Abstract
In anticipation of the “Chiari and Syringomyelia Consensus Conference” held in Milan in 2019, we performed a systematic literature review on the management of Chiari malformation type 1 (CM1) and syringomyelia (Syr) in children.
We aimed to summarize the available evidence and identify areas where consensus has not been reached and further research is needed.
In accordance with PRISMA guidelines, we formulated seven questions in Patients-Interventions-Comparators-Outcomes (PICO) format. Six PICOs concerned CM1 children with/without additional structural anomalies (Syr, craniosynostosis, hydrocephalus, tethered cord, and cranio-vertebral junction anomalies), and one PICO Syr without CM1. We searched Medline, Embase, Cochrane, and NICE databases from January 1, 1999, to May 29, 2019. Cohort studies, controlled and randomized clinical trials (CCTs, RCTs), and systematic reviews were included, all pertinent only to patients ≤ 18 years of age.
For CM1, 3787 records were found, 460 full texts were assessed and 49 studies (46 cohort studies, one RCT, and two systematic reviews) were finally included. For Syr, 376 records were found, 59 full texts were assessed, and five studies (one RCT and four cohort studies) were included. Data on each PICO were synthetized narratively due to heterogeneity in the inclusion criteria, outcome measures, and length of follow-up of the included studies.
Despite decades of experience on CM1 and Syr management in children, the available evidence remains limited. Specifically, there is an urgent need for collaborative initiatives focusing on the adoption of shared inclusion criteria and outcome measures, as well as rigorous prospective designs, particularly RCTs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chiari malformation type 1 (CM1) and syringomyelia (Syr) are increasingly diagnosed due to both the widespread use of magnetic resonance imaging (MRI) and increased clinical awareness [1, 2]; however, despite the accumulation of experience, the management of these disorders still poses clinical challenges.
CM1, radiologically defined by the position of the cerebellar tonsils herniated through the foramen magnum of five mm or more, constitutes a heterogeneous group of clinical and radiological conditions. It can be diagnosed as an isolated anomaly or in association with skeletal abnormalities of the cervical spine and cranio-vertebral junction (CVJ), Syr, craniosynostosis, hydrocephalus, tethered cord, and in a wide range of syndromic or non-syndromic clinical conditions [3, 4]. Children may present as asymptomatic or with subtle and not strictly specific signs and symptoms as well as with signs and symptoms related to associated pathologies [1, 4]. As a result, CM1 symptomatic children represent an issue for clinicians who, after making every effort to exclude all other non-Chiari origins of patient’s symptoms, judge symptoms as Chiari-related primarily based on experience and personal judgment [1].
Currently, the only treatment to reduce symptoms is posterior fossa decompression surgery with or without duraplasty, with or without excision of the cerebellar tonsils. However, there is no complete consensus on whether, when, and how to treat children with CM1; uncertainty arises from the variability of presentation of CM1 and the paucity of data on the natural history of untreated patients and the long-term outcome of those treated.
Syr refers to a longitudinally oriented fluid-filled cavity of any size in the spinal cord expanding from the region of its largest diameter in the upper and/or lower direction. The definition, diagnosis, and classification of Syr still raise many questions as not every fluid-filled cavitation of the spinal cord deserves the diagnosis of Syr, and the distinction between Syr and central canal dilatation or hydromyelia may be difficult [5,6,7].
It is universally accepted that Syr is not a disease of the spinal cord on its own, but a secondary event related to a disturbance of the cerebro-spinal fluid (CSF) flow for spinal cord tethering, intramedullary tumors, cysts, arachnoiditis due to previous infections, and traumatic events. Therefore, when Syr is present, further diagnostic efforts must be undertaken to determine the underlying pathology and consequently to focus the treatment because the natural history of significant Syr is a progressive loss of neurological function over years or decades [7].
As experience accumulates, indications for management are evolving but, despite the growing body of literature on CM1 and Syr, a lot of issues remain unclear.
In this scenario, CM patients’ associations are growing, identifying referral centers and promoting international conferences to bring experts together and share a common course of action.
In anticipation of the organization of the “Chiari and Syringomyelia Consensus Conference” held in Milan in 2019 [8, 9], as members of the scientific panel we performed a systematic literature review regarding the management of CM1 with or without other structural anomalies and Syr without CM1 in children.
We aimed to summarize the available evidence and to identify areas where the consensus has yet to be reached and further research is needed.
Methods
We performed a systematic search of the literature on the management of CM1 with or without associated structural anomalies (Syr, craniosynostosis, hydrocephalus, tethered cord, and CVJ anomalies), and Syr without CM1 in children, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement [10].
Formulation of the clinical questions
Seven clinical questions were formulated in Patients-Interventions-Comparators-Outcomes (PICO) format by a panel of one pediatric neurologist (VS), three neurosurgeons (LM, PP, LV), one neurophysiologist (PC). Six PICOs concerned CM1 with or without associated malformations, and one Syr without CM1 (Appendix 1 Table 9).
Data sources and search strategy
An expert librarian (SM) drew the searches for the following databases: Medline-PubMed, Embase, The Cochrane Library, and NICE (National Institute for Health and Care Excellence, UK). Combinations of the following subject headings and keywords were used across all databases: “Arnold Chiari malformation” or “CM1” or “CIM” and several synonyms. A specific search strategy was drawn for PICO 7. The full electronic search strategies are included in Appendix 2.
The searches were launched on May 29, 2019, to prepare the “Chiari and Syringomyelia Consensus Conference” to be held in Milan in November 2019 [8, 9].
Eligibility criteria
Participants were children (18 years or younger), with a diagnosis of CM1 with or without associated malformations, and Syr without CM1. Children with CM non-type 1, myelomeningocele, and spina bifida were excluded. Studies with mixed population (for age range or diagnosis) were considered only if data for children were available. No restrictions were made in terms of interventions and comparators. The outcome measures we considered were the following: change or appearance of symptoms and signs, change in the degree of herniation of the cerebellar tonsils, change or appearance of syringomyelia and hydrocephalus, CSF flow changes, surgical complications, need for operation or reoperation.
Eligible studies were prospective and retrospective cohort studies, controlled clinical trials (CCTs), randomized controlled clinical trials (RCTs), and systematic reviews/meta-analyses published from January 1, 1999, to May 29, 2019. We excluded case reports (up to 3 children), abstracts in congress proceedings, and studies published in languages other than English.
Identification of relevant studies
Study selection was performed by a trained researcher (MF). After deleting duplicate citations, the title and abstract of all publications were screened to assess suitability for inclusion. Publications considered potentially eligible were read in full by two researchers (MF, LV), and a third researcher (AS) was involved when consensus on the study was not achieved.
Data synthesis
For each included study, information was extracted by one researcher (MF) and checked by another (AS). These researchers appraised the quality of the studies using section A of the Critical Appraisal Skills Programme (CASP) tool for cohort studies [11] and following Higgins et al. for CCTs and RCTs [12]. Results were synthesized qualitatively.
Results
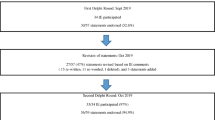
The search strategy retrieved 3787 articles for PICOs 1–6. After duplication removal, 2200 potentially relevant publications were identified. Following the selection process depicted in Fig. 1, 460 full texts were read and evaluated and 49 articles were considered eligible for this review, including two systematic reviews, one RCT, and 46 case series (Fig. 1).
Flowchart of the selection process (PICO1-6). *Any condition/symptom in which the focus of the study was that symptom/condition and CM1 was accidentally discovered (i.e., idiopathic scoliosis, headache, vertigo, etc.); **authors were contacted, but no replay was received; ***some papers cover more than one PICO: 9 for PICO1; 8 for PICO2; 21 for PICO3; 8 for PICO4; 4 for PICO5; 2 for PICO6
For PICO 7, 376 records were screened, 59 articles were assessed, and five studies, including one RCT and four case series, were encompassed in the review (Fig. 2).
Results are presented by PICO, and followed by a short commentary.
-
PICO 1: For asymptomatic CM1 children, which are the effects of neurosurgery versus conservative management on the clinical and radiological outcome?
-
PICO 2: For symptomatic CM1 children, which are the effects of neurosurgery versus conservative management on the clinical and radiological outcome?
To answer PICO 1 and 2 (Table 1 and Table 2), we identified only one cohort study that compared the effects of surgical treatment versus conservative management in 95 CM1 children, both asymptomatic and symptomatic, monitored with long-term clinical and radiological follow-up [13]. Additional eight cohort studies focused on the short- and long-term outcomes of asymptomatic and mildly symptomatic CM1 children managed without surgery [14,15,16,17,18,19,20,21], and four cohort studies described the short- and long-term effects of surgery in symptomatic CM1 children [1, 3, 22, 23].
All retrospective except for two [20, 22] collectively these studies reported the data of:
-
930 CM1 children treated conservatively. Of these, 230 (24.7%) were classified as asymptomatic at inception, 105 (11.3%) as mildly symptomatic, while for 595 (64%) no clear distinction was made between asymptomatic and mildly symptomatic [13,14,15,16,17,18,19,20,21];
-
558 CM1 children treated with surgery for their clinical and/or neuroradiological picture [1, 3, 13, 22, 23]. We omitted the series of 130 children described by Tubbs et al. in 2003 since these data were part of a subsequent study [1, 3].
In the group of patients managed conservatively, when the information was available, mildly symptomatic children ranged from 11.3% [16] to 68.6% [13]. During follow-up, ranging from 9 months to 19 years, the clinical outcome was characterized by stability or improvement in most children (from 72.7 to 100%). Resolution of symptoms was reported in a minority of cases; worsening of symptoms was reported from 4.8 to 28.6%, and new symptoms occurred in 6.3% of children. As for the radiological outcome, tonsillar ectopia remained stable in 64.1% of children, improved in 25.7%, worsened in 6.3%, and resolved in 5.9%. Similarly, Syr unfrequently worsened (up to 15.4%) or appeared (up to 21.4%). During follow-up, 50 of the 930 patients (5.3%) required surgical treatment, 32 (64%) for clinical reasons and 18 (36%) for radiological causes represented by Syr in 14 and ventriculomegaly in four [13,14,15,16,17,18,19,20,21].
Operated CM1 children were followed up from 2 months to 18 years, showing clinical improvement from about 80% up to 100%, and stabilization or improvement of Syr in near all subjects [1, 3, 13, 22, 23]. Indeed, in the group of 500 operated children with posterior fossa decompression and duraplasty, only 1.4% of 285 Syr increased [3]. Moreover, new or increased Syr appeared in four of 25 (16%) operated CM1 children in the study by Pomeraniec et al. [13]. None of the authors reported worsening of tonsillar herniation or cerebellar prolapse, but an improvement was described in the 25 children operated by Pomeraniec et al. with an average ascent of 10 mm, and in seven out of 22 (31.8%) children operated by Knerlich-Lukoschus et al. with an ascent of more than two mm upwards [13, 23]. The complication rate was very low (from 0 to 2.4%) and a new operation was required in 3% [3] to 20% of children [13]; in most instances, reoperation was for persistent Syr, rarely for unchanged symptoms.
