and 24 h reperfusion and 5 min preischemia following 15 min ischemia and 1, 3 and 24 h reperfusion, respectively. Results are presented as mean ± SEM for n = 5, normalized to control levels. *p < 0.05 mean statistically significant different as compared to controls. + p < 0.05 and ++ p < 0.01 represent statistically significant different between IR and IPC animals in the same time points
In addition, we analyze expression of pERK protein in cerebral cortex of rat. IR-dependent change in pERK1/2 expression was found (Fig. 6). We examined differences between IR groups and IPC in the rat cortex. As shown in IR groups, the protein level of pERK1/2 (Fig. 6) decreased at 3 h after ischemia to 68 % (p < 0.01) in comparison to the controls with a non-significant increase at 24 h after reperfusion in comparison to the controls. On the other hand, we determinate that IPC group initiated statistically significant elevation of pERK1/2 at 3 h after ischemia to 138 % (p < 0.001) in comparison to the controls and to 147 % (p < 0.001) at 24 h after reperfusion in comparison to controls. An elevated level of pERK protein to 115 % (p < 0.05) at 15 min after reperfusion was also found when compared IR and IPC groups. At 1 h after reperfusion was the level of pERK protein elevated to 134 % (p < 0.01) when compared IR and IPC group, at 3 h after reperfusion to 158 % (p < 0.001) when compared IR and IPC groups and at 24 h after insult to 142 % (p < 0.001) when compared IR and IPC groups, respectively, as a possible sign of protection of IPC to tissue after injury.
Protein levels of pERK1/2 in the cortex homogenates of rat brain after 15 min ischemia and 1, 3 and 24 h reperfusion with/without IPC. Comparison between control groups with lethal ischemia and 1, 3 and 24 h reperfusion and 5 min preischemia following 15 min ischemia and 1, 3 and 24 h reperfusion, respectively. Results are presented as mean ± SEM for n = 5, normalized to control levels. **p < 0.01 and ***p < 0.001 mean statistically significant different as compared to controls. + p < 0.05 and +++ p < 0.001 stand for statistically significant different between IR and IPC animals in the same time points
Double-Staining Immunoanalysis
Fluorescent immunohistochemistry was applied to detect immunoreactive pERK1/2 and p38 in neuronal cells.
p38 Immunoreactivity
The cytoplasmic fluorescent immunoreactivity of p38 was detected in the fifth cortex layer of the rat in the control groups (Fig. 2a′). As shown in IR groups, the number of p38+ cells (Fig. 7) decreased at 15 min after lethal ischemia, thought the descent in comparison to the controls was not stastistically significant. At 1 h after reperfusion, we detected elevation of p38+ cells to 110 % (p < 0.001) in comparison to the controls, at 3 h after ischemia we shown increased number of p38+ cells to 116 % (p < 0.001) in comparison to the controls and at 24 h after reperfusion to 123 % (p < 0.001), respectively (Fig. 2b′–e′).
p38 positive cells in the cortex of rat brain in PtA area after 15 min ischemia and 1, 3 and 24 h reperfusion with/without IPC. Comparison between control groups with lethal ischemia and 1, 3, and 24 h reperfusion and 5 min preischemia following 15 min ischemia and 1, 3 and 24 h reperfusion, respectively. Results are presented as mean ± SEM for n = 5, normalized to control levels. ***p < 0.001 mean statistically significant different as compared to controls. +++ p < 0.001 signify statistically significant different between IR and IPC animals in the same time points
On the other hand (Fig. 2f′–i′), the IPC group induced significant reduction of immunoreactivity of p38 already 1 h after injury to 82 % (p < 0.001; Fig. 2g′) in comparison to controls at 3 h after reperfusion to 77 % (p < 0.001; Fig. 2h′) in comparison to controls, respectively. At 24 h after insult shown recovery of number of p38+ cells to 84 % (p < 0.01; Fig. 2i′) in comparison to the controls. When compared corresponding reperfusion periods after IRI and IPC, the p38 immunoreactivity was decreased, mainly in the fifth cortex layer, to 81 % (p < 0.001; Fig. 2g′) at 1 h after reperfusion and to 65 % (p < 0.001) at 3 h after lethal ischemia (Fig. 2h′). This pattern was sustained until 24 h after reperfusion to 63 % (p < 0.001; Fig. 2i′) which corresponds with results from WB analysis (Fig. 7).
