Abstract
Background
The number of elderly patients with IgA nephropathy (IgAN) is increasing in parallel with the increased longevity in the general population. However, information is limited regarding the characteristics of such patients.
Methods
IgAN patients who were ≥60 years of age at diagnosis were retrospectively analyzed. The clinicopathological features at biopsy, therapies during the follow-up period, renal outcomes and extrarenal complications were evaluated.
Results
The characteristics of a total of 87 patients were as follows (mean values): 65 years of age, an eGFR of 47 mL/min/1.73 m2, and urinary protein excretion (UPE) of 1.9 g/day. In the initial 1-year follow-up period, UPE decreased from 2.4 to 0.4 g/day in patients treated with corticosteroids and 1.4 to 0.8 g/day in patients treated with conservative therapies, including renin–angiotensin system blockade. During the observation period, 26 % of the patients who received corticosteroids and 38 % of the patients treated with conservative therapies showed a ≥30 % decrease in their eGFR or reached end-stage renal disease. In the analysis of all patients, UPE at 1 year after the diagnosis was identified to be an independent predictor of the subsequent loss of renal function. However, neither corticosteroid therapy nor conservative therapies was identified to be an independent valuable. There was no significant difference in the incidence of the extrarenal complications between patients treated with corticosteroids and those with conservative therapies.
Conclusion
In elderly IgAN patients, the reduction of proteinuria by therapeutic interventions may lead to better renal outcomes without causing severe extrarenal complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The relative proportion of elderly individuals in the general population is increasing worldwide. In 2012, individuals who were ≥60 years of age were estimated to account for 11.5 % of the world’s population. This proportion has been predicted to increase to 21.8 % by 2050 [1]. As the average lifespan increases, the number of elderly patients with renal diseases is increasing, especially in developed countries. Indeed, 27.4 % of the patients who were registered in the Japan Renal Biopsy Registry from 2007 to 2011 were older than 65 years of age, and 10 % of these elderly patients were older than 80 years of age [2]. Thus, there has been a clear increase in the rate of elderly patients with IgA nephropathy (IgAN) in recent years.
IgAN is the most common cause of primary glomerulonephritis worldwide. Previous long-term observational studies have shown that 30–40 % of these patients progress to end-stage renal disease (ESRD) within 20 years [3–5]. Many studies have identified risk factors for the progression to ESRD in IgAN patients. In particular, severe proteinuria, renal impairment, advanced glomerulosclerosis and interstitial fibrosis/tubular atrophy at the time of the diagnosis have been consistently identified as risk factors [4, 5].
Studies on some retrospective cohorts and meta-analyses have suggested that aging or elderly age at the time of the diagnosis is another candidate risk factor for progression [6, 7]. To date, however, there are few reports on elderly patients with IgAN and detailed information, especially with regard to therapies, is limited. The present study therefore analyzed the clinical course of patients with IgAN who were diagnosed at an advanced age. To examine the safety and efficacy of each therapeutic strategy, we performed separate analyses for patients treated with corticosteroids and those treated with conservative therapies.
Materials and methods
The selection of the patients
This study included all patients with primary IgAN who were ≥60 years of age at the time of the diagnosis and underwent renal biopsies at the Jikei Hospital and our affiliated hospitals for the first time from 1992 to 2012; no patient underwent follow-up renal biopsies. IgAN was determined by the predominant deposition of mesangial IgA on immunohistochemistry. Patients with mesangial IgA deposition associated with systemic diseases, such as systemic lupus erythematosus, Henoch-Schönlein purpura, chronic liver disease, or HIV, were excluded from the study. Patients with primary IgAN who were followed for more than 1 year and/or those who achieved a >30 % reduction in the estimated glomerular filtration rate (eGFR) within a year of follow-up were examined. Patients who were followed up for less than 1 year without progression, cases that were missing data that were necessary for the study [such as urinary protein excretion (UPE) or renal function measurements], and renal specimens that contained <8 glomeruli were also excluded from the analysis. A low salt diet (6 g/day), and a low protein diet (0.6–1.0 g/kg of ideal body weight/day) were recommended to all patients according to their degree of renal insufficiency. This study was approved by the ethics review board of the Jikei University School of Medicine (26-261 7767).
