Abstract
Chronic glomerulonephritis is the second most common reason, after diabetic nephropathy, for initiation of dialysis in Japan and IgA nephropathy (IgAN) is the most prevalent form of chronic glomerulonephritis. In the half century since IgAN was initially reported, our understanding of the long-term prognosis, clinical and histological features, pathogenesis of onset and progression, risk factors for progression, and appropriate treatment under different clinical and histological conditions, has steadily increased. Strong experimental and clinical evidence, the Clinical Practice Guidelines for IgA Nephropathy in Japan, the Oxford Classification, and the Kidney Disease Improving Global Outcomes guidelines have all contributed to the appropriate treatment of IgAN. Several intensive therapies, such as tonsillectomy, steroid therapy, and their combinations, can result in clinical remission, and prevent the progression to end stage renal disease (ESRD). However, some IgAN patients still progress to ESRD even when treated with intensive therapies. In this review, we discuss the clinical and histological features of IgAN, focusing primarily on our previous reports, and our opinions on therapeutic strategies for IgAN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Half a century has passed since Berger et al. first described IgA nephropathy (IgAN) in 1968 [1]. Initially, IgAN was considered a benign disease because of its clinical and histological features of being associated with few cases of nephrotic syndrome, rapidly progressive glomerulonephritis, and crescentic glomerulonephritis. In the 1970s, intensive treatments, such as steroids, tonsillectomy, and immunosuppressive agents, were not provided to patients with IgAN. However, in the 1980s and 1990s, long-term survival analyses over 10–20 years revealed that the disease was not so benign, as 40% of IgAN patients had progressed to end-stage renal disease (ESRD) within 20 years [2,3,4]. Subsequently, several studies were performed to identify risk factors and appropriate treatments to prevent progression to ESRD.
Several investigators have identified risk factors associated with progression to ESRD (Table 1). In Japan, the Clinical Practice Guidelines for IgA Nephropathy were first reported in 1995 [5] and subsequently underwent minor revision in 2002 [6]. As per these guidelines, prognosis was divided into four groups according to histological features: good, relatively good, relatively poor, and poor. In contrast, clinical parameters such as creatinine (Cr), Cr clearance, the level of urinary protein excretion (U-Prot), and blood pressure were recognized only as supplementary parameters. However, the relative importance of these clinical parameters was re-evaluated, and the guidelines underwent major revision in 2011 (third edition) [7, 8]. In the third edition, U-Prot and estimated glomerular filtration rate (eGFR) were selected as clinical risk factors, while crescents, segmental sclerosis, and global sclerosis were selected as histological risk factors. In 2009, the first international histological classification, the Oxford Classification, was reported [9, 10] from a working group of the international IgA Nephropathy Network and the Renal Pathology Society. Mesangial hypercellularity, endothelial hypercellularity, segmental sclerosis or adhesion, and interstitial fibrosis/tubular atrophy were selected as risk factors. In 2016, the Oxford Classification was revised to include cellular and fibrocellular crescents [11].
Regarding treatment, the beneficial effects of corticosteroid therapy were first described by Kobayashi et al. in 1996 [12, 13], although this was in a retrospective cohort analysis. In 1999, Pozzi et al. [14] reported the results of a randomized controlled trial (RCT) to demonstrate the effects of intermittent steroid pulse (SP) therapy. The long-term follow-up results of this RCT were also reported in 2004 [15]. This form of SP therapy is one of the strongest evidence-based treatments in the world. In Japan, Hotta et al. [16] reported that combined tonsillectomy and corticosteroid therapy was the most effective treatment regimen to achieve clinical remission of IgAN, and those who achieved remission did not progress to ESRD. Following the report by Hotta et al., the number of IgAN patients who underwent tonsillectomy combined with SP (TSP) therapy [17] and the number of institutions that performed TSP therapy [18] increased dramatically in Japan. Moreover, a Japanese multicenter RCT that compared TSP and SP according to Pozzi’s regimen was undertaken, and its results indicated that TSP had a beneficial effect in decreasing U-Prot compared with SP [19].
In summary, the risk factors, guidelines, and treatments for IgAN have changed dramatically over the last half century. In this review, we discuss the clinical and histological features of IgAN, and share our opinions on therapeutic strategies for IgAN described in our previous reports.
Long-term prognosis of IgAN
According to reports from the 1990s, roughly 40% of patients with a 20 year natural history of IgAN progressed to ESRD [3, 4]. In our total cohort from 1974 to 2011, renal survival rate was 84.3% over 10 years, 66.6% over 20 years, 50.5% over 30 years, and 46.6% over 35 years [20]. These results were similar to previous observations, and the 35 year prognosis represents the longest analysis to date. A single group from Korea reported the 30 year prognosis, and found that the composite outcome of mortality and renal survival rates over 10, 20, and 30 years was 79.8, 66.9, and 62.5%, respectively [21]. According to these results, IgAN appears to be associated with poor prognosis. However, recent therapeutic strategies, such as oral prednisolone (oPSL), SP therapy, TSP therapy, renin-angiotensin system inhibitors (RASIs), and other supportive therapies, such as fish oil, statins, and antiplatelet agents, have improved prognosis [20, 22]. In our previous reports, mean arterial pressure, eGFR, serum albumin, serum uric acid (UA), total cholesterol (T-Cho), U-Prot, IgA/C3 ratio, and T lesions as per the Oxford Classification of histology were identified as risk factors by univariate Cox regression analysis. Among these risk factors, multivariate analysis showed that eGFR, U-Prot, and UA were associated with renal prognosis. The eGFR and U-Prot results were consistent with clinical guidelines in Japan [7, 8].
Deteriorated renal function as a risk factor for IgAN
The deterioration of renal function is a severe risk factor for progression to ESRD in IgAN. In our previous reports, a 20 ml/min/1.73 m2 decline in eGFR increased the risk of progression to ESRD by 1.93 times [95% confidence interval (CI) 1.47–2.56, P < 0.0001] according to multivariate Cox regression analysis [20]. According to the Clinical Practice Guidelines for IgA Nephropathy in Japan [7, 8], the risk of progressing to ESRD in patients with C-grade III (defined as eGFR < 60 ml/min/1.73 m2 and U-Prot ≥ 0.5 g/day) is 42.5 times higher than in patients with C-grade I (defined as U-Prot < 0.5 g/day), although the risk of progression to ESRD in patients with C-Grade II (defined as eGFR ≥ 60 ml/min/1.73 m2 and U-Prot ≥ 0.5 g/day) is 6.4 times higher than that in patients with C-grade I [23]. In a nationwide prospective cohort study of 2,269 IgAN patients in 97 centers in Japan, Cr was reported as the severest and most important risk factor compared with others such as sex, age, blood pressure, proteinuria, hematuria, serum albumin, and histological findings [24, 25]. This study was validated in 633 Caucasians in a Norwegian cohort study, which used eGFR instead of Cr. In multivariate analysis, risk of progression to ESRD was 3.1 times higher for chronic kidney disease (CKD) grade 3, 10.1 times higher for CKD grade 4, and 31.2 times higher for CKD grade 5 in comparison with CKD grade 1 [26].
