Abstract
Background
Syringomyelia and Chiari malformation are classified as rare diseases on Orphanet, but international guidelines on diagnostic criteria and case definition are missing. Aim of the study: to reach a consensus among international experts on controversial issues in diagnosis and treatment of Chiari 1 malformation and syringomyelia in adults.
Methods
A multidisciplinary panel of the Chiari and Syringomyelia Consortium (4 neurosurgeons, 2 neurologists, 1 neuroradiologist, 1 pediatric neurologist) appointed an international Jury of experts to elaborate a consensus document. After an evidence-based review and further discussions, 63 draft statements grouped in 4 domains (definition and classification/planning/surgery/isolated syringomyelia) were formulated. A Jury of 32 experts in the field of diagnosis and treatment of Chiari and syringomyelia and patient representatives were invited to take part in a three-round Delphi process. The Jury received a structured questionnaire containing the 63 statements, each to be voted on a 4-point Likert-type scale and commented. Statements with agreement <75% were revised and entered round 2. Round 3 was face-to-face, during the Chiari Consensus Conference (Milan, November 2019).
Results
Thirty-one out of 32 Jury members (6 neurologists, 4 neuroradiologists, 19 neurosurgeons, and 2 patient association representatives) participated in the consensus. After round 2, a consensus was reached on 57/63 statements (90.5%). The six difficult statements were revised and voted in round 3, and the whole set of statements was further discussed and approved.
Conclusions
The consensus document consists of 63 statements which benefited from expert discussion and fine-tuning, serving clinicians and researchers following adults with Chiari and syringomyelia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chiari malformation (CM) includes a heterogeneous group of congenital malformations mainly characterized by the caudal cerebellum ptosis through the foramen magnum. Chiari type 1 malformation (CM1) can cause a wide variety of neurological symptoms, often vague or nonspecific, such as headaches, ocular and otoneurologic disturbances, lower cranial nerve signs, cerebellar ataxia, or spasticity [1]; clinical manifestations define the Arnold-Chiari or Chiari syndrome (CS). Onset of symptoms is usually in the third decade of life. However, many individuals with CM1 remain asymptomatic even later. CM1 in the European community is classified as a rare disease (ORPHA code: 268882); in Italy, CM1 prevalence and incidence in different gender, age classes (0–17, 18–60, >60 years), and symptomatic and asymptomatic forms have been reported in a recent study, focusing on clinical phenotypes and natural history [2].
Syringomyelia (Syr) is morphologically defined at magnetic resonance imaging (MRI) as the presence of single or multiple fluid-filled cavities (syrinx) within the parenchyma of the spinal cord and/or the bulb (syringobulbia); it is classified as a rare disease (ORPHA code: 3280). About 50% of Syr patients have severe neurological damage and chronic progressive disability with complete loss of independence. Prognostically speaking, even more unfavorable is the presence of syringobulbia (swallowing and breathing bulbar centers involved). In studies conducted before the advent of modern neuroimaging, prevalence ranged from 3.3 to 8.5/100,000 [3–5]; after the advent of MRI, estimated prevalence ranged from 1.9 to 8.4/100,000 [6, 7]. The incidence of Syr in the Russian Federation is about 10 cases per 100,000 population, and the majority of cases occur in males over 30–35 years [8]. In Italy, Syr prevalence in adults is 5.9, incidence 1.06 [2].
Syringomyelia and Chiari malformation are classified as rare diseases (RD) on Orphanet, the international reference for RD and orphan drugs, but international guidelines on diagnostic criteria and case definition are missing. The increased ability to diagnose CM and Syr by MRI and its widespread availability have led to an increase of reported cases, often asymptomatic or minimally symptomatic, with the need to standardize definitions, diagnostic criteria, and treatments. Indications, optimal timing, and type of surgical intervention to treat Syr associated with CM1 are unclear; prospective and controlled trials are lacking.
Since 2008, an Italian multidisciplinary group, dedicated to the study of CM and Syr and composed of clinicians (neurologists, neurosurgeons, neuroradiologists, physiatrists, neuro-urologists, psychologists, speech pathologists, spinal surgeons, pain specialists), experts of public health for RD, and patient association representatives, was founded and named “Chiari and Syringomyelia Consortium” [2]. Diagnostic, surgical, and rehabilitative recommendations on CM1 and Syr were proposed and published by the Chiari and Syringomyelia Consortium [9]; some of these recommendations derived from the outcomes of the Consortium meetings, and others were from the “First Chiari Consensus Conference,” held in Milan in 2009 [10].
The aim of this study, issued by a panel of the Chiari-Syringomyelia Consortium, was to reach a wide and international consensus on main and controversial topics in the diagnosis and treatment of CM1 and Syr in adults.
Materials and methods
Literature review
In order to establish the statements on definition-classification/surgical planning for CM1 and isolated Syr, they were developed following several steps: (a) collecting all available evidence on clinical studies related to Syr and CM1. The following databases were queried for literature review: Medline (PubMed interface, www.pubmed.gov), Cochrane Library (Health Library of Piedmont, www.bvspiemonte.it), National Guidelines Clearinghouse (www.guideline.gov). The literature search strategy was conducted by combining the following: the Medical Subject Heading (MeSH): “Arnold-Chiari Malformation” or “Chiari Malformation” or “Chiari type 1 Malformation” or “Chiari Syndrome” or “Chiari” or “Syringomyelia” or “Arnold-Chiari Malformation” (or all the eponyms) AND “Syringomyelia,” and publication type (PT): “systematic reviews,” “practice guideline,” “meta-analysis,” “randomized controlled trial.” (b) Assessing studies for relevance and level of evidence. All studies were selected and critically evaluated. Results with low evidence level were restricted for date (last 20 years) and language (English); these were also selected and critically evaluated. The search on scientific literature resulted in 15 systematic reviews, 5 meta-analyses, 2 randomized controlled trials on Chiari and syringomyelia.
Delphi consensus study
A panel of experts of the Chiari and Syringomyelia Consortium [9], on the basis of the evidence literature review, formulated 63 draft statements on the main and controversial topics on CM1 and Syr. The statements were collected in a general addendum, including definitions, classifications, and diagnostic criteria, and in two separate questionnaires, one concerning children and the other adults, composed of different sessions on diagnostic and surgical indications, techniques, outcomes, and differential diagnosis in CM1 with Syr, in isolated CM1, and in isolated Syr.