Definitions
The eGFR was calculated by applying a modified three variable equation for estimating the GFR for Japanese individuals [8] as follows: eGFR = 194 × age−0.287 × sCr−1.094 (×0.739 if female), where sCr is the serum creatinine. Hypertension was defined as a systolic blood pressure of >140 mmHg and/or diastolic blood pressure of >90 mmHg or the usage of antihypertensive medications. Diabetes was defined as an HbA1c level of ≥6.5 % (NGSP) or the usage of hypoglycemic medications. Dyslipidemia was defined as an LDL cholesterol level of ≥140 mg/dL and/or an HDL cholesterol level of <40 mg/dL and/or a triglyceride level of ≥150 mg/dL or the usage of lipid lowering medications. Hyperuricemia was defined as a uric acid level of ≥7.0 mg/dL or the usage of anti-hyperuricemic medications. Cardiovascular disease was defined as coronary heart disease, cerebrovascular disease, peripheral arterial disease, arrhythmia, deep vein thrombosis or pulmonary embolism. Active infections were defined as infections that required treatment. Hematuria was graded according to the number of red blood cells per high-power field in urinary sediment as 0 if 0–4, 1 if 5–9, 2 if 10–30, 3 if 30–50, and 4 if >50. Patients were defined as being treated with corticosteroids when they were treated based on the pre-defined protocol of corticosteroids during the observation periods. In our cohort, more than half of the patients received a modified version of the protocol proposed by Pozzi et al. (intravenous methylprednisolone 0.5 g per day for 3 consecutive days at the beginning of months 1, 3, and 5 plus oral prednisolone 0.5 mg/kg on alternate days for 6 months) [9]; the other patients received low-dose prednisolone (30 mg/day) as an initial therapy, which was subsequently tapered for 1–2 years during the observational periods. Conservative therapies were defined as therapies that did not include corticosteroids or immunosuppressive medications. The progression of renal function was defined as a >30 % reduction in the eGFR from the baseline or patients who underwent renal replacement therapy [10].
Histopathological analysis
All of the kidney tissue specimens were obtained by a percutaneous needle biopsy. The percentage of glomeruli that were affected by global or segmental sclerosis, mesangial hypercellularity, endocapillary hypercellularity and extracapillary hypercellularity were assessed. These pathological variables were evaluated according to the definitions of the Oxford classification [11]. Acute lesions were defined as the presence of cellular crescent, fibrocellular crescent or glomerulocapillary necrosis. Interstitial fibrosis/tubulointerstitial atrophy was semi-quantitatively evaluated according to the percentage of cortical area involvement.
Statistical analysis
The continuous variables were expressed as the mean ± standard deviation (SD). The normality of the distribution of the variables was assessed using the F test. If the variables were normally distributed, then Student’s t test was used to assess the data to identify significant differences between the two groups. If the variables were not normally distributed, then the Mann–Whitney U and Wilcoxon signed-rank tests were used. Categorical variables were expressed as a percentage and compared using the Chi-square test and Fisher’s exact test. The relationship between the continuous variables and the progression was evaluated by univariate and multivariate logistic regression analyses. Because the distribution of UPE was skewed, the values were log-transformed before the univariate and multivariate regression analyses. P values of <0.05 were considered to be statistically significant. All statistical analyses were performed using the SPSS software package (SPSS, Chicago, IL).
Results
The clinicopathological characteristics at the time of the biopsy
In the initial recruitment, we identified 172 primary IgAN patients from the outpatient population at our hospitals who were ≥60 years of age at the time of the diagnostic biopsy. Of these 172 patients, 71 patients were excluded because they were followed for less than 1 year or because their records were missing data that were necessary for the study, and 14 patients were excluded because their renal specimens contained <8 glomeruli. However, two patients who underwent renal replacement therapy within 1 year after the diagnosis were included in this study.
