Abstract
Background
The adaptation of steroid therapy and the effect of renin–angiotensin–aldosterone system inhibitors (RASIs) for advanced immunoglobulin A nephropathy (IgAN) patients with impaired renal function are still controversial.
Methods
We divided 63 IgAN patients with an estimated glomerular filtration rate (eGFR) of <60 ml/min/1.73 m2 and proteinuria ≥ 0.5 g/day into two groups: the RASI group (RASI, n = 33), treated with RASIs alone; and the combination group (COMBI, n = 30), treated with corticosteroids and RASIs. We analyzed the clinical and histological background, renal survival rate, and the risk factors for progression.
Results
Renal function (mean eGFR: COMBI 46.4 vs. RASI 47.0 ml/min/1.73 m2), the amount of proteinuria (median: COMBI 1.39 vs. RASI 1.17 g/g creatinine) and histological backgrounds were not significantly different between the groups, but urinary red blood cells (U-RBCs) were significantly higher in the COMBI group than in the RASI group (median: COMBI 30.0 vs. RASI 10.0 counts/high-power field, P = 0.0171). The serial change in proteinuria did not differ until 5 years after treatment, but U-RBCs were significantly decreased in both groups (P < 0.0001), and eGFR was significantly decreased in the RASI group (P < 0.001) but not in the COMBI group. The results for each year after treatment did not differ significantly between both groups. The renal survival rate was not significantly different between the groups. There was no independent risk factor for progression by Cox regression analysis.
Conclusion
Combination therapy with steroids and RASIs was not superior to monotherapy with RASIs for advanced IgAN with impaired renal function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The mechanism of deterioration of renal function in immunoglobulin A nephropathy (IgAN) is broadly divided into two categories. One is the pathogenesis of IgAN itself, by which aberrantly glycosylated serum IgA1 causes mesangial IgA deposition and inflammatory changes, such as crescent formation and endothelial hypercellularity in the glomeruli. The other is caused by glomerular hypertension and hyperfiltration that arise from a reduction in the remaining normal, uninjured nephron by glomerular obsolescence [1–3]. The former mechanism can be treated by steroid therapy to suppress inflammatory changes in the glomeruli and interstitium [4, 5], and the latter can be treated by renin–angiotensin–aldosterone system inhibitors (RASIs), such as angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) to suppress glomerular hypertension and hyperfiltration [6–11]. In the case of advanced IgAN with impaired renal function, histological findings suggest a mixed composition of active lesions (such as crescent formation, endothelial hypercellularity, and tuft necrosis) and chronic lesions (such as glomerular obsolescence, segmental sclerosis, adhesion, and interstitial fibrosis). Therefore, these cases should be treated by combination therapy with steroids and RASIs. We have reported the beneficial effect of steroids and RASIs in advanced IgAN patients with impaired renal function [12, 13], and that the effect of ARBs is equivalent to steroid therapy in preventing end-stage renal disease (ESRD) [14]. These results allow us to hypothesize that combination therapy with steroids and RASIs might be superior to monotherapy with RASIs.
In the present study, we compared monotherapy with RASIs and combination therapy with steroids and RASIs in patients with advanced IgAN and impaired renal function.