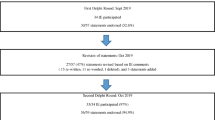
The panel appointed a Jury of 32 international multidisciplinary experts and patient association representatives on CM1 and Syr to elaborate a consensus document; the international experts, coming from European and extra European Countries, were designed by the criteria of scientific production (authors of more than 225 peer-reviewed papers on CM1/Syr) and clinical expertise, based on an experience of more than 18,000 CM1/Syr adults followed (of which 4692 CM1 and 1994 Syr patients were operated on). Thirty-one members (19 neurosurgeons, 6 neurologists, 4 neuroradiologists, and 2 patient association representatives) agreed to participate. The consensus process (Fig. 1) was based on three rounds: rounds 1 and 2 were run by email, and round 3 was face-to-face, during the Chiari Consensus Conference held in Milan in November 2019. Each member voted each statement on a 4-point Likert-type scale (strongly disagree/disagree/agree/strongly agree), according to the Delphi method [11]; comments on each statement (recommended in case of disagreement) were reported as free text. Statements with agreement <75% (threshold value) were revised and entered in the subsequent round.
In this paper, the results regarding the statements on the general addendum (n = 12) and adult questionnaire (n = 51) are reported.
Results and discussion
A description of the 63 evidence-based statements and the relative agreement (in percentage) for CM and Syr in adults, including classifications, definitions, surgical indications, and outcomes, are reported in Tables 1, 2, 3, 4, 5, and 6. Agreement percentages for each statement (% = N agree/N experts × 100), calculated and chronologically reported at round 1, round 2, and round 3, are shown in Fig. 2. At round 1, a total of 32 statements (50.8%) were approved; a total of 57 statements (90.5%) after round 2 and all the 63 statements (100%) at round 3 were approved by the experts.
Adult consensus document: agreement (%) in the three Delphi rounds. 32 statements (50.8%) were approved at round 1 (in blue); 13 were beyond the 75% but required some rewording following the experts’ comments. A total of 57 statements (90.5%) were approved at round 2 (in red). Statements with agreement <75% (threshold value) were revised, discussed, and voted in round 3 (in green), and all 63 statements were approved
Radiological criteria for the diagnosis of CM1 and Syr were not the focus of the questionnaire, as new classification criteria are in preparation by an international study group. Nevertheless, we asked the whole jury to confirm/disconfirm the 2009 Consensus Conference Diagnostic Criteria adopted since 2010 by the Italian “Chiari-Syringomyelia Consortium” as a baseline for clinical guidelines. Diagnostic recommendations on Chiari and Syr published by the Consortium were reviewed and critically evaluated by the international jury. The final average agreement was globally high (88%): definitions reached almost 98% for syringomyelia and hydromyelia, 89% for Chiari (94% for clinical definition); classification agreement was 86–87%; differential diagnosis was agreed with 91%, higher for intracranial hypertension than hypotension.
Ten of the 63 statements reached the highest agreement (95–100%), in particular on diagnostic assessment and surgical indications.
Section 1: Classifications and definitions (Table 1)
In Chiari classification, only CM1 and CM2 types were considered, from the original description by Hans Chiari [12–14]; CM types 3 and 4 are very severe embryonic anomalies, extremely rare, and not related to types 1 and 2, so they were not included in this classification (Table 1).
“CM1” is a cerebellar dysplasia, including in the wider group of the congenital malformations, due to the abnormal notochordal closure; “CM2” is a tonsil herniation associated with spinal dysraphism, such as open or, sometimes, closed, terminal cystoceles.
The most recent and controversial definitions “CM1.5” and “CM0” [15–19] were included in the Chiari classification for the first time in a scientific context as distinct entities.
“CM1.5” or “complex Chiari” implies the occurrence of tonsil prolapse and brainstem kinking in the setting of a cranio-vertebral junction (CVJ) malformation (i.e., Klippel-Feil anomaly, atlanto-occipital fusion, basilar invagination, retroversion of the odontoid process) and requires a specific surgical approach.
“CM0” defines syringomyelia (“slit-like lesion”) without tonsil descent or a crowded foramen magnum or a tight cisterna magna; the agreement on this controversial definition was, at last, reached.
There was a higher agreement for the definition of “acquired tonsillar ectopia,” also called “acquired Chiari malformation” (ACM): in a recent systematic review [20], it is defined as a cerebellar tonsil herniation secondary to space-occupying lesions, such as hydrocephalus, brain tumors (meningiomas, 36%) and arachnoid cysts (32%); offending lesions were usually large (85%), and almost all were found in the posterior fossa (89%). Syr was present in 82% of cases; surgical management of the underlying lesion, associated or less with foramen magnum decompression, equally improved ACM and associated Syr with no need to address surgery to the Syr itself.
MRI definition of CM1 and clinical definitions of “Chiari syndrome” are reported in the International Classification of Headache Disorders (ICHD-III, 2018) [21]. Awaiting for new radiological criteria, the 5 mm rule was confirmed as CM radiological definition in a recent paper [2] and by this international consensus: tonsil descent <3 mm is considered a physiological variation (normal MRI), while between 3 and 5 mm a borderline ectopia, deserving observational approach in symptomatic cases, in the presence of syrinx or peg-like tonsillar profile, or of subarachnoid space crowding in the area of the cranio-cervical junction [21, 22].
Chiari syndrome (CS) or “symptomatic Chiari” is the clinical manifestation of CM1 (clinical definition). Symptomatic Chiari is more common in adults than in children, particularly (60%) in CM1 with syringomyelia; conversely, in isolated Chiari, only 25% are symptomatic [23].
The International Headache Society (ICHD-III, 2018) includes headache attributed to CM1 among secondary headaches and suggests diagnostic criteria [21]. Chiari-distinctive headache is usually severe and paroxysmal, occipital-suboccipital, with a tendency for accentuation by Valsalva, head dependency, sudden postural change, and physical exertion; cough “triggered” headache is considered the most specific CM1-related headache. Indeed, many other types of primary headaches were reported in CM1 patients, such as migraine, tension-type headache, and cluster headache [23]. Clinical diagnostic criteria include “headache caused by CM1” and neurological symptoms and signs in relation to the brainstem (i.e., nystagmus, dysfagia, sleep apnea), cerebellar (ataxia), and spinal cord dysfunction (i.e., muscles hypotrophy, sensory and motor deficits), by a direct cord compression or the associated syrinx [1, 21, 24], as well as otoneurological deficits (e.g., dizziness, disequilibrium, sensations of alteration in ear pressure, hypoacusia or hyperacusia, nystagmus, oscillopsia). At least 2 among clinical criteria are enough to define a “symptomatic Chiari” [21].
Visual symptoms had no general consensus from the experts’ jury, as well as controversial data are reported in literature. Transient visual symptoms (spark photopsias, visual blurring, diplopia, or transient visual field deficits) are described in 33% of 364 symptomatic patients by Milhorat et al. [1], but only in 6% of symptomatic CM1 described in a larger, prospective, single-center cohort of 600 adults [24].
