Abstract
Purpose
Chiari 1 malformation (CM1) is a well-known association with complex craniosynostosis (CC), while it has been rarely reported in association with monosynostosis. The aim of the present study is to investigate on the association between CM1 and untreated sagittal synostosis (USS).
Method
The study included 48 cases of sagittal synostosis (SS), untreated for misdiagnosis and associated with CM1. The children were firstly diagnosed for CM1 by MRI (mean age 9) than for SS (mean age 10.5) by three-dimensional computerized tomography (3D-CT), which documented the absence of the sagittal suture, in the presence of residual indentation of all the other sutures. Syndromic cases were diagnosed by clinical evaluation and molecular studies.
Results
Of the 48 children harboring CM1 plus USS, 21 were asymptomatic for CM1 and are still on follow-up, while 27 children were operated for syringomyelia and scoliosis and/or occurrence of symptoms, three of them had an acute presentation (two papilledema and one sleep apneas) and 11 children had a documented increase of preoperative ICP. Craniovertebral decompression (CVD) was the first-line surgery in 24 children, 16 with duroplasty and five without and eight had also cerebellar (CBL) tonsil coagulation. A cranial vault remodelling was firstly performed in three children. Fifteen percent of children submitted to CVD needed a revision for cerebrospinal fluid (CSF) collection, while two needed both the supra- and infratentorial decompressive procedure and another two needed a treatment for the associated hydrocephalus.
Conclusions
The present study identified an USS in 27 (15.5%) of 174 CM1 children operated for a symptomatic CM1. We suggest to define this association CM1 plus USS, a new subtype of complex CM1. For the high percentage of complications and multiple procedures needed to solve the CM1, we advise to identify by 3D-CT scan these children before performing CVD. Our finding suggests also that, if left untreated, SS may lead to the delayed occurrence of a challenging subset of CM1.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There is a wide literature concerning Chiari malformation type 1 (CM1) associated with complex craniosynostosis [22]. The pathogenesis of this association is multifactorial and is well documented in some studies [1, 28, 3, 14]. The coexistence of low cranial volume, venous engorgement, hydrocephalus, and small posterior fossa [3, 24], due to precocious lambdoid stenosis, all contribute to early onset of a symptomatic CM1. Consequently, the great majority of CM1 associated with craniofacial syndromes are diagnosed and treated in infants. In less severe cases, CM1 may occur later on, with subtle presentation.
The timing of occurrence and the percentage of CM1 in complex craniosynostosis varies in function of the severity of volume constrain, and it depends on the syndrome, ranging from 70% in Crouzon and Pfeiffer and reaching 100% in the cloverleaf skull. Due to the abnormalities in venous drainage, the classical craniovertebral decompression (CVD) may be a high-risk procedure in these settings [29, 17]. Some authors proposed the posterior cranial vault expansion by osteo-distraction aimed to increase supratentorial volume for CM1 treatment/prevention as specific procedures for complex craniosynostosis [25, 16].
Up to now, there are just a few reports about the association of single synostosis with CM1 [8, 11, 23, 24, 26]. The present article focuses on cases of CM1 in which the clinical observation documented a previously unknown/untreated associated cranial deformation, which led to the diagnosis of an associated craniostenosis. In specific, the CM1 has rarely ever been considered as a possible complication of an untreated sagittal synostosis (USS), despite it has been already reported by a few case series [23, 24] .
Driven by the observation of CM1 in a couple of 11-year-old twins with USS, starting from 2008, we performed a “bottom-up” research, reviewing our large series of CM1 in pediatric population to identify the SS untreated in early infancy that caused the occurrence of CM1. This association offers some interesting insights on the interrelationships between the SS and CM1, on the treatment for CM1 plus USS complex and on the indication for surgery in SS [23].
Methods
We routinely performed a cranial vault 3D-CT scan in every child or adolescent with CM1 with a dolichocephalic skull deformation to evaluate the absence of the sagittal suture, suspecting a link between untreated SS and CM1.
