Abstract
Substantial uncertainty exists about the prevalence of depressive disorders in individuals with autism spectrum disorder (ASD). This meta-analysis quantitatively summarized studies that assessed the lifetime and current prevalence of unipolar depressive disorders in children, adolescents, and adults with ASD. We also examined demographic, methodological, and study moderators. This meta-analysis adhered to PRISMA guidelines. A total of 7857 articles were identified through 5 databases (PubMed, Web of Science, PYSCInfo, CINAHL, ProQuest Dissertations and Theses), forward searches, and backward searches. Two reviewers independently screened articles and extracted data. Sixty-six articles met inclusion criteria. Results indicated that the pooled lifetime and current prevalence was 14.4% (95% CI 10.3–19.8) and 12.3% (95% CI 9.7–15.5), respectively. Rates of depressive disorders were highest among studies that used a standardized interview to assess depressive disorders (lifetime = 28.5%, 95% CI 20.1–38.8; current = 15.3%, 95% CI 11.0–20.9) and required participants to report on their own depressive symptoms (lifetime = 48.6%, 95% CI 33.3–64.2; current = 25.9%, 95% CI 17.0–37.3). Rates were also higher in studies that included participants with higher intelligence. Lifetime, but not current, prevalence was positively associated with age and the proportion of the sample that was White. In conclusion, we found that the rates of depressive disorders are high among individuals with ASD. Compared to typically developing individuals, individuals with ASD are 4-times more likely to experience depression in their lifetime. These results suggest that individuals with ASD should be regularly screened and offered treatment for depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Global prevalence estimates indicate that 1 in 160 individuals is diagnosed with autism spectrum disorder (ASD), a lifelong neurodevelopmental disorder with two core features: persistent deficits in social communication and social interactions; and restricted, repetitive patterns of behavior, interests, and activities (American Psychiatric Association 2013; World Health Organization 2017). In the United States, prevalence estimates indicate that 1 in 68 individuals is diagnosed with ASD (Wingate et al. 2014), which suggests that the rates of ASD may be even higher when populations are well monitored. Significant heterogeneity exists in the symptom presentation and level of functioning in individuals with ASD; however, the majority of individuals with ASD experience poor outcomes, including lack of independent living, unemployment, and few peer relationships (Fernell et al. 2013).
Negative outcomes for individuals with ASD may be exacerbated by psychiatric comorbidities (Matson and Cervantes 2014), which are associated with greater adaptive behaviour impairments in individuals with ASD (Kraper et al. 2017). Unipolar depressive disorders are the most common psychiatric disorders, and they are the leading cause of disability worldwide (Ustün et al. 2004). As such, comorbid depressive disorders may result in particularly poor prognoses for individuals with ASD. Lifetime prevalence rates of unipolar depressive disorders in US epidemiological samples have been estimated at 11.7% for post-pubertal adolescents (Merikangas et al. 2010) and 16.6% for adults (Kessler et al. 2005). In contrast, there is extreme variability in reported rates of depression in studies of individuals with ASD, with lifetime prevalence estimates ranging from 1% to 76% (Billstedt et al. 2005; Joshi et al. 2013). Reliable estimates of comorbid depressive disorders in individuals with ASD are essential to ascertain the overall burden of comorbidity on the health care system and to ensure that treatment programs addressing comorbid depression are sufficient to meet the need. Depression in ASD may be associated with severe consequences, including attempted suicide (Cassidy and Rodgers 2017; Richa et al. 2014), a regression in level of functioning (Magnuson and Constantino 2011), and the need for higher levels of care. Therefore, failure to address comorbid depression in the treatment of ASD adds significantly to the personal and societal burden associated with the disorder.
Several factors may explain the wide range in estimated rates of depressive disorders in individuals with ASD. Among typically developing individuals, young adults, females, and White individuals experience higher rates of depressive disorders compared to other age groups, males, and non-White individuals (Kessler et al. 1993; Riolo et al. 2005). It is unclear whether depressive disorders in individuals with ASD follow similar trends. Intelligence may also influence the prevalence rates of depressive disorders in individuals with ASD, although the direction of the effect remains unclear. Low intellectual functioning has been associated with the presence and persistence of depressive disorders in typically developing individuals (Koenen et al. 2009). However, it has also been suggested that individuals with ASD who have average or above average intelligence may have a better understanding of the deficits associated with ASD, resulting in a greater susceptibility to becoming depressed (Chandrasekhar and Sikich 2015).