Scoliosis was included in the clinical definition of Chiari syndrome, although the experts considered it as an “optional” criterion; in fact, in a literature meta-analysis, the incidence of neuraxial abnormalities among patients with idiopathic scoliosis was about 8%, of which 35% Syr, 28% CM1 with Syr, and 25% isolated CM1 [25].
Syringomyelia-syringobulbia refers to a longitudinally oriented fluid-filled cavity within the spinal cord or in the brainstem; syringobulbia (SB) usually presents on MRI as a one-side lesion, mostly combined with Syr (cervical, cervicothoracic, or holochord) and only in 9.4% without Syr. SB is a very rare entity in adults (1%), closely associated with CM1 [2]; it is often clinically characterized by an abrupt onset of symptoms due to brainstem involvement. Because of the rarity of SB, its manifestations, treatment methods, and long-term prognosis are still not established [26].
The diagnosis of Syr-SB (“clinically defined”) is attributable by neurologists or neurosurgeons to the presence of syrinx/syringobulbia at MRI in addition to spinal/bulbar signs related to the syrinx level.
Hydromyelia or central canal dilatation (H-CCD) is an intramedullary, centrally located, non-enhancing, slit-like cavitation, often localized within a short-segment of the spinal cord and occurring in a non-enlarged or only slightly enlarged spinal cord (“idiopathic localized hydromyelia”) not associated with clinical symptoms. Patients with H-CCD clinically present without neurological deficits, despite often reporting unspecific pain syndromes; they lack electrophysiological alterations and progressive signs/symptoms specifically related to the spinal cord [27, 28].
To date, there is no generally recognized pathophysiological concept of the development of Syr. There are numerous assumptions, and the theories suggested by W. Gardner, B. Williams, and E. Oldfield are the most widely accepted. It is likely that the acquired Syr is a universal response of the nervous tissue of the spinal cord to the obstruction of CSF circulation. According to the standard classification, it can be associated with almost any spinal pathology: abnormalities of the cranio-vertebral junction (CVJ); compressions/arachnoiditis due to trauma (post-traumatic Syr, PTS); infectious processes; tumors and arachnoid cysts; stenotic degenerative-dystrophic diseases and deformities of the spine; demyelinating and autoimmune diseases; non-traumatic SAH [8].
Section 2a: Planning for CM1in adults: surgical indications and follow-up
The results are summarized in Table 2.
The Jury expressed an impressive complete agreement about the indication for surgery in symptomatic CM1-Syr complex and the abstention from operating in asymptomatic isolated CM1.
In isolated CM1, surgery is indicated in case of typical, “cough” headache together with auditory/cerebellar/bulbar/spinal signs at neurological examination, outlining the symptomatic CM1 or “Chiari syndrome” [2]. In CM1 with Syr (CM1-A), with or without CS, surgery is indicated, especially in young people, in case of (1) holocord Syr; (2) evolutionary trend (clinical/MRI worsening); (3) central syringe with Vaquero Index >0.5 or eccentric syringe; and (4) Syr-SB, as shown in Table 2.
Although the experts agreed that surgery is decided mainly basing on clinical backgrounds, related to the progression of the neurological symptoms and signs, in asymptomatic CM1-Syr complex, some instrumental diagnostic data are considered useful to support the surgical making plan. In primis, a whole neuraxis MRI to study the Syr features the following: the number of levels in the cervico-dorsal spinal cord; the syrinx size, by the syrinx/canal index (Vaquero Index), as the indirect value of the syrinx diameter and intramedullary tension [29]; the “atypical” cavity morphology, i.e., eccentric syrinx, independently from the level and size, because of its negative prognostic value in terms of clinical deterioration.
Neurophysiological studies (evoked potentials, polysomnography) are also considered useful subclinical markers in the diagnostic phase both in CM1-A and in CM1-B or in the “waiting and see” monitoring in asymptomatic or mild CM1 patients, with an agreement higher in CM1 with Syr, more in the follow-up than in the diagnosis. Somato-sensory evoked potentials (SSEPs) and brainstem auditory evoked potentials (BAEPs) were altered (43.5% and 38.5% respectively) in a CM1 cohort of 200 adults; these neurophysiological abnormalities could help in establishing objective evidence of subclinical dysfunctions that may indicate a need for surgery or to follow up further progression [30]. In recent prospective studies, polysomnographic alterations were reported in 22–50% of symptomatic CM1, mostly adults, involving a predominance of obstructive events as well as poor sleep efficiency and quality [24, 31]; central sleep apnea syndromes (CSAS) were evidenced in 5–8% by polysomnography, with the same frequency reported in a large pediatric study [32].
Section 2b: Surgery for CM1 in adults: techniques
The results are summarized in Table 3.
The accurate selection of CM1 adults eligible for intervention described in the previous sections was the key to perform a successful surgery. In the same way, we asked the experts to clarify the technical details indicated for the characteristics of each patient.
The Jury concluded unanimously that foramen magnum decompression (FMD) is the shared procedure for CM1 in adults, in the absence of hydrocephalus [33–37]. No alternative surgical approach was considered evaluable, according to the Jury’s experience; more in specific, during the Conference, the panel excluded any role of filum terminale sectioning to treat patients with CM1, as also reported in a recent systematic review [38].
FMD can be performed alone (posterior fossa decompression (PFD) or associated with duraplasty (PFDD) and/or tonsil resection (PFDRT). In children, the bone decompression alone, firstly in the case of CM1 with low symptoms or without Syr, could be indicated [39]. There are some meta-analyses [34, 40, 41] addressing the dualism between PFD and PFDD in the adults or mixed series as well as in recent comparative study [42] relating PFDD versus PFDRT. The conclusions of these papers, with all the limitations due to the lack of randomization, low numbers, and short follow-up, are that the more aggressive is the surgery, the longer is the operating time, the higher are the complication rates (the CSF leakage–related ones for PFDD, neurological symptoms for PFDRT), but the higher the efficacy of surgery on symptoms and even more on Syr. And for these reasons, PFDD is preferable for adult CM1 with Syr. Accordingly, the agreement of the panelist for PFDD in adults was complete (100%) in the case of CM1 with Syr; a final agreement was found also for PFDD in isolated CM1, but just 75% because of the risk of duraplasty.
A high agreement (81.3%) was reached about the technical details about the extension of the PFD, which should be wide enough on the foramen, but not too extended to avoid cerebellar sliding [43]; it should always include C1 laminectomy, but never be extended to C2 for the risk of CVJ instability. In the case of duraplasty, in CM1 without arachnoiditis is indicated to preserve the arachnoid membrane to avoid CSF leakage and arachnoid scarring.