The mean eGFR was 47 ± 21 mL/min/1.73 m2, the mean UPE was 1.9 ± 1.8 g/day and 17 patients (17 %) showed nephrotic range proteinuria (Table 1). In the histopathological analyses, 39 patients (39 %) showed diffuse mesangial hypercellularity. Global glomerulosclerosis was present in 24 % of the glomeruli, 64 % of the patients had more than 25 % interstitial fibrosis/tubulointerstitial atrophy, and 23 % of the patients had acute glomerular lesions.
The characteristics of the elderly IgAN patients were compared with 250 patients from the retrospective cohort of the Ministry of Health, Labour and Welfare in Japan who were 18–59 years of age (non-elderly group) [12] (Supplemental Table 1). The elderly patients exhibited more severe clinicopathological findings, such as heavy proteinuria, renal insufficiency, and hypertension, and the degrees of chronic histopathological lesions were higher than in non-elderly patients. In contrast, the degree of microscopic hematuria, the number of patients with diffuse mesangial hypercellularity, cellular and fibrocellular crescents, and the frequency of corticosteroid therapy were similar between the two groups.
The clinical findings during the follow-up
During the follow-up period, angiotensin-converting enzyme inhibitors or angiotensin type-1 receptor blockers was administered to 72 (82 %) patients, and corticosteroids were administered to 39 (45 %) patients. Twenty-four percent of the patients showed a UPE rate of ≥1 g/day or more at the end of the follow-up period. At the end of the follow-up, 28 (32 %) of the patients achieved a >30 % reduction in the eGFR and 13 (15 %) of the patients reached ESRD. Two (2 %) of the patients died during the follow-up period: one from a severe asthmatic attack, the other due to a ruptured aneurysm of the thoracic aorta. No deaths were directly related to the therapies (including corticosteroids) (Table 1).
The comparison of the clinicopathological findings and renal outcomes between patients treated with corticosteroids and those treated with conservative therapies
At the time of the biopsy, age, sex, renal function and the frequencies of patients with chronic lesions, such as global glomerulosclerosis and interstitial fibrosis/tubulointerstitial atrophy, did not differ between patients treated with corticosteroids (corticosteroids group) and those treated with conservative therapies (conservative group) (Table 1). In contrast, the level of UPE, the degree of microscopic hematuria, the frequencies of patients with diffuse mesangial hypercellularity and the frequency of acute glomerular lesions were higher in the corticosteroids group than in the conservative group.
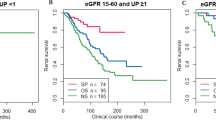
At 1 year after diagnosis, the level of UPE significantly decreased from 2.4 to 0.4 g/day in the corticosteroids group and from 1.4 to 0.8 g/day in the conservative group (Fig. 1). Similarly, the degree of microscopic hematuria was reduced in both groups at 1 year after the diagnosis. During the follow-up period, 10 (26 %) patients in the corticosteroids group and 18 (38 %) patients in the conservative group showed a ≥30 % decrease in their eGFR or reached ESRD.
The univariate and multivariate logistic regression analyses of the factors associated with the progression
The continuous variables at the biopsy and 1 year after the diagnosis were tested for an association with the progression (Table 2). In the univariate analysis, UPE, the eGFR, the prevalence of hypertension at the biopsy, and UPE at 1 year after the diagnosis were found to be significantly associated with the progression. In the multivariate logistic regression analysis, UPE at 1 year after the diagnosis was the only factor that was found to be independently associated with the progression. In contrast, neither corticosteroid therapy nor conservative therapies was identified to be an independent valuable.