The cases included in the present study were selected in a series of 636 children, with a diagnosis of CM1 obtained by magnetic resonance imaging (MRI). They were clinically evaluated between 1998 and 2018 at the Fondazione IRCCS Istituto Neurologico Carlo Besta (FINCB) of Milan by the same team of pediatric neurosurgeons and pediatric neurologists.
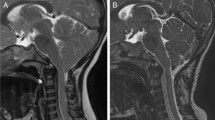
If a child met the clinical criteria of dolichocephalic skull deformity, a 3D-CT scan was performed. 3D-CT protocol included axial volumetric acquisition (thickness 0.8 mm; increment 0.3 mm; pitch 0.688 mm; rotation time 0.75 s; collimation 16 × 0.75; mAs/slice 300; kV 120; FOV 250 × 250; matrix 512 × 512) and subsequent reconstruction algorithms for bone and soft tissues. This exam clearly identified if the SS was absent or physiologically closed (previously patent) (Fig. 1).
3D-CT (a) shows the absence of the sagittal suture in a 7-year-old child (arrow). Sagittal T2-weighted image (b) shows scaphocephaly associated with Chiari 1 malformation with ectopia of the cerebellar tonsils in the cervical canal; subarachnoid spaces at the craniocervical junction are narrow. Note in c the normal appearance of the superior sagittal suture in an age-matched child (arrow)
MR protocol included sagittal T1-weighted images (w.i.), axial and coronal DP and T2 w.i., and a flow-sensitive phase-contrast (PC) technique to qualitatively assess cerebrospinal fluid (CSF) flow dynamics at the craniocervical junction. We preferentially used a CSF flow velocity of 7 cm/s with in-plane velocity encoding in the craniocaudal direction. The entity of tonsils herniation was measured in millimeters using the perpendicular line to the Basion-Opisthion line.
For each patient who was identified as affected by CM1 plus USS, the following data were collected: age at diagnosis of CM1, the presence/absence of cervicomedullary kinking, syringomyelia, hydrocephalus and craniovertebral junction (CVJ) anomalies, age at diagnosis of SS, associated malformations, age at time of surgical procedure, surgical procedures, outcome after surgical procedure, and duration of follow-up. All patients with suspicious findings were submitted also to molecular studies to roll out a syndromic craniosynostosis or other possible associated genetic disorders. Finally, the Cranial Index was measured on CT scans, according to the method recently reported by Sultan Z. Al-Shaqsi [2] was obtained.
In some recent cases with documented USS who deserved surgical treatment, intracranial pressure (ICP) measurement was performed during surgery [10]. The standardized procedure of continuous ICP monitoring includes placement of a solid sensor (Codman MicroSensor™, Johnson & Johnson, Raynham, MA, USA) 1–2 cm into the brain parenchyma by a minimal opening of the skull and dura [10].
Results
Neuroradiological findings
A total of 92/636 children (14%) showed dolichocephalic skull deformity. The 3D-CT examination clearly ascertained the 48 cases with a SS by the absence of the suture, defined as true USS, from the dolichocephalic ones, in whom a previously patent suture was documented by the typical residual sew like indentation of the sagittal bone (see Fig. 1). A previously unknown/untreated sagittal synostosis was found in 48/92, representing the 7.5% of the whole CM1 series and 16% of the surgical cases. All children had a reduced bi-parietal diameter, and many presented the typical bulging in fontanel region, with retrocoronal sinking at vertex. The Cranial Index of the 48 CM1 plus USS is reported in Fig. 2. 3D-CT scans documented the absence just of the sagittal suture (monosutural SS) in all the cases, except one, which had also a very partial closure of the right lambdoid suture (Fig. 3).
3D-CT (a, b) demonstrates complete closure of the superior sagittal suture and partial closure of the lambdoid suture on the left side. Sagittal T2-weighted image (c) shows Chiari I malformation and a huge syrinx in the cervical spinal cord. Immediate MRI after second craniovertebral decompression and cranial vault remodelling (d) demonstrating the syrinx reduction and the CSF collection at the convexity. Finally, the sagittal T2-weighted image (e) at control MRI 3 years later shows of syrinx reduction and normal position of the tonsils and medulla oblongata
A ventricular enlargement was associated in 5 cases, with the features of true hydrocephalus just in 2 cases (4%). A dilatation of the central canal was documented in 27/48 cases (56%): in 6, it was a mild dilatation of the central canal, while in the remaining 21, a true syringomyelia was documented (Table 1).