For a higher majority (87.5%), the subpial coagulation of the tonsils should be limited to very low tonsillar ectopia (below C2) and/or recurrent Syr, since this maneuver adds some morbidity other than a risk of arachnoid scarring. Despite their widespread use [44], the artificial grafts were rejected by the majority of the panelists (81.3%) in favor of autologous grafts and allografts. Many panelists presenting their series confirmed the higher risk of foreign body reaction and consequent arachnoiditis due to artificial duras. There was high accordance (93.8%) also on the need for waterproof closure of the duraplasty with non-resorbable stitches. In fact, CSF leakage and collections represent one of the main causes of surgical failure and reoperations [45].
Section 2c: Surgery for CM1 in adults: outcomes, failure, re-intervention
The results are summarized in Table 4.
The outcome measures of FMD efficacy are still a matter of debate, with some standardized assessment scales proposed [46, 47], but up to now, there are no shared, standardized assessment scales to guide clinical outcome and additional research using appropriate study designs is required for improving treatment options in CM1 and Syr [48].
The panel tried to elaborate a commune evaluation protocol. After an in-depth discussion on the timing, they concluded that an operated symptomatic CM1 is expected to solve symptoms within 12 months after surgery; conversely, it is considered a clinical failure, while the permanence of Syr and unchanged low-lying tonsils for more than 24 months is defined as a radiological failure. In case of successful surgery, an accord was reached to perform the follow-up by complete neuraxis MRI for at least 10 years.
Then, the Jury focused on the main causes of failure, whose recognition is basilar for appropriate treatment. Inadequate bone decompression, associated arachnoiditis, and CVJ instability deserve quite different approaches.
Moreover, FMD for CM1 is a procedure that involves risks, many related to the CSF leak in the intradural procedure, causing roughly 2/3 of the reoperations, as reported in a recent large multicenter study [45]; in this study, 6.8% of 672 CM1 adults needed a reoperation. Besides an inadequate technique of duraplasty, unrecognized causes for ICP, such as IIH, hydrocephalus, or associated craniosynostosis, are factors predisposing to CSF leaks. An accurate preoperative evaluation and a treatment addressed to the cause of ICP before or rather FMD are their best prevention, and their recognition and treatment are the best strategies to overcome failures.
Independently by its cause, which involves its decisive way of treatment, CSF leaks are considered by the Jury a worrying complication, deserving prompt treatment (85%) to avoid infections and arachnoiditis in all cases, except asymptomatic not-growing CSF collections. CSF leaks may also cause iatrogenic hypotension with or without subdural collections, a complication hard to be treated, as recently described [49, 50].
The percentage of patients seeking an early revaluation for persistent symptoms (mostly headache) is recently reported as significant (25%) [51]. The Jury agreed that in case of clinical or radiological failure, considered respectively as persistence of symptoms for >6 months (83%) and of Syr and/or tonsils descent for >12 months (85%), reoperation should be performed, addressing to the specific cause of failure.
Despite the incidence of persistent/residual Syr reported in a literature review [52] being not insignificant (6.7%, ranging between 0 and 22%), the indications about its treatment are lacking. So, the experts made the evaluable attempt of classifying the main causes of failures, together with their own diagnostic tool and specific treatment. Firstly, 3D CT diagnoses the incomplete foraminal decompression, needing bone erosion widening (81.5%). Then, CISS and flow MRI detect posterior fossa arachnoiditis, needing adhesiolysis and possibly tonsil resection (88.5%); this is the most frequent cause of failure, as reported by Klekamp [53] and recently by Silva [54]. Finally, the unrecognized CVJ instability, which may be alerted postoperatively by a C1–C2 facet malalignment [55], is diagnosed by dynamic study and treated by CVJ fixation [56]. Because of the reported unexceptional results of the Syr shunting procedures [57], the Jury agreed (87.5%) that they are indicated just in case of failure of cause-addressed reoperations, as for isolated symptomatic Syr.
Section 3: Isolated syringomyelia in adults: differential diagnosis, surgical indications, and techniques
The results are summarized in Table 5.
To date, there are no studies on the treatments of isolated Syr above the third level of evidence and, therefore, there are no guidelines for surgical treatment of this pathology. Fragmentary knowledge of the etiology and pathogenesis of this kind of Syr (no-CM1 associated) is in turn responsible for the lack of effective (etiologic or pathogenic) treatment. Surgery should be targeted at the underlying disease. The high risk of recurrence suggests that a patient with Syr should be under constant surveillance: approximately one-half of the patients require reoperation in the future regardless of the type of surgical procedure [58].
For these reasons, the Consensus Conference tried to share the few cornerstones on this topic, in an attempt to obtain some clues on Syr knowledge. The Jury expressed a complete agreement (100%) on the need for a whole, accurate spinal cord MRI in order to find the cause of isolated Syr, such as dysraphism or arachnoidal cysts. MRI must be completed with sequence after gadolinium injection to exclude spinal cord tumor [59]. The need for dynamic studies in case of suspected CVJ instability was reaffirmed (88.9%).
A high rate of consensus (96%) was achieved on a conservative attitude for asymptomatic, isolated, and stable Syr that should be followed up, clinically and radiologically [60].
In post-traumatic Syr (PTS), according to the literature [61], the consensus panel gave a strong recommendation (92.6%) for surgical intervention in the setting of motor neurologic deterioration as a consequence of PTS and a weak recommendation (81.5%) against surgical intervention for patients developing sensory loss/pain syndrome or for asymptomatic but expanding syrinx. These last patients do not require surgery and should be followed by MRI every 12 months. To date, no satisfactory standard treatment for PTS exists; indeed, a recent literature review shows similar outcomes, regardless of the treatment modality: the preferred methods of surgery are arachnoid lysis (48%) and syrinx drainage (31%). PTS remains a neurosurgical challenge; there is no satisfactory standard treatment even if PTS is diagnosed in its early stages of evolution [62–64].
There was a complete agreement (100%) that Syr associated with spinal dysraphism should be treated prophylactically by de-tethering, and this statement is reinforced by the reported data that Syr increases the risk of acute deterioration [65]. A high accord (94%) was expressed that Syr due to spinal cord tumor may be successfully treated simply by tumor excision. The panel suggests (87.5%) to treat evolving Syr resulting from post-traumatic or post-surgical arachnoiditis by the lysis of the scars, in accord with literature [63]; in the case of isolated Syr, surgery is supported by the use of intraoperative monitoring to prevent surgical-related damage in all these challenging operations, such as de-tethering procedures [66], myelotomy [67], and/or tumor removal [68].