Commentary
In the interval period we considered for the literature review, 13 pediatric case series were published with the aim of (a) describing the natural history of asymptomatic or minimally symptomatic CM1 children, (b) determining the frequency with which such patients eventually develop symptoms requiring surgical treatment, (c) identifying clinical and radiological predictors or risk factors and appropriate surgical candidates in this population, (d) analyzing surgical effects. Such information is of great importance for the evidence-based management and surgical decision-making in CM1 children.
The studies about conservative management, all retrospective except for one [20], were not conducted with overlapping inclusion criteria: some included only asymptomatic patients [18, 20], others even those mildly symptomatic [13,14,15,16,17, 19, 21]; some only patients without Syr [20, 21] and/or ventriculomegaly [16, 20, 21], others also patients who presented with such radiological findings [13,14,15,16,17,18,19,20]. Furthermore, the follow-up was not homogeneous either in terms of timing or method; indeed, in some studies, the patients were evaluated only by neurosurgeons [14], while in others also by pediatric neurologists and/or otolaryngologists [17, 21], and in some cases with the aid of neurophysiological investigations such as evoked potentials and polysomnography [13, 18]. Some patient groups were evaluated both clinically and radiologically, while other patients had no follow-up imaging studies [16, 19]. Finally, the surgical criteria were clearly specified in only two articles [19, 21] because not all centers followed a rigorous protocol to determine whether to surgically treat a CM1 child [17].
However, despite these differences and biases, the researchers came to similar conclusions: CM1 children who initially do not require surgery as they are asymptomatic or mildly symptomatic generally follow a benign course and can be managed conservatively as only about 5% of them during follow-up require surgical treatment for clinical or radiological reasons (Syr or ventriculomegaly).
The few published studies on the effects of surgical treatment [1, 3, 22, 23] are all retrospective, with the exception of Andersen and coworkers’ study [22]. The authors aimed to study the effect of bone decompression on auditory evoked potentials of the intraoperative Brainstem Auditory Evoked Potentials (BAEP) as an indicator of the effectiveness of bone decompression even without duraplasty; it is not clear, however, whether improvement in BAEPs can be considered a good indicator of subsequent postoperative clinical improvement [22].
Regarding the other three series of pediatric cases [1, 3, 23], two reported the long-term clinical and radiological outcomes of a large number of operated CM1 children suffering from various pathologies in association with CM1 [1, 3].
The goals of surgical management include the improvement of clinical symptoms, the ascent of the cerebellar tonsillar ectopia, and, if present, the reduction of Syr, by relieving pressure on the brainstem and restoring CSF flow. In symptomatic CM1 children, with or without Syr, surgery is indicated as being effective in almost all children, and sufficiently safe as it lacks a high complication rate [1, 3].
No study compared surgical treatment versus conservative management in symptomatic CM1 children, but Pomeraniec et al. reviewed 95 children of which 25 were surgically managed [13]. The authors reported that surgery was associated with better clinical and radiological outcomes: symptoms improved in 41.7% of conservatively managed patients and in 75% of surgically treated ones; in the conservative group, neither of the two patients with Syr showed syrinx improvement and three patients (4.3%) developed new Syr, whereas 87.5% of 16 surgically treated children showed improvement or resolution of the Syr. The authors concluded that appropriately selected symptomatic patients and those with Syr should be surgical candidates because of the high rates of clinical and radiological improvement.
Some studies aimed to identify clinical and/or neuroradiological risk factors in CM1 children as the limited understanding of the progression and of risk factors increases the ambiguity of defining surgical indications. Some clinical factors, unlike radiological characteristics, have proved to be of predictive value: an increased risk of significant neurological symptoms was observed in older children [15]; older age at diagnosis was also predictive of headache onset [15], while younger age predicted both improvement in symptoms [19] and Syr changes (improvement or worsening) [17]. Again, in the follow-up, an age inferior to 6 years old correlated to a risk of increased tonsillar ectopia, but the age between 6 and 18 years correlated to a reduction of tonsillar ectopia [16]. Regarding symptoms, the presence of cough-headache was a significant negative predictor of symptom improvement, whereas non-tussive headaches were a positive predictor for clinical improvement [19]. In addition, patients with a symptom duration of less than 2 years seem to have better outcomes after surgery [3].
In contrast, none of the radiological characteristics, including initial degree of tonsillar ectopia, tonsillar morphology, CSF flow at the foramen magnum, seems to be predictive of headache, significant neurologic symptoms development, the need for future surgery or postoperative resolution [1, 15, 17, 20].
More recently (after May 29, 2019), one review and three case series on the natural history of CM1 children have been published [24,25,26,27]. These studies came to largely overlapping conclusions: within 6 months of the first visit, 10–15% of CM1 children require surgery, in most cases due to the presence of Syr which seems the only statistically significant factor for the need for surgery [26, 27]; however, children not treated surgically at the time of diagnosis are unlikely to require surgery over time. Indeed, the evolution of CM1 was benign in most cases with the development of new symptoms or new syrinx in a smaller subgroup (from 6.4 to 7.2%) of asymptomatic or incidentally diagnosed initially managed conservatively children [26, 27].
-
PICO 3: For children with CM1 selected for surgery, without associated malformations, is bone cranio-vertebral decompression the most effective intervention?
The literature search found 22 papers satisfying our inclusion criteria: one RCT [28], 19 retrospective cohort studies [29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49], and two systematic reviews with meta-analysis [50, 51], all focusing on the comparison between posterior fossa decompression with bone decompression only (PFDO) and PFD with duraplasty (PFDD). The systematic reviews reported on nine of the 19 cohort papers. The description of the included studies is presented in Table 3 and their quality evaluation is reported in Appendix 3 Tables 10 and 11 [11]. Findings on each outcome measure are summarized in Table 4.
Duration of surgery was reported in 2/19 cohort studies. The mean duration was 105 min for the 63 children treated with PFDO versus (vs) 169 min for those treated with PFDD (n = 47) in the study by Litvak et al. [35]; it was 90 min in the 29 children treated with PFDO vs 148 min in the 36 children treated with PFDD in the study by Lee A et al. [38].
Figures were 119 min for 45 PFDO vs 166 min for 45 PFDD in the RCT [28].
The mean length of stay (reported in 7/19 studies) was between 2 [44] and 4 days [30] for PFDO; it was between 3 [38] and 7 days [43] for PFDD. In the RCT, the mean length of stay was 8 (PFDO) vs 10 days (PFDD) [28] (Table 4).
Surgical complications were reported in 13/19 cohort studies for PFDO; eight studies (62%) had < 5% surgical complications [30, 32, 35, 40, 42, 43, 46, 48]; two studies (15%) had 5–10% complications [29, 44], and three studies (23%) had 11–20% complications [38, 45, 49]. Figures for PFDD were from 14 studies: two studies (14%) with < 5% surgical complications [32, 42], seven studies (50%) with 11–20% complications [30, 35, 39, 40, 45, 46, 49], and five studies (36%) with > 20% complications [29, 38, 43, 44, 48]. The RCT found surgical complications in 12.5% of PFDO and in 57.1% of PFDD; no significant between-group difference in bleedings was reported [28] (Table 4).
Revision surgery was reported in 10/19 cohort studies. In PFDO-treated patients, it was needed in 0% of children in nine of the studies [29, 30, 35, 38, 40, 43, 44, 48, 49] and in 0.7% of children in one study [42]. Figures for PFDD-treated children ranged between 2% [35] and 19% [29]. The RCT reported 0% revision surgery for both procedures [28] (Table 4).
Overall improvement data were reported in 14/19 cohort studies. The data were presented as percentages (10 studies), change in scale values (3 studies), and report (1 study). The RCT reported this outcome with the Chicago Chiari Outcome Scale (CCOS) [28]. For one study with a scale value, a transformation in percentage was possible [49].
Overall improvement for PFDO ranged from 47% [31] to 100% [33, 47], and was ≥ 90% in 5/11 studies. For PFDD, figures ranged from 64% [44] to 100% [33, 47]; 4/11 studies reported an improvement ≥ 90%.
Three children out 4 improved after PFDO, and 3/3 after PFDD in one study on CM1 with sleep apneas [41]. Two cohort studies [38, 43] and the RCT [28] reported no difference between the two surgical techniques on the CCOS score (Table 4).
All the 20 studies had a subgroup of CM1 with syrinx, but only seven reported data on syrinx improvement for the two surgical procedures. For PFDO, improvement ranged from 40% [33] to 100% [38]; syrinx improvement was ≥ 80% in 3/7 studies. For PFDD, it ranged from 60% [44] to 100% [33] and syrinx improvement was ≥ 80% in 6/7 studies. No statistical difference on this outcome was found in five studies reporting on 53 PFDO and 139 PFDD [33, 38, 40, 43, 44], and it was commented as “no difference in percentage” in 70 Syr with the two surgical approaches [49] or no analyzed/commented in 6 PFDO (66.7% improved) vs 20 PFDD (85% improved) [30]. In the RCT, figures were 82.5% (PFDO) vs 90.5% (PFDD) and the difference was not statistically significant [28] (Table 4).
The reoperation rate was reported in 14/19 cohort studies for PFDO: it was < 5% in two of the studies [35, 43]; 5–10% in five studies [30, 32, 40, 44, 47]; 11–20% in three studies [29, 33, 48]; > 20% in four studies [41, 45, 46, 49]. It was reported in 13 cohort studies for PFDD: it was < 5% in four studies [30, 33, 35, 47]; 5–10% in four studies [32, 43, 45, 48]; 11–20% in three studies [29, 40, 49]; > 20% in two studies [41, 46].
Only four studies reported statistical analysis, with no statistical difference for the two groups [35, 46, 48, 49]. The RCT did not report on this outcome [28].
Commentary
The choice of the best surgical treatment of CM1 children without associated malformations is challenging and not clear at the state of art.
We focused on comparing PFDO and PFDD, with or without tonsillar resection. PFDD, a more aggressive choice, is associated with longer surgery and hospitalization times and higher complication rates. Consequently, some authors have suggested the use of ultrasound to optimize the surgical strategy avoiding unnecessary maneuvers and ensuring sufficient decompression [29, 32, 33, 40, 48]; however, the evidence to support this advice is weak (level 4 of evidence).
Concerning Syr, PFDD seems not advantageous over PFDO. Revision surgery comparison for the two techniques was not statistically significant in 3/4 studies [28, 35, 38]; the US KID database reported a p = 0.01 favoring PFDO, when comparing 1593 PFDO vs 1056 PFDD [42]. Considering the overall clinical improvement, one review [51] reported PFDD superiority, but all the included studies using a validated scale for clinical outcome reported no differences [28, 38, 43, 49]. In our report, overall improvement was not significant in 8/9 studies. It was p = 0.05 and favored PFDD only in one [31]. One study reported a multivariate model analyzing symptom-free survival and adjusting for all variables differing between the two groups: PFDO was associated with a twofold increased risk of symptom recurrence only in children with tonsillar herniation caudal to C1 (p = 0.034), proposing the concept of specific subgroup tailored surgery [32].