pERK Immunoreactivity
In the IR group, the imunofluorescence of pERK+ cells in the fifth layer of the cortex was very low in comparison to that in the control groups. The immunoreactivity of pERK (Fig. 8) decreased at 15 min after ischemia, however the reduction in comparison to the controls was not statistically significant (Fig. 3b″). This pattern was observed until 24 h after ischemia in comparison to the controls (Figs. 3c″–e″, 8). Imunoreactivity of pERK labeled pyramidal neurons as we detected increased with reperfusion time (Fig. 3g″–i″) after short sub-lethal ischemia followed 15 min ischemia and 1, 3 and 24 h reperfusion. We detected a significant increase of pERK+ cells at 3 h after insult to 135 % (p < 0.001; Fig. 3h″) in comparison to the controls and at 24 h after insult to 147 % (p < 0.001; Fig. 3i″) in comparison to the control (Fig. 3a″). In comparison to IR and IPC groups (Fig. 8), we detected an increased number of pERK+ cells at 1 h after insult to 118 % (p < 0.01), at 3 h after reperfusion to 145 % (p < 0.001) and 24 h after insult to 148 % (p < 0.001) what might suggest that IPC initiates protective tissue response linked with increase of imunoreactive pERK.
pERK1/2 positive cells in the cortex homogenates of rat brain in PtA area after 15 min ischemia and 1, 3 and 24 h reperfusion with/without IPC. Comparison between control groups with lethal ischemia and 1, 3 and 24 h reperfusion and 5 min preischemia following 15 min ischemia and 1, 3 and 24 h reperfusion, respectively. Results are presented as mean ± SEM for n = 5, normalized to control levels. ***p < 0.001 mean statistically significant different as compared to controls. + p < 0.05 and +++ p < 0.001 represent statistically significant different between IR and IPC animals in the same time points
Discussion
Growing evidence showed that cerebral ischemia initiates cell death signaling pathways and parallels with selective postischemic vulnerability of the brain [3, 4, 10, 29, 32]. One of the main aims of this study was to ascertain how IRI and IPC would affect the neuronal cells and to characterize the precise roles of p38 and pERK1/2 in IPC by using an in vivo model of global brain ischemia in rats. Previous studies have reported that sub-lethal global ischemia protects against neuronal damage induced by a lethal insult and stimulates the activation of MAPK/ERK and MAPK/p38 kinases [17, 18, 33, 34]. It was demonstrated that ERK1/2 after ischemia might cause neuronal damage [35], however, it was also suggested that phosphorylation of ERK after ischemia might support neuronal survival [32, 36]. Thus, this study was designed to clarify if ERK and p38 activation is associated with neuronal protection or neuronal degeneration and/or death. First, we found that sub-lethal ischemia conferred neuroprotection in four vessel occlusion model of ischemia detecting decreased number and density of Fluoro-Jade B + neurons after 72 h reperfusion in the IPC group in comparison to the IR group with the same reperfusion period. This suggested occurrence of survival of neurons what was also ascertained in other relevant studies [4, 5, 10, 11]. Recent observations showed that ERK activity is transiently increased in the ischemic core and perifocal region before cell death in both focal and global ischemia [15]. We determined that in the IR group, ERK 1/2 phosphorylation appeared to decrease as early as 15 min after injury in ischemic brain tissue, rise mildly after 1 h and gradually elevate 24 h after IRI what corresponds with similar studies [15, 37, 38]. ERK 1/2 phosphorylation was found in the ischemic surrounding cortex, and it was detected mainly in cytoplasm, glia and neurons after immunohistochemical (IHC) analysis according to Lee et al. [16]. It was also reported that ERK1/2 was activated in astrocytes of ischemic brains, and that ERK1/2 was associated with reactive gliosis [39] and participates in the survival of hilar neurons in dentate gyrus [40]. In most studies, maximal ERK activation was registered between 30 min and 2 h of reperfusion, although signals could be detected even after 6 h or longer [15].
