Abstract
Purpose
To the best of our knowledge, no study has compared intermittent steroid pulse therapy, according to Pozzi’s regimen, with versus without tonsillectomy.
Methods
In this retrospective cohort analysis, we compared clinical findings, histological findings according to the Oxford classification, and complete remission rates (RR), defined in terms of urinary protein excretion (U-Prot <0.3 g/g creatinine) and urinary red blood cell count (U-RBC <5/high-power field), after 1 year of treatment in patients with IgA nephropathy (IgAN), who received tonsillectomy with steroid pulse therapy (TSP group, n = 26) or steroid pulse therapy alone (SP group, n = 15).
Results
The baseline clinical and histological characteristics did not differ between the two groups. The RR for U-Prot analyzed by the Kaplan–Meier method did not differ between the groups (76.9 vs. 53.3 %). However, the RR for U-RBC was significantly higher in the TSP than in the SP group (88.4 vs. 33.3 %, log-rank test; P = 0.0008). The RRs for U-Prot and U-RBC were significantly higher in the TSP group than in the SP group (69.2 vs. 13.3 %, log-rank test; P = 0.0019). Cox’s regression analysis showed that combination therapy was associated with higher RR (odds ratio, 12.5; 95 % confidence interval, 2.91–86.7; P = 0.0002).
Conclusions
Tonsillectomy combined with steroid pulse therapy achieved higher RR after 1 year of treatment, compared with steroid pulse monotherapy in patients with IgAN. The long-term effects on renal survival should be analyzed in further studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
IgA nephropathy (IgAN) was first reported by Berger et al. [1], and it has since become the most common form of glomerulonephritis worldwide. Until the late 1980s, IgAN was recognized as a benign disease with a good prognosis. However, several investigators have reported that 30–40 % of patients with IgAN progress to end-stage renal disease (ESRD) within 20 years [2]. To improve the long-term prognosis of IgAN, several treatments have been proposed. In 2004, Pozzi et al. [3] reported that intermittent steroid pulse therapy delivered three times in 6 months decreased proteinuria and improved the long-term renal survival rate in a randomized controlled trial. This study was recognized as providing the strongest evidence in support of steroid pulse therapy for IgAN. Tonsillectomy in combination with steroid pulse therapy has been widely performed in Japan since Hotta et al. [4] reported its beneficial effects in 2001. They analyzed the long-term outcomes and factors associated with good prognosis of several treatments. They reported that patients who achieved clinical remission of urinary abnormalities did not develop ESRD for at least 10 years, and that tonsillectomy plus steroid pulse therapy had a significant impact on clinical remission of urinary abnormalities. Komatsu et al. [5] reported that the clinical remission rate (RR) from IgAN at 24 months was 61.8 % in patients treated with tonsillectomy combined with single-pulse steroid therapy compared with 17.6 % in patients given single-pulse steroid monotherapy. However, to the best of our knowledge, no study has compared steroid pulse monotherapy according to Pozzi’s regimen with and without tonsillectomy.
Therefore, in this study, we performed a retrospective cohort analysis to compare complete remission of urinary abnormalities between tonsillectomy combined with steroid pulse therapy and intermittent steroid pulse monotherapy according to Pozzi’s regimen. We also investigated the clinical and histological findings related to remission of urinary abnormalities.
Materials and methods
Patients
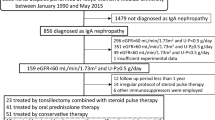
Between August 2007 and November 2009, we recommended tonsillectomy combined with steroid pulse therapy to 68 patients with newly diagnosed IgAN at Tokyo Women’s Medical University. The diagnosis of IgAN was based on light microscopic findings of mesangial proliferative changes, immunofluorescence analysis of mesangial IgA and C3 deposition, and electron microscopic observation of electron-dense deposits in the mesangial area. Of these 68 patients, 50 received tonsillectomy and steroid pulse therapy (TSP group), and 18 opted for steroid pulse monotherapy (SP group) at their own decision, despite our recommendation for tonsillectomy and steroid pulse therapy. Twenty-four patients were excluded from the TSP group for the following reasons: the patient was not observed for ≥1 year after treatment because they transferred to another hospital (8 patients), voluntary withdrawal from our hospital (2 patients), and deviation from our protocol regarding the timing of tonsillectomy or the interval of steroid pulse therapy (14 patients). Three patients were excluded from the SP group as they were not observed for ≥1 year having voluntarily transferred to another hospital. Consequently, 26 patients were included in the TSP group and 15 patients in the SP group in the present study.