Methodology choices, including recruitment setting and assessment tools, also vary widely across studies. Recruiting from a hospital-based system may inflate prevalence estimates by sampling individuals who are presenting for psychiatric treatment. In addition, reliance on prior diagnoses or unstandardized interviews may underestimate the prevalence of depressive disorders compared to standardized semi-structured interviews, which systematically ask participants about symptoms of depressive disorders (Miller et al. 2001). Informant choice may also influence prevalence rates. Parents of typically developing adolescents (i.e., adolescents without a neurodevelopmental disorder) report that they lack knowledge of their child’s feelings (Moretti et al. 1985), which may contribute to discrepancies between self- and parent-report of psychiatric comorbidities.
To our knowledge, there have been no attempts to quantitatively synthesize the existing literature on prevalence rates of depressive disorders in individuals with ASD. The current meta-analysis is the first to fill this gap by exploring the lifetime and current prevalence of unipolar depressive disorder diagnoses in children, adolescents, and adults with ASD. Lifetime prevalence refers to the proportion of individuals who have met criteria for a unipolar depressive disorder in their lifetime, whereas current prevalence refers to the proportion of individuals who met criteria for a unipolar depressive disorder at the time of the assessment or within a three-month period. Psychiatric diagnoses were assigned using a standardized interview, clinical judgement, or retrospectively (i.e., chart review or self/caregiver-report of prior diagnoses). We also examined demographic variables (age, sex, ethnicity, intelligence), methodological variables (recruitment setting, assessment method, informant) and study characteristics (year of publication, peer reviewed publication status) as moderators, which may help to explain the variability in rates found across studies.
Method
Literature Search Strategy
Studies were identified by searching the following databases: PubMed, Web of Science, PYSCInfo, CINAHL, and ProQuest Dissertations and Theses. We searched for the following search terms: autis*, ASD, Asperger, pervasive developmental disorder and PDD-NOS combined with depress*, dysthym*, internaliz*, and mood. Searches were conducted in November 2016. As a complement to this search, we performed backward searches (i.e., examining reference lists of eligible studies) and forward searches (i.e., examining articles that had cited eligible studies).
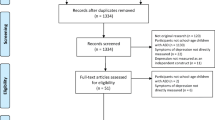
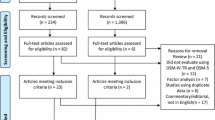
The searches yielded a total of 7857 articles. The first and second authors screened all articles. During the first stage, articles were excluded based on the title and abstract if they were not written in English, did not include participants with ASD, or did not assess depression. All articles that were deemed relevant by one or both authors were included. A total of 970 articles were identified. In the second stage, the first and second authors independently reviewed the full text of articles. Articles were excluded if they met any of the exclusion criteria from the first stage, if they did not report the lifetime or current prevalence of a depressive disorder diagnosis, or if they specifically recruited participants for psychiatric difficulties. Studies that only assessed depressive symptoms were excluded. At this stage, discrepancies between authors were discussed and resolved by consensus. The first author contacted the corresponding author of studies to clarify details, if necessary. If the authors did not respond or could not provide the information, these studies were excluded. The most common clarifications were whether authors assessed lifetime or current prevalence of depressive disorders (n = 27 or 40.91% of included studies) and whether studies differentiated between unipolar and bipolar depressive disorders (k = 6 or 9.09% of included studies). The results of the systematic literature search are shown in Fig. 1.
Corresponding authors were contacted to obtain any available unpublished data. Of the 49 unique corresponding authors, 29 authors (59.18%) responded; however, no unpublished data were obtained (i.e., the authors had no data or they were unable to send the data due to data sharing restrictions). A total of 66 articles (35 reporting lifetime prevalence, 22 reporting current prevalence, 9 reporting both) met inclusion criteria. The exact number of studies included in moderation analyses varies because of missing data on methodological and demographic characteristics.
Study Coding
Both the first and second author coded all articles. The average percent agreement across variables was 91.91% (range: 80.30–98.49%). Disagreement was resolved by consensus and the consensus ratings were used in analyses. Studies that reported two independent samples (e.g., prevalence rates stratified by age group) were coded separately. Five demographic variables were coded: age (mean, range), percentage of participants who were male, percentage of participants who were White, mean full scale intelligence quotient (FSIQ), and percentage of participants who had an IQ of less than 70. Three methodology variables were coded: recruitment setting (outpatient, community, or both), depression assessment method (standardized interview or other assessment method), and informant (caregiver, self, or both). Other assessment methods included chart review (n = 10), parent report of prior diagnoses by a health professional (n = 15), self-report of prior diagnoses by a health professional (n = 2), or an unstandardized assessment by a health professional (n = 5). Two study characteristics were coded: year of publication and peer reviewed publication status. Finally, we also coded depression diagnosis reference period (i.e., current, lifetime, or other), the sample size, and the number of participants who met criteria for a depressive disorder in order to compute the effect sizes. Because studies often failed to report the specific depressive disorders they assessed, we combined all unipolar depressive diagnoses (e.g., major depressive disorder, persistent depressive disorder, other specified depressive disorder, etc.). The coded variables for each study are presented in Table S1 in the online data supplement.