As described above, it is disputable whether deteriorated renal function is a risk factor for progression, and prevention of progression to ESRD in advanced IgAN remains challenging. In advanced IgAN patients with deterioration of renal function, histological features are important factors in determining method of treatment. If active lesions such as mesangial hypercellularity, endothelial hypercellularity, and cellular and fibrocellular crescents are still present, corticosteroid therapy has the potential to prevent progression to ESRD, or at least delay it. In our previous study [27], oPSL decreased U-Prot and delayed the increase in Cr. We used oPSL because the mean ratio of cellular and fibrocellular crescents was high (17.2%), as was that of global sclerosis (23.9%). Corticosteroid therapy appeared to be effective for active lesions, and decreased U-Prot and delayed progression to ESRD. Notably, a significant amount of glomerular hyperfiltration in the remaining glomeruli is observed in advanced IgAN patients because of global sclerosis. RASIs, such as angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, aldosterone blockers, and direct renin inhibitors, are effective for these patients by decreasing glomerular hypertension and hyperfiltration through dilatation of the efferent arteriole of glomeruli. RASIs are more beneficial for long-term renal survival compared with antiplatelet agents [28], and have effects similar to oPSL [29, 30], SP therapy [31], and TSP therapy [31] in IgAN patients with eGFR < 60 ml/min/1.73 m2. It is important to select appropriate treatments according to histological features in patients with advanced IgAN with deterioration of renal function. At minimum, administration of treatment with RASIs according to the physiological state of glomeruli might be considered.
Proteinuria in IgAN
Proteinuria is the best evaluable marker of treatment response and the best surrogate marker for predicting prognosis. High level of U-Prot is a risk factor for progression to ESRD. Our previous multivariate analysis showed that an increase of U-Prot by 1.0 g/day increased the risk of progression to ESRD by 1.34 times (95% CI 1.07–1.69, P = 0.0116) [20]. We found similar results in a nationwide multicenter retrospective cohort study to establish the Clinical Practice Guideline for IgA Nephropathy in Japan [23]. In that study, risk of progression to ESRD was increased 1.69 times by a 1.0 g/day increase in U-Prot in multivariate analysis adjusted by clinical findings and 1.61 times when adjusted for clinical findings and treatment [23]. In the above-described nationwide survey in Japan [24, 25], U-Prot was recognized as the second most common risk factor after renal function. Recently, the importance of mean U-Prot of follow-up (time-average proteinuria: TAp) has been reported [32, 33]. Of course, it is important to predict outcome from clinical findings at the time of renal biopsy. Several treatments have been reported to decrease U-Prot during follow-up, and in Japan the first goal of treatment is to achieve remission of U-Prot and hematuria [34]. Therefore, consideration of changes in U-Prot is also important in analyzing treatment response and predicting prognosis.
Although IgAN with nephrotic syndrome is rare and occurs only in 5–10% of IgAN patients [35], it seems to be important because of its severe prognosis and lack of appropriate treatment. In our previous report [35], 42 cases of IgAN with nephrotic syndrome were identified among 954 IgA patients (4.4%), and had severe renal function impairment (mean eGFR: 51.1 ml/min/1.73 m2), high level of U-Prot (mean 5.76 g/day), and urinary red blood cells (U-RBC) (mean 50/HPF). As per the Oxford Classification, M1: 60.0%, E1: 32.9%, S1: 82.9%, T1: 40.0%, T2: 25.7%, C1: 54.3%, and C2: 17.1% were observed, and were more severe than in non-nephrotic IgAN. The cumulative 15-year renal survival rate was only 25.3%, and 74.5% in non-nephrotic IgAN. Lower eGFR, Oxford T lesions, and no steroid treatment were independent risk factors for progression to ESRD by multivariate Cox regression analysis. In the Korean cohort, renal survival rate was also poor. The results over 8 years showed that renal survival was about 40% in IgAN patients with nephrotic syndrome and about 75% in those with non-nephrotic IgAN [36].
To prevent progression to ESRD, decreasing the level of U-Prot is important [36]. In this regard, analysis of TAp might be important, and appropriate treatment to decrease TAp is required.
Hematuria in IgAN
In recent years, hematuria has been recognized as a consequence of inflammation of glomerular capillaries, which is related to active glomerular lesions such as tuft necrosis, endothelial hypercellularity, and cellular and fibrocellular crescents. In several Asian studies of IgAN patients with mild proteinuria, hematuria was one of the risk factors for progression to hypertension, increase of proteinuria and progression to ESRD [37,38,39]. On the contrary, a Spanish study showed that few Caucasian patients had increased proteinuria and progression to ESRD [40]. However, another Spanish study showed that persistent hematuria was an independent risk factor for progression to ESRD [41], similar to TAp. In our cohort of 1,012 IgAN patients [20], U-RBC was not a risk factor for progression by univariate analysis (HR: 1.02, 95% CI 0.92–1.13, P = 0.6851). In Japan, U-RBC is not recognized as a risk factor of progression to ESRD in the Clinical Practice Guidelines for IgA Nephropathy [7, 23]. A nationwide survey in Japan also showed that mild hematuria (U-RBC ≤ 30/HPF) was an independent risk factor for progression, while severe hematuria was not [25, 42]. Hematuria is still seen as the most controversial risk factor for progression of IgAN. In our previous study, in IgAN patients with mild proteinuria (≤ 0.5 g/day at the time of renal biopsy), a higher level of U-RBC did not affect renal prognosis [43]. Additionally, in IgAN patients with moderate-to-severe proteinuria (≥ 1.0 g/day at the time of renal biopsy), a higher level of U-RBC did not affect the response to steroid treatment or outcome [44]. Moreover, there was no relationship between the level of U-RBC and the severity of active histological lesions [44]. In recent years, low vacuum-scanning electron microscopy has revealed the presence of large gaps, thinning, and alterations of the glomerular basement membrane (which are generally observed in patients with thin basement membrane disease) in IgAN patients in addition to active lesions [45]. These additional alterations may affect the indefinite relationship between the hematuria and outcome of IgAN, although hematuria is considered the primary result of active histological lesions. The clinical importance of hematuria is still unresolved in IgAN.
Other risk factors in IgA nephropathy
Uric acid and other metabolic factors
Recently, metabolic factors such as dyslipidemia, obesity, hypertension (HT), and impaired fasting glucose have been reported to relate to onset and progression of CKD [46, 47]. IgAN is also one of the CKDs, and the above factors are also reported to have a relationship with progression of IgAN [48,49,50]. Higher T-Cho, body mass index, and blood pressure are also independent factors for progression to ESRD in univariate analysis, and higher UA was an independent risk factor in both univariate and multivariate analysis in our previous study [20]. Hyperuricemia (HU) induces oxidative stress, which decreases endothelial nitric oxide expression and increases endothelial dysfunction, resulting in glomerular hypertension. HU also results in proliferation of vascular smooth muscle cells in preglomerular arteries with activation of the RAS [51]. In IgAN, a 1.0 mg/dl increase of UA increased the risk of progression to ESRD by 1.24 times (95% CI 1.04–1.48, P = 0.0176) in our cohort [20] and 1.17 times (95% CI 1.08–1.27, P < 0.001) in a large Chinese cohort (n = 1965) by multivariate Cox regression analysis [52]. Until progression to CKD stage G3a without decreasing UA, global glomerular sclerosis due to HU was increased in addition to the histological features caused by IgAN. Furthermore, the risk of progression to ESRD was also increased compared with IgAN with normal UA [53]. Therefore, until progression to CKD stage G3a, controlling HU appears to be important.