Treatment protocol
Patients received intravenous methylprednisolone pulses of 0.5 g/day for 3 consecutive days at the start of the steroid course and a further two pulses within 6 months after the initial pulse. They were also given oral prednisone at a dose of 0.5 mg/kg body weight on every alternate day for 6 months. After the third steroid pulse, the oral prednisone was gradually withdrawn over a period of 1 month. Tonsillectomy was performed anytime during the 6 months of steroid therapy. If the tonsillectomy was performed before starting steroid pulse therapy, the first pulse was administered 1 week after tonsillectomy. If the first pulse was administered before tonsillectomy, the second or third pulse was administered 1 week after tonsillectomy (Fig. 1).
Treatment protocol for tonsillectomy combined with steroid pulse therapy and steroid pulse monotherapy. Steroid pulse therapy was performed three times during 6 months at intervals of 2–4 months. During this time, 0.5 mg/kg prednisolone was administered orally every alternate day. Tonsillectomy was performed at any time during the 6 months. If the first steroid pulse was given before tonsillectomy, the second pulse was given after tonsillectomy. If the first and second steroid pulses were performed before tonsillectomy, tonsillectomy was performed before the final steroid pulse at 6 months after the first pulse. After the final steroid pulse, oral prednisolone was gradually tapered and withdrawn within 1 month. PSL prednisolone
Evaluation of clinical and laboratory data
We compared the following clinical findings recorded at the time of renal biopsy between the two groups: sex, age, time from onset of IgAN, episodes of gross hematuria, body mass index (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean blood pressure (MBP), serum total protein, serum creatinine (Cr), estimated glomerular filtration rate (eGFR), uric acid, low density lipoprotein, triglycerides, urinary protein excretion (U-Prot), urinary red blood cell count (U-RBC), serum IgA, and serum complement titer (CH50). We also determined U-Prot and U-RBC at 0, 1, 3, 6, 9, and 12 months after the third methylprednisolone pulse. We defined clinical remission as U-Prot <0.3 g/g Cr and U-RBC <5/high-power field (HPF). We also compared the time to achieve clinical remission in both groups.
Histological analysis of renal biopsy specimens
All specimens were obtained by percutaneous needle biopsy. The specimens were fixed with 10 % phosphate-buffered formalin (pH 7.2), embedded in paraffin, and cut into 4-μm-thick sections. The sections were stained with hematoxylin and eosin, periodic acid–Schiff, silver methenamine, and Masson trichrome for light microscopic examination.
The histological findings were graded according to the Oxford classification reported by an international consensus working group in 2009 [6, 7]. Pathologists graded each tissue section on four key pathological features: (1) mesangial hypercellularity score (M0, mesangial score ≤0.5; M1, mesangial score >0.5); (2) segmental glomerulosclerosis (S0, absence of segmental glomerulosclerosis; S1, presence of segmental glomerulosclerosis); (3) endocapillary hypercellularity (E0, absence of endocapillary hypercellularity; E1, presence of hypercellularity); and (4) tubular atrophy/interstitial fibrosis (T0, ratio of tubular atrophy/interstitial fibrosis in the total interstitium was 0–25 %; T1, 26–50 %; T2, >51 %).
Statistical analysis
Data are presented as mean ± standard deviation (SD) for normally distributed data or as medians and interquartile range (IQR) for non-normally distributed data. Data were analyzed using JMP 8.0.1 (SAS Institute, Cary, NC, USA). Unpaired Student’s t test for normally distributed data and nonparametric Wilcoxon test for non-normally distributed data were used to compare the clinical findings between the TSP and SP groups. The χ2 test was used to compare sex, administration of renin–angiotensin–aldosterone inhibitors (RASIs), and Oxford classification pathological scores between the two groups. The time to reach clinical remission of U-Prot and U-RBC was calculated using the Kaplan–Meier method and compared with the log-rank test. To confirm the reproducibility of clinical remission of U-Prot and U-RBC, we defined clinical remission as patients who maintained clinical remission until the end of study after achieving clinical remission. Non-clinical remission was defined as patients who did not achieve clinical remission or experienced relapse of U-Prot or U-RBC after achieving clinical remission. Multivariate Cox’s regression analysis was used to identify factors associated with clinical remission in both groups. All of the independent variables used in multivariate analyses were included as categorical (e.g., absent/present, coded as 0/1) or quantitative variables. Tonsillectomy (yes/no) was included as a categorical variable, whereas age, time from onset, MBP, urinary protein, U-RBC, eGFR, and histological grades were included as quantitative variables. The results of the multivariate analyses are expressed as odds ratios (ORs) with 95 % confidence intervals (CIs). Values of P < 0.05 were considered to be statistically significant in all analyses.