Study quality was assessed using the Risk of Bias tool (RoB; Hoy et al. 2012), which is specifically designed to assess risk of bias in prevalence studies. The RoB includes ten items that assess external and internal validity using forced choice response (yes, no). Two items were excluded that were not relevant to the current study. Therefore, the highest possible score on the RoB was reduced to eight. Studies were judged to be at low risk of bias (≥4 points) or high risk of bias (<4 points). Both the first and second author independently rated studies using the RoB tool and discrepancies were resolved by consensus. The average percent agreement across RoB variables was 85.85% (range: 75.76–98.49%). The RoB items and coding guide can be found in Appendix A in the online data supplement.
Data Analysis
Meta-analyses were performed with the Comprehensive Meta-Analysis software (Borenstein et al. 2005) using random-effects models. We examined studies that reported the proportion of individuals with ASD who met criteria for a lifetime or current unipolar depressive disorder. These proportions were transformed into a logit event rate effect size and the standard error was calculated. The logit event rates were transformed back to proportions after analyses were conducted to improve interpretability of the results. Forest plots were drawn to visualize the extent of heterogeneity across studies. Both the Q and I2 statistics were used to quantitatively examine heterogeneity.
Moderator Analyses
We evaluated whether the proportion of the sample that met criteria for a depressive disorder varied due to demographic variables, methodological variables, or study characteristics. We used the Qbetween statistic, an analogue to analysis of variance, to test the relation between proportions and each categorical variable. A series of all possible two-group comparisons were conducted with Bonferroni correction to follow-up significant categorical moderators. Continuous moderators were analyzed using meta-regression. Interactions among moderator variables were not tested due to insufficient power.
Publication Bias
Publication bias was estimated quantitatively using the Begg’s rank method (Begg and Mazumdar 1994) and Egger’s weighted regression analysis (Egger et al. 1997), which compute the relation between effect sizes and sample sizes. In addition, funnel plots were examined for asymmetry. If significant funnel plot asymmetry existed, the trim and fill method was used to determine the number of missing studies due to publication bias (Duval 2005; Duval and Tweedie 2000).
Results
Lifetime Prevalence of Depressive Disorders
Based on the 44 studies identified, the pooled lifetime prevalence of unipolar depressive disorders in individuals with ASD was 14.4% (95% CI 10.3–19.8). The results were found to be heterogeneous, range = 0.4% to 76.2%, I2 = 97.53, Q = 1741.71, p < 0.01. A forest plot for the meta-analysis of lifetime prevalence of depressive disorders in individuals with ASD is depicted in Fig. 2.
Factors Associated with Lifetime Prevalence
Coded moderator variables for each study are presented in Table S1 in the online data supplement. A summary of the lifetime prevalence stratified by categorical moderator variables is presented in Table 1. A significant amount of variance remained unaccounted for in all moderator analyses (ps < .001).
Demographic variables
Higher mean age of the sample was associated with higher lifetime prevalence (regression coefficient: 0.07, 95% CI 0.03–0.11, p < .001). Studies that included only adult participants aged 18 and older (40.2%, 95% CI 22.8–60.6, n = 8) had a significantly higher lifetime prevalence rate compared to studies that only included child or adolescent participants aged 18 and under (7.7%, 95% CI 4.7–12.4, n = 18), Qbetween(1) = 17.32, p < .001. Studies that included only adult participants also had higher lifetime prevalence rates compared studies that included children/adolescents and adults (14.3%, 95% CI 8.3–23.7, n = 12), Qbetween(1) = 6.99, p = .008. Studies that only included children/adolescents did not statistically differ from studies that included both children/adolescents and adults, Qbetween(1) = 2.78, p = .10. In addition, the proportion of males in the sample was not associated with lifetime prevalence rates (regression coefficient: = 0.01, 95% CI -0.05–0.02, p = .39).