Age
Given the current aging society in Japan, aging in IgAN patients is an important factor to consider, although IgAN frequently occurs in younger people. In our cohort, mean age at diagnosis was 32.9 years [20]. In a Japanese cohort from a nationwide survey, among 5679 patients with IgAN, only 497 (8.8%) patients were > 65 years old [54]. As renal function (eGFR) gradually decreases with age, histological findings also change. Global and focal segmental sclerosis, tubular atrophy and interstitial changes, and arterio- and arteriolosclerosis are increased, as shown by light microscopy [55]. In older IgAN patients (≥ 60 years old) in our cohort [56], blood pressure, blood urea nitrogen, UA, T-Cho, U-Prot, and N-acetyl-β-d-glucosaminidase were significantly higher, while total protein, albumin, and eGFR were significantly lower than in middle-aged (40–59 years old), and/or younger (20–39 years old) patients. Older IgAN patients were associated with higher numbers of T lesions as per the Oxford Classification compared with younger patients, although the number of active lesions, such as M1 and E1 was similar. The grade of arteriolosclerosis was significantly higher in older IgAN patients compared with middle-aged and younger patients. In total, 51.6% of older IgAN patients were treated with corticosteroids, and 67.7% of patients were treated with RASIs. However, cumulative renal survival rate was poor (22.9%/19 years), and was significantly lower than that of middle-aged (69.2%/20 years) and younger patients (84.9%/20 years) [56]. The most important factor for preventing progression to ESRD was reducing proteinuria by therapeutic intervention [57]. Older IgAN patients frequently have active and chronic histological lesions associated with IgAN, in addition to chronic lesions associated with aging, HT, HU, and dyslipidemia (DL). Therefore, careful treatment of IgAN and other risk factors is required.
Histopathological features and glomerular depositions
Histopathological features, such as mesangial hypercellularity, endocapillary proliferation, cellular and fibrocellular crescents as active lesions, global and segmental sclerosis, fibrous crescents, increased amounts of mesangial matrix, glomerular tuft adhesions to Bowman’s capsule, and tubulointerstitial change as chronic lesions, are important factors for prognostic prediction of IgAN, as well as clinical findings, such as renal function and U-Prot (Table 1). Several histological grading systems for analyzing the above histological factors have been reported in the past half century [58,59,60]; however, no global consensus has been reached. The Oxford Classification has been used worldwide under global consensus since its introduction [9,10,11]. In Japan, the third edition of the Clinical Practice Guidelines for IgA Nephropathy has also been used to evaluate the histopathological findings [7, 8]. However, it has been controversial whether the glomerular immune deposits are predictive markers of prognosis. According to Suzuki, the pathogenesis of IgAN is considered a multi-hit process [61]. Hit 1 is the secretion of galactose-deficient (Gd) IgA1 into the circulation, Hit 2 is the production of IgG or IgA autoantibodies against the Gd-IgA1 hinge region, Hit 3 is the formation of immune complexes with Gd-IgA1, and Hit 4 is glomerular deposition of Gd-IgA1 and subsequent glomerular injury. From the perspective of a multi-hit pathogenesis, IgG deposition appears to be the critical event associated with pathogenesis, disease activity, and prognosis. In our cohort, IgG deposition was related to glomerular tuft adhesions to Bowman’s capsule, although there was no correlation with other histological or clinical findings, or renal prognosis [62]. Other studies indicated that IgG deposition was related to U-Prot, eGFR, and T lesions as per the Oxford Classification, and was an independent risk factor for progression to ESRD (HR 2.9, 95% CI 1.6–5.3, P = 0.001) by multivariate analysis [63]. It was also shown that IgG deposition was related to poor complete remission of urinary parameters by multivariate analysis (HR 0.31, 95% CI 0.12–0.77, P = 0.016), and poor renal prognosis [64]. Recently, the deposition of Gd-IgA was detected by immunofluorescence analysis [65]. Therefore, further research will clarify the importance of the colocalization of IgG and Gd-IgA deposits with regard to the pathogenesis of IgAN.
Treatment of IgAN
TSP therapy
The Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend RASIs to reduce proteinuria in IgA patients with U-Prot > 1 g/day. In IgAN patients with persistent proteinuria, corticosteroid therapy is recommended instead of conservative therapies [66]. Combined corticosteroid therapy with RASIs was reported to reduce proteinuria and prevent progression to ESRD in several RCTs [67, 68]. SP therapy was also reported to have beneficial effects on IgAN by Pozzi et al. [14, 15]. However, in Japan, TSP therapy has become the primary treatment for IgAN, and many clinical studies have analyzed its beneficial effects since the report by Hotta et al. [16]. In IgAN patients with U-Prot ranging from 1.0 to 3.5 g/day, and Cr < 1.5 mg/dl according to inclusion criteria of Pozzi’s RCT [14, 15], the decrease in U-Prot from baseline during the 12 months after TSP therapy was significantly higher than after SP therapy (coefficient estimate: −1.316, 95% CI −2.617 to −0.015, P = 0.047) [19]. Additionally, multivariate logistic regression analysis showed that TSP therapy was an independent factor for the resolution of proteinuria (odds ratio: 2.98, 95% CI 1.01–8.83, P = 0.049), although the effect on remission of U-RBC and both U-Prot and U-RBC was similar to that of SP therapy in a multicenter RCT [19]. Komatsu et al. performed a prospective controlled study that compared TSP and SP therapy. TSP therapy significantly decreased U-Prot and U-RBC, and multivariate analysis indicated that TSP therapy was an independent factor that contributed to remission of U-Prot (HR: 6.20, 95% CI 1.98–19.50, P = 0.002) [69]. In our cohort, TSP therapy was associated with a significantly higher rate of remission of U-RBC and urinary abnormalities (clinical remission) compared with SP therapy [70], there was also a significantly higher rate of remission of U-RBC, U-Prot, and both, and the renal survival rate was significantly improved compared with oPSL therapy [71]. It was recently reported that the production of Gd-IgA1 is related to tonsillar Toll-like receptor (TLR)-9, a proliferation-inducing ligand (APRIL) in tonsillar B cells, and B cell-activating factor belonging to TNF (BAFF) in tonsils [61, 72,73,74,75]. APRIL expression in tonsillar B cells was induced by TLR-9 and correlated with disease activity [75]. These results indicate that tonsillectomy is an appropriate treatment for IgAN. However, worldwide, it cannot be confirmed that tonsillectomy is a well-recognized treatment for IgAN, especially in Europe [76]. Tonsillectomy may be considered overtreatment and as such has not been recognized as an appropriate treatment in Europe, because there is a lack of an appropriate protocol that accommodates different IgAN patients. In reality, the protocol regarding the number of SP treatments in TSP therapy (three vs. one) is not related to the ratio of IgAN patients who achieved remission of U-Prot, U-RBC, and both [77]. Moreover, in IgAN patients with U-Prot < 1.0 g/g Cr or IgAN patients with CKD G3, there was no significant difference in 20-year renal survival rate among those treated with TSP, SP, oPSL, and RASI [31]. These results indicate that the protocol for TSP therapy should be adjusted according to disease activity in each IgAN patient. Short duration of nephropathy may have beneficial effects for achieving clinical remission [78]. However, there are some IgAN patients who will not progress to ESRD despite a lack of therapeutic intervention, such as TSP therapy, tonsillectomy, SP therapy, oPSL, RASIs, or even antiplatelet agents. We are currently facing a dilemma regarding the goal of treatment for IgAN [79].