Methods
Patients
From January 1984 to December 2007, 718 patients were diagnosed with primary IgAN by renal biopsy at Tokyo Women’s Medical University. The diagnosis of IgAN was based on light microscopic findings of mesangial proliferative changes, immunofluorescence study findings of mesangial IgA and C3 deposition, and electron microscopic findings of electron-dense deposits in the mesangial area. Patients with systemic diseases such as diabetes mellitus, collagen diseases, abnormal hypergammaglobulinemia and chronic liver diseases were excluded from the study. We selected all patients who met the following criteria: (1) clinical grade 3 at the time of renal biopsy as determined according to the clinical grading criteria of the Japanese Society of Nephrology at the time of renal biopsy [grade 1, urinary protein excretion (U-Prot) <0.5 g/day; grade 2, estimated glomerular filtration rate (eGFR) ≥60 ml/min/1.73 m2 and U-Prot ≥ 0.5 g/day; grade 3, eGFR < 60 ml/min/1.73 m2 and U-Prot ≥ 0.5 g/day] [13–15]; (2) U-Prot was under the nephrotic range (3.5 g/day) at the time of renal biopsy; and (3) patients were treated by monotherapy with RASIs or combination therapy with steroids and RASIs after renal biopsy. There were 63 patients who met these criteria. Drug prescription was according to each doctor’s decision. We divided the 63 patients into two groups according to the treatment that they had received: (A) RASI group, treated with RASIs (n = 33), and (B) combination therapy (COMBI) group, treated with corticosteroids and RASIs (n = 30). The median observation period was 9.0 years (range 2–24 years) in the RASI group and 8.0 years (range 4–24 years) in the COMBI group. The clinical data that were analyzed in each group included sex, age, body mass index, systolic blood pressure (SBP), diastolic blood pressure, and mean blood pressure. Laboratory data included serum total protein (TP), serum albumin, blood urea nitrogen, serum creatinine (S–Cr), eGFR, serum uric acid, serum total cholesterol, high-density lipoprotein cholesterol, triglyceride (TG), serum IgG, serum IgA, serum IgM, CH50, C3, C4, U-Prot, urinary red blood cells (U-RBCs), urinary β2-microglobulin, and urinary N-acetylglutamate. We also performed survival analysis until reaching 50% decrease of eGFR and progression to ESRD (requiring dialysis or renal transplantation), and analyzed the risk factors for progression to the endpoints.
Histological findings of the renal biopsy specimens
All specimens were obtained by percutaneous needle biopsy. The specimens were fixed with 10% phosphate-buffered formalin (pH 7.2), embedded in paraffin, and cut into 4-μm-thick sections. The sections were stained with hematoxylin and eosin, periodic acid-Schiff, silver methenamine, and Masson trichrome for light microscopic examination.
The histological findings were graded according to the histological grading criteria of the Japanese Society of Nephrology as follows: grade 1, <24.9% of the total number of glomeruli with glomerular lesions; grade 2, 25–49.9%; grade 3, 50–74.9%; and grade 4, >75%. Glomerular lesions were classified as global sclerosis, segmental sclerosis, and crescent formation. The grades were appended with ‘A’ when there were active lesions (e.g., cellular and fibrocellular crescents) and with ‘C’ when there were chronic lesions (e.g., global sclerosis, segmental sclerosis and fibrous crescents) [13–15]. These histological parameters were compared between the RASI and COMBI groups. The combination of clinical and histological grade according to the Japanese Society of Nephrology (Table 1) was also evaluated as follows: low risk for progression to ESRD, medium risk, high risk, and very high risk, i.e., cases that had a high risk of progressing to ESRD within 5 years.
Treatment protocol
In the COMBI group, patients were initially treated with prednisolone at a dose of 0.5–0.8 mg/kg/day for the first 4 weeks, and it was gradually reduced by 2.5–5 mg/month, and continued for at least 2 years. Steroid pulse therapy was administered to four patients. We excluded cases that were treated with other immunosuppressive agents. In the COMBI group, an ACEI was administered to 11 patients and an ARB to 19 patients. In the RASI group, an ACEI was administered to 17 patients and an ARB to 15 patients. The selection of RASIs was not fixed and depended on each doctor’s decision, and the dose of RASIs was adjusted to give blood pressure of 130/80 mmHg. Antiplatelet agents or anticoagulation therapy were also administered to both groups. Tonsillectomy was performed on five patients (16.7%) in the COMBI group, and zero cases (0%) in the RASI group during the follow-up period, but was not significant.
Statistical analysis
Data are expressed as mean ± SD for normally distributed data and median ± inter quartile range (IQR) for non-normally distributed data, and were analyzed using JMP®8.0.1 (SAS Institute Inc, Cary, NC, USA). The unpaired Student’s t test was used for normally distributed data and Mann–Whitney U test for non-normally distributed data. The Chi-squared test was used to compare histological grades and sex distribution at the time of renal biopsy between the steroid and ARB groups. The Friedman test using StatMate for Windows was used to evaluate serial changes in eGFR, U-Prot and U-RBCs. The cumulative renal survival rate until the endpoints was calculated according to the Kaplan–Meier method and log-rank test. Multivariate Cox regression analysis was used to evaluate the risk factors for progression to ESRD in both groups. Differences with P values < 0.05 were considered to be statistically significant in all the analyses.