The mean tonsil descent in the surgical group was 12 mm, while it was 5–6 mm in the non-surgical group. In all the cases, both symptomatic and asymptomatic, the MRI documented a reduced CSF flow at the craniocervical junction and a compensatory pulsatile descent of the cerebellar tonsils was observed during systole (Fig. 4). Eight children (16.3%) have been classified as CM1.5. They were also submitted to dynamic CT, which excluded CVJ instability in all of them.
Sagittal T1-weighted image (a) and MRI CSF flow study (b) demonstrate Chiari I malformation associated with a mild retroflexion of the dens, associated with small hydrosyringomyelia in C4-C5. Note in b the absence of normal CSF pulsatility in the Silvio’s aqueductus and in the retro-tonsillar subarachnoid spaces. 3D-CT (c) and sagittal T1-weighted image (d). Image c shows superior sagittal synostosis; image d shows Chiari 1.5 malformation with basilar invagination. Note the small posterior fossa with downward displacement of the cerebellar tonsils and distortion of the medulla oblongata
Clinical pictures
The series is resumed in Table 1, showing the clinical and radiological data.
A male prevalence (29/19) was observed. The mean age at diagnosis of CM1 was 9 years, ranging from 4 to 18 years, while the mean age of diagnosis of SS was 10.4 years. In fact, SS was diagnosed at the same time of CM1 in 30 children and after CM1 in 17 cases, with a delay of 1 year in 7, of 2 years in 5 and of more than 3 years in the remaining 5, with a maximum of 17 years of delay. Only 1 child had the SS diagnosis in infancy by X-ray, but the malformation was left untreated, because the surgery was retained too dangerous by the pediatrician.
Signs and symptoms that led to the diagnosis of CM1 were various (Table 1): headache was prevalent (22, 44%), despite just 9 children had typical CM1 headache, according to the international classification IHS [15], papilledema with visual deficit [4], scoliosis [3], sleep apneas [2], gait disorders [1], drop attacks [1], and dizziness [1].
The diagnosis of CM1 was an incidental finding in 21 patients (43%): 3 children were asymptomatic (2 submitted to MRI for head trauma and 1 for diagnosis of Alagille syndrome), while the remaining had symptoms unrelated to CM1 (2 Tics, 2 seizures, 2 macrocrania, 2 somatic hypoevolutism). It is worth noting that 12 children were submitted to MRI for a condition of intellectual disability of unknown aetiology and 1 for behavioral disorders. In 4 children, an associated growth hormone (GH) deficiency was identified and treated by supplementation.
In addition to the child affected by Alagille syndrome, the clinical and genetic evaluation identified 21 children with clinical syndromes, despite having just the isolated SS closure; in 19, a syndrome was excluded, and in 8, there were no suggestive clinical elements for a syndromic diagnosis. The clinical conditions and the genetically determined syndromes are reported in Table 1.
Neuropsychological testing documented mental delay in 14/48 cases, 12 of mild and 2 of mean severity. Two children had autistic spectrum diseases.
The 21 children, who were considered asymptomatic for CM1 and had no significant syringomyelia, were submitted to control craniospinal MRI every year. The mean CBL tonsils descent in this group was 5 mm, and a minimal dilatation of the central canal was present just in 6/21 (28.5%). After a mean observation time of 4 years, none of them worsened, neither clinically nor at control MRI.
Surgical treatments
Table 2 shows the surgical data and the outcome. In 27 patients (56.2%), surgical treatment was indicated for CM1 symptoms and/or evolving scoliosis and/or enlarging syringomyelia. The age at surgery ranged from 4 to 19 years, with a mean of 7 years.
It is worth noting that the mean descent of cerebellar (CBL) tonsils in this surgical group was 12 mm. A syringomyelia was present in 21/27 (77.7%), alone or associated with scoliosis [3] or symptoms (visual deficits, dizziness, bulbar signs, sleep apneas, typical headache, gait disturbances).