Other supportive therapies
In this section, we describe the effects of fish oil and statins that are used to treat DL. There is insufficient evidence for these therapies because of a lack of large RCTs, and their effectiveness remains controversial for the treatment of IgAN. However, these therapies also have antiarteriosclerotic effects, and given that glomeruli are aggregations of arteries, they may have beneficial effects on the progression of glomerulosclerosis and diminished renal function. Moreover, during the long-term period from onset of IgAN to the end of life, cerebrocardiovascular events are risk factors for progression to ESRD or death, and these therapies may also have beneficial effects on such life-threatening events in IgAN patients.
Fish oil
Fish oil contains substantial amounts of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) as polyunsaturated fatty acids (PUFAs). PUFAs have been reported to have anti-inflammatory effects that block several inflammatory cytokines/cascades, such as tumor necrosis factor-α [80], interleukin-6 [81], and cyclooxygenase-2 [81, 82]. Moreover, PUFAs have been shown to inhibit expression of profibrotic genes such as transforming growth factor-β, fibronectin, connective tissue growth factor, and type IV collagen [83] in mesangial cells and in a mouse model of IgAN [81, 84, 85]. In 1984, EPA and DHA therapy were first reported to improve renal function for 1 year compared with nonsupplemented control subjects [86]. Subsequently, several RCTs were performed and a meta-analysis of the results revealed beneficial effects in reducing U-Prot, but not in preserving renal function. In addition, their antiproteinuric effects were not dose-dependent [87]. In our previous study [88], 1 year treatment with EPA combined with RASIs decreased U-Prot when compared with dilazep combined with RASIs (median U-Prot: baseline: 0.80, after 1 year: 0.41 g/g Cr with EPA, P < 0.001; and baseline: 0.88, after 1 year: 0.60 g/g Cr with dilazep, not significant). In another study [89], additional treatment with DHA and EPA stabilized renal function (median %ΔeGFR: before addition of DHA: −7.35% for 6 months, and after addition of DHA: +1.26% for 6 months, P = 0.0132) in advanced IgAN with deterioration of renal function (mean eGFR 48.3 ml/min/1.73 m2). Its pleiotropic effects were beyond the antiproteinuric, antihypertensive, and antidyslipidemic effects. Although these studies were small retrospective analyses, and the effects of PUFAs on IgAN remain controversial, PUFAs have potential for IgAN because of their pleiotropic effects and ease of use without severe adverse events. We believe PUFA may represent a therapeutic strategy for use in future large RCTs for the treatment of IgAN.
Statins
Recently, the evidence of beneficial effects of statins on cardiovascular events and progression to ESRD in CKD patients has dramatically increased [90], although there is a lack of strong evidence for their effect in IgAN. Following suppression of glomerular inflammation in IgAN by immunosuppressive therapies such as TSP, SP, or oPSL, the primary goal for the treatment of IgAN is changed to management of CKD to control and reduce risk factors such as HT, HU, DL, and obesity. Statins may have beneficial effects in IgAN that prevent progression to ESRD. In our previous study [91], in 24 patients with deterioration of renal function (mean eGFR: 55.8 ml/min/1.73 m2), mean %ΔeGFR was −5.9% for 1 year before statin treatment was started, and was significantly increased to 2.4% for 1 year after statin treatment was started (P = 0.0098). In other studies, the beneficial effects of statins on IgAN, such as antiproteinuric effects [92, 93], anti-inflammatory effects [94, 95], and stabilization of renal function [92, 93] were described, although the evidence was weak. We anticipate that strong evidence for the use of statins in preventing progression to ESRD in IgAN will be reported in the future.
Therapeutic strategies for IgAN
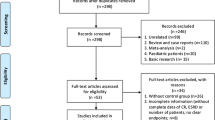
A therapeutic strategy for IgAN is shown in Fig. 1. The initial step in the development of IgAN is a mucosal infection. Therefore, tonsillectomy is important for removing this trigger and to stop subsequent production of Gd-IgA1. Tonsillectomy also suppresses the relapse of nephropathy in IgAN patients after achieving clinical remission by reducing the risk of tonsillitis and mucosal infections in the future. Furthermore, epipharyngeal abrasive therapy and oral care may have beneficial effects on the treatment of IgAN, although there is no evidence supporting this. Corticosteroid therapy is the most effective method of suppressing Gd-IgA1, immune complexes with Gd-IgA1, and mesangial IgA deposition, owing to its immunosuppressive effects. Other immunosuppressive agents, such as cyclophosphamide, calcineurin inhibitors (tacrolimus and cyclosporin A), and antimetabolites (azathioprine, mycophenolate mofetil, and mizoribine) may affect these factors because of their mechanism of action. However, there is currently no strong supporting evidence, and recommendations in the KDIGO guidelines are relatively weak [66]. The anti-inflammatory effects of corticosteroid therapy suppress glomerular inflammation, such as mesangial hypercellularity, endothelial hypercellularity, tuft necrosis, and cellular and fibrocellular crescents. It is critical to suppress active lesions in IgAN as soon as possible, before glomerular inflammation spreads diffusely and globally to other glomeruli. If there are no active lesions in glomeruli, corticosteroid therapy should be carefully considered, referring to clinical findings and the patient’s social background (age, sex, marital status, future pregnancy intentions, and occupation). After active lesions are suppressed, prognosis depends on the stress on the remaining glomeruli in the form of glomerular hyperfiltration and glomerular hypertension, as well as on CKD management. RASIs are most effective treatment to reduce glomerular hyperfiltration and hypertension. Once RASIs are started, they should be continued until progression to ESRD, because hyperfiltration and glomerular hypertension in the remaining glomeruli will become severe, along with the deterioration of renal function and the continuous decline in the number of remaining glomeruli. Importantly, hyperkalemia and teratogenicity must also be considered carefully. In CKD management, the risk factors for progression of CKD, such as HT, DL, HU, and obesity, should be well controlled. The onset of other diseases in the future, such as diabetes mellitus, cerebrocardiovascular disease, malignancy, systemic disease, and other visceral diseases represent a risk factor for the deterioration of renal function. Since the peak age at onset of IgAN is relatively young, IgAN patients must be treated with careful consideration of the need for long-term observation.