Extrarenal complications during the follow-up
During the follow-up period, the rates of patients with hypertension, diabetes, dyslipidemia, hyperuricemia, cardiovascular diseases, malignancies and active infections were evaluated as extrarenal complications (Fig. 2). Patients in both groups showed relatively high frequencies of extrarenal complications, both at the biopsy and at the final observation. The incidences of the extrarenal complications during the observation periods did not significantly differ between the groups.
The frequencies of newly diagnosed extrarenal complications during the follow-up. Elderly IgAN patients had various extrarenal complications at the time of the biopsy, and the incidences of all extra-renal complications increased during the follow-up period. There were no significant differences between the groups regarding the incidences of the extrarenal complications
Discussion
In our current retrospective study, we explored the clinical course of patients with IgAN who were of advanced age at the time of diagnosis. In our cohort, 45 % of the patients were treated with corticosteroids after diagnosis, whereas the remaining 55 % of the patients were treated with conservative therapies. Importantly, the amount of UPE decreased significantly during the initial 1-year follow-up period after the biopsy in both groups. This parameter was shown to be an independent predictor of the renal outcome in this study population. In recent observational studies of patients with IgAN, proteinuria during the follow-up, such as time–average proteinuria and proteinuria at 1 year after the diagnosis, was a significant predictor of the renal outcome [5, 13–15]. Our present results suggest that a reduction in the UPE level improves the renal outcome in elderly IgAN patients in the same manner as it improves the renal outcome in non-elderly IgAN patients. In contrast, corticosteroid therapy and RAS inhibitors were not identified to be predictors of progression, likely due to the presence of a complex interplay with potential selection bias that must be taken into account when considering therapeutic indications for elderly patients, such as frailty, mental status, living environment or the family’s wishes.
Many previous studies have shown that UPE and the eGFR at the time of the diagnostic biopsy are significant predictors of the renal outcome in IgAN patients [16–18]. In this study, however, these variables were not identified to be independent predictors of the renal outcome. This may be explained by the fact that, in addition to having moderate to severe renal dysfunction at the time of the biopsy, most of the present elderly IgAN patients had a relatively larger UPE level. Indeed, we found significant differences in the renal function, UPE, and presence of chronic histopathological lesions, such as tubulointerstitial changes and global glomerulosclerosis, at the biopsy between the elderly patients of the present study and non-elderly IgAN patients ranging from 18 to 59 years of age (Supplemental Table 1). These findings are consistent with the recently reported studies that show the severe and advanced features of IgAN in elderly patients at the time of diagnosis [19, 20]. At present, the precise reasons for the consistent finding of such severe and advanced features in elderly patients with IgAN remain unclear. Our preliminary data show that patients with a long-term history of urinary abnormalities before the diagnosis tended to have severe clinicopathological features. This may simply reflect the differences in the duration from the disease onset to the diagnostic biopsy. In contrast, the degrees of cellular and/or fibrocellular crescents did not significantly differ in comparison to non-elderly IgAN patients (Supplemental Table 1). These results suggest that a persistent and longstanding immunological activity of the disease may also underlie the advanced features of elderly patients (in addition to the age-related effects in the kidneys), including ischemic and hypertensive renal injuries.
In a subgroup of the present cohort, corticosteroid therapy led to a reduction of UPE at 1 year, despite heavy proteinuria at the time of the biopsy. From many previous studies, the therapeutic effectiveness of corticosteroid therapy in patients with IgAN is well established [9, 21–23]. In addition, a recent systematic review confirmed the benefits of corticosteroid therapy in patients with IgAN [23]. However, most of the previous studies excluded patients with severe renal dysfunction, thus the therapeutic effectiveness of corticosteroids could not be observed. Based on these studies, the Kidney Disease Improving Global Outcomes (KDIGO) guidelines for the treatment of GN suggests that IgAN patients with persistent proteinuria (>1 g/day) and a preserved GFR (>50 mL/min/1.73 m2) receive a 6-month course of corticosteroid therapy [24]. In contrast, a large retrospective study recently reported that corticosteroid therapy prevented the decline of the renal function and reduced UPE in IgAN patients with an initial eGFR of <50 mL/min/1.73 m2 [25]. The findings of our present study may therefore support the efficacy of corticosteroid treatment that was observed in elderly IgAN patients characterized by moderate to severe renal dysfunction.
