Abstract
Background
High uric acid level is a known risk factor for deterioration of renal function in chronic kidney disease (CKD), but its influence on the progression of IgA nephropathy (IgAN) remains unclear.
Methods
Adult IgAN patients (n = 611) were classified according to CKD stage. Renal survival rates and clinical and histological findings were compared between patients with high (H-UA) and normal (N-UA) uric acid levels in different CKD stages.
Results
The proportion of patients with H-UA increased significantly with increasing CKD stage (stage G1, 12.3 %; stage G2, 19.0 %; stage G3a, 43.7 %; stage G3b–4, 69.0 %; P < 0.001). The 30-year renal survival rate was similar in patients with H-UA and N-UA in CKD stages G1, G2, and G3b–4, but was significantly lower in patients with H-UA than with N-UA in CKD stage G3a (24.7 vs. 51.9 %; P = 0.0205). The clinical findings were similar in patients with H-UA and N-UA, but the interval from onset to biopsy differed between groups. The proportion of patients with global sclerosis was significantly higher in patients with H-UA than with N-UA in CKD stage G3a (33.3 vs. 11.4 %; P = 0.0005), but the Oxford classifications were similar between groups. Multivariate Cox regression analysis identified H-UA (HR 1.36, 95 % CI 1.07–1.72, P = 0.011) and a large amount of proteinuria (HR 1.38, 95 % CI 1.09–1.74, P = 0.0084) as independent predictors of end-stage renal disease.
Conclusions
H-UA induced global glomerular sclerosis and accelerated the progression of IgAN in CKD stage G3a.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
We previously reported on the 30-year prognosis of patients with IgA nephropathy (IgAN). We found that a high serum uric acid level, low estimated glomerular filtration rate (eGFR), and large amount of proteinuria were risk factors for progression to end-stage renal disease (ESRD) [1]. A low eGFR and large amount of proteinuria are recognized risk factors for progression to ESRD in patients with IgAN, but it remains unclear whether a high uric acid level is also associated with progression to ESRD in these patients. It has recently been reported that a high uric acid level is associated with the development of chronic kidney disease (CKD) [2], and with decline in renal function in patients with CKD [3]. We previously reported that a high uric acid level was associated with all-cause mortality and cardiovascular mortality in patients with CKD stage G2–4 [4]. Considering these findings, we hypothesized that a high uric acid level accelerates renal impairment in patients with IgAN.
This study compared the proportions of patients with high uric acid levels among different stages of CKD. Long-term renal survival was compared between patients with high and normal uric acid levels for each CKD stage. Clinical and histological findings were compared between patients with high and normal uric acid levels in the CKD stages with significant differences in renal survival rates between these two groups.
Subjects and methods
Patients
A total of 611 adults were diagnosed with IgAN at Tokyo Women’s Medical University between 1974 and 2005. The patients were classified according to their CKD stage, and each CKD stage was divided into patients with a high uric acid level (H-UA: uric acid level >7.0 mg/dL for males and >6.0 mg/dL for females at the time of renal biopsy) and a normal uric acid level (N-UA: uric acid level <6.9 mg/dL for males and <5.9 mg/dL for females).
The renal survival rates (survival without ESRD, defined as requiring dialysis or renal transplantation) were compared between patients with H-UA and N-UA for each CKD stage. In the CKD stages with a significant difference in renal survival rate between patients with H-UA and N-UA, the histological and clinical findings at the time of renal biopsy were compared between groups, including the sex, body mass index, systolic blood pressure, diastolic blood pressure, mean arterial pressure, interval from onset to renal biopsy, medications to increase or decrease the uric acid level, eGFR, urinary protein excretion (U-Prot), urinary red blood cell count, and blood levels of albumin, uric acid, total cholesterol, triglycerides, immunoglobulin A, and complement C3. The risk factors associated with progression to ESRD in the CKD stages with a significant difference in renal survival rate between patients with H-UA and N-UA were also evaluated. eGFR was calculated using the modified isotope dilution mass spectrometry–modification of diet in renal disease study for Japan equation [eGFR = 194 × serum-creatinine−1.094 × age−0.287 × 0.739 (if female)] [5].
This retrospective cohort study was conducted in accordance with the guidelines of the Declaration of Helsinki and was approved by the Medical Ethics Committee of Tokyo Women’s Medical University (#3206). Written informed consent for renal biopsy was obtained from all patients.