In the literature for surgery in the CM1 children population, we found no homogeneity in recruitment criteria. Methodology varied substantially between studies and also the radiological definition of CM1 was not homogenous. Clinical outcomes evaluation was frequently difficult to compare across studies. The timing for reporting the selected outcomes was extremely variable and not consistent among studies. The statistical analysis was done on population samples too small for appropriate analysis with stratifications or adjusting for confounders.
The two reviews on this topic underlined the low level of quality and the presence of several biases in the studies included in the meta-analysis [50, 51].
-
PICO 4. For children with CM1 and associated malformations (hydrocephalus or craniosynostosis or tethered cord), which is the most effective surgical approach?
-
PICO 5. For CM1 children with cranio-vertebral junction malformation, is cranio-vertebral decompression more effective than other surgical approaches?
The management of some diseases associated with CM1 is controversial because of the still unclear pathogenesis and for the difference in the therapeutic options adopted by the different centers. The review of the literature did not show any high level of evidence to support specific theories or strategies. No trials nor systematic reviews have been published so far.
Thirteen retrospective studies (level 4 of evidence) fulfilled the selection criteria (Tables 5 and 6). In four articles, the association between CM1 and craniosynostosis was analyzed [52,53,54,55]. One study pointed out some epidemiological data on such association in a series of 383 children treated for craniosynostosis [55]. 7.5% of patients (29 cases) showed CM1 mainly as a result of pansynostosis, lambdoid or multisutural synostosis, the presence of venous anomalies (28%), syndrome (45%), or hydrocephalus (52%) being the most important findings shared by the two conditions. In 13 cases, only the repair of the craniosynostosis was realized with good results on CM1. The simultaneous performance of craniosynostosis repair and suboccipital decompression was indicated as safe and effective in selected cases (syndromic and/or lambdoid synostosis) by another study [54]. On the other hand, foramen magnum decompression alone was found to be effective in improving significantly central sleep apneas in children with syndromic synostosis and CM1 [52]. The last study revealed that there is a predominance in the tonsillar descent to the synostotic suture side in asymmetric craniosynostosis cases [53].
Three papers concerned the association between CM1 and hydrocephalus [1, 3, 39]. Hydrocephalus was present in 11% of cases in the large series (130 cases) described by Tubbs and coworkers in 2003 [1] and in 9.6% of cases in the update (500 cases) provided in 2011 [3]. The correct functioning of CSF shunt was verified prior to suboccipital decompression of hydrocephalic patients. In the third study, children with hydrocephalus were grouped separately from those with CM1 alone or with syringomyelia [39]. In this subset of patients (8 cases), the hydrocephalus was treated first (CSF shunt) and only one patient required suboccipital decompression.
There was only one study addressing the association between CM1 and tethered cord [56]. The incidence of CM1 among 170 children who underwent spinal cord detethering was 10% (17 cases). All patients showed an improvement of their symptoms, which were considered related to tethered cord rather than CM1 (headache, lower extremity sensory disturbance, constipation, scoliosis, urinary incontinence, toe walking, etc.). No radiological modification of the tonsillar descent was obtained.
Finally, the study by Balestrino et al., who reported on 31 children with associated anomalies out of 172 pediatric CM1 (16 with hydrocephalus, 6 with craniosynostosis, and 9 with tethered cord), confirmed the attitude of treating the symptomatic associated condition first. Among them, 37.5% of hydrocephalic children, 50% of those with craniosynostosis, and 22.2% of those with tethered cord also required the foramen magnum decompression for their CM1 [57].
The last four studies reported on the association between CM1 and other CVJ anomalies [58,59,60,61]. The first study emphasized that a ventral compression of the brainstem is a common finding in CM1 children and young adults (48% and 28% out of 40 patients had flattening and distortion of the brainstem, respectively) but only a minority of them (5%) show a real basilar invagination [58]. A one-step treatment by means of suboccipital decompression and posterior fixation was proposed for the management of CM1 and basilar invagination based on a preliminary and successful experience on 11 children [59]. Basilar invagination, clival-axial angle < 125°, and Chiari 1.5 were found to be the main risk factors predicting the need for posterior fixation [60]. The last study investigated the possibility of successful treatment with atlanto-axial fixation not only CM1 children with basilar invagination but also those without manifest bone anomalies [61].
Commentary
Craniosynostosis
Maldevelopment of posterior fossa (PF), premature fusion of sutures and basal synchondroses, and comorbidities (e.g., venous hypertension, OSAS) account for an incidence of CM1 in syndromic synostosis as high as 80–100% [62]. An associated large foramen magnum (reduced A-P diameter but wide L-L diameter) would favor the tonsillar descent, while a small one (both A-P and L-L diameters reduced) would prevent it [63, 64]. Moreover, about 5–6% of children with isolated sagittal synostosis, 45–60% with lambdoid synostosis, and 60% with Mercedes-Benz synostosis harbor CM1 [65,66,67,68].
Since an etiologic treatment is suggested for CM1 whenever possible, the craniosynostosis is treated first [55]. The early recognition of unisutural synostosis is therefore mandatory to avoid management mistakes. The benefic effects on CM1 come from the PF expansion (direct decompression of the PF, improvement of possibly associated hydrocephalus) and/or from the anterior distraction (relief from raised intra-cranial pressure). Some authors proposed to maximize the bi-parieto-occipital expansion through a posterior vault distraction both in syndromic and non-syndromic uni- or bi-lambdoid synostoses [69] or even in CM1 subjects without craniosynostosis [70]. The latter proposal seems reasonable only in case of repeatedly failed foramen magnum osteo-dural decompression, also because of the high rate of complications (50%) [71].
A certain debate exists about the management of CM1 and Syr in children with a late diagnosis of craniosynostosis [54, 72, 73]. A reliable option is to address CM1 in case of specific symptoms/syringomyelia and the synostosis in case of raised intra-cranial pressure (ICP) [74, 75]. ICP monitoring may be useful in selected cases [76]. Further help will come in the future from the genetic assessment [77].
Hydrocephalus
The pathogenesis of the primary association between CM1 and hydrocephalus remains partially obscure. The tonsillar herniation resulting from raised ICP due to hydrocephalus is just transient and reversible (not CM1) [78], while the venous engorgement resulting from the hypoplasic posterior fossa and the occlusion of the jugular foramina can justify both CM1 (due to cerebellar edema) and hydrocephalus (due to CSF hypo-resorption) in syndromic patients [79]. In non-syndromic CM1 children, hydrocephalus would result from occlusion of the basal CSF pathways, which would be complete in a minority of patients (only 7–10% of CM1 subjects develop hydrocephalus), while it would be partial in the remaining cases (no hydrocephalus) [80,81,82].
Hydrocephalus complicates the management of CM1 and prolongs the hospital stay [83]. Because of its “obstructive” genesis, endoscopic third ventriculostomy (ETV) is regarded as the best therapeutic option, providing a high rate of success on hydrocephalus (90.5% of cases), CM1 (78.5% and 74% of clinical and radiological resolution, respectively), and syringomyelia (76% and 89%) [80]. Only 11% of patients require a treatment for persisting CM1 after ETV because of significant PF hypoplasia [84, 85]. Hydrocephalus should be treated first because more symptomatic, to reduce the risk of complications of raised ICP after PF decompression and because of the low rate of persisting CM1 symptoms after ETV. Favorable outcomes with PF decompression and successful evolution of the hydrocephalus are reported, especially in the case of ventriculomegaly (that is without raised ICP) [86].
Tethered cord
An “evident” tethered cord syndrome is sporadically associated with CM1 (up to 6–10% in selected series, < 1% in the clinical practice) [87, 88]. The spinal cord detethering improves the not related-CM1 symptoms [56]. Should typical CM1 symptoms be present too, both CM1 and tethered cord have to be surgically addressed, starting from the most symptomatic one, in separate stages [87, 89] or concurrently [90].
A relevant debate is around occult tethered cord syndrome (OTCS) and CM1. OTCS is defined as a symptomatic condition associated with normal appearance and position of conus and filum on MRI. Some studies showing a fibrous composition of an apparently normal filum or its abnormally posterior position in prone MRI, and improvement of urologic symptoms after filum sectioning, support this definition [91,92,93]. A first controversy concerns the too general criteria for OCTS definition and evolution, and the similar outcome of medical treatment and filum section on randomized studies [94]. A second controversy is on the caudal traction theory, which is advocated to explain the association among CM1, CVJ anomalies, Syr, and scoliosis (neuro-cranio-vertebral syndrome), which would be a continuum with occult tethered cord (filum disease) and which would benefit from the extradural filum section [95, 96]. The sporadic and late occurrence of CM1 in children with tethered cord [97] and the tonsillar ascent after filum section in isolated cases support this theory [89, 98, 99]. However, the scientific impact of some of these studies is poor. Moreover, there is no evidence of changed position of the tonsils after spinal cord detethering in large series [56, 100, 101]. Clinical and experimental studies are against the caudal traction theory, showing normal course of the thoraco-lumbar roots (no CM1 in experimental models of tethered cord, no tonsils movement in case of caudal spinal cord traction in cadaveric models, no correlation between conus position and presence/severity of CM1) [102]. Some anatomical findings (fusion of the filum at the level or above S1 in about one-third of cases and off the midline in 11% of cases) question the effectiveness of extradural section of the filum [103, 104]. The absence of small posterior fossa in patients with tethered cord [105] prompted some authors to the preliminary identification of a subpopulation of CM1 subjects (normal PF, low lying tonsils, associated OTCS) that could benefit from filum section [106]. To date, however, there is no evidence to consider occult tethered cord as CM1 comorbidity and to promote the filum section in CM1 [100, 107,108,109].
CVJ abnormalities
CM1 associated with CVJ anomalies configures the so-called complex CM1 [110]. This condition could be the result of a primary mesodermal development defect leading to invagination of the odontoid (basilar invagination) or an acquired process due to softening of the skull (basilar impression) or rheumatoid arthritis (cranial settling), coupled with PF hypoplasia [111, 112], or the consequences of atlanto-axial instability. The definition of the latter is not universally accepted yet [113,114,115]. The management of complex CM1 has been traditionally based on the suboccipital decompression alone (in case of mild ventral compression) or the ventral decompression (in case of significant basilar invagination) plus suboccipital decompression (if required) and occipito-cervical stabilization (in case of instability) [116,117,118]. The experience with large series shows that ventral decompression is required only in a minority of cases [119]. The knowledge of anatomy and age-related morphometric measures is mandatory in children [120]. Accordingly, some authors have proposed personal management algorithms based on anatomical landmarks (e.g., the clival-axial angle and the basion-C2 distance) [121].