In all symptomatic cases, the neurological deterioration once started, became rapidly progressive within a few months. Three children had an acute onset: 2 with papilledema and visual loss and 1 with sleep apneas.
As the first surgical approach, 23 children were submitted to a CVD, without dural opening in 5, with duroplasty in 10, and with tonsil coagulation in 8 cases.
CVD was performed by the same surgeon, with the same technique: in prone position, a small suboccipital craniectomy, widely extended at the foramen magnum, was associated with C1 laminectomy; under magnification, a dural longitudinal incision made on the midline was performed at the level of craniovertebral junction, trying to preserve the arachnoidal plane. The CBL tonsils were coagulated to obtain the shrinkage in 8 cases, due to their too low position or to their extrusion through the dural opening secondary to the increased intracranial pressure (ICP). Finally, an allograft rhomboid duroplasty was tightly closed with an unreasonable 5 or 6 zeros continuum suture.
Two children had an associated symptomatic hydrocephalus: 1 case was treated by VCS, while the other, a 15-year-old boy who presented with an acute visual loss and clinical signs of raised ICP, needed a shunt, because of failure of the VCS controlling increased ICP despite a good flow documented at cine-MRI; consequently, a programmable shunt was implanted, then a CVD was performed; a permanent low pressure setting (< 90 mmHg) of the shunt was needed to preserve the minimal residual visual acuity. The permanent visual impairment in this case was explained by the concomitance of long-lasting increased ICP with entrapment of CSF in the optic nerve sheets, due to narrow elongated optic canals.
Three patients needed a revision of the duroplasty for CSF leak and recurrent collections, which represented 15% of CVD with dural opening (3/19).
When the first surgery failed controlling symptoms or syringomyelia, another surgical option was offered. Up to now, multiple surgeries were performed in 2 cases.
The first of them, a 7-year-old child after a first CVD with duroplasty had a limited ascent of the tonsils and a relevant residual syringomyelia was still evident at the second year control MRI; a redo CVD surgery was performed, extending the craniectomy more laterally at the foramen magnum, coagulating and resecting the CBL tonsils; afterwards, he had recurrent CSF collections, unresponsive to subsequent surgical revision, probably due to an increased ICP. Trying to solve the problem, posterior cranial vault expansion was performed, causing a diffusion of the CSF collection along the wide area of cranial vault dissection. The problem was solved positioning a subgaleo-peritoneal programmable shunt, which was progressively closed and finally removed 1 year afterwards. Since these observations of indirect signs of increased ICP, due to the intracranial craniocerebral disproportion, we changed our strategy in children with CM1 associated with USS (Fig. 3).
Firstly, we started routine intraoperative ICP measurement. Up to now, 11/27 children had a documented increase of ICP: the mean pressure measured before surgery was 19 mmHg (ranging from 10 to 24 mmHg); these intraoperative results before CVD are reported in Table 2. The pressure temporarily dropped after duroplasty, to rise again after surgery and remain so in the first postoperative week. Afterwards, the ICP progressively normalized in all the cases and ICP measurement was stopped in a few days. In order to prevent CSF collection, a compressive bandage was maintained for a couple of weeks in all the cases.
Secondly, whenever possible according to age and skull conformation, we performed a cranial vault remodelling before CVD. This procedure was aimed to increase the skull volume, to reduce the competition for space between brain and CBL, mimicking the effects of osteo-distraction techniques for complex craniosynostosis (Fig. 5). The classical osteodistraction procedure has the effect of “elongating the skull” and consequently is not suitable for the USS.
Post-surgery 3D-CT reconstruction demonstrates the effects of cranial vault remodelling by the free flaps technique: this remodelling, which increases both the wide and the vertical diameter, was performed before CVD to obtain increased skull volume, so reducing competition for space between the brain and CBL
We performed a complete cranial vault remodelling, by a zig-zag bicoronal approach, using a personal free flaps technique, extended also on the sagittal area to favor vertical and wide expansion (Fig. 6).