Histological examination of renal biopsy specimens
Renal specimens were obtained by percutaneous needle biopsy. The proportions of glomeruli with lesions were evaluated as previously reported, including global sclerosis, segmental sclerosis or adhesions, cellular or fibrocellular crescents, and fibrous crescents [1]. The histological findings were also graded according to Oxford classification [6, 7], which scores four key pathological features in each specimen: (1) mesangial hypercellularity, scored as M0 if >50 % of glomeruli had fewer than three cells per mesangial area or M1 if >50 % of glomeruli had more than three cells per mesangial area; (2) segmental glomerulosclerosis, scored as absent (S0) or present (S1); (3) endocapillary hypercellularity, scored as absent (E0) or present (E1); and (4) tubular atrophy/interstitial fibrosis, scored according to the percentage of tubular atrophy/interstitial fibrosis in the total interstitium as T0 (0–25 %), T1 (26–50 %), or T2 (>51 %). Biopsy specimens containing fewer than eight glomeruli were excluded from the analyses.
Statistical analysis
Data are presented as the mean ± standard deviation for normally distributed data and median (interquartile range) for non-normally distributed data. All analyses were performed using JMP 10.0.1 (SAS Institute, Cary, NC, USA). Clinical and histological findings were compared between groups the Student’s t test, Mann–Whitney U test, or χ2 test. Cumulative renal survival rates were calculated using the Kaplan–Meier method, and were compared between groups using the log-rank test. Factors associated with progression to ESRD were identified using univariate and multivariate Cox regression analyses. In the univariate analyses, sex (male/female) and histological grade (Oxford classification) were analyzed as categorical variables, and age, body mass index, mean arterial pressure, eGFR, U-Prot, urinary red blood cell count, and blood levels of albumin, uric acid, total cholesterol, triglyceride, IgA, and complement C3 were analyzed as quantitative variables. The factors that were significantly associated with progression to ESRD on univariate analyses were included in the multivariate analysis. The results of the univariate and multivariate analyses are expressed as hazard ratios (HRs) with 95 % confidence intervals (CIs). In all the analyses, P < 0.05 was considered statistically significant.
Results
Proportion of patients with H-UA for each CKD stage
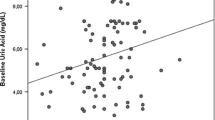
The proportion of patients with H-UA was 12.3 % (23/187 patients) in CKD stage G1, and increased significantly with increasing CKD stage (stage G2: 19.0 %, 52/274 patients; stage G3a: 43.7 %, 45/103 patients; stage G3b–4: 69.0 %, 29/42 patients; P < 0.001) (Fig. 1).
Renal survival rates in patients with H-UA and N-UA for each CKD stage
To avoid introducing bias due to underlying renal function, renal survival rates were compared between patients with H-UA and N-UA for each CKD stage. The eGFR was similar between patients with H-UA and N-UA for each CKD stage. The renal survival rate was similar between patients with H-UA and N-UA for CKD stages G1, G2, and G3b–4, but significantly higher in patients with N-UA than with H-UA for CKD stage G3a (52.9 vs. 24.7 %; log-rank test, P = 0.0205) (Fig. 2). As the impact of H-UA was significant in patients with IgAN and CKD stage G3a, these patients were more extensively analyzed.
Renal survival rates in patients with H-UA and N-UA for each CKD stage. a Among patients with CKD stage G1, patients with H-UA and N-UA had a similar eGFR at the time of renal biopsy [104.6 (98.9–108.6) vs.103.2 (96.6–116.6) mL/min/1.76 m2; log-rank test, P = 0.7856] and similar 30-year renal survival rate (83.3 vs. 79.7 %; log-rank test, P = 0.9917). b Among patients with CKD stage G2, patients with H-UA and N-UA had a similar eGFR at the time of renal biopsy [72.8 (65.2–78.1) vs. 75.2 (67.7–82.4) mL/min/1.76 m2; log-rank test, P = 0.0578] and similar 30-year renal survival rate (73.9 vs. 48.3 %; log-rank test, P = 0.5758). c Among patients with CKD stage G3a, patients with H-UA and N-UA had a similar eGFR at the time of renal biopsy [53.2 (49.4–56.7) vs. 55.0 (51.1–58.4) mL/min/1.76 m2; log-rank test: P = 0.1040], but the renal survival rate was significantly lower in patients with H-UA than with N-UA (67.9 vs. 89.7 % at 10 years, 49.5 vs. 69.3 % at 20 years, and 24.7 vs. 51.9 % at 30 years; P = 0.0205). d Among patients with CKD stage G3b–4, patients with H-UA and N-UA had a similar eGFR at the time of renal biopsy [38.7 (33.8–42.9) vs. 40.7 (36.3–43.8) mL/min/1.7 6 m2; log-rank test, P = 0.3162] and similar 15-year renal survival rate (34.2 vs. 21.3 %; log-rank test, P = 0.8299)
Clinical, laboratory, and histological findings in patients with IgAN and CKD stage G3a
Table 1 shows the clinical and laboratory findings in patients with IgAN and CKD stage G3a who had H-UA and N-UA. The interval from onset to renal biopsy was significantly longer in patients with H-UA than with N-UA [7.5 years (4.0–12.0) vs. 3.0 years (1.0–9.0), P = 0.0142], but the other clinical and laboratory findings were similar between patients with H-UA and N-UA. Only two patients with H-UA and one patient with N-UA were treated with the medications to increase the uric acid level, such as furosemide or trichlormethiazide. Eight patients were treated with the medication to decrease the uric acid level (allopurinol) at the time of renal biopsy, and five of them were well controlled, but the other three were not. Table 2 shows the glomerular lesions and Oxford classifications in patients with IgAN and CKD stage G3a who had H-UA and N-UA. The median proportion of glomeruli with global sclerosis was significantly higher in patients with H-UA than with N-UA [33.3 % (13.6–50.0) vs. 11.4 % (7.14–28.8), P = 0.0005], but the proportions of glomeruli with segmental sclerosis or adhesions, cellular or fibrocellular crescents, and fibrous crescents were not significantly different between patients with H-UA and N-UA. The Oxford classifications were not significantly different between the two groups.