Consistent with the findings reported by [41], in our study, the protein level of pERK was decreased first, and then increased and finally declined nearly to the sham level. Similarly, the ERK1/2 was activated during pre-ischemic exercise, and was substantially activated in response to IRI too [42]. Other authors [43] have shown that the IR-induced activation was partially inhibited by IPC. This limited activation, in turn play a role in downstream anti- or pro-apoptotic pathways by regulating expression of Bcl-xL, Bax and AIF in response to IRI, leading to a reduction in neuronal apoptosis and infarct volume. These authors also demonstrated that blocking pERK1/2 reverses the reduction in brain damage. As we showed in this study the immunoreactivity of pERK in the neuronal cells was in correlation with WB analysis. We located a decrease of pERK+ cells after 15 min ischemia, a modest increase after 1 h reperfusion in comparison to the control animal, followed by a more intensive decrease of pERK+ cells till 24 h reperfusion. Small elevations after 24 h reperfusion can be explained by non specific labeling in the injured tissue, power of insult and time lasting after insult, DNA damage, neuronal nucleus breakdown and overexpression of this protein (reviewed in references [17]), but in the end, the number of positive cells considerably decreased 1 h, after ischemia which could indicate death of vulnerable neurons. It was also often difficult to identify the nature or small cell bodies, which were only poorly labeled in sections processed for IHC analysis. In our analysis of experiments, a contrary situation was detected in IPC groups. The maximum protein level was observed 24 h after insult. This finding was in correlation with IHC analyses, where we detected a increased number of pERK+ cells in comparison to the control and also to IR groups with the same reperfusion period with maximum after 24 h. These results suggest that the ERK pathway is activated in the early stage of global cerebral ischemia. Its activation is associated with neuronal protection [41–43] and may become a promising therapeutic option in attenuating ischemic injury.
Prolonged activation of p38 has been shown to be involved in neuronal apoptosis and p38 inhibitors promote the survival of a variety of neurons in vitro [15, 18, 23, 28, 37, 44]. However, in response to specific stimuli, p38 has been shown to preferentially accumulate in the cytosol. Thus, it is possible that the intracellular distribution of p38 is associated with its substrate specificity and determined by the nature of the stimuli [45]. In our study, the first peak of p38 activation in IR groups was registered at 1 h of reperfusion, followed by a slight increase in activation. A second wave of increase in p38 activity was found 3 h after ischemia, but the level was lower than in the previous group and the highest level of protein level was detected 24 h after ischemia. The number of p38+ cells was in correlation with WB analysis after 24 h. We detected also significant differences between IPC and IR groups with identical reperfusion time, with maximum after 24 h. Whether such a dynamics in p38 activation represents tissue effort to sustain toxic effects or contributes to tissue injury in early and later stages of reperfusion, as corresponds with previous studies [15, 18, 28], remains to be clarified. Most reports linking p38 activity and excitotoxic injury have analyzed cell survival in culture hours and/or days after trauma [18, 28, 33, 34, 42]. Our results suggest that, p38 MAPK activation may have also short-term neurodisturband role during transient vessel occlusion. Therefore, a viable therapeutic intervention to prevent ischemic brain damage might involve the use of p38 inhibitors only after reperfusion [28, 34]. This is in line of recent experiments of Cao et al. [32] which show a negative feedback regulation of ERK cascade after sublethal cerebral ischemia in rat hippocampus. Further in vivo studies may be necessary to understand the role of both MAPKs in neural protection during the development of cerebral IPC. Together these data strongly imply both the MAPKs activation processes involved in neuronal damage following a stroke.
Conclusion
In conclusion, ERK 1/2 and p38 are activated after global cerebral ischemia and play an important role in ischemic injury. The present study indicates for the neuroprotectant role of ERK1/2 MAPK and for the neurodisturbant effect of p38 MAPK in tissues response to IRI and in the phenomenon of tolerance. Thus, the MAPKs signaling pathways might serve to understand the molecular mechanisms involved in the structural integrity and function of neuronal cells after ischemic challenge.