Onset, progression, and treatment of IgA nephropathy. After mucosal infection, production of Gd-IgA1 and subsequent formation of immune complexes with Gd-IgA1 and IgG autoantibodies occur. They induce glomerular IgA deposition and subsequent glomerular injury. Glomerular active lesions progress to chronic lesions, and chronic lesions induce glomerular hypertension and hyperfiltration in the remaining glomeruli, culminating in ESRD. Tonsillectomy suppresses the production of Gd-IgA1, while corticosteroid therapy suppresses the circulation and deposition of Gd-IgA1 through immunosuppressive mechanisms and suppresses active glomerular lesions through anti-inflammatory mechanisms. Glomerular hypertension and hyperfiltration in the remaining glomeruli induced by chronic glomerular lesions are treated by RASIs. The control of other risk factors, such as HT, DL, HU, and obesity is also important for the progression of CKD in IgAN
Conclusions
In this review, clinical and pathological characteristics and therapeutic strategies for IgAN were discussed. IgAN is a slow but progressive disease with various active and chronic histological lesions, mild-to-moderate proteinuria, and several degrees of hematuria. Appropriate treatment to adjust for the different histological and clinical features should be provided. Fortunately, recent therapeutic interventions have improved prognosis of the disease. Moreover, along with furthering of our understanding of the pathogenesis of IgAN, new treatments such as biologics and mucosa-related therapies have been trialed. In the future, we believe it will be possible to prevent the progression to ESRD in all IgAN patients.
References
Berger J, Hinglais N. Les dépôts intercapillaries d’IgA-IgG. J Urol Nephrol. 1968;74:694–5.
D’Amico G. Clinical features and natural history in adults with IgA nephropathy. Am J Kidney Dis. 1988;12:353–7.
Alamartine E, Sabatier JC, Guerin C, Berliet JM, Berthoux F. Prognostic factors in mesangial IgA glomerulonephritis: an extensive study with univariate and multivariate analysis. Am J Kidney Dis. 1991;18:12–9.
Koyama A, Igarashi M, Kobayashi M. Coworkers of the research group on progressive renal disease: natural history and risk factors for immunoglobulin A nephropathy in Japan. Am J Kidney Dis. 1997;29:526–32.
Sakai H, Abe K, Kobayashi Y, Koyama A, Shigematsu H, Harada T, Yoshikawa N, Arakawa M, Itoh H, Osawa K, Sakai O, Dohi K, Yamanaka N, Nagasawa T, Kurokawa K. Clinical guidelines of IgA nephropathy. Jpn J Nephrol. 1995;37:417–21.
Tomino Y, Sakai H. Special study group (IgA nephropathy) on progressive glomerular disease clinical guidelines for immunoglobulin A(IgA) nephropathy in Japan, second version. Clin Exp Nephrol. 2003;7:93–7.
Matsuo S, Kawamura T, Joh K, Utsunomiya Y, Okonogi H, Miyazaki Y, Koike K, Yokoo T, Matsushima M, Komura H, Ogura M, Horikoshi T, Suzuki Y, Furusu A, Kimura K, Yasuda T, Shirai S, Endo M, Hattori M, Akioka Y, Hirano K, Katafuchi R, Hisano S, Shimizu A, Hashiguchi A, Furukawa T, Tomino Y. Clinical guidelines for immunoglobulin A (IgA) nephropathy in Japan third version. Nippon Jinzo Gakkai Shi. 2001;53:123–35.
Yuzawa Y, Yamamoto R, Takahashi K, Katafuchi R, Tomita M, Fujigaki Y, Kitamura H, Goto M, Yasuda T, Sato M, Urushihara M, Kondo S, Kagami S, Yasuda Y, Komatsu H, Takahara M, Haraguchi Y, Kimura K, Matsuo S. Evidence-based clinical practice guidelines for IgA nephropathy 2014. Clin Exp Nephrol. 2016;20:511–35.
A Working Group of the International IgA Nephropathy Network and the Renal Pathology Society. The Oxford classification of IgA nephropathy: rationale, clinicopathological correlations, and classification. Kidney Int. 2009;76:534–45.
A Working Group of the International IgA Nephropathy Network and the Renal Pathology Society. The Oxford classification of IgA nephropathy: pathology definitions, correlations, and reproducibility. Kidney Int. 2009;76:546–56.
Trimarchi H, Barratt J, Cattran DC, Cook HT, Coppo R, Haas M, Liu ZH, Roberts IS, Yuzawa Y, Zhang H, Feehally J, IgAN Classification Working Group of the International IgA Nephropathy Network and the Renal Pathology Society; Conference Participants. Oxford classification of IgA nephropathy 2016: an update from the IgA Nephropathy Classification Working Group. Kidney Int. 2017;91:1014–21.
Kobayashi Y, Fujii K, Hiki Y, Tateno S. Steroid therapy in IgA nephropathy: prospective pilot study in moderate proteinuric cases. Q J Med. 1986;61:935–43.
Kobayashi Y, Hiki Y, Kokubo T, Horii A, Tateno S. Steroid therapy during the early stage of progressive IgA nephropaty. Nephron. 1996;72:237–42.
Pozzi C, Bolasco PG, Fogazzi GB, Andrulli S, Altieri P, Ponticelli C, Locatelli F. Corticosteroids in IgA nephropathy: a randomised controlled trial. Lancet. 1999;13(353):883–7.
Pozzi C, Andrulli S, Del Vecchio L, Melis P, Fogazzi GB, Altieri P, Ponticelli C, Locatelli F. Corticosteroid effectiveness in IgA nephropathy: long-term results of a randomized, controlled trial. Am J Soc Nephrol. 2004;15:157–63.
Hotta O, Miyazaki M, Furuta T, Tomioka S, Chiba S, Horigome I, Abe K, Taguma Y. Tonsillectomy and steroid pulse therapy significantly impact on clinical remission in patients with IgA nephropathy. Am J Kidney Dis. 2001;38:736–43.
Miura N, Imai H, Kikuchi S, Hayashi S, Endoh M, Kawamura T, Tomino Y, Moriwaki K, Kiyomoto H, Kohagura K, Nakazawa E, Kusano E, Mochizuki T, Nomura S, Sasaki T, Kashihara N, Soma J, Tomo T, Nakabayashi I, Yoshida M, Watanabe T. Tonsillectomy and steroid pulse (TSP) therapy for patients with IgA nephropathy: a nationwide survey of TSP therapy in Japan and an analysis of the predictive factors for resistance to TSP therapy. Clin Exp Nephrol. 2009;13:460–6.
Matsuzaki K, Suzuki Y, Nakata J, Sakamoto N, Horikoshi S, Kawamura T, Matsuo S, Tomino Y. Nationwide survey on current treatments for IgA nephropathy in Japan. Clin Exp Nephrol. 2013;17:827–33.
Kawamura T, Yoshimura M, Miyazaki Y, Okamoto H, Kimura K, Hirano K, Matsushima M, Utsunomiya Y, Ogura M, Yokoo T, Okonogi H, Ishii T, Hamaguchi A, Ueda H, Furusu A, Horikoshi S, Suzuki Y, Shibata T, Yasuda T, Shirai S, Imasawa T, Kanozawa K, Wada A, Yamaji I, Miura N, Imai H, Kasai K, Soma J, Fujimoto S, Matsuo S, Tomino Y, Special IgA Nephropathy Study Group. A multicenter randomized controlled trial of tonsillectomy combined with steroid pulse therapy in patients with immunoglobulin A nephropathy. Nephrol Dial Transpl. 2014;29:1546–53.
Moriyama T, Tanaka K, Iwasaki C, Oshima Y, Ochi A, Kataoka H, Itabashi M, Takei T, Uchida K, Nitta K. Prognosis in IgA nephropathy: 30 year analysis of 1,012 patients at a single center in Japan. PLoS One. 2014;9:e91756.
Lee H, Kim DK, Oh KH, Joo KW, Kim YS, Chae DW, Kim S, Chin HJ. Mortality of IgA nephropathy patients: a single center experience over 30 years. PLoS ONE. 2012;7:e51225.