The elderly IgAN patients of the present study had a relatively large number of extrarenal complications at the time of the biopsy and during the follow-up period. However, there was no difference in the incidence of extrarenal complications, such as hypertension, diabetes, dyslipidemia, hyperuricemia, cardiovascular diseases, malignancies or active infections, between the two groups. A recent systematic review showed that corticosteroid therapy was associated with an increased risk of extrarenal complications in IgAN [23], however, the main reason for such results was the increased risk of cushingoid features, and the risk of diabetes was not shown to increase as a result of corticosteroid therapy. Although the spectrum and prevalence of extrarenal complications was relatively high in the elderly IgAN patients, there were no severe complications that led to death in the present study population. These results suggested that corticosteroid therapy is relatively safe even in elderly patients with IgAN who have moderate to severe clinicopathological features.
In the present study, we recruited patients who were older than 60 years of age at the diagnosis because only a few studies are currently available on IgAN patients in this age group. “Elderly” is defined as over 60 years of age according to the definition of the United Nations Population Fund [1], whereas the World Health Organization defines elderly as over 65 years of age [26]. Thus, the definition of elderly is not universal. Importantly, approximately half of the patients in this study were those between 60 and 64 years of age, and we found no significant differences in the clinicopathological features or renal outcomes between patients 60 and 64 years of age and those who were ≥65 years of age. Moreover, we compared the clinicopathological features and renal outcomes according to the difference in the onset age of IgAN. There was no difference in the frequencies of patients who reached ESRD and the decline rate of the renal function, irrespective of the therapies.
There are some limitations associated with the present study. First, potential selection bias exists due to the method of treatment selection. The clinicopathological characteristics at the time of the biopsy were distinctly different in the corticosteroids group and the conservative group. Second, we could not integrate the criteria for selecting the corticosteroid therapy protocols. However, in the corticosteroids group, there was no significant difference in the progression or the degree of reduction of UPE between the patients treated with the modified version of the protocol proposed by Pozzi and those treated with oral low-dose prednisolone therapy. Third, this study was retrospectively designed. Further prospective studies are therefore needed in order to clarify the precise nature and the safety and efficacy of therapies in elderly IgAN patients.
In conclusion, the results of this retrospective study suggested that therapeutic interventions, including those using corticosteroid therapy, reduce UPE and lead to a better renal outcome without causing severe extrarenal complications in elderly IgAN patients, despite the presence of severe and advanced clinicopathological features at the time of the diagnosis. Further studies are required to better develop therapeutic strategies that can be safely and effectively applied to the treatment of IgAN patients who are of advanced age at the time of the diagnosis.
References
UNFPA and HelpAge International. Ageing in the twenty-first century: a celebration and a challenge. 2012.
Yokoyama H, Sugiyama H, Sato H, et al. Renal disease in the elderly and the very elderly Japanese: analysis of the Japan Renal Biopsy Registry (J-RBR). Clin Exp Nephrol. 2012;16:903–20.
D’Amico G. The commonest glomerulonephritis in the world: IgA nephropathy. Q J Med. 1987;64:709–27.
Manno C, Strippoli GF, D’Altri C, et al. A novel simpler histological classification for renal survival in IgA nephropathy: a retrospective study. Am J Kidney Dis. 2007;49:763–75.
Le W, Liang S, Hu Y, et al. Long-term renal survival and related risk factors in patients with IgA nephropathy: results from a cohort of 1155 cases in a Chinese adult population. Nephrol Dial Transplant. 2012;27:1479–85.
Goto M, Kawamura T, Wakai K, et al. Risk stratification for progression of IgA nephropathy using a decision tree induction algorithm. Nephrol Dial Transplant. 2009;24:1242–7.