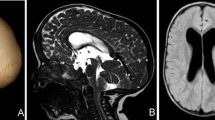
3D-CT (a, b) and Sagittal T1 weighted image (c) show pansynostosis, small posterior cranial fossa with tonsils ectopia, medulla oblongata kinking and empty sella secondary to endocranial hypertension. 3D-CT (d, e) show the anterior vault cranioplasty and craniovertebral decompression (CVD). The cerebellar tonsils are at the level of the foramen magnum and the kinking of the medulla oblongata is less evident (f). However note in F the presence of a large syrinx. After II surgical intervention of Cranial vault remodelling (g, h) the cerebellar tonsils and the medulla oblongata position are normal and the syrinx is disappeared (i)
The policy “Cranial Vault Remodelling first” was applied in the last 4 cases, respectively, 4, 5, 7, and 11 years old. In one case, the CVD was performed a few weeks after the cranioplasty, due to the persistence of a symptomatic syringomyelia; this is the second child submitted to a double surgery, aimed to enlarge both supra- and infratentorial volumes.
Surgical outcome
At a mean follow-up of 5 years (min 1, max 16 years), 26/27 operated children were evaluable. All of them, after completing their surgical path, had benefit on preoperative symptoms, except the aforementioned detrimental visual function, which just stabilized; this child improved by all the other point of views.
The control MRI showed a restoration of normal posterior fossa CSF flow and an upward migration of CBL tonsils in 23/27 and a stable picture in the remaining 4. Among the 20 evaluable children harboring a syringomyelia, 17 (85%) displayed a shrinkage while 3 remained stable at mean term follow-up (Fig. 7).
Sagittal T2 weighted image performed before (a) and 4 years after operation (b), in a child affected by CM1 plus SS, operated by CVD at 10 years of age; the picture shows the complete shrinkage of the syrinx, associated with normalization of clinical picture, and the benefit remained the same al late control, 8 years after
More in detail, the cranial vault remodelling addressed to USS was performed in 5 children. In 2 cases in addition to CVD (1 after and 1 before): both experienced good clinical and radiological results, with shrinkage of the syringomyelia and disappearance of symptoms (Fig. 3e). The remaining 3 are still under evaluation: 2 are stable at MRI and the third, after a good initial response, displayed recently a late worsening 6 years after first surgery.
It is worth noting that other 4 cases displayed this biphasic response. After an initial favorable clinical and MRI outcome, a delayed radiological worsening was observed in 5 children (respectively at 10, 8, 7, 6, and 3 years after first surgery), characterized by recurrence of tonsil descent and reappearance of syringomyelia, associated with clinical symptoms in 3/5 children (Fig. 8).
Showing the “double-phase” outcome: sagittal T2 weighted images performed before (a) and 5 years after surgery (b), in a child affected by CM1 plus SS, operated by CVD at 6 years of age; the picture shows the disappearance of the pre-syrinx and the tonsils ascent. The 10-year postoperative MRI (c) showed the reappearance of CM1, with tonsils descent and occurrence of asymptomatic syringomyelia. The associated USS was suspected and confirmed by a 3D-CT at this time
Discussion
The present study identified a subset of CM1 children, associated with USS, characterized by early onset of symptoms, high percentage of increased ICP, and mental delay. CM1 plus USS had high frequency of surgical complications after CVD and a low efficacy of CVD alone controlling symptoms and syringomyelia.
While there is a wide literature concerning the occurrence of CM with complex craniosynostosis, there are just a few reports about the association of monosynostosis with CM [6, 11, 20]. Some authors reported a very low incidence (1.1%) [11], but a recent study reported an increased incidence of CM1 in a large series of ISS, especially with delayed diagnosis and treatment (5.7%) [8].
In our series of CM1 children, the association with SS was observed in a significant percentage, especially if more serious surgical cases are taken into account (15.5%), reinforcing the suspicion of a cause-effect relationship between SS and CM1.