Results
Comparison of clinical findings at time of renal biopsy in the RASI and COMBI groups
Table 2 shows the clinical findings at the time of renal biopsy between the ARB and steroid groups. SBP was significantly lower in the COMBI group than the RASI group (124.0 ± 14.8 vs. 135.4 ± 15.0 mmHg, P = 0.0036). TP was significantly higher in the RASI group than in the COMBI group (6.67 ± 0.64 vs. 6.29 ± 0.53 mg/dl, P = 0.0152). S–Cr and eGFR were similar between both groups. TG level was significantly higher in the COMBI group than in the RASI group (P = 0.0473). U-Prot was not significantly different between the groups, but U-RBC was significantly higher in the COMBI group than in the RASI group [median 30.0 counts/high-power field (hpf) vs. median 10.0 counts/hpf, P = 0.0171).
Comparison of clinical and histological grades according to the Japanese Society of Nephrology
All patients were classified as clinical grade 3. With regard to histological changes, the frequencies of grades 3 and 4 and the number of chronic lesions tended to be higher in the RASI group than in the COMBI group, but there were no significant differences between the groups by the Chi-squared test. With regard to the combination of clinical and histological grade, all the patients were graded as high risk or very high risk. The number of very high risk cases tended to be larger in the RASI group than in the COMBI group, but there was no significant difference between the groups (Table 3).
Serial changes in clinical parameters between the groups
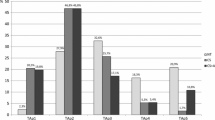
Figure 1 shows the serial change in eGFR from the time of renal biopsy to 5 years after treatment. The serial change from 0 to 5 years after treatment was significantly decreased in the RASI group (P < 0.001), but not in the COMBI group, although eGFR for each year after treatment was not significantly different between the COMBI and RASI groups. Serial change in U-Prot from the time of renal biopsy to 5 years after treatment tended to decrease in both groups, but was not significant. Furthermore, U-Prot for each year after treatment was not significantly different between the groups (Fig. 2). Figure 3 shows the serial change in U-RBC from the time of renal biopsy to 5 years after treatment, and it was significantly decreased in both groups (P < 0.0001 in COMBI group and P < 0.0001 in RASI group). However, there was no significant difference for each year after treatment between the groups, although U-RBC count at the time of biopsy was significantly higher in the COMBI than the RASI group.
Serial changes in eGFR in the COMBI and RASI groups from time of biopsy to 5 years after treatment. Median eGFR (ml/min/1.73 m2) in the COMBI group was 47.3 (39.3–54.1) at the time of renal biopsy, 47.3 (40.4–58.1) at 1 year, 48.4 (39.7–55.6) at 2 years, 44.2 (34.2–50.8) at 3 years, 44.1 (33.7–51.8) at 4 years, and 44.7 (33.6–51.3) at 5 years after treatment. There was no significant difference by the Friedman test from 0 to 5 years after treatment. Median eGFR (ml/min/1.73 m2) in the RASI group was 49.7 (40.4–55.1) at the time of renal biopsy, 46.9 (36.4–52.1) at 1 year, 43.4 (31.3–52.6) at 2 years, 41.4 (28.1–55.2) at 3 years, 42.4 (26.1–57.4) at 4 years, and 41.6 (21.6–52.8) at 5 years after treatment. There was a significant difference by the Friedman test from 0 to 5 years after treatment (P < 0.001). The eGFR for each year after treatment did not differ significantly between the groups by Mann–Whitney U test
