Abstract
Background
A thorough observation of the root exit zone (REZ) and secure transposition of the offending arteries is crucial for a successful microvascular decompression (MVD) for hemifacial spasm (HFS). Decompression procedures are not always feasible in a narrow operative field through a retrosigmoid approach. In such instances, extending the craniectomy laterally is useful in accomplishing the procedure safely. This study aims to introduce the benefits of a skull base approach in MVD for HFS.
Methods
The skull base approach was performed in twenty-eight patients among 335 consecutive MVDs for HFS. The site of the neurovascular compression (NVC), the size of the flocculus, and the location of the sigmoid sinus are measured factors in the imaging studies. The indication for a skull base approach is evaluated and verified retrospectively in comparison with the conventional retrosigmoid approach. Operative outcomes and long-term results were analyzed retrospectively.
Results
The extended retrosigmoid approach was used for 27 patients and the retrolabyrinthine presigmoid approach was used in one patient. The measurement value including the site of NVC, the size of the flocculus, and the location of the sigmoid sinus represents well the indication of the skull base approach, which is significantly different from the conventional retrosigmoid approach. The skull base approach is useful for patients with medially located NVC, a large flocculus, or repeat MVD cases. The long-term result demonstrated favorable outcomes in patients with the skull base approach applied.
Conclusions
Preoperative evaluation for lateral expansion of the craniectomy contributes to a safe and secure MVD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Microvascular decompression (MVD) is popularized as a potentially curative treatment for hemifacial spasm (HFS) [1,2,3]. The offending arteries are commonly located on the root exit zone (REZ) of the facial nerve [4]. A secure transposition of the offender can relieve symptoms in most patients [5, 6]. The conventional retrosigmoid approach is commonly adopted to access the cerebellopontine angle, where the medial edge of the sigmoid sinus is exposed, and the dura is reflected along with the edge of the sinus to create an operative corridor [7, 8]. Irrespective of an appropriate retrosigmoid craniectomy, there are some difficult cases in manipulating neurovascular compression (NVC) due to a narrow operative field. In such cases, MVD may fail due to missing the offender or incomplete transposition of the responsible vessels [9]. Manipulating the arteries and cranial nerves in a narrow surgical field carries the risk of serious neurological complications. The surgical corridor is mainly affected by the site of the NVC, the size of the flocculus, and the location of the sigmoid sinus. Obtaining adequate exposure is essential to performing a safe surgery as well as avoiding risks.
Skull base approaches, such as the extended retrosigmoid approach [10,11,12] or the retrolabyrinthine presigmoid approach [13,14,15,16] are used to widen the operative field for medially located cerebellopontine angle lesions. With the extended retrosigmoid approach, the sigmoid sinus is thoroughly skeletonized with partial removal of the presigmoid air cells to retract the dura laterally together with the sigmoid sinus [10, 11]. The presigmoid approach allows observation far laterally with the retrolabyrinthine mastoidectomy to create a surgical corridor [13, 15, 16]. These approaches are rarely discussed in MVD surgery [17, 18]. We have been applying these approaches to patients whose surgical field is assumed to be narrow. The aim of this study is to find an indicator of when to apply a skull base approach by retrospective evaluation of our approach selection.
Methods
Patient cohort
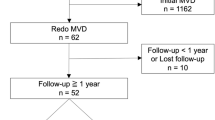
There was a total of 28 patients (8.4%) in whom the extended retrosigmoid approach (n = 27) or the retrolabyrinthine presigmoid approach (n = 1) was applied among 335 consecutive MVDs for HFS from April 2005 to May 2022 (Fig. 1). These approaches were used for patients whose operative field was predicted to be narrow due to a medially located NVC, a large flocculus, or a medially located sigmoid sinus. Patient demographic data was collected from the medical records. There were 19 females (68%) and 9 males (32%), and the mean age at surgery was 54 years, ranging from 23 to 73 years. All patients suffered from typical HFS that affected one side of the face, except for one patient who suffered bilateral HFS due to tortuous vertebral arteries on both sides. The left side was more dominantly affected in 19 patients (68%) than the right side in 9 patients (32%). The duration between the onset and MVD was a median of 5 years and a mean of 5.4 years, ranging from 1 to 18 years. Five patients (18%) had previously failed MVD(s) (Table 1).