Komatsu H, Fujimoto S, Hara S, Fukuda A, Fukudome K, Yamada K, Sato Y, Kitamura K. Recent therapeutic strategies improve renal outcome in patients with IgA nephropathy. Am J Nephrol. 2009;30:19–25.
Okonogi H, Kawamura T, Joh K, Koike K, Miyazaki Y, Ogura M, Tsuboi N, Hirano K, Matsushima M, Yokoo T, Horikoshi S, Suzuki Y, Yasuda T, Shirai S, Shibata T, Hattori M, Akioka Y, Katafuchi R, Hashiguchi A, Hisano S, Shimizu A, Kimura K, Maruyama S, Matsuo S, Tomino Y, Special IgA Nephropathy Study Group. A grading system that predicts the risk of dialysis induction in IgA nephropathy patients based on the combination of the clinical and histological severity. Clin Exp Nephrol. 2018. https://doi.org/10.1007/s10157-018-1657-0 [Epub ahead of print].
Wakai K, Kawamura T, Endoh M, Kojima M, Tomino Y, Tamakoshi A, Ohno Y, Inaba Y, Sakai H. A scoring system to predict renal outcome in IgA nephropathy: from a nationwide prospective study. Nephrol Dial Transplant. 2006;21:2800–8.
Goto M, Wakai K, Kawamura T, Ando M, Endoh M, Tomino Y. A scoring system to predict renal outcome in IgA nephropathy: a nationwide 10 year prospective cohort study. Nephrol Dial Transplant. 2009;24:3068–74.
Bjørneklett R, Vikse BE, Bostad L, Leivestad T, Iversen BM. Long-term risk of ESRD in IgAN; validation of Japanese prognostic model in a Norwegian cohort. Nephrol Dial Transpl. 2012;27:1485–91.
Moriyama T, Honda K, Nitta K, Yumura W, Nihei H. The effectiveness of steroid therapy for patients with advanced IgA nephropathy and deteriorated renal function. Clin Exp Nephrol. 2004;8:237–42.
Moriyama T, Amamiya N, Ochi A, Tsuruta Y, Shimizu A, Kojima C, Itabashi M, Takei T, Uchida K, Nitta K. Long-term beneficial effects of angiotensin-converting enzyme inhibitor and angiotensin receptor blocker therapy for patients with advanced immunoglobulin A nephropathy and impaired renal function. Clin Exp Nephrol. 2011;15:700–7.
Moriyama T, Amemiya N, Ochi A, Tsuruta Y, Shimizu A, Itabashi M, Takei T, Uchida K, Nitta K. Comparison of steroids and angiotensin receptor blockers for patients with advanced IgA nephropathy and impaired renal function. Am J Nephrol. 2011;34:233–40.
Moriyama T, Nakayama K, Ochi A, Amemiya N, Tsuruta Y, Kojima C, Itabashi M, Takei T, Uchida K, Nitta K. Comparison of inhibitors of renin-angiotensin-aldosterone system (RAS) and combination therapy of steroids plus RAS inhibitors for patients with advanced immunoglobulin A nephropathy and impaired renal function. Clin Exp Nephrol. 2012;16:231–7.
Hoshino J, Fujii T, Usui J, Fujii T, Ohashi K, Takaichi K, Suzuki S, Ubara Y, Yamagata K. Renal outcome after tonsillectomy plus corticosteroid pulse therapy in patients with immunoglobulin A nephropathy: results of a multicenter cohort study. Clin Exp Nephrol. 2016;20:618–27.
Reich HN, Troyanov S, Scholey JW, Cattran DC. Toronto glomerulonephritis registry. Remission of proteinuria improves prognosis in IgA nephropathy. J Am Soc Nephrol. 2007;18:3177–83.
Sarcina C, Tinelli C, Ferrario F, Visciano B, Pani A, De Silvestri A, De Simone I, Del Vecchio L, Terraneo V, Furiani S, Santagostino G, Corghi E, Pozzi C. Corticosteroid treatment influences TA-proteinuria and renal survival in IgA nephropathy. PLoS One. 2016;14:e0158584.
Suzuki Y, Matsuzaki K, Suzuki H, Sakamoto N, Joh K, Kawamura T, Tomino Y, Matsuo S. Proposal of remission criteria for IgA nephropathy. Clin Exp Nephrol. 2014;18:481–6.
Moriyama T, Nakayama K, Iwasaki C, Ochi A, Tsuruta Y, Itabashi M, Tsukada M, Takei T, Uchida K, Nitta K. Severity of nephrotic IgA nephropathy according to the Oxford classification. Int Urol Nephrol. 2012;44:1177–84.
Kim JK, Kim JH, Lee SC, Kang EW, Chang TI, Moon SJ, Yoon SY, Yoo TH, Kang SW, Choi KH, Han DS, Kie JH, Lim BJ, Jeong HJ, Han SH. Clinical features and outcomes of IgA nephropathy with nephrotic syndrome. Clin J Am Soc Nephrol. 2012;7:427–36.
Szeto CC, Lai FM, To KF, Wong TY, Chow KM, Choi PC, Lui SF, Li PK. The natural history of immunoglobulin A nephropathy among patients with hematuria and minimal proteinuria. Am J Med. 2001;110:434–7.
Shen P, He L, Li Y, Wang Y, Chan M. Natural history and prognostic factors of IgA nephropathy presented with isolated microscopic hematuria in Chinese patients. Nephron Clin Pract. 2007;106:157–61.
Shen P, He L, Huang D. Clinical course and prognostic factors of clinically early IgA nephropathy. Neth J Med. 2008;66:242–7.
Gutiérrez E, Zamora I, Balları´n JA, Arce Y, Jime´nez S, Quereda C, Olea T, Martı´nez-Ara J, Segarra A, Bernis C, Garcı´a A, Goicoechea M, de Garcı´a-Vinuesa S, Rojas-Rivera J, Praga M, Grupo de Estudio de Enfermedades Glomerulares de la Sociedad Espan˜ola de Nefrologı´a (GLOSEN). Long-term outcomes of IgA nephropathy presenting with minimal or no proteinuria. J Am Soc Nephrol. 2012;23:1753–60.
Sevillano AM, Gutiérrez E, Yuste C, Cavero T, Mérida E, Rodríguez P, García A, Morales E, Fernández C, Martínez MA, Moreno JA, Praga M. Remission of Hematuria Improves Renal Survival in IgA Nephropathy. J Am Soc Nephrol. 2017;28:3089–99.
Goto M, Kawamura T, Wakai K, Ando M, Endoh M, Tomino Y. Risk stratification for progression of IgA nephropathy using a decision tree induction algorithm. Nephrol Dial Transpl. 2009;24:1242–57.
Tanaka K, Moriyama T, Iwasaki C, Takashi T, Nitta K. Effect of hematuria on the outcome of IgA nephropathy with minimal or no proteinuria. Clin Exp Nephrol. 2016;26:107–12.
Iwasaki C, Moriyama T, Tanaka K, Takei T, Nitta K. Effect of hematuria on the outcome of IgA nephropathy with proteinuria. J Nephropathol. 2016;5:72–8.