Results
Clinical findings at the time of renal biopsy
Table 1 compares the baseline clinical characteristics between the TSP and SP groups. Age, sex, time from onset, number of patients with episodes of gross hematuria, BMI, SBP, DBP, and MBP did not differ between the two groups. The median (IQR) Cr was 0.86 (0.67–0.97) mg/dl in the TSP group and 0.84 (0.65–0.97) mg/dl in the SP group. The median (IQR) U-Prot was 0.63 (0.23–1.38) g/day in the TSP group and 0.62 (0.32–1.33) g/day in the SP group. The median (IQR) U-RBC was 25 (8.75–50)/HPF in the TSP group and 30 (10–50)/HPF in the SP group. Cr, U-Prot, and U-RBC were not significantly different between the two groups. Furthermore, the other laboratory parameters assessed were not significantly different between the two groups. RASIs were administered to 11 patients (42 %) in the TSP group and five (33 %) in the SP group, which was not significantly different.
Histological findings
Table 2 shows the histological grade according to the Oxford classification for both groups. Mesangial hypercellularity score, segmental glomerulosclerosis, endocapillary hypercellularity, and tubular atrophy/interstitial fibrosis were not significantly different between the two groups. None of the patients in either group showed >50 % tubular atrophy/interstitial fibrosis.
Clinical RRs
Figure 2 shows the RR for U-Prot, which was not significantly different between the TSP and SP groups, as analyzed by Kaplan–Meier analysis and the log-rank test (76.9 vs. 53.3 %, log-rank test P = 0.1749). Figure 3 shows the RR for U-RBC. The log-rank test confirmed that the RR for U-RBC was significantly higher in the TSP group than in the SP group (88.4 vs. 33.3 %, log-rank test P = 0.0008). Figure 4 shows the combined RRs for both U-Prot and U-RBC. The combined RR was significantly higher in the TSP group than in the SP group (69.2 vs. 13.3 %, log-rank test P = 0.0019).
Comparison of the clinical RR for hematuria between the TSP and SP groups. Kaplan–Meier analysis and the log-rank test were performed to compare the RR for U-RBC (<5/HPF) between the two groups. The RR for U-RBC was significantly higher in the TSP group than in the SP group (log-rank test, P = 0.0008)
Comparison of the clinical RR for proteinuria and hematuria between the TSP and SP groups. Kaplan–Meier analysis and the log-rank test were performed to compare the RR for both U-Prot (<0.3 g/g Cr) and U-RBC (<5/HPF) between the two groups. The RR for U-Prot and U-RBC was significantly higher in the TSP group than in the SP group (log-rank test, P = 0.0019)
Multivariate analysis of factors associated with remission
The results of multivariate Cox’s regression analysis to identify factors associated with complete remission in all patients are shown in Table 3. The widely recognized risk factors for IgAN progression include renal function (i.e., eGFR), blood pressure, and proteinuria, while the time from onset was considered by Ieiri et al. [8] to be one of the important factors associated with clinical remission. Therefore, these factors, as well as histological findings in terms of Oxford classification, were included as independent variables in the analysis. Tonsillectomy combined with steroid pulse therapy was approximately 12 times more effective than steroid pulse monotherapy for achieving clinical remission (OR, 12.5; 95 % CI, 2.91–56.7; P = 0.0002). Higher eGFR was also favorably associated with clinical remission (OR, 2.10; 95 % CI, 1.28–3.79; P = 0.0021), whereas tubular atrophy/interstitial fibrosis was independently associated with reduced likelihood of clinical remission (OR, 0.11; 95 % CI, 0.01–0.88; P = 0.0374). The other factors evaluated in this analysis, including age, time from onset, MBP, U-Prot, U-RBC, eGFR, and histological grade were not associated with clinical remission.
Discussion
In this study, we showed that tonsillectomy combined with steroid pulse therapy had a significantly better effect on clinical remission in terms of U-Prot and U-RBC than steroid pulse monotherapy (69.2 vs. 13.3 %). Cox’s regression analysis showed that combination therapy was approximately 12-fold more effective than steroid pulse monotherapy for remission of urinary factors. We suspect that there are two main reasons for the difference in clinical RR between the two groups. First, combination therapy had a significantly better effect on remission of U-RBC compared with monotherapy (88.4 vs. 33.3 %), although the effects of both treatments on the remission of U-Prot were equal. Second, U-RBC relapsed during the observation period in four patients (26.6 %) in the steroid pulse monotherapy group compared with none in the combination therapy group. Based on these results, we suspect that steroid pulse therapy is sufficient to achieve remission of U-Prot but not both U-Prot and U-RBC, and that tonsillectomy combined with steroid pulse therapy is required to achieve both.