The Jury agreed (87.5%) that spino-peritoneal, spino-subarachnoidal, or spino-pleural shunt must be reserved for the few cases when de-tethering, tumor removal, or adhesiolysis has failed [64], because of its high rate of delayed failures, despite an initial good response [57].
Section 4: Specific conditions related to CVJ Malformations: surgical options
The results are summarized in Table 6.
Cranio-vertebral junction (CVJ) instability is defined as a mobile dislocation between C0, C1, and C2 leading to neuroaxial compression, neurological deficits, progressive deformity, or structural pain. Any radiological measurements and criteria have been proposed or used in the diagnosis of CVJ instability. The consensus statement on basilar invagination and CVJ instability [69] included three metrics which may be useful in the identification of CCI and basilar invagination: the clivo-axial angle (angle between the clivus line and the posterior axial line, equal or less than 135 degrees), the Harris measurement (distance from the basion to the posterior axial line equal or greater than 9 mm), and the Grabb-Oakes method (draw a line from the basion to the posterior inferior edge of the C2 vertebra greater than 9 mm). A wide consensus was achieved for radiological assessment in order to define CVJ instability (94%); the standard diagnostic workup for CVJ instability in CM should include (other than MRI) dynamic X-rays plus dynamic CT scan with 2 and 3D reconstructions [70].
Regarding the treatment, the Jury concluded (88.2%) that only symptomatic patients presenting with CM1.5 associated with basilar invagination or basilar impression need to be treated.
CVJ fixation has no indication if there is no documented instability (100% of agreement). When there is no instability, indeed, in symptomatic patients, a posterior reduction is attempted first and, if failed, the adjunctive surgical option is anterior decompression [71, 72]. In these instances (CM1 with symptomatic basilar invagination without atlanto-axial instability), even FMD has been proved to be successful [73]. On the other hand, the surgical option for CM1.5 patients with CVJ instability and related symptoms is represented by CVJ fixation, with or without FMD [74].
Fixations by C0–C3 or C1–C2 in CM patient with CVJ instability should be decided on the basis of local anatomy; in particular, for C1–C2 fixation, radiological preoperative evaluations (on the vertebral artery course or the C2 isthmus diameter) are mandatory to identify the best approach [75].
Conclusions
This study describes the first systematic consensus process on Chiari and syringomyelia in adults; it was fruitful with a total of 63 statements agreed. The final document, shared at the international level by experts together with patient representatives, is the result of a huge, collaborative, and multidisciplinary work project; it may provide a useful background for future international guidelines and common research platforms.
Strong recommendations in adults, including the statements with the highest agreement (95–100%), are summarized as follows:
1. CM1 should be differentiated from cerebellar tonsil herniation secondary to space-occupying lesions (hydrocephalus, arachnoid cysts, brain tumors) and termed “acquired tonsillar ectopia.”
2. Syringomyelia-syringobulbia is defined by the presence of syrinx/syringobulbia at MRI; for a clinical definition, spinal/bulbar signs related to the syrinx level are mandatory.
3. False tonsil descent due to intracranial hypertension must be excluded by clinical pattern, fundoscopy, and MRI pattern, completed with venous angio-MRI; direct ICP monitoring could be indicated in selected cases.
4. In symptomatic CM1 without Syr, surgery is indicated with typical headache and auditory/cerebellar/bulbar/spinal signs.
5. In CM1 with Syr, surgery is indicated for holocord Syr, clinical/MRI worsening, central syringe, and Vaquero Index >0.5 or eccentric syringe, syringomyelia-syringobulbia with spinal/bulbar signs.
6. In CM1 with Syr, foramen magnum decompression with duraplasty is the best technique.
7. In adults with isolated Syr, a painstaking diagnostic assessment should include: whole neuraxis MRI to diagnose an associated dysraphism (tethering of the medulla at any level due to split cord malformation, limited dorsal myeloschisis, retained medullary cord, terminal myelocystocele, conus lipomas, thickened and fatty filum with a conus below L3, so defined “low-lying conus”); contrast-enhanced MRI to diagnose spinal cord tumors.
8. In the case of Syr associated with dysraphism, a de-tethering procedure is indicated.
9. In asymptomatic isolated Syr, a follow-up, clinical and MRI, is indicated.
10. CVJ fixation is not indicated in CM1 without a documented CVJ instability.
Change history
17 November 2021
A Correction to this paper has been published: https://doi.org/10.1007/s10072-021-05724-y
References
Milhorat TH, Chou MW, Trinidad EM, Kula RW, Mandell M, Wolpert C, Speer MC (1999) Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients. Neurosurgery 44(5):1005–1017
Ciaramitaro P, Garbossa D, Peretta P, Piatelli G, Massimi L, Valentini L, Migliaretti G, Baldovino S, Roccatello D, Kodra Y, Taruscio D, Interregional Chiari and Syringomyelia Consortium on behalf of the Interregional Chiari and Syringomyelia Consortium (2020) Syringomyelia and Chiari Syndrome Registry: advances in epidemiology, clinical phenotypes and natural history based on a North Western Italy cohort. Ann Ist Super Sanita 56(1):48–58
Kurland LT (1958) Descriptive epidemiology of selected neurologic and myopathic disorders with a particular refrence to a survey in Rochester, Minnesota. J Chronic Dis 8:378–415
Brewis M, Poskanzer DC, Rolland C et al (1966) Neurological diseases in an English city. Acta Neurol 42(S24):1–89
Gudmundsson KR (1968) The prevalence of some neurological diseases in Iceland. Acta Neurol Scand 44:57–69
Brickell KL, Anderson NE, Charleston AJ, Hope JK, Bok AP, Barber PA (2006) Ethnic differences in syringomyelia in New Zealand. J Neurol Neurosurg Psychiatry 77:989–991
Sakushima K, Tsuboi S, Yabe I, Hida K, Terae S, Uehara R, Nakano I, Sasaki H (2012) Nationwide survey on the epidemiology of syringomyelia in Japan. J Neurol Sci 313:147–152
Klimov VS, Gulay YU, Evsyukov AV, Moysak GI (2017) Syringosubarachnoid shunting in treatment of syringomyelia: a literature review and a clinical case report. Burdenko’s Journal of Neurosurgery 3:22–29
Ciaramitaro P, Baldovino S, Roccatello D et al (2011) Chiari and Syringomyelia Consortium: a model of multidisciplinary and sharing path for rare diseases. Neurol Sci 32(Suppl 3):S271–S272
Consensus Conference on Chiari Malformation (2009) Neurol Sci 2011; 32 (S3)