Duan ZY, Cai GY, Chen YZ, et al. Aging promotes progression of IgA nephropathy: a systematic review and meta-analysis. Am J Nephrol. 2013;38:241–52.
Matsuo S, Imai E, Horio M, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Pozzi C, Bolasco PG, Fogazzi GB, et al. Corticosteroids in IgA nephropathy: a randomised controlled trial. Lancet. 1999;353:883–7.
Levey AS, Inker LA, Matsushita K, et al. GFR decline as an end point for clinical trials in CKD: a scientific workshop sponsored by the National Kidney Foundation and the US Food and Drug Administration. Am J Kidney Dis. 2014;64:821–35.
Working Group of the International IgA Nephropathy Network, The Renal Pathology Society, Roberts IS, Cook HT, Troyanov S, et al. The Oxford classification of IgA nephropathy: pathology definitions, correlations, and reproducibility. Kidney Int. 2009;76:546–56.
Kawamura T, Joh K, Okonogi H, et al. A histologic classification of IgA nephropathy for predicting long-term prognosis: emphasis on end-stage renal disease. J Nephrol. 2013;26:350–7.
Donadio JV, Bergstralh EJ, Grande JP, et al. Proteinuria patterns and their association with subsequent end-stage renal disease in IgA nephropathy. Nephrol Dial Transplant. 2002;17:1197–203.
Hirano K, Kawamura T, Tsuboi N, et al. The predictive value of attenuated proteinuria at 1 year after steroid therapy for renal survival in patients with IgA nephropathy. Clin Exp Nephrol. 2013;17:555–62.
Reich HN, Troyanov S, Scholey JW, et al. Remission of proteinuria improves prognosis in IgA nephropathy. J Am Soc Nephrol. 2007;18:3177–83.
Geddes CC, Rauta V, Gronhagen-Riska C, et al. A tricontinental view of IgA nephropathy. Nephrol Dial Transplant. 2003;18:1541–8.
Frimat L, Briancon S, Hestin D, et al. IgA nephropathy: prognostic classification of end-stage renal failure. Nephrol Dial Transplant. 1997;12:2569–75.
Berthoux F, Mohey H, Laurent B, et al. Predicting the risk for dialysis or death in IgA nephropathy. J Am Soc Nephrol. 2011;22:752–61.
Wen YK, Chen ML. Differences in new-onset IgA nephropathy between young adults and the elderly. Ren Fail. 2010;32:343–8.
Oshima Y, Moriyama T, Itabashi M, et al. Characteristics of IgA nephropathy in advanced-age patients. Int Urol Nephroly. 2015;47:137–45.
Pozzi C, Andrulli S, Del Vecchio L, et al. Corticosteroid effectiveness in IgA nephropathy: long-term results of a randomized, controlled trial. J Am Soc Nephrol. 2004;15:157–63.
Katafuchi R, Ninomiya T, Mizumasa T, et al. The improvement of renal survival with steroid pulse therapy in IgA nephropathy. Nephrol Dial Transplant. 2008;23:3915–20.
Lv J, Xu D, Perkovic V, et al. Corticosteroid therapy in IgA nephropathy. J Am Soc Nephrol. 2012;23:1108–16.
Radhakrishnan J, Cattran DC. The KDIGO practice guideline on glomerulonephritis: reading between the (guide)lines–application to the individual patient. Kidney Int. 2012;82:840–56.
Tesar V, Troyanov S, Bellur S, et al. Corticosteroids in IgA nephropathy: a retrospective analysis from the VALIGA study. J Am Soc Nephrol. 2015;. doi:10.1681/ASN.2014070697.
World Health Organization. Good health adds life to years. Global brief for World Health Day. 2012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Okabayashi, Y., Tsuboi, N., Haruhara, K. et al. Reduction of proteinuria by therapeutic intervention improves the renal outcome of elderly patients with IgA nephropathy. Clin Exp Nephrol 20, 910–917 (2016). https://doi.org/10.1007/s10157-016-1239-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-016-1239-y