Imaging study
All patients were examined preoperatively with computed tomography (CT) and magnetic resonance imaging (MRI) in fast imaging employing steady-state acquisition (FIESTA) (0.8-mm-thick) and contrast-enhanced T1 spoiled gradient recalled (SPGR) (0.6-mm- thick) images. Three-dimensional (3D) images of the operative view were created using the GammaPlan (Elekta, Stockholm, Sweden) by drawing the anatomical structures related to this procedure [19]. CT with bone window images was taken in all patients postoperative day one.
Measurement of the flocculus height and sigmoid-petrous distance
Exposure of the REZ is mainly limited by the site of the NVC, the size of the flocculus, and the location of the sigmoid sinus for the dural opening. The following two measurements were performed on FIESTA or T1 SPGR images for patients who had the skull base approach applied (n = 28) and for those who used the conventional retrosigmoid approach for a reference (n = 290). A line connecting the NVC to the medial edge of the sigmoid sinus is drawn to demonstrate the approach direction. The most distant point on the flocculus from the line is identified, and the perpendicular length to the line is measured as the flocculus height (FH, Fig. 2a). The distance between the posterior border of the sigmoid sinus and the petrous surface is measured at the level of the jugular foramen as the sigmoid-petrous distance (SP, Fig. 2b). The data set is plotted into a coordinate with FH value on the X-axis and SP value on the Y-axis. The standard deviation value of FH and SP among all patients is calculated for each patient. In describing the measured values, P-values were obtained by linear regression test. The statistical test was set to be significant at P < 0.05 (2-sided P-value). SAS software (version 9.4; SAS Institute, Inc., Cary, North Carolina) was used for the statistical analyses.
Measurement method. a The flocculus height (FH) is measured as the perpendicular length from the most distant point on the flocculus to the line (yellow) connecting the NVC (neurovascular compression, white arrowhead) to the medial edge of the sigmoid sinus (red arrowhead). b The sigmoid-petrous length (SP) is measured at the posterior edge of the sigmoid sinus from the line (white) starting from the midpoint on the clivus along with the petrous surface (white arrows) at the level of the jugular foramen (green arrowhead)
Operative technique
All patients are operated in the lateral position with monitoring of auditory brainstem evoked response (ABR) and lateral spread response (LSR). When the amplitude of ABR decreases to less than 50% of baseline, the operative procedures are halted until ABR recovers to more than 70% of baseline for hearing preservation. LSR is used to confirm the adequacy of nerve decompression [20]. Spinal drainage is placed for patients whose subarachnoid space is assumed to be narrow. A skin incision is made at the retro auricular region, and the suboccipital muscles are divided between the occipitomastoid suture and the occipital artery. A craniectomy is performed using either the conventional or the extended retrosigmoid approach except for one patient with a retrolabyrinthine presigmoid approach. In the conventional retrosigmoid approach, the craniectomy is limited to exposing the medial edge of the sigmoid sinus (Fig. 3a). In the extended retrosigmoid approach, the craniectomy is extended to skeletonize the sigmoid sinus toward the occipital condyle. A limited posterior mastoidectomy is added to create room to allow for lateral mobilization of the sinus. (Fig. 3b). Partial far lateral transcondylar drilling to flatten the posterior fossa base allows access toward the REZ beyond the lower cranial nerves [21]. In the retrolabyrinthine presigmoid approach, the lateral aspect of the posterior fossa dura is widely exposed by the mastoidectomy (Fig. 3c). The dural incisions differ in each approach. While the upper end of the incision is placed near the mastoid emissary vein in the conventional retrosigmoid approach, it comes to the transverse-sigmoid junction in the extended retrosigmoid approach. In the presigmoid approach, the dural incision is made on the lateral aspect of the posterior fossa dura along with