Michael A, Erio Z (1996) Gazing into the oracle: the Delphi method and its application to social policy and public health. Kingsley Publishers, London
Chiari H (1987) Concerning alterations in the cerebellum resulting from cerebral hydrocephalus (1891). Pediatr Neurosci 13:3–8
Chiari H (1896) Über veränderungen des Kleinhirns, des Pons un der Medulla Oblongata in folge von congenitaler Hydrocephalie des Grosshirns. Denkschr Akad Wiss Wien 63:71–116
Chiari H (1891) Über Veränderungen des Kleinhirns Infolge von Hydrocephalie des Grosshirns. Dtsch Med Wochenschr 17:1172–1175
Tubbs RS, Elton S, Grabb P, Dockery SE, Bartolucci AA, Oakes WJ (2001) Analysis of the posterior fossa in children with the Chiari 0 malformation. Neurosurgery 48:1050–1055
Tubbs RS, Iskandar BJ, Bartolucci AA, Oakes WJ (2004) A critical analysis of the Chiari 1.5 malformation. J Neurosurg 101:179–183
Iskandar BJ, Hedlund GL, Grabb PA, Oakes WJ (1998) The resolution of syringohydromyelia without hindbrain herniation after posterior fossa decompression. J Neurosurg 89:212–216
Kyoshima K, Kuroyanagi T, Oya F, Kamijo Y, El-Noamany H, Kobayashi S (2002) Syringomyelia without hindbrain herniation: tight cisterna magna. Report of four cases and a review of the literature. J Neurosurg 96:239–249
Isik N, Elmaci I, Kaksi M, Gokben B, Isik N, Celik M (2011) A new entity: Chiari zero malformation and its surgical method. Turk Neurosurg 21:264–268
Wang J, Alotaibi NM, Samuel N, Ibrahim GM, Fallah A, Cusimano MD (2017) Acquired Chiari malformation and syringomyelia secondary to space-occupying lesions: A Systematic Review. World Neurosurg 98:800–808
International Headache Society (2018) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 38(1):1–211
Urbizu A, Poca M-A, Vidal X, Rovira A, Sahuquillo J, Macaya A (2014) MRI-based morphometric analysis of posterior cranial fossa in the diagnosis of Chiari malformation type I. J Neuroimaging 24(3):250–256
Taylor RF, Larkins MV (2002) Headache and Chiari I malformation: clinical presentation, diagnosis and controversies in management. Curr Pain Headache Rep 6:331–337
Ciaramitaro P, Garbossa D, Ferraris M (2019) Massaro F (2019) Clinical diagnosis-Part I: what is really caused by Chiari I? Childs Nervous System. Published online 35:1673–1679. https://doi.org/10.1007/s00381-019-04206-z
Faloon M, Sahai N, Pierce TP, Dunn CJ, Sinha K, Hwang KS, Emami A (2018) Incidence of neuraxial abnormalities is approximately 8% among patients with adolescent idiopathic scoliosis: a meta-analysis. Clin Orthop Relat Res 476(7):1506–1513
Shen J, Shen J, Huang K, Wu Y, Pan J, Zhan R (2019) Syringobulbia in patients with Chiari malformation type i: a systematic review. Biomed Res Int: 4829102. Published online 2019 Mar 19. 2019:1–8. https://doi.org/10.1155/2019/4829102
Victor M, Ropper HA (2002) Adams &Victor’s: principles of neurology. McGraw Hill
Roser F, Ebner FH, Sixt C, Hagen JM, Tatagiba MS (2010) Defining the line between hydromyelia and syringomyelia. A differentiation is possible based on electrophysiological and magnetic resonance imaging studies. Acta Neurochir 152:213–219
Vaquero J, Martinez R, Arias A (1990) Syringomyela-Chiari complex: magnetic resonance imaging and clinical evaluation of surgical treatment. J Neurosurg 73(1):64–68
Moncho D, Poca MA, Minoves T, Ferrè A, CanasV SJ (2016) Are evoked potentials clinically useful in the study of patients with Chiari malformation type 1? J Neurosurg 15:95–108
Ferrèa PM, de la Calzada MD, Moncho D, Romero O, Sampol G, Sahuquillo J (2017) Sleep-related breathing disorders in Chiari malformation type 1: a prospective study of 90 patients. Sleep Jun 1:40(6). https://doi.org/10.1093/sleep/zsx069
Tubbs RS, Beckman J, Naftel RP, Chern JJ, Wellons JC, Rozzelle CJ, Blount JP, Oakes WJ (2011) Institutional experience with 500 cases of surgically treated pediatric Chiari malformation type I. J Neurosurg Pediatr 7(3):248–256
Siasios J, Kapsalaki E, Fountas K (2012) Surgical management of patients with Chiari I malfomation. Int J Pediatr:640127 Published online 2012 Jun 28. https://doi.org/10.1155/2012/640127
Förander P, Sjåvik K, Solheim O, Riphagen I, Gulati S, Salvesen Ø, Jakolac AS (2014) The case for duraplasty in adults undergoing posterior fossa decompression for Chiari I malformation: a systematic review and meta-analysis of observational studies. Clin Neurol Neurosurg 125:58–64
Zhao JL, Li MH, Wang CL, Meng W (2016) A systematic review of Chiari I malformation: techniques and outcomes. World Neurosurg 88:7–14. https://doi.org/10.1016/j.wneu.2015.11.087
Hao X, LinYang C, Rui H, Chang G, Ting L (2017) Posterior fossa decompression with and without duraplasty for the treatment of Chiari malformation type I: a systematic review and meta-analysis. Neurosurg Rev 40:213–221
Langbridge B, Phillips E, Choi D (2017) Chiari malformation type 1: a systematic review of natural history and conservative management. World Neurosurgery 104:213–219
Milano JB, Barcelos ACES, Onishi FJ, Daniel JW, Botelho RV, Dantas FR, Neto ER, de Freitas Bertolini E, Mudo ML, Brock RS, de Oliveira RS, Joaquim AF (2020) The effect of filum terminale sectioning for Chiari 1 malformation treatment: systematic review. Neurol Sci 41(2):249–256
Massimi L, Novegno F, Rocco D (2011) C. Chiari type I malformation in children. Adv Tech Stand Neurosurg 37:143–211
Xu H, Chu L, He R, Ge C, Lei T (2017) Posterior fossa decompression with and without duraplasty for the treatment of Chiari malformation type I-a systematic review and meta-analysis. Neurosurg Rev 40:213–221
Lin W, Duan G, Xie J, Shao J, Wang Z, Jiao B (2018) Comparison of results between posterior fossa decompression with and without duraplasty for the surgical treatment of Chiari malformation type I: a systematic review and meta-analysis. World Neurosurg 110:460–474
Jia C, Li H, Wu J et al (2019) Comparison decompression by duraplasty or cerebellar tonsillectomy for Chiari malformation-I complicated with syringomyelia. Clin Neurol Neurosurg 176:1–7. https://doi.org/10.1016/j.clineuro.2018.11.008
Zhang Y, Zhang N, Qiu H, Zhou J, Li P, Ren M, Shen G, Chen L, Zhou C, Yang D, Liu Y, Mao Y, Gu X, Zhao Y (2011) An efficacy analysis of posterior fossa decompression techniques in the treatment of Chiari malformation with associated syringomyelia. J Clin Neurosci 18:1346–1349
Williams LE, Vannemreddy PS, Watson KS et al (2013) The need in dural graft suturing in Chiari I malformation decompression: a prospective, single-bind, randomized trial comparing sutured and sutureless duraplasty materials. Surg Neurol Int 4:26
Bhimani AD, Esfahani DR, Denyer S, Chiu RG, Rosenberg D, Barks AL, Arnone GD, Mehta AI (2018) Adult Chiari I malformations: an analysis on surgical risk factors and complications using an International Database. World Neurosurg 115:e490–e500