Masuda Y, Yamanaka N, Ishikawa A, Kataoka M, Arai T, Wakamatsu K, Kuwahara N, Nagahama K, Ichikawa K, Shimizu A. Glomerular basement membrane injuries in IgA nephropathy evaluated by double immunostaining for α5(IV) and α2(IV) chains of type IV collagen and low-vacuum scanning electron microscopy. Clin Exp Nephrol. 2015;19:427–35.
Rashidbeygi E, Safabakhsh M, Delshad Aghdam S, Mohammed SH, Alizadeh S. Metabolic syndrome and its components are related to a higher risk for albuminuria and proteinuria: evidence from a meta-analysis on 10,603,067 subjects from 57 studies. Diabetes Metab Syndr. 2019;13:830–43.
Thomas G, Sehgal AR, Kashyap SR, Srinivas TR, Kirwan JP, Navaneethan SD. Metabolic syndrome and kidney disease: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2011;6:2364–73.
Syrjänen J, Mustonen J, Pasternack A. Hypertriglyceridaemia and hyperuricemia are risk factors for progression of IgA nephropathy. Nephrol Dialysis Transplant. 2000;15:34–42.
Shimamoto M, Ohsawa I, Suzuki H, Hisada A, Nagamachi S, Honda D, Inoshita H, Shimizu Y, Horikoshi S, Tomino Y. Impact of body mass index on progression of IgA nephropathy among japanese patients. J Clin Lab Anal. 2015;29:353–60.
D’Amico G. Natural history of idiopathic IgA nephropathy and factors predictive of disease outcome. Semin Nephrol. 2004;24:179–96.
Johnson RJ, Nakagawa T, Jalal D, Sánchez-Lozada LG, Kang DH, Ritz E. Uric acid and chronic kidney disease: which is chasing which? Nephrol Dial Transplant. 2013;28:2221–8.
Zhu B, Yu DR, Lv JC, Lin Y, Li Q, Yin JZ, Du YY, Tang XL, Mao LC, Li QF, Sun Y, Liu L, Li XF, Fei D, Wei XY, Zhu CF, Cheng XX, Chen HY, Wang YJ. Uric Acid as a Predictor of Immunoglobulin A nephropathy progression: a cohort study of 1965 cases. Am J Nephrol. 2018;48:127–36.
Moriyama T, Itabashi M, Takei T, Kataoka H, Sato M, Shimizu A, Iwabuchi Y, Nishida M, Uchida K, Nitta K. High uric acid level is a risk factor for progression of IgA nephropathy with chronic kidney disease stage G3a. J Nephrol. 2015;28:451–6.
Komatsu H, Fujimoto S, Yoshikawa N, Kitamura H, Sugiyama H, Yokoyama H. Clinical manifestations of Henoch-Schönlein purpura nephritis and IgA nephropathy: comparative analysis of data from the Japan Renal Biopsy Registry (J-RBR). Clin Exp Nephrol. 2016;20:552–60.
Nitta K, Okada K, Yanai M, Takahashi S. Aging and chronic kidney disease. Kidney Blood Press Res. 2013;38:109–20.
Oshima Y, Moriyama T, Itabashi M, Takei T, Nitta K. Characteristics of IgA nephropathy in advanced-age patients. Int Urol Nephrol. 2015;47:137–45.
Okabayashi Y, Tsuboi N, Haruhara K, Kanzaki G, Koike K, Shimizu A, Miyazaki Y, Ohno I, Kawamura T, Ogura M, Yokoo T. Reduction of proteinuria by therapeutic intervention improves the renal outcome of elderly patients with IgA nephropathy. Clin Exp Nephrol. 2016;20:910–7.
Lee SM, Rao VM, Franklin WA, Schiffer MS, Aronson AJ, Spargo BH, Katz AI. IgA nephropathy: morphological predictors of progressive renal disease. Hum Pathol. 1982;13:314–22.
Haas M. Histologic subclassification of IgA nephropathy: a clinicopathologic study of 244 cases. Am J Kidney Dis. 1997;29:829–42.
Shigematsu H. Histological grading and staging of IgA nephropathy. Pathorol Int. 1997;47:194–202.
Suzuki H. Biomarkers fo rIgA nephropathy on the basis of multi-hit pathogenesis. Clin Exp Nephrol. 2018. https://doi.org/10.1007/s10157-018-1582-2 [Epub ahead of print].
Moriyama T, Shimizu A, Takei T, Uchida K, Honda K, Nitta K. Characteristics of immunoglobulin A nephropathy with mesangial immunoglobulin G and immunoglobulin M deposition. Nephrol (Carlton). 2010;15:747–54.
Wada Y, Ogata H, Takeshige Y, Takeshima A, Yoshida N, Yamamoto M, Ito H, Kinugasa E. Clinical significance of IgG deposition in the glomerular mesangial area in patients with IgA nephropathy. Clin Exp Nephrol. 2013;17:73–82.
Shin DH, Lim BJ, Han IM, Han SG, Kwon YE, Park KS, Lee MJ, Oh HJ, Park JT, Han SH, Kang SW, Yoo TH. Glomerular IgG deposition predicts renal outcome in patients with IgA nephropathy. Mod Pathol. 2016;29:743–52.
Suzuki H, Yasutake J, Makita Y, Tanbo Y, Yamasaki K, Sofue T, Kano T, Suzuki Y. IgA nephropathy and IgA vasculitis with nephritis have a shared feature involving galactose-deficient IgA1-oriented pathogenesis. Kidney Int. 2018;93:700–5.
KDIGO clinical practice guidelines for glomerulonephritis-chapter 10: immunoglobulin A nephropathy. Kindey Int Supple 2012;2:S209–17.
Manno C, Torres DD, Rossini M, Pesce F, Schena FP. Randomized controlled clinical trial of corticosteroids plus ACE inhibitors with long-term follow-up in proteinuric IgA nephropathy. Nephrol Dial Transpl. 2009;24:3694–701.
Lv J, Zhang H, Chen Y, Li G, Jiang L, Singh AK, Wang H. Combination therapy of prednisolone and ACE inhibitor versus ACE inhibitor therapy alone in patients with IgA nephropathy: a randomized controlled trial. Am J Kidney Dis. 2009;53:26–32.
Komatsu H, Fujimoto S, Hara S, Sato Y, Yamada K, Kitamura K. Effect of tonsillectomy plus steroid pulse therapy on clinical remission of IgA nephropathy: a controlled study. Clin J Am Soc Nephrol. 2008;3:1301–7.
Ochi A, Moriyama T, Takei T, Uchida K, Nitta K. Comparison between steroid pulse therapy alone and in combination with tonsillectomy for IgA nephropathy. Int Urol Nephrol. 2013;45:469–76.
Hoshino Y, Moriyama T, Uchida K, Tsuchiya K, Nitta K. Comparison of oral steroids with tonsillectomy plus steroid pulse therapy in patients with IgA nephropathy. Clin Exp Nephrol. 2017;21:617–23.
Zhai YL, Zhu L, Shi SF, Liu LJ, Lv JC, Zhang H. Increased APRIL expression induces IgA1 aberrant glycosylation in IgA nephropathy. Med (Baltim). 2016;95:e3099.
Kim YG, Alvarez M, Suzuki H, Hirose S, Izui S, Tomino Y, Huard B, Suzuki Y. Pathogenic role of a proliferation-inducing ligand (APRIL) in murine IgA nephropathy. PLoS ONE. 2015;10:e0137044.