Some authors have raised a debate by indicating the central atlanto-axial instability as a common precursor for CVJ anomalies, including CM1 [122, 123]. This hypothesis concerns both an evident instability and a “microinstability” (absence of radiological signs of instability but intraoperative findings at facet atlanto-axial joints pointing that). Accordingly, the posterior C1-C2 fusion has been used as a unique, standard approach for all CVJ anomalies, with reported good results [124,125,126]. However, despite the effectiveness of C1-C2 stabilization in selected cases, its results are not better than suboccipital decompression in CM1 subjects and C1-C2 fusion is not advisable in case of significant bleeding from paravertebral venous plexus, gross C1-2 rotation, or vertical C1-2 joints with unilateral C1 or C2 facet hypoplasia, maldevelopment of the lateral masses and facet joints, very young age, unfavorable course of the vertebral artery [127, 128]. According to a recent meta-analysis of the literature, there is no evidence to support the atlanto-axial instability theory and the C1-C2 surgical strategy [129].
The need to look for instability in every CM1 case is another controversial topic [100]. The misdiagnosis of basilar invagination or atlanto-axial dislocation in CM1 patients is burdened by a high risk of failed suboccipital decompression and challenging revision (fixation) surgery [130]. Therefore, a careful preoperative work-up seems to be recommended in CM1 children, where some findings, like the retroverted dens (81–84%), are very common [131, 132]. The diagnostic and therapeutic approach must be tailored to the type of abnormality and the patient’s age [133].
-
PICO 6: For children with failed CM1 surgery, is early redo surgery (≤ 12 months) more effective than late redo (> 12 months) or no surgery?
From 460 screened papers, we identified two cohort studies (Table 7).
Kennedy et al. reported a series of 156 children including 44% with associated syringomyelia, who underwent PFDO as their first surgery [134]. PFDO failed in 14 (9%) children, at a mean time of 22 months. The criteria for reoperation were “persistent, recurrent, or new CM1 symptoms” or progression of scoliosis without improvement of Syr. The tonsils descent below C2 and associated Syr were risk factors for reoperation. A more aggressive surgery, such as PFDD with or without tonsils coagulation, was performed in 11/14. In the second paper, Tubbs and coworkers reported a small series (8 children) of PFDO failures due to arachnoid veil and Magendie occlusion, and suggested posterior fossa re-exploration in case of Syr not responding to surgery [135].
Commentary
Despite the relevance of the problem, evidence on failed CM1 surgery is lacking. All together the included studies report 22 reoperated children, a too low number to draw definitive conclusions. Moreover, populations are different: Kennedy et al. reported the results of a “mininvasive” approach on mildly symptomatic children. For these children submitted to PFDO, an upgrade surgery seems enough [134].
Sacco and Scott reported a series of 16 reoperations. CM1 and CM2 were included, as well as CM1 with associated malformations. This paper, with mixed population and no data on the time and type of first surgery, still needs some comments: the authors identified younger age (< 5 years) and associated craniosynostosis as risk factors for surgical failure, and add fourth ventricle stenting as surgical option for reoperations [136].
Tubbs et al. and Sacco and Scott deal with more aggressive approaches and both indicate posterior fossa arachnoiditis as a possible cause of failure, suggesting different reoperation techniques (stenting versus adhesiolysis) [135, 136].
In conclusion, due to the low numbers, different types of surgery, and different inclusion criteria, none of the included papers was able to indicate the correct timing for CM1 postoperative follow-up, the criteria to indicate reintervention, and the type of redo surgery. A correct pathway still needs to be processed.
-
PICO 7: For children with syringomyelia without CM1, which is the most effective clinical, radiological, and surgical planning?
Syr without CM1 is a rare occurrence and recognizes disparate causes as spinal tumors, vascular malformations, tethered cord, cysts, and arachnoiditis due to previous infections, hemorrhages, and/or traumas. In all these cases, Syr is defined as secondary Syr without CM1 [137]. Once all the possible known causes are excluded, the literature defines Syr without CM1 as isolated Syr [137].
Of 376 identified references concerning Syr without CM1, 19 articles were evaluated as full papers and five were included: one RCT and four cohort studies (Fig. 2).
The RCT included 30 children with terminal Syr due to tethered cord [138], sixteen children were randomly assigned to spinal cord untethering and 14 children to untethering plus syrinx drainage. The differences for improvement rates of sensory deficits and urinary disfunction were statistically significant (p = 0.036 and p = 0.05, respectively) in favor of the combined procedure.
Lee JY et al. retrospectively reviewed a uniform group of 33 patients with preoperative syringomyelia associated with tethered cord and treated by untethering alone. After surgery, 31 of 32 patients (97%) showed long-term stability (mean follow-up 36 months) or a decrease in the syrinx measures. Only in one patient with retethering the syrinx increased and new urinary symptoms appeared. The authors concluded that untethering alone may be sufficient for the management of syringomyelia associated with tethered cord [139].
Three retrospective case series concerned isolated Syr followed for a mean time ranging between 16 and 24 months [137, 140, 141]. Magge et al. reported a good natural course in 32 children, with 91% of stabilization or improvement [137]; Joseph et al. confirmed the good outcome with no neurological deterioration neither Syr increase in all 39 cases [140]. The authors suggested defensive CSF puncture in case of pain (that was the only symptom reported), assuming as a cause a CFS focal temporary block.
Rodriguez et al. diagnosed isolated Syr in 98 children (37 with scoliosis); during the mean follow-up period of 20.5 months (1–143 months), only six out of 78 children (7.7%) showed clinical deterioration and three out of 38 (7.9%) larger syrinx (Table 8) [141].
Commentary
No eligible papers were found on syrinx secondary to spinal tumors, arachnoidal cysts, or spinal vascular malformations.
Two included papers pertain to Syr due to spinal dysraphism and they indicate the need of detethering surgery [138, 139]. The syrinx due to tethered cord has a typical low location next to the site of tethering, defined terminal Syr, and displays a progressive caudo-cranial extension [142]. Hence, the indication to extend the MRI study to the whole cord in Syr without CM1. The Erkan and coworkers’ study suggests better results if fenestration of terminal syrinx is added; the study quality is low/unclear: randomization was “simple” leading to selection and allocation bias, no blinding assessment was done, the follow-up was short, and conclusions were based on a limited sample. So the suggestion to manipulate the conus, opening the syrinx, has a too low level of evidence to be a strong recommendation [138].
Despite its frequency, we found no eligible papers about syrinx secondary to spinal tumors: there were just case reports or case series with mixed ages. The indication of these papers is to perform always a contrast-enhanced MRI in Syr without CM1, and, if a tumor is present, its removal is usually enough to obtain syrinx shrinkage [143].
Neither for vascular malformations nor cysts, we found any eligible paper; the suggestion offered by case reports is to address surgery to the malformation [144] or to the cyst [145, 146] to obtain syrinx shrinkage.
Isolated Syr is quite rare. Little data are reported about its evolution, but the natural course seems favorable even without surgical treatment, with no correlation between clinical symptoms and MRI findings [137, 140, 141].
The work by Vogel and coworkers focused on post-traumatic Syr (PTS) due to spinal cord injuries (SCI) during childhood; the authors collected a large series of 216 pediatric SCI cases with a long-term follow-up. They concluded that PTS with delayed deterioration is quite rare (3%) after pediatric SCI [147].
The role of Syr in patients with scoliosis remains an open problem: is it the cause or the consequence? The data seems to indicate that Syr is the cause of scoliosis. A scoliosis rate between 30 and 70% is reported in patients with CM1 and Syr and recently, through the analysis of a series of 825 patients with CM1 and Syr, 260 of whom with scoliosis, an association between the size of Syr and scoliosis, but not between the degree of tonsillar ectopia and scoliosis, has been demonstrated [148]. However, it is also possible that scoliosis can cause Syr since idiopathic syringes are common in scoliosis [148].
Rodriguez et al. found no statistical difference comparing radiological and clinical course in isolated Syr with and without scoliosis [141]. Furdock et al. reported the presence of Syr in 48 out of 267 (18%) spinal MRI of 305 pediatric scoliosis [149].
Taking into account scoliosis due to Syr, Yeom et al. reported a cut-off at the age of 10 years and Brockmayer et al. a curve angle inferior to 40° to obtain the regression of scoliosis without fixation when Syr is correctly treated [150, 151]. Samdani et al. underlined the impact of Syr size on the outcome after surgical correction of scoliosis and risk of worsening along fixation due to intraoperative neurophysiological monitoring failure [152].
Sha et al. reported comparable results in idiopathic and Syr-related scoliosis by thoracic fixation in 28 children and Qin and coworkers proposed selective thoracic fusion as the best choice treatment for Syr-associated scoliosis in a case–control study [153, 154]; unfortunately in both studies, details about causes of Syr and its previous neurosurgical treatments were lacking.
Conclusions
In conclusion, CM1 with or without Syr and Syr without CM1 still represent clinical challenges. As more is discovered about the natural history of untreated children and the long-term outcome of the treated ones, the management of these conditions continues to evolve.
The available evidence about the management of children with CM1 and Syr can be summarized as follows:
-
1) Asymptomatic or mildly symptomatic CM1 children without Syr generally have a benign prognosis (at least over the short intervals reported in the literature), as they may improve or remain symptomatically stable with conservative management. However, they need to maintain long-term clinical and radiological follow-up because the risk of worsening is low but not nil; about 5% of them require surgical treatment during follow-up.
-
2) Symptomatic CM1 children, which represent a low rate of CM1 children at the time of diagnosis, and CM1 patients with Syr have indications for surgery. Posterior fossa decompression surgery involves both clinical and radiological improvement with the ascent of the cerebellar tonsils and stabilization or improvement of Syr in a high percentage of children. The complication rate is very low (0 to 2.4%); from 3 to 20% of treated children require a reintervention for persistent Syr in most cases, rarely because of unchanged symptoms.
It is not clear, however, when to decide for surgery because little is known about the natural history of symptomatic CM1 children without Syr, there are no defined and generally accepted strict criteria for selecting patients for surgery, there are no validated methodologies for predicting which children will show worsening of symptoms and for deciding whether to intervene or not and the decision for suboccipital decompression can be subjective.
-
3) PFDD is associated with statistically significant longer operation time and hospitalization, and higher complication rates than PFDO. The comparison between PFDO and PFDD does not allow any further conclusion as the reported series were limited by small sample size, lack of clear and more homogeneous characterization of patients, and adequate criteria for outcomes selection and evaluation and a long-term follow-up. Large collaborative studies with proper design are necessary.
-
4) Taking into account the limitations related to missing high-level evidence studies, the present analysis allows to answer to PICO 4 as follows: (a) CM1-associated hydrocephalus can be successfully treated by ETV and should be addressed first to treat the raised ICP and select children needing PF decompression; (b) the management of craniosynostosis-related CM1 should contemplate first the treatment of the synostosis, if this is early detected. In case of late diagnosis, the best therapeutic option can be found by assessing the possible raised ICP; (c) in case of CM1 associated with an obvious tethered cord, the management of the two conditions should be separated, starting with the most symptomatic of them (tethered cord is treated by spinal cord detethering, CM1 by posterior fossa decompression). On the other hand, there is not enough evidence yet to support the (extradural) section of the filum terminale to treat symptomatic CM1 children with “occult tethered cord.”