Aliaga L, Hekman KE, Yassari R, Straus D, Luther G, Chen J, Sampat A, Frim D (2012) A novel scoring system for assessing Chiari malformation type I treatment outcomes. Neurosurgery 70:656–665
Klekamp J, Samii M (1993) Introduction of a score system for the clinical evaluation of patients with spinal processes. Acta Neurochir 123:221–223
Greenberg JK, Milner E, Yarbrough CK, Lipsey K, Piccirillo JF, Smyth MD, Park TS, Limbrick DD (2015) Outcome methods used in clinical studies of Chiari malformation type I: a systematic review. J Neurosurg 122(2):262–272. https://doi.org/10.3171/2014.9.JNS14406
Prasad GK et al (2016) Coexistent supratentorial and infratentorial subdural hygromas with hydrocephalus after Chiari decompression surgery: review of literature. World Neurosurg 93:208–214
Rossini Z, Milani D, Costa F, Castellani C, Lasio G, Fornari M (2017) Subdural fluid collection and hydrocephalus after foramen magnum decompression for Chiari malformation type I: management algorithm of a rare complicatio. World Neurosurg 106:1057.e9–1057.e15. https://doi.org/10.1016/j.wneu.2017.07.112
Feghali J, Marinaro E, Yangiran X et al (2020) Emergency department visits following suboccipital decompression for adult Chiari malformation type I. World Neurosurg 144:e789–e796
James M, Schuster JM, Zhang F, Norvell DC (2013) Hermsmeyer JT (2013), Persistent/recurrent syringomyelia after chiari decompression—natural history and management strategies: a systematic review. Evid Based Spine Care J 4:116–125
Klekamp J (2012) Neurological deterioration after foramen magnum decompression for Chiari malformation type I: old or new pathology? J Neurosurg Pediatric 10(6):538–547. https://doi.org/10.3171/2012.9.PEDS12110
Silva A, Thanabalasundaram G, Wilkinson B, Tsermoulas G, Flint G (2020) Experience with revision craniovertebral decompression in adult patients with Chiari malformation type 1, with or without syringomyelia. British J Neurosurg DOI:1–6. https://doi.org/10.1080/02688697.2020.1823935
Loe ML, Vivas-Buitrago T, Domingo RA et al (2020) Prognostic significance of C1–C2 facet malalignment after surgical decompression in adult Chiari malformation type I: a pilot study based on the Chicago Chiari Outcome Scale. J Neurosurg Spine 16:1–7
Du YQ, Qiao GY, Yin YH, Li T, Yu XG (2020) Posterior atlantoaxial facet joint reduction, fixation and fusion as revision surgery for failed suboccipital decompression in patients with basilar invagination and atlantoaxial dislocation: operative nuances, challenges and outcomes. Clin Neurol Neurosurg 194:105793
Soleman J, Roth G, Bartoli A et al (2017) Syringo-subarachnoid shunt for the treatment of persistent syringomyelia following decompression in Chiari type I malformation: surgical results. World Neurosurg 108:836–843
Ghobrial GM (2015) Arachnolysis or cerebrospinal fluid diversion for adult-onset syringomyelia? A systematic review of the literature. World Neurosurg 83(5):829–835. https://doi.org/10.1016/j.wneu.2014.06.044
Batzdorf U (2005) Primary spinal syringomyelia. J Neurosurg Spine 3:429–435
Roy AK, Slimack NP, Ganju A (2011) Idiopathic syringomyelia: retrospective case series, comprehensive review, and update on management. Neurosurg Focus 31(6):E15
Bonfield CM, Levi AD, Arnold PM, Okonkwo DO (2010) Surgical management of post traumatic syringomyelia. Spine 35(21S):S245–S258. https://doi.org/10.1097/BRS.0b013e3181f32e9c
Kleindienst A, Laut FM, Roeckelein V, Buchfelder M, Dodoo-Schittko F (2020) Treatment of posttraumatic syringomyelia: evidence from a systematic review. Acta Neurochir (Wien) 1 62(10):2541–2556. https://doi.org/10.1007/s00701-020-04529-w
Klekamp J, Batzdorf U, Samii M, Bothe HW (1997) Treatment of syringomyelia associated with arachnoid scarring caused by arachnoiditis or trauma. J Neurosurg 86:233–240
Cacciola F, Capozza M, Perrini P, Benedetto N, Di Lorenzo N (2009) Syringopleural shunt as a rescue procedure in patients with syringomyelia refractory to restoration of cerebrospinal fluid flow. Neurosurgery 65(3):471–476. https://doi.org/10.1227/01.NEU.0000350871.47574.DE
Massimi L, Dellapepa GM, Tamburrini G, Di Rocco C (2011) Sudden onset of Chiari malformation type I in previously asymptomatic patients. Report of 3 cases. J Neurosurg Pediatrics 8:438–442
Valentini LG, Visintini S, Mendoal C, et al. (2005) The role of intraoperative electromyographic monitoring in lumbosacral lipomas. Operative Neurosurgery 56(ONS Suppl 2):315-323
Prestor B, Benedicic M (2008) Electrophysiologic and clinical data support the use of dorsal root entry zone myelotomy in syringosubarachnoid shunting for syringomyelia. Surgical Neurology 69;466- 473
Verla T, Fridley J, Khan AB et al (2016) Neuromonitoring for intramedullary spinal cord tumor surgery. World Neurosurgery 96:108–116. https://doi.org/10.1016/j.wneu.2016.07.066
Henderson FC, Francomano CA, Koby M et al (2019) Cervical medullary syndrome secondary to craniocervical instability and ventral brainstem compression in hereditary hypermobility connective tissue disorders: 5-year follow-up after craniocervical reduction, fusion, and stabilization. Neurosurg Rev 42(4):915–936. https://doi.org/10.1007/s10143-018-01070-4
El Asri AC, Akhaddar A, Gazzaz M et al (2010) Dynamic CT scan of the craniovertebral junction: a role in the management of os odontoideum. Neurol Neurochir Pol 44(6):603–608
Klekamp J (2015) Chiari I malformation with and without basilar invagination: a comparative study. Neurosurg Focus 38(4):E12
Vitali M, Canevari FR, Cattalani A, Somma T, Grasso VM, Barbanera A (2019) Stability-sparing endoscopic endonasal odontoidectomy in a malformative craniovertebral junction: case report and biomechanical considerations. In: Visocchi M. (eds) New Trends in craniovertebral junction surgery. Acta Neurochir Suppl 125 Springer, Cham
de Oliveira SU, de Oliveira MF, Heringer LC, Santos Barcelos ACE, Vieira Botelho R (2018) The effect of posterior fossa decompression in adult Chiari malformation and basilar invagination: a systematic review and meta-analysis. Neurosurg Rev 41(1):311–321
Goel A, Bhatjiwale M, Desai K (1998) Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg 88(6):962–968
Yeom JS, Buchowski JM, Kim HJ, Chang BS, Lee CK, Riew KD (2013) Risk of vertebral artery injury: comparison between C1–C2 transarticular and C2 pedicle screws. Spine J 13(7):775–785
Acknowledgements
The authors would like also to thank the following Patients’ Associations for their participation and support (in alphabetical order): AICRA for Craniosynostosis (Italy), AISMAC (Italy), APAISER (France), ASAP (USA), Bobby Jones Chiari & Syringomyelia Foundation’s (USA), Deutsche Syringomyelie und Chiari Malformation (Germany), FEMACPA (Spain), National Syringomyelia Association (Bulgaria), SACA (Ireland).