Goto T, Bandoh N, Yoshizaki T, Nozawa H, Takahara M, Ueda S, Hayashi T, Harabuchi Y. Increase in B-cell-activation factor (BAFF) and IFN-gamma productions by tonsillar mononuclear cells stimulated with deoxycytidyl-deoxyguanosine oligodeoxynucleotides (CpG-ODN) in patients with IgA nephropathy. Clin Immunol. 2008;126:260–9.
Muto M, Manfroi B, Suzuki H, Joh K, Nagai M, Wakai S, Righini C, Maiguma M, Izui S, Tomino Y, Huard B, Suzuki Y. Toll-Like receptor 9 stimulation induces aberrant expression of a proliferation-inducing ligand by tonsillar germinal Center B cells in IgA nephropathy. J Am Soc Nephrol. 2017;28:1227–38.
Feehally J, Coppo R, Troyanov S, Bellur SS, Cattran D, Cook T, Roberts IS, Verhave JC, Camilla R, Vergano L, Egido J, Wiecek A, Karkoszka H, Tesar V, Maixnerova D, Ots-Rosenberg M, Quaglia M, Rollino C, Magistroni R, Cusinato S, Cravero R, Peruzzi L, Lundberg S, Gesualdo L, Cancarini G, Feriozzi S, Ferrario F, VALIGA study of ERA-EDTA Immunonephrology Working Group. Tonsillectomy in a European Cohort of 1,147 Patients with IgA Nephropathy. Nephron. 2016;132:15–24.
Watanabe H, Goto S, Kondo D, Takata T, Yamazaki H, Hosojima M, Yamamoto S, Kaneko Y, Aoyagi R, Narita I. Comparison of methods of steroid administration combined with tonsillectomy for IgA nephropathy patients. Clin Exp Nephrol. 2017;21:257–65.
Ieiri N, Hotta O, Sato T, Taguma Y. Significance of the duration of nephropathy for achieving clinical remission in patients with IgA nephropathy treated by tonsillectomy and steroid pulse therapy. Clin Exp Nephrol. 2012;16:122–9.
Imai H, Miura N. A treatment dilemma in adult immunoglobulin A nephropathy: what is the appropriate target, preservation of kidney function or induction of clinical remission? Clin Exp Nephrol. 2012;16:195–201.
Diaz Encarnacion MM, Warner GM, Cheng J, Gray CE, Nath KA, Grande JP. N-3 fatty acids block TNF-α-stimulated MCP-1 expression in rat mesangial cells. Am J Physiol Renal Physiol. 2011;300:F1132–51.
Jia Q, Zhou HR, Bennink M, Pestka JJ. Docosahexaenoic acid attenuates mycotoxin-induced Immunoglobulin A nephropathy, interleukin-6 transcription, and mitogen-activated protein kinase phosphorylation in mice. J Neutr. 2004;134:3343–9.
Piante G, Musacchio E, valvason C, Clari G, Bordin L, Sartori L, Naggio B. Further insights about the beneficial effects of n-3 fatty acids in the early molecular events of renal fibrosis in vitro. J Nephrol. 2013;26:652–9.
Piante G, Musacchio E, Valvason C, Baggio B. EPA and DHA suppress Ang II- and arachidonic acid-induced expression of profibrotic genes in human mesangial cells. J Nephrol. 2009;22:137.
Pestka JJ, Zhou HR, Jia Q, Timmer AM. Dietary fish oil suppresses experimental immunoglobulin A nephropathy in mice. J Nutr. 2002;132:261–9.
Jia Q, Shi Y, Bennink M, Pestka JJ. Docosahexaenoic acid and eicosapentaenoic acid, but not α-linolenic acid, suppress deoxynivalenol-induced experimental IgA nephropathy in mice. J Nutr. 2004;134:1353–61.
Hamazaki T, Tateno S, Shishido M. Eicosapentaenoic acid and IgA nephropathy. Lancet. 1984;1:1017–8.
Chou HH, Chiou YY, Hung PH, Chiang PC, Wang ST. Omega-3 fatty acids amerilrate proteinuria but not renal function in IgA nephropathy: a meta analysis of randomized controlled trials. Nephron Clin Pract. 2012;121:c30–5.
Moriyama T, Iwasaki C, Tanaka K, Ochi A, Shimizu A, Shiohira S, Itabashi M, Takei T, Uchida K, Tsuchiya K, Nitta K. Effects of combination therapy with renin-angiotensin system inhibitors and eicosapentaenoic acid on IgA nephropathy. Intern Med. 2013;52:193–9.
Moriyama T, Kumon S, Kamiyama T, Karasawa K, Uchida K, Nitta K. The renoprotective effects of docosahexaenoic acid as add-on therapy in patients receiving eicosapentaenoic acid as treatment for IgA nephropathy: a pilot uncontrolled trial. Intern Med. 2018;57:173–9.
Su X, Zhang L, Lv J, Wang J, Hou W, Xie X, Zhang H. Effect of statins on kidney disease outcomes: a systematic review and meta-analysis. Am J Kidney Dis. 2016;67:881–92.
Moriyama T, Oshima Y, Tanaka K, Iwasaki C, Ochi A, Itabashi M, Takei T, Uchida K, Nitta K. Statins stabilize the renal function of IgA nephropathy. Ren Fail. 2014;36:356–60.
Buemi M, Allegra A, Corica F, Aloisi C, Giacobbe M, Pettinato G, Corsonello A, Senatore M, Frisina N. Effect of fluvastatin on proteinuria in patients with immunoglobulin A nephropathy. Clin Pharmacol Ther. 2000;67:427–31.
Kano K, Nishikura K, Yamada Y, Arisaka O. Effect of fluvastatin and dipyridamole on proteinuria and renal function in childhood IgA nephropathy with mild histological findings and moderate proteinuria. Clin Nephrol. 2003;60:85–9.
Lundberg S, Lundahl J, Gunnarsson I, Jacobson SH. Atorvastatininduced modulation of monocyte respiratory burst in vivo patients with IgA nephropathy: a chronic inflammatory kidney disease. Clin Nephrol. 2010;73:221–8.
Nakamura T, Ushiyama C, Hirokawa K, et al. Effect of cerivastatin on proteinuria and urinary podocytes in patients with chronic glomerulonephritis. Nephrol Dial Transpl. 2002;17:798–802.
Acknowledgements
I am grateful to the Japanese Society of Nephrology for this clinical scientific award. I would like to thank Dr. Kazuho Honda, Dr. Kosaku Nitta and Dr. Hiroshi Nihei for special mentorship and Dr. Noriko Mori (Shizuoka general hospital) for giving me strong motivation to treat and study IgA nephropathy. I thank Richard Robins, PhD, and Cathel Kerr, BSc, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The author declares there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article was presented as the Clinical Scientist Award memorial lecture at the 61st annual meeting of the Japanese Society of Nephrology, held at Sendai, Japan in 2018.
About this article
Cite this article
Moriyama, T. Clinical and histological features and therapeutic strategies for IgA nephropathy. Clin Exp Nephrol 23, 1089–1099 (2019). https://doi.org/10.1007/s10157-019-01735-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-019-01735-4