Studies with a higher proportion of participants who were White were associated with higher lifetime prevalence rates (regression coefficient = 0.07, 95% CI 0.03–0.11, p < .001). Greater mean IQ of the sample was associated with greater lifetime prevalence (regression coefficient: 0.06, 95% CI: 0.03–0.09, p < .001). Studies with a mean IQ greater than 100 had significantly higher prevalence rates (52.8%, 95% CI 39.8–65.4, n = 7) than studies with a mean IQ less than 100 (12.2%, 95% CI 6.4–22.1, n = 8), Qbetween(1) = 21.18, p < .001. The proportion of individuals who had an IQ of less than 70 was not associated with lifetime prevalence (regression coefficient: -0.01, 95% CI: -0.03–0.01, p = .21).
Methodology variables
Lifetime prevalence rates did not vary by recruitment setting, Qbetween(2) = 3.48, p = .18. However, the pooled lifetime prevalence in studies that used standardized semi-structured interviews (28.5%, 95% CI 20.1–38.8, k = 22) was significantly higher than that reported in studies that used other assessment methods (6.7%, 95% CI 4.2–10.3, n = 22), Qbetween(1) = 25.70, p < .001.
Further, lifetime prevalence rates varied significantly based on the informant, Qbetween(2) = 20.27, p < .001. Studies in which participants reported on their own depressive symptoms had significantly higher prevalence rates (48.6%, 95% CI 33.3–64.2, n = 6) compared to studies in which caregivers reported on the participants’ depressive symptoms (14.4%, 95% CI 10.1–20.0, n = 21), Qbetween(1) = 20.25, p < .001. The lifetime prevalence rates in studies in which both the caregivers and participants reported on their depressive symptoms (23.0%, 95% CI 7.9–51.0, n = 7) did not differ from studies in which participants or caregivers independently reported on their depressive symptoms, Qbetween(1) = 2.59, p = .11 and Qbetween(1) = 0.76, p = .39, respectively.
Study characteristics
Year of publication was not associated with lifetime prevalence rates (regression coefficient: 0.05, 95% CI -0.14–0.05, p = .34). The lifetime prevalence rates in studies that were published in peer reviewed journals (n = 39) did not differ significantly from studies that had not undergone peer review (n = 5), Qbetween(1) = 2.05, p = .15.
Publication Bias
The funnel plot (Fig. 3) is symmetrical, suggesting no publication bias. Similarly, quantitative assessments of publication bias were not significant (p = .12 for Begg’s rank correlation analysis; p = .37 for Egger’s weighted regression analysis).
Current Prevalence of Depressive Disorders
Based on the 31 studies identified, the pooled current prevalence of unipolar depressive disorders in individuals with ASD was 12.3% (95% CI 9.7–15.5). The results were found to be heterogeneous, range = 0.6% to 50.0%, I2 = 80.36, Q = 152.77, p < .001. A forest plot for the meta-analysis of current prevalence of depressive disorders in individuals with ASD is depicted in Fig. 4.
Factors Associated with Current Prevalence
Coded moderator variables for each study are presented in Table S1 in the online data supplement. A summary of the current prevalence stratified by categorical moderator variables is presented in Table 1. A significant amount of variance remained unaccounted for in all moderator analyses (ps < .001).
Demographic variables
Age was not associated with current prevalence rates (regression coefficient: 0.01, 95% CI -0.02–0.05, p = .39). Further, current prevalence rates did not differ among studies that only included adult participants, studies that only included child/adolescent participants, and studies that included both adults and children/adolescents, Qbetween(2) = 2.45, p = .29. In addition, current prevalence rates were not associated with sex (regression coefficient: = 0.02, 95% CI -0.02–0.05, p = .48), ethnicity (regression coefficient: = 0.00, 95% CI -0.02–0.02, p = .93), or FSIQ (regression coefficient = 0.02, 95% CI -0.01–0.04, p = .17). However, studies that contained more individuals with an IQ of less than 70 had lower current prevalence rates of depressive disorders (regression coefficient: -0.01, 95% CI -0.02–0.01, p < .001).
Methodology variables
The current prevalence rates of depressive disorders in individuals with ASD did not vary depending on the setting from which participants were recruited, Qbetween(2) = 0.93, p = .63. However, the pooled current prevalence rates reported in studies that used a standardized semi-structured interview (15.3%, 95% CI 11.0–20.9, n = 18) was significantly higher than the pooled current prevalence rates reported in studies that used other assessment methods (9.3%, 95% CI 6.6–13.0, n = 13), Qbetween(1) = 4.28, p = .04.