-
5) CVJ anomalies are quite commonly associated to CM1. In case of complex CM1, the therapeutic options should be pondered according to the degree of ventral compression and the presence of instability, ranging from posterior decompression alone to posterior decompression and occipito-cervical fixation to ventral decompression and occipito-cervical fixation (with posterior decompression). Therefore, posterior decompression maintains its value in subjects without instability. There is not enough evidence yet to support the use of (occipito-) cervical fixation without obvious instability to manage pediatric CM1. The need to look for possible instability in children without evident CVJ anomalies is debated.
-
6) Complications and failures of CM1 surgery still represent a problem, but the criteria for follow-up and reintervention and the type of redo surgery are lacking.
-
7) Syr without CM1 is a rare occurrence. The few available data indicate to address first, if identified, the possible cause (dysraphism, tumor, vascular malformation, arachnoiditis); isolated Syr without CM1 seems to have an indolent course.
In summary, despite decades of experience, the management of children with CM1 and Syr remains unclear and controversial due to the lack of large, prospective, high-quality clinical trials on well-defined patient populations, and sufficient follow-up. The first prospective randomized clinical trial, organized by the Park-Reeve Syringomyelia Research Consortium, comparing PFDO and PFDD in a large group of homogeneous patients (NCT02669836), represents the first step to achieve an evidence-based consensus for surgical decision-making [155].
The Italian “Chiari-Syringomyelia Consortium,” made up of doctors (neurologists, neurosurgeons, neuroradiologists, physiatrists, neurourologists, psychologists, speech therapists, of pain), public health experts for rare diseases, and representatives of patient associations, proposed diagnostic, surgical, and rehabilitative recommendations on CM1 and Syr derived from the results of the Consortium meetings and of the “First Chiari Consensus Conference” held in Milan in 2009 [156].
The present review served at the 2019 “Chiari and Syringomyelia Consensus Conference” which was held in Milan with the aim of bringing together experts to share collaborative initiatives focusing on the adoption of shared inclusion criteria and outcome measures, as well as rigorous prospective designs, for the development of evidence-based strategies [8, 9].
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Tubbs RS, McGirt MJ, Oakes WJ (2003) Surgical experience in 130 pediatric patients with Chiari I malformations. J Neurosurg 99:291–296. https://doi.org/10.3171/jns.2003.99.2.0291
Kahn EN, Muraszko KM, Maher CO (2015) Prevalence of Chiari I malformation and syringomyelia. Neurosurg Clin N Am 26:501–507. https://doi.org/10.1016/j.nec.2015.06.006
Tubbs RS, Beckman J, Naftel RP et al (2011) Institutional experience with 500 cases of surgically treated pediatric Chiari malformation type I. J Neurosurg Pediatr 7:248–256. https://doi.org/10.3171/2010.12.PEDS10379
Saletti V, Viganò I, Melloni G et al (2019) Chiari I malformation in defined genetic syndromes in children: are there common pathways? Child’s Nerv Syst 35:1727–1739. https://doi.org/10.1007/s00381-019-04319-5
Milhorat TH (2000) Classification of syringomyelia. Neurosurg Focus 8:1–6. https://doi.org/10.3171/foc.2000.8.3.1
Blegvad C, Grotenhuis JA, Juhler M (2014) Syringomyelia: a practical, clinical concept for classification. Acta Neurochir (Wien) 156:2127–2138. https://doi.org/10.1007/s00701-014-2229-z
Klekamp J (2018) How should syringomyelia be defined and diagnosed? World Neurosurg 111:e729–e745. https://doi.org/10.1016/j.wneu.2017.12.156
Massimi L, Peretta P, Erbetta A et al (2021) Diagnosis and treatment of Chiari malformation type 1 in children: the International Consensus Document. Neurol Sci Jun 7:9. https://doi.org/10.1007/s10072-021-05317-9 (Online ahead of print)
Ciaramitaro P, Massimi L, Bertuccio A et al (2021) Diagnosis and treatment of Chiari malformation and syringomyelia in adults: international consensus document. Neurol Sci Jun 15:3. https://doi.org/10.1007/s10072-021-05347-3 (Online ahead of print)
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
CASP Checklist. https://casp-uk.b-cdn.net/wp-content/uploads/2018/03/CASP-Cohort-Study-Checklist-2018_fillable_form.pdf
Higgins J, Savović J, Page M et al (2017) Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins J, Churchill R, Chandler J, Cumpston M (eds) Cochrane handbook for systematic reviews of interventions version 5.2 (updated June 2017). Cohrane, London
Pomeraniec IJ, Ksendzovsky A, Awad AJ et al (2016) Natural and surgical history of Chiari malformation Type I in the pediatric population. J Neurosurg Pediatr 17:343–352. https://doi.org/10.3171/2015.7.PEDS1594
Novegno F, Caldarelli M, Massa A et al (2008) The natural history of the Chiari Type I anomaly. J Neurosurg Pediatr 2:179–187. https://doi.org/10.3171/PED/2008/2/9/179
Aitken LA, Lindan CE, Sidney S et al (2009) Chiari Type I malformation in a pediatric population. Pediatr Neurol 40:449–454. https://doi.org/10.1016/j.pediatrneurol.2009.01.003
Benglis D, Covington D, Bhatia R et al (2011) Outcomes in pediatric patients with Chiari malformation Type I followed up without surgery: clinical article. J Neurosurg Pediatr 7:375–379. https://doi.org/10.3171/2011.1.PEDS10341
Strahle J, Muraszko KM, Kapurch J et al (2011) Natural history of Chiari malformation Type I following decision for conservative treatment: clinical article. J Neurosurg Pediatr 8:214–221. https://doi.org/10.3171/2011.5.PEDS1122
Massimi L, Caldarelli M, Frassanito P, Di Rocco C (2011) Natural history of Chiari type I malformation in children. Neurol Sci 32(Suppl 3):275–277. https://doi.org/10.1007/s10072-011-0684-3
Killeen A, Roguski M, Chavez A et al (2015) Non-operative outcomes in Chiari i malformation patients. J Clin Neurosci 22:133–138. https://doi.org/10.1016/j.jocn.2014.06.008
Whitson WJ, Lane JR, Bauer DF, Durham SR (2015) A prospective natural history study of nonoperatively managed Chiari I malformation: does follow-up MRI surveillance alter surgical decision making? J Neurosurg Pediatr 16:159–166. https://doi.org/10.3171/2014.12.PEDS14301
Leon TJ, Kuhn EN, Arynchyna AA et al (2019) Patients with “benign” Chiari I malformations require surgical decompression at a low rate. J Neurosurg Pediatr 23:498–506. https://doi.org/10.3171/2018.10.PEDS18407
Anderson RCE, Emerson RG, Dowling KC, Feldstein NA (2003) Improvement in brainstem auditory evoked potentials after suboccipital decompression in patients with Chiari I malformations. J Neurosurg 98:459–464. https://doi.org/10.3171/jns.2003.98.3.0459
Knerlich-Lukoschus F, Jünger S, Messing-Jünger M (2019) Management: opinions from different centers-the Sankt Augustin experience. Childs Nerv Syst 35:1885–1888. https://doi.org/10.1007/s00381-019-04183-3
Chatrath A, Marino A, Taylor D et al (2019) Chiari I malformation in children-the natural history. Childs Nerv Syst 35:1793–1799. https://doi.org/10.1007/s00381-019-04310-0
Marianayagam NJ, Ben SN, Zarchi O et al (2020) Conservative management for pediatric patients with Chiari 1 anomaly: a retrospective study. Clin Neurol Neurosurg 189:105615. https://doi.org/10.1016/j.clineuro.2019.105615
Davidson L, Phan TN, Myseros JS et al (2021) Long-term outcomes for children with an incidentally discovered Chiari malformation type 1: what is the clinical significance? Childs Nerv Syst 37:1191–1197. https://doi.org/10.1007/s00381-020-04980-1
Carey M, Fuell W, Harkey T, Albert GW (2021) Natural history of Chiari I malformation in children: a retrospective analysis. Childs Nerv Syst 37:1185–1190. https://doi.org/10.1007/s00381-020-04913-y
Jiang E, Sha S, Yuan XX et al (2018) Comparison of clinical and radiographic outcomes for posterior fossa decompression with and without duraplasty for treatment of pediatric Chiari I malformation: a prospective study. World Neurosurg 110:e465–e472. https://doi.org/10.1016/j.wneu.2017.11.007
Navarro R, Olavarria G, Seshadri R et al (2004) Surgical results of posterior fossa decompression for patients with Chiari I malformation. Child’s Nerv Syst 20:349–356. https://doi.org/10.1007/s00381-003-0883-1
Yeh DD, Koch B, Crone KR (2006) Intraoperative ultrasonography used to determine the extent of surgery necessary during posterior fossa decompression in children with Chiari malformation type I. J Neurosurg 105:26–32. https://doi.org/10.3171/jns.2006.105.1.26
Galarza M, Sood S, Ham S (2007) Relevance of surgical strategies for the management of pediatric Chiari type I malformation. Child’s Nerv Syst 23:691–696. https://doi.org/10.1007/s00381-007-0297-6
McGirt MJ, Attenello FJ, Datoo G et al (2008) Intraoperative ultrasonography as a guide to patient selection for duraplasty after suboccipital decompression in children with Chiari malformation Type I. J Neurosurg Pediatr 2:52–57. https://doi.org/10.3171/PED/2008/2/7/052
Shamji MF, Ventureyra ECG, Baronia B et al (2010) Classification of symptomatic Chiari I malformation to guide surgical strategy. Can J Neurol Sci 37:482–487. https://doi.org/10.1017/S0317167100010507
Ventureyra ECG, Aziz HA, Vassilyadi M (2003) The role of cine flow MRI in children with Chiari I malformation. Child’s Nerv Syst 19:109–113. https://doi.org/10.1007/s00381-002-0701-1
Litvack ZN, Lindsay RA, Selden NR (2013) Dura splitting decompression for Chiari I malformation in pediatric patients: Clinical outcomes, healthcare costs, and resource utilization. Neurosurgery 72:922–928. https://doi.org/10.1227/NEU.0b013e31828ca1ed
Limonadi FM, Selden NR (2004) Dura-splitting decompression of the craniocervical junction: reduced operative time, hospital stay, and cost with equivalent early outcome. J Neurosurg 101:184–188. https://doi.org/10.3171/ped.2004.101.2.0184