Serial changes in U-Prot in the COMBI and RASI groups from time of biopsy to 5 years after treatment. Median (IQR) U-Prot (g/g Cre) in the COMBI group was 1.385 (0.96–1.97) at the time of renal biopsy, 0.505 (0.29–0.97) at 1 year, 0.40 (0.18–0.95) at 2 years, 0.395 (0.11–1.05) at 3 years, 0.33 (0.19–1.03) at 4 years, and 0.46 (0.24–1.02) at 5 years after treatment. The serial change of U-Prot tended to decrease, but there was no significant difference by the Friedman test. Median (IQR) U-Prot (g/g Cre) in the RASI group was 1.17 (0.71–1.65) at the time of renal biopsy, 0.61 (0.16–1.15) at 1 year, 0.78 (0.26–1.49) at 2 years, 0.75 (0.03–1.12) at 3 years, 0.52 (0.12–0.91) at 4 years, and 0.75 (0.17–1.80) at 5 years after treatment. It also tended to decrease, but there was no significant difference by the Friedman test from 0 to 5 years after treatment. Each median U-Prot at 0, 1, 2, 3, 4 and 5 years after treatment did not differ significantly between the groups by Mann–Whitney U test
Serial changes in U-RBCs in the COMBI and RASI groups from time of biopsy to 5 years after treatment. Median (IQR) U-RBCs (counts/hpf) in the COMBI group was 30 (10–100) at the time of renal biopsy, 5 (1–13.75) at 1 year, 5 (1–10) at 2 years, 5 (0.63–10) at 3 years, 5 (0.5–10) at 4 years, and 1 (0.25–10) at 5 years after treatment. There was a significant difference by the Friedman test from 0 to 5 years after treatment (P < 0.0001). Median (IQR) U-RBC (counts/hpf) in the RASI group was 10 (3.5–45) at the time of renal biopsy, 5.5 (1–10) at 1 year, 5 (0.2–10) at 2 years, 2 (0.5–6) at 3 years, 1 (0.175–5) at 4 years, and 1 (1–5) at 5 years after treatment. There was a significant difference by the Friedman test from 0 to 5 years after treatment (P < 0.0001). Each median U-RBC value at 1, 2, 3, 4 and 5 years after treatment did not differ significantly by Mann–Whitney U test between both groups, although U-RBC count during treatment was significantly different between both groups (P = 0.0171) (Table 2)
Survival analysis until 50% decrease in eGFR and ESRD
Figures 4 and 5 show the survival analysis until 50% decrease in eGFR from baseline (Fig. 4) and until the development of ESRD (Fig. 5). The cumulative survival rate was not significantly different between the groups (log-rank test: until 50% decrease of eGFR, P = 0.7665; until ESRD, P = 0.1810).
Risk factors for progression to ESRD
The hazard ratio (HR) of possible risk factors of the development of ESRD is listed in Table 4; they were not effective for predicting progression of renal disease.
Discussion
We hypothesized that combination therapy with steroids and RASIs was superior to monotherapy with RASIs for long-term renal survival and prevention of ESRD, even in patients with advanced IgAN and impaired renal function. We speculated that the anti-inflammatory and immunosuppressive effects of steroid therapy repaired the active histological lesions and the antiglomerular hypertensive and antihyperfiltration effects of RASIs protected the remaining normal glomeruli.
Manno et al. conducted a randomized controlled study to compare combination therapy with steroids and ACEIs and monotherapy with ACEIs. Their inclusion criteria were moderate histological grade, eGFR ≥ 50 ml/min/1.73 m2, and U-Prot ≥ 1.0 g/day, and 48 cases were treated with combination therapy and 49 with ACEI monotherapy. They showed that renal survival rate, doubling of S–Cr, and ESRD after 8 years were significantly better in the combination therapy group than in the ACEI monotherapy group [16]. Lv et al. reported similar results, although their study was smaller in size and had a shorter observation period. Their inclusion criteria were U-Prot ≥ 1.0 g/24 h and ≤ 5.0 g/day, and eGFR ≥ 30 ml/min/1.73 m2 [17]. Choi et al. [18] reported that a combination of steroids and ARBs significantly decreased U-Prot and hematuria and improved renal function over 4 years in 50 patients with IgAN whose S–Cr was <2.0 mg/dl. All these studies support our hypothesis because they also expected the same mechanism for the beneficial effect of steroids and RASIs in IgAN, although they included IgAN patients with normal renal function.