References
Lehotsky J, Burda J, Danielisova V, Gottlieb M, Kaplan P, Saniova B (2009) Ischemic tolerance: the mechanisms of neuroprotective strategy. Anat Rec 292:2002–2012
Lehotsky J, Racay P, Pavlikova M, Tatarková Z, Urban P, Chomova M, Kovalska M, Kaplan P (2009) Cross-talk of intracellular calcium stores in the response to neuronal ischemia and ischemic tolerance. Gen Physiol Biophys 28:104–113
Liu XQ, Sheng R, Qin ZH (2009) The neuroprotective mechanism of brain ischemic preconditioning. Acta Pharmacol Sin 30:1071–1080
Pavlikova M, Tatarkova Z, Sivonova M, Kaplan P, Krizanova O, Lehotsky J (2009) Alterations induced by ischemic preconditioning on secretory pathways Ca2+-ATPase (SPCA) gene expression and oxidative damage after global cerebral ischemia/reperfusion in rats. Cell Mol Neurobiol 29:909–916
Pignataro G, Scorziello A, Di Renzo G, Annunziato L (2009) Post-ischemic brain damage: effect of ischemic preconditioning and postconditioning and identification of potential candidates for stroke therapy. FEBS J 276:46–57
Heidbreder M, Naumann A, Tempel K, Dominiak P, Dendorfer A (2008) Remote vs. ischaemic preconditioning: the differential role of mitogen-activated protein kinase pathways. Cardiovasc Res 78:108–115
Lutz J, Thümel K, Heemann U (2010) Anti-inflammatory treatment strategies for ischemia/reperfusion injury in transplantation. J Inflamm 7:27
Szydlowska K, Tymianski M (2010) Calcium, ischemia and excitotoxicity. Cell Calcium 47:122–129
Riedemann NC, Ward PA (2003) Complement in ischemia reperfusion injury. Am J Pathol 162:363–367
Pavlikova M, Kovalska M, Tatarkova Z, Sivonova-Kmetova M, Kaplan P, Lehotsky J (2011) Response of secretory pathways Ca(2+) ATPase gene expression to hyperhomocysteinemia and/or ischemic preconditioning in rat cerebral cortex and hippocampus. Gen Physiol Biophys 30:S61–S69
Urban P, Pavlikova M, Sivonova M, Kaplan P, Tatarkova Z, Kaminska B, Lehotsky J (2009) Molecular analysis of endoplasmic reticulum stress response after global forebrain ischemia/reperfusion in rats: Effect of neuroprotectant simvastatin. Cell Mol Neurobiol 29:181–192
Lehotsky J, Urban P, Pavlikova M, Tatarkova Z, Kaminska B, Kaplan P (2009) Molecular mechanisms leading to neuroprotection/ischemic tolerance. Effect of preconditioning on the stress reaction of endoplasmic reticulum. Cell Mol Neurobiol 29:917–925
Pozo Devoto V, Giusti MS, Chavez JC, Fiszer de Plazas S (2008) Hypoxia-induced apoptotic cell death is prevented by oestradiol via oestrogen receptors in the developing central nervous system. J Neuroendocrinol 20:375–380
Gidday JM (2006) Cerebral preconditioning and ischaemic tolerance. Nat Rev Neurosci 7:437–448
Irving EA, Barone FC, Reitha AD, Hadingham SJ, Pardone AA (2000) Differential activation of MAPK/ERK and p38/SAPK in neurones and glia following focal cerebral ischaemia in the rat. Mol Brain Res 77:65–75
Lee CH, Yoo KY, Park OK, Choi JH, Kang IJ, Bae E, Kim SK, Hwang IK, Won MH (2010) Phosphorylated extracellular signal-regulated kinase 1/2 immunoreactivity and its protein levels in the gerbil hippocampus during normal aging. Mol Cells 29:373–378
Roux PP, Blenis J (2004) ERK and p38 MAPK-activated protein kinases: a family of protein kinases with diverse biological functions. Microbiol Mol Biol Rev 68:320–344
Lu Q, Rau TF, Harris V, Johnson M, Poulsen DJ, Black SM (2011) Increased p38 mitogen-activated protein kinase signaling is involved in the oxidative stress associated with oxygen and glucose deprivation in neonatal hippocampal slice cultures. Eur J Neurosci 34:1093–1101