Chotai S, Medhkour A (2014) Surgical outcomes after posterior fossa decompression with and without duraplasty in Chiari malformation-I. Clin Neurol Neurosurg 125:182–188. https://doi.org/10.1016/j.clineuro.2014.07.027
Lee A, Yarbrough CK, Greenberg JK et al (2014) Comparison of posterior fossa decompression with or without duraplasty in children with Type I Chiari malformation. Child’s Nerv Syst 30:1419–1424. https://doi.org/10.1007/s00381-014-2424-5
Lee S, Wang KC, Cheon JE et al (2014) Surgical outcome of Chiari I malformation in children: clinico-radiological factors and technical aspects. Child’s Nerv Syst 30:613–623. https://doi.org/10.1007/s00381-013-2263-9
Narenthiran G, Parks C, Pettorini B (2015) Management of Chiari I malformation in children: effectiveness of intra-operative ultrasound for tailoring foramen magnum decompression. Child’s Nerv Syst 31:1371–1376. https://doi.org/10.1007/s00381-015-2699-1
Pomeraniec IJ, Ksendzovsky A, Yu PL, Jane JA (2015) Surgical history of sleep apnea in pediatric patients with Chiari type 1 malformation. Neurosurg Clin N Am 26:543–553. https://doi.org/10.1016/j.nec.2015.06.009
Shweikeh F, Sunjaya D, Nuno M et al (2015) National trends, complications, and hospital charges in pediatric patients with Chiari malformation type I treated with posterior fossa decompression with and without duraplasty. Pediatr Neurosurg 50:31–37. https://doi.org/10.1159/000371659
Gallo P, Sokol D, Kaliaperumal C, Kandasamy J (2017) Comparison of three different cranio-cervical decompression procedures in children with Chiari malformation Type I: does the surgical technique matter? Pediatr Neurosurg 52:289–297. https://doi.org/10.1159/000479327
Pisapia JM, Merkow MB, Brewington D et al (2017) External validity of the Chiari severity index and outcomes among pediatric Chiari I patients treated with intra- or extra-dural decompression. Child’s Nerv Syst 33:313–320. https://doi.org/10.1007/s00381-016-3300-2
Raza-Knight S, Mankad K, Prabhakar P, Thompson D (2017) Headache outcomes in children undergoing foramen magnum decompression for Chiari I malformation. Arch Dis Child 102:238–243. https://doi.org/10.1136/archdischild-2016-310662
Grahovac G, Pundy T, Tomita T (2018) Chiari type I malformation of infants and toddlers. Child’s Nerv Syst 34:1169–1176. https://doi.org/10.1007/s00381-017-3712-7
Entezami P, Gooch MR, Poggi J et al (2019) Current management of pediatric chiari type 1 malformations. Clin Neurol Neurosurg 176:122–126. https://doi.org/10.1016/j.clineuro.2018.12.007
Gernsback J, Tomita T (2019) Management of Chiari I malformation in children: personal opinions. Child’s Nerv Syst 35:1921–1923. https://doi.org/10.1007/s00381-019-04180-6
Walker-Palmer TK, Cochrane DD, Singhal A, Steinbok P (2019) Outcomes and complications for individual neurosurgeons for the treatment of Chiari I malformation at a children’s hospital. Child’s Nerv Syst 35:1895–1904. https://doi.org/10.1007/s00381-019-04201-4
Durham SR, Fjeld-Olenec K (2008) Comparison of posterior fossa decompression with and without duraplasty for the surgical treatment of Chiari malformation Type I in pediatric patients: a meta-analysis. J Neurosurg Pediatr 2:42–49. https://doi.org/10.3171/PED/2008/2/7/042
Lu VM, Phan K, Crowley SP, Daniels DJ (2017) The addition of duraplasty to posterior fossa decompression in the surgical treatment of pediatric Chiari malformation Type I: a systematic review and meta-analysis of surgical and performance outcomes. J Neurosurg Pediatr 20:439–449. https://doi.org/10.3171/2017.6.PEDS16367
Addo NK, Javadpour S, Kandasamy J et al (2013) Central sleep apnea and associated chiari malformation in children with syndromic craniosynostosis: treatment and outcome data from a supraregional national craniofacial center. J Neurosurg Pediatr 11:296–301. https://doi.org/10.3171/2012.11.PEDS12297
Karppinen A, Koljonen V, Valanne L, Leikola J (2012) Asymmetric laterality of Chiari type i malformation in patients with non-syndromic single-suture craniosynostosis. Acta Neurochir (Wien) 154:2103–2107. https://doi.org/10.1007/s00701-012-1470-6
Scott WW, Fearon JA, Swift DM, Sacco DJ (2013) Suboccipital decompression during posterior cranial vault remodeling for selected cases of Chiari malformations associated with craniosynostosis: clinical article. J Neurosurg Pediatr 12:166–170. https://doi.org/10.3171/2013.4.PEDS12463
Strahle J, Muraszko KM, Buchman SR et al (2011) Chiari malformation associated with craniosynostosis. Neurosurg Focus 31:3–10. https://doi.org/10.3171/2011.6.FOCUS11107
Glenn C, Cheema AA, Safavi-Abbasi S et al (2015) Spinal cord detethering in children with tethered cord syndrome and Chiari type 1 malformations. J Clin Neurosci 22:1749–1752. https://doi.org/10.1016/j.jocn.2015.05.023
Balestrino A, Consales A, Pavanello M et al (2019) Management: opinions from different centers—the Istituto Giannina Gaslini experience. Child’s Nerv Syst 35:1905–1909. https://doi.org/10.1007/s00381-019-04162-8
Grabb PA, Mapstone TB, Oakes WJ (1999) Ventral brain stem compression in pediatric and young adult patients with Chiari I malformations. Neurosurgery 44:520–528. https://doi.org/10.1097/00006123-199903000-00050
Kim LJ, Rekate HL, Klopfenstein JD, Sonntag VKH (2004) Treatment of basilar invagination associated with Chiari I malformations in the pediatric population: cervical reduction and posterior occipitocervical fusion. J Neurosurg 101:189–195. https://doi.org/10.3171/ped.2004.101.2.0189
Bollo RJ, Riva-Cambrin J, Brockmeyer MM, Brockmeyer DL (2012) Complex Chiari malformations in children: an analysis of preoperative risk factors for occipitocervical fusion: clinical article. J Neurosurg Pediatr 10:134–141. https://doi.org/10.3171/2012.3.PEDS11340
Goel A, Gore S, Shah A et al (2018) Atlantoaxial fixation for Chiari 1 formation in pediatric age-group patients: report of treatment in 33 patients. World Neurosurg 111:e668–e677. https://doi.org/10.1016/j.wneu.2017.12.137
Rijken BFM, Lequin MH, Van Der Lijn F et al (2015) The role of the posterior fossa in developing Chiari I malformation in children with craniosynostosis syndromes. J Cranio-Maxillofacial Surg 43:813–819. https://doi.org/10.1016/j.jcms.2015.04.001
Calandrelli R, D’Apolito G, Panfili M et al (2016) Role of “major” and “minor” lambdoid arch sutures in posterior cranial fossa changes: mechanism of cerebellar tonsillar herniation in infants with multisutural craniosynostosis. Child’s Nerv Syst 32:451–459. https://doi.org/10.1007/s00381-015-2956-3
Rijken BFM, Lequin MH, Van Veelen MLC et al (2015) The formation of the foramen magnum and its role in developing ventriculomegaly and Chiari i malformation in children with craniosynostosis syndromes. J Cranio-Maxillofacial Surg 43:1042–1048. https://doi.org/10.1016/j.jcms.2015.04.025
Chivoret N, Arnaud E, Giraudat K et al (2018) Bilambdoid and sagittal synostosis: report of 39 cases. Surg Neurol Int 9:206. https://doi.org/10.4103/sni.sni_454_17
Davis AA, Zuccoli G, Haredy MM et al (2019) The incidence of Chiari malformations in patients with isolated sagittal synostosis. Plast Reconstr Surg - Glob Open 7:1–5. https://doi.org/10.1097/GOX.0000000000002090
Fearon JA, Dimas V, Ditthakasem K (2016) Lambdoid craniosynostosis: the relationship with Chiari deformations and an analysis of surgical outcomes. Plast Reconstr Surg 137:946–951. https://doi.org/10.1097/01.prs.0000480014.18541.d8
Ranganathan K, Rampazzo A, Hashmi A et al (2018) The role of preoperative imaging in the management of nonsyndromic lambdoid craniosynostosis. J Craniofac Surg 29:36–39. https://doi.org/10.1097/SCS.0000000000004026
Lin LO, Zhang RS, Hoppe IC et al (2019) Onset and resolution of Chiari malformations and hydrocephalus in syndromic craniosynostosis following posterior vault distraction. Plast Reconstr Surg 144:932–940. https://doi.org/10.1097/PRS.0000000000006041
Afshari FT, Solanki GA, Lo WB, Rodrigues D (2020) Posterior calvarial augmentation for Chiari malformation type 1 refractory to foramen magnum decompression. World Neurosurg 139:70–74. https://doi.org/10.1016/j.wneu.2020.03.218
McMillan K, Lloyd M, Evans M et al (2017) Experiences in performing posterior calvarial distraction. J Craniofac Surg 28:664–669. https://doi.org/10.1097/SCS.0000000000003458
Iyengar RJ, Klinge PM, Chen WS et al (2016) Management of craniosynostosis at an advanced age: controversies, clinical findings, and surgical treatment. J Craniofac Surg 27:e435–e441. https://doi.org/10.1097/SCS.0000000000002725
Winston KR, Stence NV, Boylan AJ, Beauchamp KM (2015) Upward translation of cerebellar tonsils following surgical expansion of supratentorial cranial vault: a unified biomechanical explanation of Chiari Type I. Pediatr Neurosurg 50:243–249. https://doi.org/10.1159/000437146
Valentini LG, Saletti V, Erbetta A et al (2019) Chiari 1 malformation and untreated sagittal synostosis: a new subset of complex Chiari? Child’s Nerv Syst 35:1741–1753. https://doi.org/10.1007/s00381-019-04283-0
Leikola J, Hukki A, Karppinen A et al (2012) The evolution of cerebellar tonsillar herniation after cranial vault remodeling surgery. Child’s Nerv Syst 28:1767–1771. https://doi.org/10.1007/s00381-012-1816-7
Piper RJ, Magdum SA (2019) Chiari 1 malformation and raised intracranial pressure. Child’s Nerv Syst 35:1719–1725. https://doi.org/10.1007/s00381-019-04232-x
Glass GE, O’Hara J, Canham N et al (2019) ERF-related craniosynostosis: the phenotypic and developmental profile of a new craniosynostosis syndrome. Am J Med Genet A 179:615–627. https://doi.org/10.1002/ajmg.a.61073
Di Rocco C (2019) Should we stop using the term “malformation” for Chiari type I? Child’s Nerv. Syst 35:1649–1650. https://doi.org/10.1007/s00381-019-04311-z
Di Rocco C, Frassanito P, Massimi L, Peraio S (2011) Hydrocephalus and Chiari type I malformation. Child’s Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 27:1653–1664. https://doi.org/10.1007/s00381-011-1545-3