Our results, however, indicated that combination therapy with steroids and RASIs was not superior to monotherapy with RASIs in terms of long-term renal survival rate until 50% decrease in eGFR and ESRD. This unexpected result could have been because the main mechanism for long-term progression of advanced IgAN with impaired renal function was not mainly immunopathology and glomerular and interstitial inflammation, but glomerular hypertension and hyperfiltration caused by activation of the RAS. The decline in the reduction of U-Prot and U-RBC in the COMBI group until 2 years after treatment seemed to be higher than that in the RASI group (U-Prot—COMBI group 1.39 → 0.40 g/g Cre, RASI group 1.17 → 0.78 g/g Cre; U-RBC—COMBI group 30 → 5 counts/hpf, RASI group 10 → 5 counts/hpf); however, U-Prot and U-RBC for each year after treatment were not significantly different between the groups, and the difference between the groups became smaller with each year. Moreover, serial change of eGFR over 5 years was significantly decreased in the RASI group, although the renal function in the COMBI group was maintained over 5 years; however, there was no difference between either group in the renal survival rate over the long-term observation period. These results indicated that the beneficial effect of steroid therapy seemed to be observed earlier, but it did not affect the long-term renal survival. The results of multivariate Cox regression also supported this indication, because combination therapy of RASIs and steroids did not decrease the HR for progression to ESRD. Moreover there was no independent risk factor for progression to ESRD. We suspected that in the cases which already had deteriorated renal function, many small factors might become a risk for progression; therefore, independent risk factors could not be analyzed by multivariate Cox regression. In the studies by Manno et al. the reduction in U-Prot occurred earlier in the combination therapy than in the ACEI monotherapy group during the first 2 years, but was not significantly different after 2 years. This result also indicated that the effect of steroid treatment was only seen during the treatment period, and the long-term renoprotective effect was mainly dependent on the RASIs. They included IgAN patients with normal renal function (mean eGFR 97.5 ml/min/1.73 m2 in the ACEI monotherapy group and 100.4 ml/min/1.73 m2 in the combination group) and moderate histological lesions. We suspect that they also included many cases whose main etiology of renal impairment was active inflammatory change, and that were affected mainly by steroid therapy and minimally by ACEI therapy. Moreover, their study period was shorter than in our study, and we suspect that with our longer study period, patients tended to be more affected by the RASIs than the steroids, because IgAN is a slow progressive renal disease caused by the glomerular hypertension and hyperfiltration. In our study, the longer observation period, severe renal dysfunction and severe histological lesions seemed to lead to quite different results from those of Manno et al. Considering the severe adverse effects of steroid therapy, monotherapy with RASIs should be implemented, and steroid therapy should be carefully given to patients with advanced IgAN and impaired renal function, although IgAN patients with normal renal function or moderate histological lesions should be treated with combination therapy. In our study, several adverse events relating to steroid therapy were observed in the COMBI group: 5 cases of cataract, 1 case of fasting glycemia, 3 cases of hyperlipidemia, 1 cases of osteoporosis, and 1 case of depression. There were no severe adverse events in the RASI group; severe hyperkalemia and unexpected deterioration of renal function were not seen in either group. Careful use of RASIs could prevent as well as aid recovery from these adverse events.
Our study had some limitations. It was a retrospective observational study and some clinical and histological findings at baseline were significantly different between the treatment groups. Manno et al. and Lv et al. carried out randomized controlled trials; therefore, to avoid selection bias, a large, prospective, randomized control study should be conducted. We believe that this is the first step to resolving the therapeutic strategy for patients with advanced IgAN and impaired renal function.
In conclusion, in patients with advanced IgAN and impaired renal function, combination therapy with steroids and RASIs was not superior to monotherapy with RASIs for prevention of progression to ESRD, and steroid treatment for advanced IgAN with impaired renal function should be considered carefully.