The pathogenesis of CM1 in SS has been explained by the downward compensatory cranial growth, which causes a constraint to the posterior cranial vault vertical expansion, resulting in a posterior fossa smaller than normal [11]. The reduced supratentorial volume contributes to downward CBL migration (Fig. 9), directly or through the increase of ICP, probably also related to the venous hypertension due to superior sagittal sinus constriction in the bony groove [9].
Resumes the pathogenetic mechanisms of CM1 due to USS: the posterior and transverse skull tightness (a) responsible for the craniocerebral disproportion, causes a conflict for space between the brain and the cerebellum, evidenced by the caudal displacement of the tentorium (c). The associated downward compensatory cranial growth results in a posterior fossa smaller than normal (b). The venous hypertension due to superior sagittal sinus constriction in the bony groove (d) may also contribute to occurrence of symptoms, increasing the ICP
These pathogenetic mechanisms, which progressively enhance their effects along growth, may explain the delayed occurrence of CM1 observed in the present series of USS, if compared with the young age of presentation observed in complex craniosynostosis: in CM1 plus USS symptoms that occurred during school age in the great majority of cases. It could not be incidental that the youngest child of the series presented beside the SS also a partial lambdoid closure (Fig. 3). The posterior fossa condyle asymmetry due to the lambdoidal stenosis probably contributed with the syrinx and to the early occurrence of the rapidly progressive scoliosis. In this specific case, the almost double suture closure contributed to the early occurrence of symptoms, behaving somehow half way between isolated and complex craniosynostosis.
An increased ICP was measured in the majority of surgical cases when tested. This data explains the high percentage of CSF collections (15%) in CM1 plus USS, quite more relevant than the figures of the global CM1 series (< 5%), treated by the same surgeon, with the same technique [30].
In the meantime, the increased ICP may play a role in the development delay observed in 30% of this CM1 plus USS series, which is higher than the figures reported for ISS. One limitation of the present study is the lack of a genetic study for ERF mutation, frequently associated with increased ICP, but due its rarity, especially in association with monosynostosis, its occurrence is unlikely possible in all the cases of the present series associated with increased ICP [13, 8].
Moreover, the long-term efficacy of CVD on symptoms and syringomyelia was lower than figures reported by the same technique performed by the same surgeon on CM1 children [30]. Finally, 5 cases presented a biphasic outcome, characterized by an initial prolonged improvement, followed by a delayed recurrence of syrinx and symptoms, an uncommon behavior in CM1 treated by this technique (Fig. 8). This outcome suggests a double causal factor (competition for volume and small posterior fossa), both needing a surgical treatment, one by cranial vault remodelling and the other by CVD.
It is clear that the best prevention of CM1 plus USS would have been a timed and efficient SS correction. So far, it is still not clear up to which age cranial vault remodelling alone may prevent the restriction of posterior fossa, causing CM1 and syringomyelia: 3 children submitted firstly to cranioplasty are still on evaluation, while 2 cases submitted to both procedures are doing well. It is likely that, once CM1 due to USS becomes symptomatic, both procedures are needed to revert it. The advantage obtained performing cranial vault expansion before CVD is to reduce complication rate after CVD.
Last but not least, the present observation offers some suggestions in favor of functional aim of SS correction. In fact, the role of surgical correction SS is still matter of debate, as well as the technique, due to the difficulties comparing the long-term aesthetical and functional results. The cosmesis is hard to objective and quantify, and the long-term cognitive outcome may be influenced by many variables that are frequently difficult if not impossible to ascertain. Neurodevelopmental studies highlighted that SS is associated with an increased risk for mild but persistent deficits in attention and processing speed, learning, memory, speech and language, and visuospatial abilities [4, 12, 5, 7, 18, 19, 21, 27]. However, there are limited data about the factors, both intrinsic (e.g. presence and duration of raised intracranial pressure, associated brain abnormalities, presence of gene mutations) and extrinsic (e.g. patient’s environment, socioeconomic background, age at surgery, type of surgical intervention) that influence the neurodevelopmental outcome [8]. Due to this uncertainty, balancing the operative risks versus natural history, some authors even questioned the indication for surgery in SS and others stated that it has just a cosmetic aim [18].