the anterior edge of the sigmoid sinus toward the jugular bulb (Fig. 3a’, 3b’, 3c’). The different approach direction to the REZ is shown in figure (Fig. 3a’’, 3b’’, 3c’’). After the dural incision, the cerebellar hemisphere is gently retracted from the base and the lateral surface of the posterior fossa. The lower cranial nerves are identified. After elevating the flocculus and the choroid plexus of the lateral recess, the offending vascular loop is usually found above the glossopharyngeal nerve. The REZ of the facial nerve is confirmed with a facial nerve stimulator. The offending vessels are transposed from the REZ with a Teflon sling or bridge as described in our previous report [22]. Fibrin glue is applied to fixate the Teflon sling onto the petrous dura. Adequacy of nerve decompression was confirmed by thorough exposure of the REZ and disappearance or decreased amplitude of LSR [20]. When a normal muscle response wave persists after decompression, no offending vessel on the REZ is re-confirmed using a facial stimulator. The dura is closed with the double collagen matrix grafting (DuraGen®, Integra Lifesciences, Plainsboro, NJ, USA) [23]. The air cells are sealed with small pieces of collagen matrix grafts with fibrin glue. Calcium phosphate paste (BIOPEX-R®, HOYA Technosurgical, Tokyo, Japan) with vancomycin is used for the cranioplasty.
Craniectomy and dural incisions. a, a’, a’’ The conventional retrosigmoid approach. The craniectomy is limited to exposing the medial edge of the sigmoid sinus (a). The dural flap is inverted along with the medial edge of the sigmoid sinus from near the mastoid emissary vein toward the lowest point of the sinus. The reflection of the dural flap does not affect the location of the sigmoid sinus (a’). A schematic axial slice shows the corridor to the NVC through the conventional retrosigmoid approach (a’’). b, b’, b’’ The extended retrosigmoid approach. The craniectomy is extended to skeletonize the sigmoid sinus (b). Inversion of the dural flap together with the sigmoid sinus provides a wider corridor and more medial access than the conventional retrosigmoid approach. The presigmoid mastoid air cells are drilled in cases where more lateral retraction is required. Note that the sigmoid sinus is almost collapsing by the dural retraction (b’). A schematic illustration shows a more lateral approach direction to the NVC (b’’). c, c’, c’’ The retrolabyrinthine presigmoid approach. An extensive mastoidectomy is performed to expose the lateral aspect of the posterior fossa dura. Bone removal reaches the temporal tegmen superiorly and the infrajugular condylar fossa inferiorly. The retrosigmoid area is partially opened to expose the entire sigmoid sinus (c). The dural incision is made on the dura along with the anterior edge of the sigmoid sinus (c’). A schematic axial slice shows a far lateral approach to the NVC (c’’)
Assessment of surgical outcomes
For twenty-eight patients with application of the skull base approach, their postoperative neurological status was assessed either at our clinic, by telephone interviews, or by mailed questionnaires for remote patients. The status of facial spasms was evaluated immediately after surgery, postoperative 1-week, 1-month, 1-year, and the last follow-up visit. Any neurological complications, including delayed facial palsy, post-operative facial weakness, hearing impairment, hoarseness, dysphagia, cerebrospinal fluid leakage, and infectious complications were recorded.
Results
FH and SP measurements
The measurement results from 28 patients with skull base approaches are demonstrated (Table 1). The FH is measured at a median of 11.2 mm and a mean of 10.9 mm, ranging from 4.2 to 14.8 mm. The standard deviation value of FH in the patients with the skull base approach is a median of 62.0 and a mean of 61.1 among all patients. The SP is measured at a median of 6.6 mm and a mean of 6.5 mm, ranging from 0 to 13 mm. The standard deviation value of SP is a median of 52.1 and a mean of 51.6, ranging from 23.3 to 80.0. The standard deviation value is larger in the FH measurement (the median 62.0) than in the SP measurement (the median 52.1). The range is narrower in the FH measurement (40.7–73.1) than in the SP measurement (23.3–80.0).