Further, current prevalence rates varied significantly based on the informant, Qbetween(2) = 11.17, p = .004. Studies in which participants reported on their own depressive symptoms had significantly higher prevalence rates (25.9%, 95% CI 17.0–37.3, n = 4) compared to studies in which caregivers reported on the participants’ depressive symptoms (10.4%, 95% CI 7.3–14.6, n = 14), Qbetween(1) = 10.65, p = .001, and studies in which both caregivers and the participants’ reported on the participants’ depressive symptoms (12.1%, 95% CI 7.9–18.2, n = 12). The current prevalence rates in studies in which both the caregivers and participants reported on their depressive symptoms did not differ from studies in which only caregivers reported on the participants’ depressive symptoms, Qbetween(1) = 0.29, p = .59.
Study characteristics
Year of publication was not associated with current prevalence rates (regression coefficient: 0.02, 95% CI -0.05–0.09, p = .60). Only one study was retrieved that assessed current prevalence rates and was not in a peer-reviewed journal (1.8%, 95% CI 0.03–11.8). This study had significantly lower current prevalence rates than studies that were published in peer reviewed journals (12.7%, 95% CI 10.0–15.9, n = 30), Qbetween(1) = 4.09, p = .04.
Publication Bias
As shown in Fig. 5, the funnel plot is asymmetrical, suggesting publication bias may be present. Quantitative measures of publication bias were significant (Egger’s weight regression analysis, p = .04) or trending (Begg’s rank correlation analysis, p = .09). The trim and fill method imputed five missing studies due to publication bias. After adjustment for publication bias, the current prevalence of depressive disorders was 15.6% (95% CI 14.32–16.91).
Discussion
The current meta-analysis is the first to quantitatively summarize rates of unipolar depressive disorders in individuals with ASD. The results confirm that depression is a problem of considerable magnitude in this population. The pooled lifetime prevalence rate was 14.4% and the pooled current prevalence rate was 12.3%. The lifetime prevalence of depression in children with ASD 18-years-old and younger is similar to the lifetime rates found in post-pubertal typically developing adolescents (Merikangas et al. 2010). However, we found that the current prevalence of depression in studies that only assessed youth with ASD is four-fold higher than current prevalence in youth without ASD (Angold and Costello 2001). When our analyses are restricted to adult samples, the prevalence of depression in individuals with ASD is three- to four-fold higher than the rates seen in typically developing adults (Kessler et al. 2003, 2005).
Demographic Moderators
The current meta-analysis identified several factors that may influence the rates depressive disorder in individuals with ASD. Samples that included more White participants had higher lifetime prevalence of depressive disorders. This finding is consistent with studies in the general population that suggest that White individuals report higher levels of depression compared to non-White individuals (Breslau et al. 2008; Riolo et al. 2005). It is possible that non-White individuals with ASD may be under-diagnosed, particularly in the studies that relied on unstandardized methods for assessing depression or when standardized interviews are not culturally sensitive. Insufficient power precluded us from investigating whether the relation between ethnicity and rates of depressive disorders varied across assessment methods, but future researchers are encouraged to disentangle this relation.
Higher FSIQ was also associated with higher lifetime prevalence and samples that contained more people in the Extremely Low IQ range (i.e., IQ < 70) had lower current prevalence of depressive disorders. Individuals with low intellectual functioning may have difficulties identifying and communicating their thoughts and feelings, making it difficult to diagnose depressive disorders in this population. Conversely, individuals with ASD who had average or above average intellectual functioning may be more aware of their deficits (e.g., in social interactions), which may be associated with higher rates of depressive disorders (Chandrasekhar and Sikich 2015).
No age differences were found in the current prevalence of depressive disorders in individuals with ASD. This finding is in contrast to the typically developing literature, which has found that the 12-month prevalence of major depressive disorder is threefold higher in young adults compared to older adults; however, age is not linearly related to depression in typically developing samples, which may have prevented us from detecting age trends (American Psychiatric Association 2013; Costello et al. 1988; Kessler et al. 2010; Regier et al. 1988). In addition, no sex differences were found in the current or lifetime prevalence rates. This null finding is in contrast to the typically developing literature, which consistently reports that females experience 1.5- to 3-fold higher rates of current and lifetime depressive disorders compared to males (American Psychiatric Association 2013; Kessler et al. 1993). However, it should be noted that the majority of the studies included in the current meta-analysis included a preponderance of males, and they were primarily focused on children. Therefore, we may have been underpowered to find age and sex effects. Age and sex differences may also be difficult to detect in individuals with ASD due to a potential interaction between these variables. Gotham and colleagues found that males with ASD have high rates of depressive symptoms throughout adolescence, where as females endorse more depressive symptoms as they age (Gotham et al. 2015). Targeted, longitudinal studies are required to determine the unique sex and developmental trends associated with the onset of depression in individuals with ASD.