Independent predictors of progression to ESRD
Table 3 shows the results of univariate and multivariate Cox regression analyses to identify independent clinical and histological predictors of progression to ESRD at the time of renal biopsy. Univariate analyses showed that H-UA, high total cholesterol level, and high U-Prot were associated with progression to ESRD. Multivariate analysis identified a 1.0 mg/dl increase on the uric acid level (HR 1.36, 95 % CI 1.07–1.72, P = 0.011) and 0.5 g/day increase in U-Prot (HR 1.38, 95 % CI 1.09–1.74, P = 0.0084) as independent predictors of progression to ESRD.
Discussion
The data from this study suggest that a high uric acid level is a risk factor for progression to ESRD in patients with IgAN and CKD stage G3a, and that a high uric acid level induces glomerular global sclerosis. The synergistic effects of global sclerosis and renal dysfunction due to IgAN result in a poorer prognosis in patients with IgAN who have H-UA than in those who have N-UA. These findings indicate that the uric acid level should be well controlled in patients with IgAN, before progression to CKD stage G3a.
A high uric acid level results in increased activity of the renin-angiotensin system, oxidative stress, mitochondrial dysfunction, epithelial-mesenchymal transition, endothelial dysfunction, and vascular smooth muscle cell proliferation. These changes lead to arteriosclerosis, glomerular hypertension, glomerulosclerosis, and interstitial disorders of the kidney, as well as to systemic disorders such as metabolic syndrome, non-alcoholic fatty liver disease, hypertension, and diabetes mellitus [8, 9]. These effects suggest that a high uric acid level may be a risk factor for progression of IgAN to ESRD. It was previously reported that a high uric acid level in patients with IgAN was a risk factor for progression to ESRD [10–17]. Ohno et al. [11] reported that a high uric acid level was associated with glomerular and tubular damage, increased proteinuria, hypertension, and a poor prognosis. Myllymäki et al. [12] also reported that a high uric acid level was associated with severe tubulointerstitial damage. Cheng et al. [16] reported that a high uric acid level was associated with global glomerulosclerosis, tubulointerstitial nephritis, and vascular lesions, and was a risk factor for progression to ESRD in patients with IgAN with both normal and abnormal renal function. Zhou et al. [17] reported that the uric acid level was a predictor of tubulointerstitial lesions in patients with IgAN and normal renal function. These findings suggest that a high uric acid level induces glomerular, tubulointerstitial, and vascular damage, resulting in further deterioration of renal function and progression to ESRD in patients with IgAN [8, 9]. In this study of patients with IgAN, 12.3 % of patients with CKD stage G1 and 19.0 % of patients with CKD stage G2 had a high uric acid level. If the uric acid level is not controlled before progression to CKD stage G3a, the renal function may deteriorate as a result of the glomerular, interstitial, and vascular damage induced by IgAN as well as the high uric acid level. It is well established that renal dysfunction itself causes a high uric acid level, and in this study the proportion of patients with IgAN who had a high uric acid level was significantly higher in patients with CKD stage G3a (43.7 %) and stage G3b–4 (69.0 %) than in patients with lower CKD stages. A high uric acid level causes renal dysfunction, and renal dysfunction causes a high uric acid level. This positive feedback cycle accelerates progression to ESRD. The duration of renal disease (interval from onset to renal biopsy) was significantly longer in patients with H-UA than with N-UA. This delay in diagnosis may have increased the renal dysfunction and the progression of both IgAN and hyperuricemia. It is therefore important to control the uric acid level before progression to CKD stage G3a, to prevent progression to ESRD. Five of the patients with N-UA started treatment with allopurinol before progression to CKD G3a. The uric acid level in these patients was well controlled, and 80 % of them did not progress to ESRD. Conversely, nine of patients with H-UA started treatment with allopurinol after renal biopsy, but five of these patients progressed to ESRD. Among patients with IgAN and CKD stage G3a, the proportion of glomeruli with global sclerosis was threefold higher in patients with H-UA than with N-UA. If the uric acid level can be controlled before progression to CKD stage G3a, global glomerular sclerosis and the risk of progression to ESRD may be reduced.