The graph plotting the values of FH and SP from all patients is shown (Fig. 4). The measurement values from the patients with the skull base approaches are shown in red. The values from the patients with the conventional retrosigmoid approach are indicated in blue. The averages are shown as large dots, respectively. Most patients with the skull base approaches were distributed in the right half of the coordinate which indicates the FH value is larger than those of the conventional retrosigmoid approach. The SP measurement values vary on Y-axis in both approaches.
Distribution of the FH and SP values. The measurement result from all patients is plotted in a coordinate with FH value on the X-axis and SP value on the Y-axis. The small red dots represent the cases with the skull base approaches applied. The small blue dots indicate the cases with the conventional retrosigmoid approach used. The large dots are the average of both approaches. A horizontal line (green) and a vertical line (yellow) indicate the average value of the SP and FH in the conventional retrosigmoid approach. Most cases with the skull base approach (red dots) show a larger FH value than the average of the conventional retrosigmoid approach (yellow line)
Analyses of the standard deviation and chart plotting show that the FH measurement is more consistent with our choice of skull base approach than the SP measurement. Statistical analyses showed the FH measurement has significant differences between both approaches (Fig. 5).
Operative results
The extended retrosigmoid approach was applied in all patients except one (96%). Intraoperative spinal drainage was placed in 3 patients (10.7%) for patients with a narrow subarachnoid space. The REZ of the facial nerve was safely exposed and the offenders were securely transposed in all patients. The offenders involved were either single or multiple vessels. The posterior inferior cerebellar artery (PICA) and the anterior inferior cerebellar artery (AICA) were similarly involved in NVC in 12 patients (43%), respectively, followed by the vertebral artery (VA) and the common trunk of the anterior and inferior cerebellar artery (APC) in 8 patients (29%) each. The transposition was performed using either a Teflon bridge in 13 patients (46%), a Teflon sling in 11 patients (39%), and a Teflon wedge in 4 patients (14%). A decrease in the ABR amplitude was noted in 2 patients (7.1%), which was transient and recovered by the end of surgery (Table 1).
Surgical outcomes and follow-up
The follow-up period was a median of 35 months and a mean of 40 months, ranging from 1 to 151 months. Immediate spasm-free was noted in 23 patients (82%). They decreased to 19 patients (68%) at postoperative 1-week. At the final follow-up, 27 patients (96%) were noted as spasm-free. One patient (3.6%) recurred 2 years after the first MVD, in whom exploratory surgery was conducted and an unrecognized offender was revealed at the mid-cisternal portion. Delayed facial palsy was observed in 2 patients (7.1%), which resolved within a month. Immediate facial weakness was found in one patient (3.6%) who required extensive manipulation during the decompression procedure. No persistent neurological deficit was found postoperatively. One patient had a CSF leak (3.6%). Meningitis was noted in one patient (3.6%). One patient had a wound infection (3.6%) in total (Table 1).