References
Locatelli F, Del Vecchio L, Pozzi C. IgA glomerulonephritis: beyond angiotensin-converting enzyme inhibitors. Nat Clin Pract. 2006;2:24–31.
Barratt J, Feehally J. IgA nephropathy. J Am Soc Nephrol. 2005;16:1097–2088.
Tumlin JA, Madaio MP, Hennigar R. Idiopthic IgA nephropathy: pathogenesis, histopathology, and therapeutic options. Clin J Am Soc Nephrol. 2004;2:1054–61.
Cheng J, Zhang X, Zhang W, He Q, Tao X, Chen J. Efficacy and safety of glucocorticoids therapy for IgA nephropathy: a meta-analysis of randomized controlled trials. Am J Nephrol. 2009;30:315–22.
Strippoli GFM. IgA nephropathy: a disease in search of a large-scale clinical trial to reliably inform practice. Am J Kidney Dis. 2009;53:5–8.
Dillon JJ. Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers for IgA nephropathy. Semin Nephrol. 2004;24:218–24.
Cheng J, Zhang W, Zhang XH, He Q, Tao XJ, Chen JH. ACEI/ARB therapy for IgA nephropathy: a meta analysis of randomized controlled trials. Int J Clin Pract. 2009;63:880–8.
Chan JCM, Trachtman H. Modulating the progression in IgA nephropathy. Nephron Clin Pract. 2006;104:61–8.
Dillon JJ. Treating IgA nephropathy. J Am Soc Nephrol. 2001;12:846–7.
Ballardie FW. Quantitative appraisal of treatment options for IgA nephropathy. J Am Soc Nephrol. 2007;18:2806–9.
Laville M, Alamartine E. Treatment options for IgA nephropathy in adults: aproposal for evidence-based strategy. Nephrol Dial Transpl. 2004;19:1947–51.
Moriyama T, Honda K, Nitta K, Yumura W, Nihei H. The effectiveness of steroid therapy for patients with advanced IgA nephropathy and impaired renal function. Clin Exp Nephrol. 2004;8:237–42.
Moriyama T, Amamiya N, Ochi A, Tsuruta Y, Shimizu A, Kojima C, et al. Long-term beneficial effects of angiotensin-converting enzyme inhibitor and angiotensin receptor blocker therapy for patients with advanced immunoglobulin A nephropathy and impaired renal function. Clin Exp Nephrol. 2011;15:700–07.
Moriyama T, Amemiya N, Ochi A, Tsuruta Y, Shimizu A, Itabashi M, et al. Comparison of steroids and angiotensin receptor blockers for patients with advanced IgA nephropathy and impaired renal function. Am J Nephrol. 2011;34:233–40.
Clinical guidelines for immunoglobulin A (IgA) nephropathy in Japan, third version. Nippon Jinzo Gakkai Shi 2001; 53:123–135.
Manno C, Torres DD, Rossini M, Pesce F, Schena FP. Randomized controlled clinical trial of corticosteroids plus ACE-inhibitors with long-term follow-up in proteinuric IgA nephropathy. Nephrol Dial Transpl. 2009;24:3694–701.
Lv J, Zhang H, Chen Y, Li G, Jiang L, Singh AK, et al. Combination therapy of prednisolone and ACE inhibitor versus ACE-inhibitor therapy alone in patients with IgA nephropathy: a randomized controlled trial. Am J Kidney Dis. 2009;53:26–32.
Choi S, Lee D, Jeong KH, Moon JY, Lee SH, Lee TW, et al. Prognostic relevance of clinical and histological features in IgA nephropathy treated with steroid and angiotensin receptor blockers. Clin Nephrol. 2009;72:353–9.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Moriyama, T., Nakayama, K., Ochi, A. et al. Comparison of inhibitors of renin–angiotensin–aldosterone system (RAS) and combination therapy of steroids plus RAS inhibitors for patients with advanced immunoglobulin A nephropathy and impaired renal function. Clin Exp Nephrol 16, 231–237 (2012). https://doi.org/10.1007/s10157-011-0545-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-011-0545-7