Methodological Moderators
Assessing depressive disorders in individuals with ASD with standardized semi-structured interviews resulted in higher rates compared to studies that assessed depressive disorders using non-standardized procedures. Standardized interviews are the most reliable way of assessing psychiatric disorders in the general population (Miller et al. 2001). As such, the rates reported using such instruments may be a more accurate reflection of the true prevalence rate of depression in the ASD population. At the same time, however, individuals with ASD often underestimate their impairments compared to caregiver-report, which may result in biased prevalence estimates (Johnson et al. 2009). Some have suggested that existing standardized interviews may need to be adapted for individuals with ASD because existing measures may mischaracterize ASD symptoms or phrase questions in ways that are difficult for individuals with ASD to understand (Chandrasekhar and Sikich 2015; Mazzone et al. 2012). Only five studies in the current meta-analysis used adapted interviews; thus more research is needed directly comparing the reliability and validity of adapted and non-adapted interviews.
Self-report of depressive symptoms resulted in higher lifetime and current prevalence rates compared to caregiver-report. This finding is consistent with the typically developing literature, which has found that children report higher rates of psychiatric comorbidities than their caregivers (Achenbach et al. 1987). It is possible that individuals with ASD may be reporting depressive symptoms that their caregivers are missing. In contrast, it is also possible that differences may be due to a third variable interaction (e.g., caregiver-report may be more likely to be obtained when participants have more severe ASD symptoms). Again, future research that is able to examine interactions between these moderators is needed to address this issue.
Strengths and Limitations
The current meta-analysis has a number of notable strengths. First, we employed a methodologically rigorous approach according to current guidelines that resulted in screening nearly 8000 articles, allowing us to provide a comprehensive overview of the current literature. Second, studies were not excluded based on geographical location, thus allowing for the generalization of our findings to the global population of individuals with ASD. Finally, we focused on depressive diagnoses rather than symptoms, and thus the prevalence rates reported here reflect the presence of a clinically significant psychiatric comorbidity.
The results of the meta-analysis should be interpreted in light of some limitations. First, our sample size in the meta-analysis that assessed current prevalence of depressive disorders was small (n = 31), which contributes to low power for moderation analyses. In addition, the small number of studies that assessed each moderator precluded us from investigating interactions among moderator variables. Exploring these interactions would have provided more accurate rates of depressive disorders in individuals with ASD. Finally, as with all meta-analyses, we were limited by existent studies. The results reflect only what is available in terms of existing literature. On average, the participants included in the current meta-analysis were young (Mage = 11.30), male (81.65% male), and had slightly below average cognitive abilities (MFSIQ = 91.37). Consequently, the overall prevalence estimates presented in the current study are not representative of all individuals with ASD. Future research is needed to better understand the prevalence of depressive disorders in subgroups of individuals with ASD.
Conclusions
The current study is an essential step in supporting individuals with ASD by elucidating the pervasiveness of comorbid depression in this population. In North America, nearly 1 million individuals with ASD will experience a depressive disorder in their lifetime. Consequently, health care providers should be aware that depression in individuals with ASD is a common problem. The impairments associated with depression may be compounded by the presence of additional psychiatric comorbidities, such as anxiety, which is highly prevalent in individuals with ASD (van Steensel et al. 2011). Regularly screening for comorbidities will facilitate access to treatments (Kiep et al. 2015; McGillivray and Evert 2014) and prevent compounding the disability associated with ASD, thereby minimizing the personal and societal costs of these disorders.
References
Achenbach, T. M., McConaughy, S. H., & Howell, C. T. (1987). Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin, 101(2), 213–232. https://doi.org/10.1037/0033-2909.101.2.213
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington: American Psychiatric Publishing.
Angold, A., & Costello, E. J. (2001). The epidemiology of depression in children and adolescents. In I. M. Goodyer (Ed.), The depressed child and adolescent (2nd ed., pp. 143–178). New York: Cambridge University Press.
Begg, C. B., & Mazumdar, M. (1994). Operating characteristics of a rank correlation test for publication bias. Biometrics, 50, 1088–1101.
Billstedt, E., Gillberg, C., & Gillberg, C. (2005). Autism after adolescence: Population-based 13- to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. Journal of Autism and Developmental Disorders, 35, 351–360. https://doi.org/10.1007/s10803-005-3302-5
Borenstein, M., Rothstein, D., & Cohen, J. (2005). Comprehensive meta-analysis: A computer program for research synthesis [computer software]. Englewood: Biostat.