Case presentations
Case 1: The extended retrosigmoid approach for a repeat MVD (Fig. 6)
The extended retrosigmoid approach for the 3rd MVD (49 M, left). a A measurement of FH value. The FH is a perpendicular length measured from the most distant point on the flocculus to the line connecting the NVC and the medial edge of the sigmoid sinus. b An operative photo in the second MVD through the conventional retrosigmoid approach. A Teflon mass inserted in the previous MVD disturbed the access to the NVC. c The extended retrosigmoid approach in the third MVD allowed exposing the NVC. The posterior inferior cerebellar artery (PICA) is compressing the root exit zone (REZ) of the facial nerve. d A postoperative computed tomography (CT) shows extended drilling of the mastoid air cells over the sigmoid sinus
A 49-year-old man suffered from HFS on the left for 5 years. The FH value in this patient was 14.2 (Fig. 6a). His first MVD was operated elsewhere through the conventional retrosigmoid approach with a padding method using Teflon felt. His HFS did not improve and he then was referred to our institution. An MRI revealed a PICA compression remaining on the REZ with deep indentation into the pons. The second MVD was conducted through the more inferior retrosigmoid approach. A Teflon mass was found around the mid-cisternal portion of the facial nerve root. The inserted Teflon felt was partially removed toward the REZ (Fig. 6b). Due to a narrow operative field, the PICA was transposed laterally at the descending portion without confirming the REZ, resulting in a failed second MVD. Postoperative MRI revealed the PICA loop remained on the REZ. Reviewing a 3D image from an operative view suggested that the decompression procedure was difficult through the conventional retrosigmoid approach due to a large flocculus and the medially located PICA loop. The third MVD was conducted 1 week after the second surgery with the extended retrosigmoid approach. The PICA loop compressing the REZ was clearly visualized (Fig. 6c). Decompression was performed safely. The patient became spasm-free immediately after surgery and maintained it for 3 years. No postoperative complication was noted. The postoperative CT shows sufficient drilling of the mastoid air cells over the sigmoid sinus to gain an operative view from the lateral aspect (Fig. 6d).
Case 2: The extended retrosigmoid approach for the first MVD (Fig. 7)
The extended retrosigmoid approach for the 1st MVD (54F, left). a The FH value was 12.4 mm, which predicts a narrow operative field if operated through the conventional retrosigmoid approach. b A three-dimensional (3D) image shows the relationships between the cranial nerves and the offending vessels. The vertebral artery (VA) and the PICA are compressing the pons deeply at the REZ of the facial nerve c An operative photo showing presigmoid bone drilling after skeletonizing the sigmoid sinus (SS, sigmoid sinus; TS, transverse sinus). The presigmoid dura is seen under the suction tube. d The dura is inverted together with the sigmoid sinus colored in purple. The venous flow is confirmed with Doppler ultrasound from the intradural side (red arrow). e An operative photo showing the exposure of the offending vessels and the lower cranial nerves. The NVC on the facial nerve is located on the other side of the offender. f A bone window CT slice shows the extended drilling of the mastoid air cells over the sigmoid sinus along with the lateral wall of the petrous bone
A 54-year-old woman with HFS on the left was operated through the extended retrosigmoid approach for the first MVD based on the FH measurement. The FH value was 12.4, predicting a narrow surgical corridor if operated through the conventional retrosigmoid approach. (Fig. 7a). A 3D image depicted a deeply indented VA and PICA into the pons (Fig. 7b). A partial mastoidectomy with infrajugular drilling was performed after skeletonizing the sigmoid sinus to allow lateral retraction of the sinus (Fig. 7c). A dural incision from the transverse-sigmoid junction toward the inferior point of the sigmoid sinus was made. The dural flap was inverted together with the sigmoid sinus to create a wide operative view from the lateral aspect. The venous flow of the sigmoid sinus was confirmed patent with Doppler ultrasound (Fig. 7d). The offending arteries were clearly exposed (Fig. 7e) and safely transposed using a Teflon bridge. Her facial spasm disappeared immediately after surgery without any complications. No recurrence was noted for 14 months. A postoperative CT shows extensive drilling of the mastoid air cells of the presigmoid area (Fig. 7f).