Shen CP, Tsimberg Y, Salvadore C, Meller E (2004) Activation of Erk and JNK MAPK pathways by acute swim stress in rat brain regions. BMC Neurosci 5:36
Melania A, Gianfriddo M, Vannucchi MG, Cipriania S, Baraldi PG, Giovannini MG, Pedata F (2006) The selective A2A receptor antagonist SCH 58261 protects from neurological deficit, brain damage and activation of p38 MAPK in rat focal cerebral ischemia. Brain Res 1073–1074:470–480
Yang J, Yu Y, Duerksen-Hughes PJ (2003) Protein kinases and their involvement in the cellular responses to genotoxic stress. Mutat Res 543:31–58
Suzuki T, Okumura-Noji K, Nishida E (1995) ERK2-type mitogen-activated protein kinase (MAPK) and its substrates in postsynaptic density fractions from the rat brain. Neurosci Res 22:277–285
Carletti R, Tacconi S, Bettini E, Ferraguiti F (1995) Stress activated protein kinases, a novel family of mitogen-activated protein kinases are heterogeneously expressed in the adult rat brain and differentially disturbed extracellular-signal-regulated protein kinases. Neuroscience 69:1103–1110
Li DY, Tao L, Liu H, Christopher TA, Lopez BL, Ma XL (2006) Role of ERK1/2 in the anti-apoptotic and cardioprotective effects of nitricoxide after myocardial ischemia and reperfusion. Apoptosis 11:923–930
Ostrakhovitch EA, Cherian MG (2005) Inhibition of extracellular signal regulated kinase (ERK) leads to apoptosis inducing factor (AIF) mediated apoptosis in epithelial breast cancer cells: the lack of effect of ERK in p53 mediated copper induced apoptosis. J Cell Biochem 95:1120–1134
Stoica BA, Movsesyan VA, Knoblach SM, Faden AI (2005) Ceramide induces neuronal apoptosis through mitogen-activated protein kinases and causes release of multiple mitochondrial proteins. Mol Cell Neurosci 29:355–371
Chen KD, Chen LY, Huang HL, Lieu CH, Chang YN, Chang MDT, Lai YK (1998) Involvement of p38 mitogen-activated protein kinase signaling pathway in the rapid induction of the 78-kDa glucose-regulated protein in 9L rat brain tumor cells. J Biol Chem 273:749–755
Wang YX, Xu XY, Su WL, Wang Q, Zhu WX, Chen F, Jin G, Liu YJ, Li YD, Sun YP, Gao WC, Ruan CP (2010) Activation and clinical significance of p38 MAPK signaling pathway in patients with severe trauma. J Surg Res 161:119–125
Lehotsky J, Murin R, Strapkova A, Uhrikova A, Tatarkova Z, Kaplan P (2004) Time course of ischemia/reperfusion-induced oxidative modification of neural proteins in rat forebrain. Gen Physiol Biophys 23:401–415
Sivonova M, Kaplan P, Durackova Z, Dobrota D, Drgova A, Tatarkova Z, Pavlikova M, Halasova E, Lehotsky J (2008) Time course of peripheral oxidative stress as consequence of global ischaemic brain injury in rats. Cell Mol Neurobiol 28:431–441
Tatarkova Z, Engler I, Calkovska A, Mokra D, Dgrova A, Hodas P, Lehotsky J, Dobrota D, Kaplan P (2011) Effect of long-term normobaric hypoxia on oxidative stress in mitochondria of the guinea pig brain. Neurochem Res 36:1475–1481
Cao Q, Qian M, Wang XF, Wang B, Wu HW, Zhu XJ, Wang YW, Guo J (2011) Negative feedback regulation of Raf/MEK/ERK cascade after sublethal cerebra ischemia in the rat hippocampus. Neurochem Res 36:153–162
Bu X, Huang P, Qi Z, Zhang N, Han S, Fang L, Li J (2007) Cell type-specific activation of p38 MAPK in the brain regions of hypoxic preconditioned mice. Neurochem Int 51:459–466