Massimi L, Pennisi G, Frassanito P et al (2019) Chiari type I and hydrocephalus. Child’s Nerv Syst 35:1701–1709. https://doi.org/10.1007/s00381-019-04245-6
Sadique SI, Pandey P, Chaudhuri AK (2020) Cerebrospinal fluid flowmetry in pediatric patients with Chiari malformation I with surgical implications. World Neurosurg 135:e83–e86. https://doi.org/10.1016/j.wneu.2019.10.184
Seaman SC, Dawson JD, Magnotta V et al (2020) Fourth ventricle enlargement in Chiari malformation Type I. World Neurosurg 133:e259–e266. https://doi.org/10.1016/j.wneu.2019.08.230
Elsamadicy AA, Koo AB, David WB et al (2021) Pre-operative headaches and obstructive hydrocephalus predict an extended length of stay following suboccipital decompression for pediatric Chiari I malformation. Child’s Nerv Syst 37:91–99. https://doi.org/10.1007/s00381-020-04688-2
Massimi L, Pravatà E, Tamburrini G et al (2011) Endoscopic third ventriculostomy for the management of Chiari I and related hydrocephalus: outcome and pathogenetic implications. Neurosurgery 68:950–956. https://doi.org/10.1227/NEU.0b013e318208f1f3
Hayhurst C, Osman-Farah J, Das K, Mallucci C (2008) Initial management of hydrocephalus associated with Chiari malformation Type I-syringomyelia complex via endoscopic third ventriculostomy: an outcome analysis. J Neurosurg 108:1211–1214. https://doi.org/10.3171/JNS/2008/108/6/1211
Deng X, Wu L, Yang C et al (2013) Surgical treatment of chiari I malformation with ventricular dilation. Neurol Med Chir (Tokyo) 53:847–852. https://doi.org/10.2176/nmc.oa2012-0206
Valentini LG, Selvaggio G, Erbetta A et al (2013) Occult spinal dysraphism: lessons learned by retrospective analysis of 149 surgical cases about natural history, surgical indications, urodynamic testing, and intraoperative neurophysiological monitoring. Child’s Nerv Syst 29:1657–1669. https://doi.org/10.1007/s00381-013-2186-5
Kashlan ON, Wilkinson DA, Morgenstern H et al (2019) Predictors of surgical treatment in children with tethered fibrofatty filum terminale. J Neurosurg Pediatr 1:1–8. https://doi.org/10.3171/2019.8.PEDS19292
Zhou Y, Zhu L, Lin Y, Cheng H (2017) Chiari type i malformation with occult tethered cord syndrome in a child: a case report. Med (United States) 96:13–15. https://doi.org/10.1097/MD.0000000000008239
Gluncic V, Turner M, Burrowes D, Frim D (2011) Concurrent Chiari decompression and spinal cord untethering in children: feasibility in a small case series. Acta Neurochir (Wien) 153:109–114. https://doi.org/10.1007/s00701-010-0811-6
Selçuki M, Vatansever S, Inan S et al (2003) Is a filum terminale with a normal appearance really normal? Child’s Nerv Syst 19:3–10. https://doi.org/10.1007/s00381-002-0665-1
Selden NR, Nixon RR, Skoog SR, Lashley DB (2006) Minimal tethered cord syndrome associated with thickening of the terminal filum. J Neurosurg 105:214–218. https://doi.org/10.3171/ped.2006.105.3.214
Steinbok P, Kariyattil R, MacNeily AE (2007) Comparison of section of filum terminale and non-neurosurgical management for urinary incontinence in patients with normal conus position and possible occult tethered cord syndrome. Neurosurgery 61:550–556. https://doi.org/10.1227/01.NEU.0000290902.07943.E6
Steinbok P, MacNeily AE, Hengel AR et al (2016) Filum section for urinary incontinence in children with occult tethered cord syndrome: a randomized, controlled pilot study. J Urol 195:1183–1188. https://doi.org/10.1016/j.juro.2015.09.082
Royo-Salvador MB, Solé-Llenas J, Doménech JM, González-Adrio R (2005) Results of the section of the filum terminale in 20 patients with syringomyelia, scoliosis and Chiari malformation. Acta Neurochir (Wien) 147:515–523. https://doi.org/10.1007/s00701-005-0482-y
Royo-Salvador MB, Fiallos-Rivera MV, Salca HC, Ollé-Fortuny G (2020) The Filum disease and the Neuro-Cranio-vertebral syndrome: definition, clinical picture and imaging features. BMC Neurol 20:1–16. https://doi.org/10.1186/s12883-020-01743-y
Abel TJ, Chowdhary A, Gabikian P et al (2006) Acquired Chiari malformation Type I associated with a fatty terminal filum: case report. J Neurosurg 105:329–332. https://doi.org/10.3171/ped.2006.105.4.329
Kapoor A, Dhandapani S, Singh P (2014) The triad of holocord syringomyelia, Chiari malformation and tethered cord: amelioration with simple detethering–a case for revisiting traction hypothesis? Neurol India 62:708–709
Sgouros S (2011) Acquired Chiari I malformation in a child with corrected diastematomyelia disappeared after thickened filum division. Pediatr Neurosurg 46:402–405. https://doi.org/10.1159/000323423
Canheu AC, Santos MV, Furlanetti LL et al (2020) The Brazilian Society for Pediatric Neurosurgery: consensus on Chiari I deformity. Child’s Nerv Syst 36:17–18. https://doi.org/10.1007/s00381-019-04413-8
Valentini LG, Selvaggio G, Visintini S et al (2011) Tethered cord: natural history, surgical outcome and risk for Chiari malformation 1 (CM1). Neurol Sci 32:353–356. https://doi.org/10.1007/s10072-011-0745-7
Massimi L, Peraio S, Peppucci E et al (2011) Section of the filum terminale: is it worthwhile in Chiari type I malformation? Neurol Sci 32(Suppl 3):S349–S351. https://doi.org/10.1007/s10072-011-0691-4
Pinto FCG, de Fontes RBV, de Leonhardt MC et al (2002) Anatomic study of the filum terminale and its correlations with the tethered cord syndrome. Neurosurgery 51:30–725
Hansasuta A, Tubbs RS, Oakes WJ (1999) Filum terminale fusion and dural sac termination: study in 27 cadavers. Pediatr Neurosurg 30:176–179. https://doi.org/10.1159/000028790
Tubbs RS, Bui CJ, Rice WC et al (2007) Critical analysis of the Chiari malformation Type I found in children with lipomyelomeningocele. J Neurosurg 106:196–200. https://doi.org/10.3171/ped.2007.106.3.196
Milhorat TH, Bolognese PA, Nishikawa M et al (2009) Association of Chiari malformation type I and tethered cord syndrome: preliminary results of sectioning filum terminale. Surg Neurol 72:20–35. https://doi.org/10.1016/j.surneu.2009.03.008
Bolognese PA, Brodbelt A, Bloom AB, Kula RW (2019) Chiari I malformation: opinions on diagnostic trends and controversies from a panel of 63 international experts. World Neurosurg 130:e9–e16. https://doi.org/10.1016/j.wneu.2019.05.098
Milano JB, Barcelos ACES, Onishi FJ et al (2020) The effect of filum terminale sectioning for Chiari 1 malformation treatment: systematic review. Neurol Sci 41:249–256. https://doi.org/10.1007/s10072-019-04056-2
Epstein NE (2018) A review of the disagreements in the prevalence and treatment of the tethered cord syndromes with chiari-1 malformations. Surg Neurol Int 9:161. https://doi.org/10.4103/sni.sni_230_18
Brockmeyer DL, Spader HS (2015) Complex Chiari malformations in children. Diagnosis and management. Neurosurg Clin N Am 26:555–560. https://doi.org/10.1016/j.nec.2015.06.002
Diniz JM, Botelho RV (2020) The role of clivus length and cranial base flexion angle in basilar invagination and Chiari malformation pathophysiology. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol 41:1751–1757. https://doi.org/10.1007/s10072-020-04248-1
Shane Tubbs R, Griessenauer CJ, Hendrix P et al (2015) Relationship between pharyngitis and peri-odontoid pannus: a new etiology for some Chiari i malformations? Clin Anat 28:602–607. https://doi.org/10.1002/ca.22563
Lacy J, Bajaj J, Gillis CC (2020) Atlantoaxial instability. In: StatPearls [Internet]. Treasure Island: StatPearls Publishing; 2021 Jan
Passias PG, Wang S, Kozanek M et al (2013) Relationship between the alignment of the occipitoaxial and subaxial cervical spine in patients with congenital atlantoxial dislocations. J Spinal Disord Tech 26:15–21. https://doi.org/10.1097/BSD.0b013e31823097f9
Rojas CA, Bertozzi JC, Martinez CR, Whitlow J (2007) Reassessment of the craniocervical junction: normal values on CT. Am J Neuroradiol 28:1819–1823. https://doi.org/10.3174/ajnr.A0660
Klekamp J (2015) Chiari I malformation with and without basilar invagination: a comparative study. Neurosurg Focus 38:E12. https://doi.org/10.3171/2015.1.FOCUS14783
Alalade AF, Ogando-Rivas E, Forbes J et al (2019) A dual approach for the management of complex craniovertebral junction abnormalities: endoscopic endonasal odontoidectomy and posterior decompression with fusion. World Neurosurg X 2:100010. https://doi.org/10.1016/j.wnsx.2019.100010
Liao C, Visocchi M, Zhang W et al (2019) The relationship between basilar invagination and Chiari malformation Type I: a narrative review. Acta Neurochir Suppl 125:111–118. https://doi.org/10.1007/978-3-319-62515-7_16
Chatterjee S, Shivhare P, Verma SG (2019) Chiari malformation and atlantoaxial instability: problems of co-existence. Child’s Nerv Syst 35:1755–1761. https://doi.org/10.1007/s00381-019-04284-z
Bapuraj JR, Bruzek AK, Tarpeh JK et al (2019) Morphometric changes at the craniocervical junction during childhood. J Neurosurg Pediatr 24:227–235. https://doi.org/10.3171/2019.4.PEDS1968
Ho WSC, Brockmeyer DL (2019) Complex Chiari malformation: using craniovertebral junction metrics to guide treatment. Child’s Nerv Syst 35:1847–1851. https://doi.org/10.1007/s00381-019-04214-z
Goel A, Sathe P, Shah A (2017) Atlantoaxial fixation for basilar invagination without obvious atlantoaxial instability (Group B basilar invagination): outcome analysis of 63 surgically treated cases. World Neurosurg 99:164–170. https://doi.org/10.1016/j.wneu.2016.11.093
Goel A (2019) A review of a new clinical entity of “central atlantoaxial instability”: expanding horizons of craniovertebral junction surgery. Neurospine 16:186–194. https://doi.org/10.14245/ns.1938138.069
Goel A (2015) Is atlantoaxial instability the cause of Chiari malformation? Outcome analysis of 65 patients treated by atlantoaxial fixation. J Neurosurg Spine 22:116–127. https://doi.org/10.3171/2014.10.SPINE14176
Goel A, Kaswa A, Shah A (2019) Atlantoaxial fixation for treatment of Chiari formation and syringomyelia with no craniovertebral bone anomaly: report of an experience with 57 cases. Acta Neurochir Suppl 125:101–110. https://doi.org/10.1007/978-3-319-62515-7_15