Case 3: The retrolabyrinthine presigmoid approach for a repeat MVD (Fig. 8)
The retrolabyrinthine presigmoid approach for the 3rd MVD (62F, left). a A 3D image showing the anatomical relationships of the related structures. The REZ is compressed by the PICA loop far medially and rostrally in the deep. Two Teflon felts are inserted around the VA in the previous two failed MVDs. The lower cranial nerves are dislocated with the tortuous VA rostrally. The retrolabyrinthine presigmoid approach was applied. b The NVC was located far medially and rostrally into the pons. The measurement of FH value (14.8 mm) indicates the conventional retrosigmoid approach may cause difficulty in exposing the NVC. c An operative photo after mastoidectomy. The presigmoid dura, the posterior semicircular canal (PSC), and the endolymphatic sac (ES) are exposed. Infrajugular drilling was extended toward the condylar fossa. The retrosigmoid dura is partially exposed to allow medial retraction of the sigmoid sinus. The dural incision is made on the presigmoid dura (red dashed line). d An operative photo after dissecting the previously inserted Teflon felts from the lower cranial nerves. The deeply situated PICA loop is observed compressing the REZ of the facial nerve. e A postoperative CT shows the mastoidectomy reaches the labyrinth
This is the only patient in whom the presigmoid approach was utilized (Fig. 8a). The FH value was 14.8, which was the largest in our series (Fig. 8b). A 62-year-old woman had suffered from severe HFS on the left for 7 years. Her previous two MVDs operated elsewhere resulted in failures due to incomplete decompression through the conventional retrosigmoid approach. Multiple Teflon felts around the lower cranial nerves and the facial vestibulocochlear nerve complex were found on radiological study. The location of NVC by a PICA loop was located far medially on the pons (Fig. 8a). An inferior retrosigmoid craniectomy and limited extreme lateral infrajugular transcondylar exposure (ELITE) approach was performed and the presigmoid dura was exposed toward the jugular bulb (Fig. 8c). Meticulous dissection and removal of Teflon felt from the cranial nerves allowed access to the REZ of the facial nerve through the presigmoid approach (Fig. 8d). The compressing PICA loop was visualized and transposed safely with Teflon slings. Her facial spasm was relieved immediately after surgery without any neurological complications. She maintained spasm-free for 5 years. A postoperative CT shows an extensive mastoidectomy for the retrolabyrinthine presigmoid approach (Fig. 8e).
Discussion
The retrosigmoid approach is generally applied in MVD for HFS [1, 5, 7, 8]. This approach provides a very sufficient operative field to manage almost all patients with HFS. It is rare that the REZ is inaccessible via the retrosigmoid approach except when the NVC is located far medial or rostral due to severe compression by the tortuous arteries [4, 24]. Some variations of the retrosigmoid approach in MVD surgery are reported to minimize cerebellar retraction and obtain sufficient exposure [25,26,27]. Extending the craniectomy inferiorly or laterally contributes to widening the operative corridor, however, the necessity for each patient has not yet been discussed. The significance of this study is to identify the necessity of additional drilling to the lateral before surgery. A larger FH value may predict when to consider the extended retrosigmoid approach.
Despite a variety of approaches in development to access medially located tumors and vascular lesions in skull base, the application of these approaches is rarely discussed in MVD surgery. The location of the REZ is usually accessible via the conventional retrosigmoid approach in most cases [1, 5, 7, 8]. Even in cases with far medially located NVC, the decompression procedures may be quickly accomplished with more retraction of the cerebellum for a limited time. Surgical maneuvers in a narrow operative field, however, involve risks such as cranial nerve or vascular injuries, and failure of MVD [9]. Obtaining a maneuverable operative field is essential to performing a safe and secure MVD. The skull base approaches should be taken into consideration when such operative conditions are predicted. Some authors reported the benefit of either fully endoscopic MVD [28, 29] or simultaneous endoscopic and microscopic visualization in MVD [30]. Endoscopic MVD minimizes the risks of brain retraction and extensive dissection required for microscopic procedures. Using an endoscope has an advantage over a microscope in the visualization of structure and identification of neurovascular conflict. Our simple method to predict a narrow operative field is also useful for considering the application of endoscopic MVD.
A variety of decompression methods for the facial nerve were reported in the literature [31,32,33,34,35,36]. The padding method using a shredded Teflon felt on the REZ to separate the offender was initially introduced [1,2,3]. Later, transposing the offender away from the REZ using a Teflon sling is reported to provide better surgical outcomes than the padding method [37]. While the padding method can be accomplished in a narrow operative field, the transposition technique with a sling requires a wider surgical field to manipulate the involving vessels. Visualizing the REZ and identifying the adjacent structures is the prerequisite for performing this technique. Limited exposure of the sigmoid sinus leaves a ledge of bone which compromises the surgical exposure and requires more cerebellar retraction to expose the REZ [11]. This study demonstrated that some patients could benefit from the skull base approach by widening the operative field, especially for repeat MVD cases.