Hotta et al. [4] reported that clinical remission of both U-Prot and U-RBC is the most important factor for maintenance of renal function. In their study, the renal survival rate was significantly higher in patients who achieved remission than in those who did not (100 vs. 22.6 %). They also reported that tonsillectomy and steroid pulse therapy was the most effective means of achieving clinical remission. Pozzi et al. [3] previously reported on the efficacy of steroid pulse monotherapy. In that study, the 10-year survival rate was significantly higher in IgAN patients with U-Prot of 1–3.5 g/day and plasma Cr ≤1.5 mg/dl who received steroid pulse therapy compared with those who did not (97 vs. 53 %, P = 0.0003). Their results in terms of renal survival were similar to those reported by Hotta et al. [4]. Pozzi et al. [3] also reported that minimal response rate of proteinuria (<1 g/day) was significantly higher in patients who received steroid therapy (72 vs. 30 %). However, they did not show the response of U-RBC to steroid pulse monotherapy; therefore, we cannot establish the effect of this response on long-term renal survival in that study.
A more recent study by Pozzi et al. [9] showed that azathioprine combined with steroid pulse therapy did not improve the 5–7-year renal survival rate of patients with IgAN, U-Prot ≥1.0 g/day, and Cre ≤2.0 mg/dl. Interestingly, the 7-year renal survival rate in a control group of patients given steroid pulse monotherapy was only 84 %. These results indicate that steroid pulse monotherapy does not dramatically improve the renal survival rate, because it was similar to that in previous studies examining long-term renal survival in patients with IgAN [10, 11]. Therefore, steroid pulse therapy combined with other treatments likely to be more effective than azathioprine should be investigated to establish whether such combinations can improve the outcome of IgAN. Sato et al. [12] reported that the 10-year renal survival rate of patients with IgAN and Cre ≤2.0 mg/dl was 100 % after tonsillectomy combined with steroid pulse therapy in a retrospective cohort study. Their results differ from those reported by Pozzi et al. [9], and tonsillectomy might represent an effective alternative to azathioprine combined with steroid pulse therapy. We suspect that the difference in renal survival rate between steroid pulse monotherapy and combination therapy might be due to the remission of U-RBC achieved by the latter.
Several recent studies have shown that microhematuria is an important predictor for the progression of IgAN to ESRD. Microhematuria was reported to be a risk factor for the progression of IgAN to proteinuria and/or hypertension, and even ESRD in some patients [13–15]. Moreover, Manno et al. [16] reported that microhematuria at the clinical onset of IgAN increases the risk of progression to ESRD by 2.18-fold. Rauta et al. [17] reported that U-RBC is associated with the renal outcomes in patients with IgAN patients and initially normal renal function, and that U-RBC might represent a high degree of glomerular inflammation. These results prompted the hypothesis that achieving clinical remission of both U-Prot and U-RBC is required to prevent progression to ESRD.
Ieiri et al. [8] reported that a shorter duration of nephropathy was the most important factor for achieving clinical remission, whereas hypertension, impaired renal function, and severe histological changes were not associated with clinical remission in multivariate Cox’s regression analysis. In our study, however, the time from onset was not associated with clinical remission in multivariate Cox’s regression analysis, although TSP therapy and higher eGFR were favorably associated with CR, while tubular atrophy and interstitial fibrosis were associated with reduced likelihood of achieving CR. We suspect that this discrepancy is attributable to our inclusion of all patients in the TSP and SP groups, whereas Ieiri et al. limited their analysis to patients who received tonsillectomy combined with steroid therapy, but not steroid pulse monotherapy. In our study, 87.6 % of patients in the SP group did not achieve CR, which probably had a greater effect on the multivariate analysis than the 30.8 % of patients in the TSP group who did not achieve CR.
There are some limitations to our study. First, this study was a retrospective cohort study, not a randomized controlled trial. Second, the sample size was very small; with only 15 and 26 patients in the SP and TSP groups, respectively. Finally, the effect of treatment on long-term renal survival should be analyzed, because the goal of treatment for IgAN is to prevent its progression to ESRD. A multicenter, randomized controlled trial was recently completed in Japan, and the results will be published in the near future. We hope that our results provide useful support for the results of that study and confirm the benefits of tonsillectomy combined with steroid pulse therapy for IgAN.
In conclusion, tonsillectomy combined with steroid pulse therapy achieved remission of both hematuria and proteinuria, whereas steroid pulse monotherapy achieved remission of proteinuria alone. We believe that achieving clinical remission of both proteinuria and hematuria is the most important factor for the prevention of ESRD and favorable long-term outcome of IgAN. The achievement of remission of hematuria represents an important difference between both therapies examined here. In the future, we must analyze the long-term renal survival rates in both cohorts of patients.