The present series of CM1 plus USS gives some clues about natural history of ISS: if left untreated, SS carries the risk to develop a symptomatic CM1, associated with increased ICP and hard to treat by CVD alone. Consequently, cranioplasty for ISS has the functional meaning to prevent the occurrence of these events. Based on our observation, different surgical techniques for ISS correction should be evaluated at long term, not only by their cosmetic results, but also by their functional effects, as their capability to prevent the occurrence delayed CM1.
Conclusions
The present study identified a subset of CM1, associated with USS, which is challenging both at presentation, with a rapidly progressive neurological deterioration, and at treatment, due to the high ICP associated. We advise identifying this complex CM1 subset by 3D-CT scan once observing a dolichocephalic deformation in a child with CM1. If asymptomatic, CM1 plus USS deserve a careful clinical follow-up and sequenced RM to rule out occurrence of syrinx and hydrocephalus, which may have catastrophic effects on vision. Once symptomatic, it deserves prompt surgery; peri-operative ICP monitoring could be useful identifying cases that eventually need cranial vault expansion. Cranial vault remodelling as the first choice may be taken into account, despite advanced age at diagnosis can make it a major procedure.
References
Al-Otibi M, Jea A, Kulkarni AV (2007) Detection of important venous collaterals by computed tomography venogram in multisutural synostosis. J Neurosurg 107:508–510
Al-Shaqsi SZ, Rai A, Forrest C, Phillips JJ (2019) Standardization of cranial index measurement in sagittal craniosynostosis. J Craniofacial Surg 30(2):366–369
Aydin S, Hanimoglu H, Tanriverdi T, Yentur E, Kaynar MY (2005) Chiari type I malformations in adults: a morphometric analysis of the posterior cranial fossa. Surg Neurol 64:237–241
Boltshauser E, Ludwig S, Dietrich F, Landolt MA (2003) Sagittal craniosynostosis: cognitive development, behaviour, and quality of life in unoperated children. Neuropeditrics 34:293–300
Chieffo D, Tamburrini G, Massimi L, Di Giovanni S, Giasanti C, Caldarelli M, Di Rocco C (2010) Long-term neuropsychological development in single-suture craniosynostosis treated early. J Neurosurg Pediatr 5:232–237
Cinalli G, Spennato P, Sainte-Rose C, Arnaud E, Aliberti F, Brunelle F (2005) Chiari malformation in craniosynostosis. Childs Nerv Syst 21:889–901
Da Costa AC, Vicki A, Savarirayan AR, Wrennall JA, Chong DK, Holmes AD, Greensmith AL, Meara JG (2012) Neurodevelopmental functioning of infants with untreated single-suture craniosynostosis during early infancy. Childs Nerv Syst 28:869–877
Davis AA, Zuccoli G, Haredy MM, Runkel L, Losee J, Pollack IF, Tamber MS, Tyler-Kabara E, Goldstein JA, Nischal KK (2019) The incidence of Chiari malformations in patients with isolated sagittal synostosis. Plast Reconstr Surg Glob Open 7(2):2090
Di Rocco C, Frassanito P, Massimi L, Peraio S (2011) Hydrocephalus and Chiari type I malformation. Childs Nerv Syst 27:1653–1664
Eide PK (2008) Comparison of simultaneous continuous intracranial pressure (ICP) signals from ICP sensors placed within the brain parenchyma and the epidural space. Med Eng Phys 30:34–40
Engel M, Castrillón-Oberndorfer G, Hoffmann J, Orakcioglu B, Rohde S, Seeberger R, Freudlsperger C (2012) Chiari malformation in nonsyndromal single craniosynostosis--much ado about nothing? Acta Neurochir 154(10):1803–1807
Fearon JA, Singh DJ, Beals SP, Yu JC (2007) The diagnosis and treatment of single-sutural synostoses: are computed tomographic scans necessary? Plast Reconstr Surg 120:1327–1331