The indication for a skull base approach should be carefully considered because unnecessary drilling of the mastoid air cells carries surgical risks, such as venous sinus injury, CSF leak, and wound infection [38]. One of the unique risks of the extended retrosigmoid approach is venous sinus occlusion. Tense retraction of the dura may cause sinus occlusion during surgery that may result in fatal sequelae due to venous infarction if it is the dominant side. Intraoperative confirmation of the venous flow using Doppler ultrasound or indocyanine green venography is useful for avoiding sinus occlusion. On the other hand, endoscopic MVD may avoid a mastoidectomy that can put the sigmoid sinus at risk or require more reconstructive steps if it is damaged [28,29,30]. It may also benefit in avoiding CSF leaks. Applying a skull base approach or an endoscopic procedure should be carefully considered based on the surgeon’s experiences and techniques.
This study demonstrated the anatomical diversity of the structures that relate to performing an MVD. Although skilled neurosurgeons may be able to manage HFS patients solely through the retrosigmoid approach, predicting the difficulty of the procedure and considering the additional bone removal to avoid a narrow surgical field contribute to performing a safe MVD, which may be more beneficial for less experienced neurosurgeons. Training on cadaver dissection and being familiar with petrous bone anatomy is necessary to take these approaches into surgical consideration.
Limitations of the present study include those that are inherent to studies of retrospective design with a small number of patients and a relatively short follow-up period. Another limitation is the comparison of two approaches on the same patient is impossible, therefore, the exact benefit of the skull base approach cannot be precisely evaluated. The absolute FH value cannot be generalized because there is an inherent bias in the FH measurement.
Conclusion
A simple preoperative measurement is introduced to evaluate the necessity of expanding a craniectomy laterally to obtain a wider operative field in MVD.
References
Barker FG 2nd, Jannetta PJ, Bissonette DJ, Shields PT, Larkins MV, Jho HD (1995) Microvascular decompression for hemifacial spasm. J Neurosurg 82:201–210
Jannetta PJ (1975) The cause of hemifacial spasm: definitive microsurgical treatment at the brainstem in 31 patients. Trans Sect Otolaryngol Am Acad Ophthalmol Otolaryngol 80:319–322
Jannetta PJ, Abbasy M, Maroon JC, Ramos FM, Albin MS (1977) Etiology and definitive microsurgical treatment of hemifacial spasm. Operative techniques and results in 47 patients. J Neurosurg 47:321–328
Mercier P, Sindou M (2018) The conflicting vessels in hemifacial spasm: literature review and anatomical-surgical implications. Neurochirurgie 64:94–100
Sindou M, Mercier P (2018) Microvascular decompression for hemifacial spasm: Surgical techniques and intraoperative monitoring. Neurochirurgie 64:133–143
Sindou M, Mercier P (2018) Microvascular decompression for hemifacial spasm: outcome on spasm and complications. a review. Neurochirurgie 64:106–116
Ojemann RG (2001) Retrosigmoid approach to acoustic neuroma (vestibular schwannoma). Neurosurgery 48:553–558
Zhang KW, Shun ZT (1995) Microvascular decompression by the retrosigmoid approach for idiopathic hemifacial spasm: experience with 300 cases. Ann Otol Rhinol Laryngol 104:610–612
Bigder MG, Kaufmann AM (2016) Failed microvascular decompression surgery for hemifacial spasm due to persistent neurovascular compression: an analysis of reoperations. J Neurosurg 124:90–95