Breslau, J., Javaras, K. N., Blacker, D., Murphy, J. M., & Normand, S. L. T. (2008). Differential item functioning between ethnic groups in the epidemiological assessment of depression. The Journal of Nervous and Mental Disease, 196(4), 297. https://doi.org/10.1097/NMD.0b013e31816a490e
Cassidy, S., & Rodgers, J. (2017). Understanding and prevention of suicide in autism. The Lancet Psychiatry, 4(6), e11. https://doi.org/10.1016/S2215-0366(17)30162-1
Chandrasekhar, T., & Sikich, L. (2015). Challenges in the diagnosis and treatment of depression in autism spectrum disorders across the lifespan. Dialogues in Clinical Neuroscience., 17(2), 219–227.
Costello, E. J., Costello, A. J., Edelbrock, C., Burns, B. J., Dulcan, M. K., Brent, D., & Janiszewski, S. (1988). Psychiatric disorders in pediatric primary care: Prevalence and risk factors. Archives of General Psychiatry, 45(12), 1107–1116.29.
Duval, S. (2005). The trim and fill method. In H. R. Rothstein, A. J. Sutton, & M. Borenstein (Eds.), Publication bias in meta-analysis: Prevention, assessment and adjustments (pp. 127–144). Hoboken: Wiley.
Duval, S., & Tweedie, R. (2000). Trim and fill: A simple funnelplot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56, 455–463. https://doi.org/10.1111/j.0006-341X.2000.00455.x
Egger, M., Smith, G. D., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. British Medical Journal, 315, 629–634.
Fernell, E., Eriksson, M. A., & Gillberg, C. (2013). Early diagnosis of autism and impact on prognosis: A narrative review. Clinical Epidemiology, 5, 33–43. https://doi.org/10.2147/CLEP.S41714
Gotham, K., Brunwasser, S. M., & Lord, C. (2015). Depressive and anxiety symptom trajectories from school age through young adulthood in samples with autism spectrum disorder and developmental delay. Journal of the American Academy of Child & Adolescent Psychiatry, 54(5), 369–376. https://doi.org/10.1016/j.jaac.2015.02.005
Hoy, D., Brooks, P., Woolf, A., Blyth, F., March, L., Bain, C., et al. (2012). Assessing risk of bias in prevalence studies: Modification of an existing tool and evidence of interrater agreement. Journal of Clinical Epidemiology, 65(9), 934–939. https://doi.org/10.1016/j.jclinepi.2011.11.014
Johnson, S. A., Filliter, J. H., & Murphy, R. R. (2009). Discrepancies between self-and parent-perceptions of autistic traits and empathy in high functioning children and adolescents on the autism spectrum. Journal of Autism and Developmental Disorders, 39(12), 1706–1714. https://doi.org/10.1007/s10803-009-0809-1
Joshi, G., Wozniak, J., Petty, C., Martelon, M. K., Fried, R., Bolfek, A., et al. (2013). Psychiatric comorbidity and functioning in a clinically referred population of adults with autism spectrum disorders: A comparative study. Journal of Autism and Developmental Disorders, 43(6), 1314–1325. https://doi.org/10.1007/s10803-012-1679-5
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Koretz, D., Merikangas, K. R., et al. (2003). The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R). The Journal of the American Medical Association, 289(23), 3095–3105. https://doi.org/10.1001/jama.289.23.3095
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. https://doi.org/10.1001/archpsyc.62.6.593
Kessler, R. C., Birnbaum, H., Bromet, E., Hwang, I., Sampson, N., & Shahly, V. (2010). Age differences in major depression: Results from the National Comorbidity Survey Replication (NCS-R). Psychological Medicine, 40(2), 225–237. https://doi.org/10.1017/S0033291709990213
Kessler, R. C., McGonagle, K. A., Swartz, M., Blazer, D. G., & Nelson, C. B. (1993). Sex and depression in the National Comorbidity Survey I: Lifetime prevalence, chronicity and recurrence. Journal of Affective Disorders, 29(2), 85–96.