Glass GE, O’Hara J, Canham N, Cillier SD, Dunaway D, Fenwick AL, Jeelani NO, Johnson D, Lester T, Lord H, JEV M, Nishikawa H, Noons P, Schwiebert K, Shipste C, Taylor-Beadling A, SRF T, Vasudevan P, Wall SA, AOM W, Wilson LC (2019) ERF-related craniosynostosis: the phenotypic and developmental profile of a new craniosynostosis syndrome. Am J Med Genet A 179(4):615–627
Goldstein JA, Paliga JT, Bailey RL, Heuer GG, Taylor JA (2013) Posterior vault distraction with midface distraction without osteotomy as a first stage for syndromic craniosynostosis. J Craniofac Surg. 24(4):1263–1267
Headache Classification Committee of the International Society (2013) The international classification of headache disorders 3rd edition (Beta version). Cephalalgia 33(9):629–808
Iida C, Sakamoto Y, Miwa T, Yoshida K, Kishi K (2019) Posterior distraction first or fronto-orbital advancement first for severe syndromic craniosynostosis. J Craniofac Surg 30(1):47–49
Jeevan DS, Anlsow P, Jayamohan J (2008) Abnormal venous drainage in syndromic craniosynostosis and the role of CT venography. Childs Nerv Syst 24:1413–1420
Kapp-Simon KA, Speltz ML, Cunningham ML, Patel PK, Tomita T (2007) Neurodevelopment of children with single suture craniosynostosis: a review. CNeS 23:269–281
Knight SJ, Anderson VA, Spencer-Smith MM, Da Costa AC (2014) Neurodevelopmental outcomes in infants and children with single-suture craniosynostosis: a systematic review. Dev Neuropsychol 39:159–186
Leikola J, Koljonen V, Valanne L, Hukki J (2010) The incidence of Chiari malformation in non-syndromic single suture craniosynostosis. Childs Nerv Syst 26:771–774
Lekovic GP, Bristol RE, Rekate HL (2004) Cognitive impact of craniosynostosis. Semin Pediatr Neurol 11:305–310
Mathijssen IM (2015) Guideline for care of patients with the diagnoses of craniosynostosis: working group on craniosynostosis. J Craniofac Surg 26:1735–1807
Pouratian N, Sansur CA, Newman SA, Jane JA Jr, Jane JA Sr (2007) Chiari malformations in patients with uncorrected sagittal synostosis. Surg Neurol 67:422–428
Rijken BF, Lequin MH, van der Lijn F, van Veelen-Vincent ML, de Rooi J, Hoogendam YY, Niessen WJ, Mathijssen IM (2015) The role of the posterior fossa in developing Chiari I malformation in children with craniosynostosis syndromes. J Craniomaxillofac Surg 43:813–819
Sakamoto Y, Miwa T, Nakajima H, Yoshida K, Kishi K (2016) A new technique for posterior distraction in craniosynostosis: the double-door technique. J Craniofac Surg 27(4):950–952
Sandberg DI, Navarro R, Blanch J, Ragheb J (2007) Anomalous venous drainage preventing safe posterior fossa decompression in patients with Chiari malformation type I and multisutural craniosynostosis. J Neurosurg 106:490–494
Shipster C, Hearst D, Somerville A, Stackhouse J, Hayward R, Wade A (2003) Speech, language, and cognitive development in children with isolated sagittal synostosis. Dev Med Child Neurol l45:34–43
Strahle J, Muraszko KM, Buchman SR, Kapurch J, Garton HJ, Maher CO (2011) Chiari malformation associated with craniosynostosis. Neurosurg Focus 31(3):E2
Thompson DN, Hayward RD, Harkness WJ, Bingham RM, Jones BM (1995) Lessons from a case of kleeblattscha. Case report. J Neurosurg 82:1071–1074
Valentini L, Visintini S, Saletti V, Chiapparini L, Estienne M, Solero CL (2011) Treatment for Chiari 1 malformation (CIM): analysis of a pediatric surgical series. Neurol Sci 32(Suppl 3):S321–S324
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Laura Valentini.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Valentini, L.G., Saletti, V., Erbetta, A. et al. Chiari 1 malformation and untreated sagittal synostosis: a new subset of complex Chiari?. Childs Nerv Syst 35, 1741–1753 (2019). https://doi.org/10.1007/s00381-019-04283-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04283-0