Brust TB, Cayabyab FS, Zhou N, MacVicar BA (2006) p38 Mitogen-activated protein kinase contributes to adenosine A1 receptor-mediated synaptic depression in area CA1 of the rat hippocampus. J Neurosci 26:12427–12438
Campos-Gonzalez R, Kindy MS (1992) Tyrosine phosphorylation of microtubule-associated protein kinase after transient ischemia in the gerbil brain. J Neurochem 59:1955–1958
Hu BR, Wieloch T (1994) Tyrosine phosphorylation and activation of mitogen-activated protein kinase in the rat brain following transient cerebral ischemia. J Neurochem 62:1357–1367
Wang Z, Chen X, Zhou L, Wu D, Che X, Yang G (2003) Effects of extracellular signal -regulated kinase (ERK) on focal cerebral ischemia. Chin Med J 116:1497–1503
Yan XB, Hou HL, Wu LM, Liu J, Zhou JN (2007) Lithium regulates hippocampal neurogenesis by ERK pathway and facilitates recovery of spatial learning and memory in rats after transient global cerebral ischemia. Neuropharmacology 53:487–495
Lennmyr F, Karlsson S, Gerwins P, Ata KA, Terent A (2002) Activation of mitogen-activated protein kinases in experimental cerebral ischemia. Acta Neurol Scand 106:333–340
Veeranna GJ, Shetty KT, Takahashi M, Grant P, Pant HC (2000) Cdk5 and MAPK are associated with complexes of cytoskeletal proteins in rat brain. Mol Brain Res 76:229–236
Gu Z, Jiang Q, Zhang G (2001) Extracellular signal-regulated kinase ½ activation in hippocampus after cerebral ischemia may not interfere with postischemic cell death. Brain Res 901:79–84
Zhang QG, Wang RM, Han D, Yang LC, Li J, Brann DW (2009) Preconditioning neuroprotection in global cerebral ischemia involves NMDA receptor-mediated ERK-JNK3 crosstalk. Neurosci Res 63:205–212
Liebelt B, Papapetrou P, Ali A, Guo M, Ji X, Peng C, Rogers R, Curry A, Jimenez D, Ding Y (2010) Exercise preconditioning reduces neuronal apoptosis in stroke by up-regulating heat shock protein-70 (heat shock protein-72) and extracellular-signal-regulated-kinase 1/2. Neuroscience 166:1091–1100
Wang X, Wang H, Xu L, Rozanski DJ, Sugawara T, Chan PH, Trzaskos JM, Feuerstein GZ (2003) Significant neuroprotection against ischemic brain injury by inhibition of the MEK1 protein kinase in mice: exploration of potential mechanism associated with apoptosis. J Pharmacol Exp Ther 304:172–178
Wood CD, Thornton TM, Sabio G, Davis RA, Rincon M (2009) Nuclear localization of p38 MAPK in response to DNA damage. Int J Biol Sci 5:428–437
Paxinos G, Watson C (eds.) (2006) The Rat Brain in Stereotaxic Coordinates. Academic Press, London. http://www.scribd.com/doc/22822097/Rat-Brain-Atlas
Acknowledgments
This study was supported by Grants VEGA 213/12, from the Ministry of Education of the Slovak Republic, UK-55-15/07 from Ministry of Health of the Slovak Republic, VVCE 0064-07 and UK/10/2010 and by project ‘‘Identification of novel markers in diagnostic panel of neurological diseases‘‘code: 26220220114, co-financed from EU sources and European Regional Development Fund. The authors are grateful to Mrs. Zdenka Cetlová and Ing. Ján Fillo for their excellent help with animals. The authors are also thankful to Mrs. Monika Letrichová, Margatéta Kondeková and Agáta Rešetárová for their help with immunohistochemical analysis of brain tissue.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kovalska, M., Kovalska, L., Pavlikova, M. et al. Intracellular Signaling MAPK Pathway After Cerebral Ischemia–Reperfusion Injury. Neurochem Res 37, 1568–1577 (2012). https://doi.org/10.1007/s11064-012-0752-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-012-0752-y