References
Berger J, Hinglais N (1968) Inter capillary deposits of IgA-IgG. J Urol Nephrol (Paris) 74:694–695
D’Amico G (2000) Natural history of idiopathic IgA nephropathy: role of clinical and histological prognostic factors. Am J Kidney Dis 36:227–237
Pozzi C, Andrulli S, Del Vecchio L, Melis P, Fogazzi GB, Altieri P, Ponticelli C, Locatelli F (2004) Corticosteroid effectiveness in IgA nephropathy: long-term results of a randomized, controlled trial. J Am Soc Nephrol 15:157–163
Hotta O, Miyazaki M, Furuta T, Tomioka S, Chiba S, Horigome I, Abe K, Taguma Y (2001) Tonsillectomy and steroid pulse therapy significantly impact on clinical remission in patients with IgA nephropathy. Am J Kidney Dis 38:736–743
Komatsu H, Fujimoto S, Hara S, Sato Y, Yamada K, Kitamura K (2008) Effect of tonsillectomy plus steroid pulse therapy on clinical remission of IgA nephropathy: a controlled study. Clin J Am Soc Nephrol 3:1301–1307
A Working Group of the International IgA Nephropathy Network and the Renal Pathology Society (2009) The Oxford classification of IgA nephropathy: rationale, clinicopathological correlations, and classification. Kidney Int 76:534–545
A Working Group of the International IgA Nephropathy Network and the Renal Pathology Society (2009) The Oxford classification of IgA nephropathy: pathology definitions, correlations, and reproducibility. Kidney Int 76:546–556
Ieiri N, Hotta O, Sato T, Taguma Y (2012) Significance of the duration of nephropathy for achieving clinical remission in patients with IgA nephropathy treated by tonsillectomy and steroid pulse therapy. Clin Exp Nephrol 16:122–129
Pozzi C, Andrulli S, Pani A, Scaini P, Del Vecchio L, Fogazzi G, Vogt B, De Cristofaro V, Allegri L, Cirami L, DeniProcaccini A, Locatelli L (2010) Addition of azathioprine to corticosteroids does not benefit patients with IgA nephropathy. J Am Soc Nephrol 21:1783–1790
Le W, Liang S, Hu Y, Deng K, Bao H, Zeng C, Liu Z (2012) Long-term renal survival and related risk factors in patients with IgA nephropathy: results from a cohort of 1,155 cases in a Chinese adult population. Nephrol Dial Transplant 27:1479–1485
Li PK, Ho KK, Szeto CC, Yu LM, Lai FM (2002) Prognostic indicators of IgA nephropathy in the Chinese—clinical and pathological perspectives. Nephrol Dial Transplant 17:64–69
Sato M, Hotta O, Tomioka S, Horigome I, Chiba S, Miyazaki M, Noshiro H, Taguma Y (2003) Cohort study of advanced IgA nephropathy: efficacy and limitations of corticosteroids with tonsillectomy. Nephron Clin Pract 93:c137–c145
Szeto CC, Lai FM, To KF, Wong TY, Chow KM, Choi PC, Lui SF, Li PK (2001) The natural history of immunoglobulin a nephropathy among patients with hematuria and minimal proteinuria. Am J Med 110:434–437
Shen P, He L, Li Y, Wang Y, Chan M (2007) Natural history and prognostic factors of IgA nephropathy presented with isolated microscopic hematuria in Chinese patients. Nephron Clin Pract 106:c157–c161
Kim BS, Kim YK, Shin YS, Kim YO, Song HC, Kim YS, Choi EJ (2009) Natural history and renal pathology in patients with isolated microscopic hematuria. Korean J Int Med 24:356–361
Manno C, Strippoli GF, D’Altri C, Torres D, Rossini M, Schena FP (2007) A novel simpler histological classification for renal survival in IgA nephropathy: a retrospective study. Am J Kidney Dis 49:763–775
Rauta V, Finne P, Fagerudd J, Rosenlof K, Tornroth T, Gronhagen-Riska C (2002) Factors associated with progression of IgA nephropathy are related to renal function—a model for estimating risk of progression in mild disease. Clin Nephrol 58:85–94
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ochi, A., Moriyama, T., Takei, T. et al. Comparison between steroid pulse therapy alone and in combination with tonsillectomy for IgA nephropathy. Int Urol Nephrol 45, 469–476 (2013). https://doi.org/10.1007/s11255-012-0251-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-012-0251-8