In conclusion, patients with IgAN who had CKD stage G3a and H-UA had a higher proportion of global glomerular sclerosis and an increased risk of progression to ESRD compared with patients with N-UA. Glomerular impairment by a high uric acid level may accelerate progression to ESRD in addition to the renal dysfunction caused by IgAN. The uric acid level should be controlled before progression to CKD stage G3a.
References
Moriyama T, Tanaka K, Iwasaki C et al (2014) Prognosis in IgA nephropathy: 30-year analysis of 1,012 patients at a single center in Japan. PLoS ONE 9:e91756
Ryoo JH, Choi JM, Oh CM, Kim MG (2013) The association between uric acid and chronic kidney disease in Korean men: a 4-year follow-up study. J Korean Med Sci 28:855–860
Sedaghat S, Hoorn EJ, van Rooij FJA et al (2013) Serum uric acid and chronic kidney disease: the role of hypertension. PLoS ONE 8:e76827
Miyaoka T, Mochizuki T, Takei T, Tsuchiya K, Nitta K (2014) Serum uric acid levels and long-term outcomes in chronic kidney disease. Heart Vessels 29:504–512
Matsuo S, Imai E, Horio M, Yasuda Y et al (2009) Revised equation for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53:982–992
Cattran DC, Coppo R, Cook HT, A Working Group of the International IgA Nephropathy Network and the Renal Pathology Society et al (2009) The Oxford Classification of IgA Nephropathy: rationale, clinicopathological correlations, and classification. Kidney Int 2009:534–545
Roberts IS, Cook HT, Troyanov S, A Working Group of the International IgA Nephropathy Network and the Renal Pathology Society et al (2009) The Oxford classification of IgA nephropathy: pathology definitions, correlations, and reproducibility. Kidney Int 76:546–556
Johnson RJ, Nakagawa T, Jalal D, Sánxhez-Lozada LG, Kang DH, Ritz E (2013) Uric acid and chronic kidney disease: which chasing which? Nephrol Dial Transplant 28:2221–2228
Ohno I (2011) Relationship between hyperuricemia and chronic kidney disease. Nucleosides Nucleotides Nucleic Acid 30:1039–1044
Syrjänen J, Mustonen J, Pasternack A (2000) Hypertriglyceridaemia and hyperuricemia are risk factors for progression of IgA nephropathy. Nephrol Dialysis Transplant 15:34–42
Ohno I, Hosoya T, Gomi H, Ichida K, Okabe H, Hikata M (2001) Serum uric acid and renal prognosis in patients with IgA nephropathy. Nephron 87:333–339
Myllymäki J, Honkanen T, Syrjänen J, helin H, Rantala I, Pasternack A, Mustonen J (2005) Uric acid correlates with the severity of histological parameters in IgA nephropathy. Nephrol Dial Transplant 20:89–95
Shi Y, Chen W, Jalal D et al (2012) Clinical outcome of hyperuricemia in IgA nephropathy: a retrospective cohort study and randomized controlled trial. Kidney Blood Press Res 35:153–160
Sulikowska B, Manitius J, Odrowąż-Sypniewska G, Łysiak-Szydłowska W, Rutkowski B (2008) Uric acid excretion and dopamine-induced glomerular filtration response in patients with IgA nephropathy. Am J Nephrol 28:391–396
Sulilpwska B, Johnson RJ, Odrowąż-Sypniewska G, Manitius J (2012) Uric acid, renal vasoconstriction and erythropoietin relationship in IgA nephropathy revealed by dopamine-induced glomerular filtration response. Kidney Blood Press Res 35:161–166
Cheng GY, Liu DW, Zhang N, Tang L, Zhao ZZ, Liu ZS (2013) Clinical and prognostic implications of serum uric acid levels on IgA nephropathy: a cohort study of 348 cases with a mean 5-year follow-up. Clin Nephrol 80:40–46
Zhou J, Chen Y, Liu Y et al (2014) Plasma uric acid level indicates tubular interstitial lesions at early stage of IgA nephropathy. BMC Nephrol 15:11
Conflict of interest
All authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moriyama, T., Itabashi, M., Takei, T. et al. High uric acid level is a risk factor for progression of IgA nephropathy with chronic kidney disease stage G3a. J Nephrol 28, 451–456 (2015). https://doi.org/10.1007/s40620-014-0154-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-014-0154-0