Goel A, Vutha R, Shah A et al (2019) Spinal kyphoscoliosis associated with Chiari formation and syringomyelia “recovery” following atlantoaxial fixation: a preliminary report and early results based on experience with 11 surgically treated cases. World Neurosurg 125:e937–e946. https://doi.org/10.1016/j.wneu.2019.01.212
Deora H, Behari S, Sardhara J et al (2019) Is cervical stabilization for all ccases of Chiari-I malformation an overkill? Evidence speaks louder than words! Neurospine 16:195–206. https://doi.org/10.14245/ns.1938192.096
Salunke P, Karthigeyan M, Malik P, Panchal C (2020) Changing perception but unaltered reality: how effective is C1–C2 fixation for Chiari malformations without instability? World Neurosurg 136:e234–e244. https://doi.org/10.1016/j.wneu.2019.12.122
Wagner A, Grassner L, Kögl N et al (2020) Chiari malformation type I and basilar invagination originating from atlantoaxial instability: a literature review and critical analysis. Acta Neurochir (Wien) 162:1553–1563. https://doi.org/10.1007/s00701-020-04429-z
Du Y-Q, Qiao G-Y, Yin Y-H et al (2020) Posterior atlantoaxial facet joint reduction, fixation and fusion as revision surgery for failed suboccipital decompression in patients with basilar invagination and atlantoaxial dislocation: operative nuances, challenges and outcomes. Clin Neurol Neurosurg 194:105793. https://doi.org/10.1016/j.clineuro.2020.105793
Ishak B, Dhaliwal G, Rengifo R et al (2020) The retroverted dens: a review of its anatomy, terminology, and clinical significance. World Neurosurg 137:304–309. https://doi.org/10.1016/j.wneu.2020.01.231
Ladner TR, Dewan MC, Day MA et al (2015) Posterior odontoid process angulation in pediatric Chiari I malformation: an MRI morphometric external validation study. J Neurosurg Pediatr 16:138–145. https://doi.org/10.3171/2015.1.PEDS14475
Menezes AH, Dlouhy BJ (2020) Atlas assimilation: spectrum of associated radiographic abnormalities, clinical presentation, and management in children below 10 years. Child’s Nerv Syst 36:975–985. https://doi.org/10.1007/s00381-019-04488-3
Kennedy BC, Nelp TB, Kelly KM et al (2015) Delayed resolution of syrinx after posterior fossa decompression without dural opening in children with Chiari malformation Type I. J Neurosurg Pediatr 16:599–606. https://doi.org/10.3171/2015.4.PEDS1572
Tubbs RS, Webb DB, Oakes WJ (2004) Persistent syringomyelia following pediatric Chiari I decompression: Radiological and surgical findings. J Neurosurg 100:460–464. https://doi.org/10.3171/ped.2004.100.5.0460
Sacco D, Scott RM (2003) Reoperation for Chiari malformations. Pediatr Neurosurg 39:171–178. https://doi.org/10.1159/000072467
Magge SN, Smyth MD, Governale LS et al (2011) Idiopathic syrinx in the pediatric population: a combined center experience - clinical article. J Neurosurg Pediatr 7:30–36. https://doi.org/10.3171/2010.10.PEDS1057
Erkan K, Unal F, Kiris T, Karalar T (2000) Treatment of terminal syringomyelia in association with tethered cord syndrome: clinical outcomes with and without syrinx drainage. Neurosurg Focus 8:1–6. https://doi.org/10.3171/foc.2000.8.3.9
Lee JY, Phi JH, Cheon JE et al (2012) Preuntethering and postuntethering courses of syringomyelia associated with tethered spinal cord. Neurosurgery 71:23–29. https://doi.org/10.1227/NEU.0b013e31824cebc6
Joseph RN, Batty R, Raghavan A et al (2013) Management of isolated syringomyelia in the paediatric population-a review of imaging and follow-up in a single centre. Br J Neurosurg 27:683–686. https://doi.org/10.3109/02688697.2013.771728
Rodriguez A, Kuhn EN, Somasundaram A, Couture DE (2015) Management of idiopathic pediatric syringohydromyelia. J Neurosurg Pediatr 16:452–457. https://doi.org/10.3171/2015.3.PEDS14433
Thuy M, Chaseling R, Fowler A (2015) Spinal cord detethering procedures in children: a 5 year retrospective cohort study of the early post-operative course. J Clin Neurosci 22:838–842. https://doi.org/10.1016/j.jocn.2014.11.019
She DJ, Lu YP, Xiong J et al (2019) MR imaging features of spinal pilocytic astrocytoma. BMC Med Imaging 19:1–8. https://doi.org/10.1186/s12880-018-0296-y
Srivatanakul K, Songsaeng D, Ozanne A et al (2009) Spinal arteriovenous malformation associated with syringomyelia: report of 4 cases. J Neurosurg Spine 10:436–442. https://doi.org/10.3171/2009.2.SPINE08172
Shenoy SN, Raja A (2004) Spinal neurenteric cyst: report of 4 cases and review of the literature. Pediatr Neurosurg 40:284–292. https://doi.org/10.1159/000083741
Wang MY, Levi ADO, Green BA (2003) Intradural spinal arachnoid cysts in adults. Surg Neurol 60:49–55. https://doi.org/10.1016/S0090-3019(03)00149-6
Vogel LC, Krajci KA, Anderson CJ (2002) Adults with pediatric-onset spinal cord injury: part 2: musculoskeletal and neurological complications. J Spinal Cord Med 25:117–123. https://doi.org/10.1080/10790268.2002.11753611
Strahle J, Taiwo R, Averill C et al (2019) Radiological and clinical associations with scoliosis outcomes after posterior fossa decompression in patients with Chiari malformation and syrinx from the Park-Reeves Syringomyelia Research Consortium. J Neurosurg Pediatr 10:1–7. https://doi.org/10.3171/2020.1.PEDS18755
Furdock R, Brouillet K, Luhmann SJ (2019) Organ system anomalies associated with congenital scoliosis: a retrospective study of 305 patients. J Pediatr Orthop 39:E190–E194. https://doi.org/10.1097/BPO.0000000000001279
Yeom JS, Lee CK, Park KW et al (2007) Scoliosis associated with syringomyelia: analysis of MRI and curve progression. Eur Spine J 16:1629–1635. https://doi.org/10.1007/s00586-007-0472-1
Brockmeyer D, Gollogly S, Smith JT (2003) Scoliosis associated with Chiari 1 malformations: the effect of suboccipital decompression on scoliosis curve progression: a preliminary study. Spine 28:2505–2509. https://doi.org/10.1097/01.BRS.0000092381.05229.87
Samdani AF, Hwang SW, Singla A et al (2017) Outcomes of patients with syringomyelia undergoing spine deformity surgery: do large syrinxes behave differently from small? Spine J 17:1406–1411. https://doi.org/10.1016/j.spinee.2017.04.006
Sha S, Qiu Y, Sun W et al (2016) Does surgical correction of right thoracic scoliosis in syringomyelia produce outcomes similar to those in adolescent idiopathic scoliosis? J Bone Jt Surg - Am 98:295–302. https://doi.org/10.2106/JBJS.O.00428
Qin X, Sun W, Xu L et al (2016) Effectiveness of selective thoracic fusion in the surgical treatment of syringomyelia-associated scoliosis. Spine 41:E887–E892. https://doi.org/10.1097/BRS.0000000000001452
Hale AT, Adelson PD, Albert GW et al (2020) Factors associated with syrinx size in pediatric patients treated for Chiari malformation type I and syringomyelia: a study from the Park-Reeves Syringomyelia Research Consortium. J Neurosurg Pediatr 6:1–11. https://doi.org/10.3171/2020.1.PEDS19493
Ciaramitaro P, Garbossa D, Peretta P, Interregional Chiari and Syringomyelia Consortium, on behalf of the Interregional Chiari and Syringomyelia Consortium et al (2020) Syringomyelia and Chiari Syndrome Registry: advances in epidemiology, clinical phenotypes and natural history based on a North Western Italy cohort. Ann Ist Super Sanita 56(1):48–58. https://doi.org/10.4415/ANN_20_01_08
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. The bibliographic research and data analysis were performed by Mariangela Farinotti, Saba Motta, Alessandra Solari, and Laura Grazia Valentini. The first draft of the manuscript was written by Veronica Saletti and Mariangela Farinotti; all authors made substantial contributions to the writing of the article and reviewed it critically for intellectual content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Laura Grazia Valentini and Veronica Saletti are members of the European Reference Network for rare and/or complex craniofacial anomalies and ear, nose and throat (ENT) disorders (ERN CRANIO).
Appendices
Appendix 1
Appendix 2: Search strategies for Medline (PubMed)
((("Arnold-Chiari Malformation"[Mesh] OR "Chiari malformation"[Title/Abstract] OR "arnold-chiari"[Title/Abstract] OR "arnold-chiari malformation"[Title/Abstract] OR "chiari type 1.5 malformation"[Title/Abstract] OR "Chiari malformation type 1"[Title/Abstract] OR "Chiari malformation type I"[Title/Abstract] OR "Chiari I"[Title/Abstract] OR "Chiari 1"[Title/Abstract] OR "Chiari type 1"[Title/Abstract] OR "Chiari type I"[Title/Abstract]))) OR (("Chiari syndrome"[Title/Abstract]) NOT Budd-Chiari Syndrome))) NOT ((((("Chiari Malformation Type 2"[Title/Abstract]) OR "Chiari Malformation Type II"[Title/Abstract]) OR "Type II Arnold-Chiari Malformation"[Title/Abstract]) OR "Chiari type II"[Title/Abstract]) OR "Chiari type 2"[Title/Abstract])))
NOT ((animals[MeSH Terms]) OR (animals[MeSH Terms] AND humans[MeSH Terms]))
Filters: Child: birth-18 years
Filters: Publication date from 1999/01/01 to 2019/05/22
“Syringomyelia"[Mesh] OR (Syringomyelia[Title/Abstract] OR Syringomyelias[Title/Abstract] OR Syringomyelus[Title/Abstract] OR syrinx[Title/Abstract] OR Syringobulbia[Title/Abstract] OR Myelosyringosis[Title/Abstract] OR "Morvan Disease"[Title/Abstract] OR "Morvan Diseases"[Title/Abstract] OR "Morvan's Disease"[Title/Abstract] OR "Morvan's Diseases"[Title/Abstract] OR "Morvans Disease"[Title/Abstract] OR Hydrosyringomyelia[Title/Abstract] OR Hydromyelia[Title/Abstract])
NOT ((animals[MeSH Terms]) OR (animals[MeSH Terms] AND humans[MeSH Terms]))
Filters: Child: birth-18 years
Filters: Publication date from 1999/01/01 to 2019/05/22
Appendix 3
Rights and permissions
About this article
Cite this article
Saletti, V., Farinotti, M., Peretta, P. et al. The management of Chiari malformation type 1 and syringomyelia in children: a review of the literature. Neurol Sci 42, 4965–4995 (2021). https://doi.org/10.1007/s10072-021-05565-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05565-9