International Experts Jury of the Chiari & Syringomyelia Consensus Conference: list of affiliations
-
Andrea Barbanera, Department of Neurosurgery, “SS Antonio e Biagio e Cesare Arrigo” Hospital, Alessandria, Italy
-
Alessandro Bertuccio, Department of Neurosurgery, “SS Antonio e Biagio e Cesare Arrigo” Hospital, Alessandria, Italy
-
Paolo Bolognese, Chiari Neuosurgical Center, Mount Sinai, South Nassau, Oceanside (NY), US
-
Andrew Brodbelt, Consultant Neurosurgeon, The Walton Centre NHS Foundation Trust, Liverpool, UK
-
Carlo Celada, AISMAC, Italy
-
Luisa Chiapparini, Service of Neuroradiology, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy
-
Palma Ciaramitaro, CRESSC, Department of Neuroscience, AOU Citta’ della Salute e della Scienza di Torino, Torino, Italy
-
Dario Cocito, Istituti Clinici Scientifici Maugeri, Torino, Italy
-
Marcella Curone, Casa di Cura del Policlinico, Igea Headache Center, Milan, Italy
-
Grazia Devigili, Department of Clinical Neuroscience, Fondazione IRCCS Istituto Neurologico Carlo Besta. Milan, Italy
-
Alessandra Erbetta, Service of Neuroradiology, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy
-
Marilena Ferraris, Service of Neuroradiology, Diagnostic Imaging Department, AOU Citta’ della Salute e della Scienza di Torino, Torino, Italy
-
Marika Furlanetto, Department of Neurosurgery, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy
-
Diego Garbossa, Department of Neurosurgery, University of Torino, Torino, Italy
-
Mado Gilanton, APAISER, France
-
George Jallo, Johns Hopkins University Department of Neurosurgery, Johns Hopkins Hospital, Baltimore, MD, US
-
Marieta Karadjova, Neurology Department, University of Sofia, Sofia, Bulgaria
-
Jörg Klekamp, Christliches Krankenhaus Quakenbrück, Department of Neurosurgery, Quakenbrück, Germany
-
Fulvio Massaro, Department of Neurosurgery, University of Torino, Torino, Italy
-
Luca Massimi, Pediatric Neurosurgery, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy
-
Sylvia Morar, Neurosurgery Department, Reference Center Rares Diseases C-MAVEM, CHU Bicetre APHP, Paris, France
-
Fabrice Parker, Neurosurgery Department, Reference Center Rares Diseases C-MAVEM, CHU Bicetre APHP, Paris, France
-
Paola Peretta, Pediatric Neurosurgery, Ospedale Infantile Regina Margherita, AOU Citta’ della Salute e della Scienza di Torino, Torino, Italy
-
Paolo Perrini, Department of Translational Research and of New Surgical and Medical Technologies, University of Pisa, Pisa, Italy
-
Maria Antonia Poca, Neurosurgery and Pediatric Neurosurgery, Vall d’Hebron Hospital Universitari, Neurotrauma and Neurosurgery Research Unit, and Universitat Autònoma de Barcelona, Barcelona, Spain.
-
Juan Sahuquillo, Neurosurgery and Pediatric Neurosurgery, Vall d’Hebron Hospital Universitari, Neurotrauma and Neurosurgery Research Unit, and Universitat Autònoma de Barcelona, Barcelona, Spain.
-
Marcus Stoodley, The Australian School of Advanced Medicine, Macquarie University, NSW 2109, Australia.
-
Giuseppe Talamonti, Department of Neurosurgery, ASST Niguarda, Milan, Italy
-
Fabio Triulzi, Neuroradiology Unit, Fondazione IRCCS Ca Granda Ospedale Maggiore Policlinico, Milan, Italy
-
Maria Consuelo Valentini, Service of Neuroradiology, Diagnostic Imaging Department, AOU Citta’ della Salute e della Scienza di Torino, Torino, Italy
-
Massimiliano Visocchi, Department of Neurosurgery, Catholic University School of Medicine, Rome, Italy
-
Laura Valentini, Department of Neurosurgery, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy
Data and materials availability
Data is available at the reader’s request.
Code availability
Not applicable.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Palma Ciaramitaro, Luca Massimi, Alessandro Bertuccio, Alessandra Solari, Mariangela Farinotti, Paola Peretta, Veronica Saletti, Andrea Barbanera, Diego Garbossa, and Laura Valentini. The first draft of the manuscript was written by Palma Ciaramitaro and Laura Valentini, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The original published online version does not include the full list of authors. The correct author names are given above.
Rights and permissions
About this article
Cite this article
Ciaramitaro, P., Massimi, L., Bertuccio, A. et al. Diagnosis and treatment of Chiari malformation and syringomyelia in adults: international consensus document. Neurol Sci 43, 1327–1342 (2022). https://doi.org/10.1007/s10072-021-05347-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05347-3