Kiep, M., Spek, A. A., & Hoeben, L. (2015). Mindfulness-based therapy in adults with an autism spectrum disorder: Do treatment effects last? Mindfulness, 6, 637–644. https://doi.org/10.1007/s12671-014-0299-x
Koenen, K. C., Moffitt, T. E., Roberts, A. L., Martin, L. T., Kubzansky, L., Harrington, H., et al. (2009). Childhood IQ and adult mental disorders: A test of the cognitive reserve hypothesis. American Journal of Psychiatry, 166(1), 50–57. https://doi.org/10.1176/appi.ajp.2008.08030343
Kraper, C. K., Kenworthy, L., Popal, H., Martin, A., & Wallace, G. L. (2017). The gap between adaptive behavior and intelligence in autism persists into young adulthood and is linked to psychiatric co-morbidities. Journal of Autism and Developmental Disorders, 47(10), 3007–3017. https://doi.org/10.1007/s10803-017-3213-2
Magnuson, K. M., & Constantino, J. N. (2011). Characterization of depression in children with autism spectrum disorders. Journal of Developmental and Behavioral Pediatrics, 32(4), 332–340. https://doi.org/10.1097/DBP.0b013e318213f56c
Matson, J. L., & Cervantes, P. E. (2014). Commonly studies comorbid psychopathologies among persons with autism spectrum disorder. Research in Developmental Disabilities, 35, 952–962. https://doi.org/10.1016/j.ridd.2014.02.012
Mazzone, L., Ruta, L., & Reale, L. (2012). Psychiatric comorbidities in asperger syndrome and high functioning autism: Diagnostic challenging. Annuals of General Psychiatry, 11(16), 1–13. https://doi.org/10.1186/1744-859X-11-16
McGillivray, J. A., & Evert, H. T. (2014). Group cognitive behavioural therapy program shows potential in reducing symptoms of depression and stress among young people with ASD. Journal of Developmental Disorders, 44, 2041–2051. https://doi.org/10.1007/s10803-014-2087-9
Merikangas, K. R., He, J. P., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., et al. (2010). Lifetime prevalence of mental disorders in US adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. https://doi.org/10.1016/j.jaac.2010.05.017
Miller, P. R., Dasher, R., Collins, R., Griffiths, P., & Brown, F. (2001). Inpatient diagnostic assessments: 1. Accuracy of structured vs. unstructured interviews. Psychiatry Research, 105, 255–264.
Moretti, M. M., Fine, S., Haley, G., & Marriage, K. (1985). Childhood and adolescent depression: Child-report versus parent-report information. Journal of the American Academy of Child Psychiatry, 24(3), 298–302. https://doi.org/10.1016/S0002-7138(09)61090-6
Regier, D. A., Boyd, J. H., Burke, J. D., Rae, D. S., Myers, J. K., Kramer, M., et al. (1988). One-month prevalence of mental disorders in the United States: Based on five epidemiologic catchment area sites. Archives of General Psychiatry, 45(11), 977–986.
Richa, S., Fahed, M., Khoury, E., & Mishara, B. (2014). Suicide in autism spectrum disorders. Archives of Suicide Research, 18, 327–339. https://doi.org/10.1080/13811118.2013.82483
Riolo, S. A., Nguyen, T. A., Greden, J. F., & King, C. A. (2005). Prevalence of depression by race/ethnicity: Findings from the National Health and nutrition examination survey III. American Journal of Public Health, 95(6), 998–1000. https://doi.org/10.2105/AJPH.2004.047225
Ustün, T. B., Ayuso-Mateos, J. L., Chatterji, S., Mathers, C., & Murray, C. J. (2004). Global burden of depressive disorders in the year 2000. British Journal of Psychiatry, 184, 386–392.
van Steensel, F. J., Bögels, S. M., & Perrin, S. (2011). Anxiety disorders in children and adolescents with autistic spectrum disorders: A meta-analysis. Clinical Child and Family Psychology Review, 14(3), 302. https://doi.org/10.1007/s10567-011-0097-0
Wingate, M., Kirby, R. S., Pettygrove, S., Cunniff, C., Schulz, E., Ghosh, T., et al. (2014). Prevalence of autism spectrum disorders among children aged 8 years: Autism and developmental disabilities monitoring network, 11 sites, United States, 2010. Morbidity and Mortality Weekly Surveillance Summaries, 63, 1–22.
World Health Organization. (2017). Autism spectrum disorders: Fact sheet. Retrieved from: http://www.who.int/mediacentre/factsheets/autism-spectrum-disorders/en.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
Meta-analyses are exempt from research ethics board review because the data is collected from publically available information.
Informed Consent
Because the study did not involve interaction with participants, informed consent was not required.
Electronic supplementary material
ESM 1
(DOCX 122 kb)
Rights and permissions
About this article
Cite this article
Hudson, C.C., Hall, L. & Harkness, K.L. Prevalence of Depressive Disorders in Individuals with Autism Spectrum Disorder: a Meta-Analysis. J Abnorm Child Psychol 47, 165–175 (2019). https://doi.org/10.1007/s10802-018-0402-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-018-0402-1