Liebelt BD, Huang M, Britz GW (2018) A comparison of cerebellar retraction pressures in posterior fossa surgery: extended retrosigmoid versus traditional retrosigmoid approach. World Neurosurg 113:e88–e92
Quiñones-Hinojosa A, Chang EF, Lawton MT (2006) The extended retrosigmoid approach: an alternative to radical cranial base approaches for posterior fossa lesions. Neurosurgery 58:208–214
Raza SM, Quinones-Hinojosa A (2011) The extended retrosigmoid approach for neoplastic lesions in the posterior fossa: technique modification. Neurosurg Rev 34:123–129
Alonso F, Dekker SE, Wright J, Wright C, Alonso A, Carmody M, Tubbs RS, Bambakidis NC (2017) The retrolabyrinthine presigmoid approach to the anterior cerebellopontine region: expanding the limits of trautmann triangle. World Neurosurg 104:180–185
Borghei-Razavi H, Shibao S, Schick U (2015) Anatomical variations of the presigmoid suprabulbar infralabyrinthine approach. Neurosurgery 76:E242-243
Rassi MS, Zamponi JO Jr, Cândido DNC, Oliveira JG, Passos GAR, Borba LAB (2018) Combined presigmoid and retrosigmoid approach to petroclival meningiomas. J Neurol Surg B Skull Base 79:S402–S403
Troude L, Baucher G, Lavieille JP, Roche PH (2021) The presigmoid retrolabyrinthine approach: Technical note. Neurochirurgie 67:503–507
De Ridder D, Menovsky T (2007) Neurovascular compression of the abducent nerve causing abducent palsy treated by microvascular decompression. Case report J Neurosurg 107:1231–1234
Wiet RJ, Schramm DR, Kazan RP (1989) The retrolabyrinthine approach and vascular loop. Laryngoscope 99:1035–1039
Inoue T, Hirai H, Shimizu T, Tsuji M, Shima A, Suzuki F, Matsuda M (2012) Ocular neuromyotonia treated by microvascular decompression: usefulness of preoperative 3D imaging: case report. J Neurosurg 117:1166–1169
Thirumala PD, Altibi AM, Chang R, Saca EE, Iyengar P, Reddy R, Anetakis K, Crammond DJ, Balzer JR, Sekula RF (2020) The utility of intraoperative lateral spread recording in microvascular decompression for hemifacial spasm: a systematic review and meta-analysis. Neurosurgery 87:E473–E484
Mintelis A, Sameshima T, Bulsara KR, Gray L, Friedman AH, Fukushima T (2006) Jugular tubercle: Morphometric analysis and surgical significance. J Neurosurg 105:753–757
Inoue T, Shitara S, Goto Y, Arham A, Prasetya M, Radcliffe L, Fukushima T (2021) Bridge technique for hemifacial spasm with vertebral artery involvement. Acta Neurochir (Wien) 163:3311–3320
Inoue T, Shitara S, Shima A, Goto Y, Fukushima T (2021) Double collagen matrix grafting for dural closure in microvascular decompression: an alternative use of autologous fascial grafting. Acta Neurochir (Wien) 163:2395–2401
Bejjani GK, Sekhar LN (1997) Repositioning of the vertebral artery as treatment for neurovascular compression syndromes. Technical note J Neurosurg 86:728–732
Huang J, Zhan Y, Li Y, Jiang L, Wang K, Wu Z, Xie Y, Shi Q (2021) The efficacy and safety of <2 cm micro-keyhole microvascular decompression for hemifacial spasm. Front Surg 28:685155
Kim EY, Park HS, Kim JJ, Lee SC, Ha CK, Park HC (2001) A more basal approach in microvascular decompression for hemifacial spasm: the para-condylar fossa approach. Acta Neurochir (Wien) 143:141–144
Shimizu K, Matsumoto M, Wada A, Mizutani T (2015) Lateral basal approach with a supine, no-retractor method for microvascular decompression for hemifacial spasm. Acta Neurochir (Wien) 157:803–806
Feng BH, Zhong WX, Li ST, Wang XH (2020) Fully endoscopic microvascular decompression of the hemifacial spasm: our experience. Acta Neurochir (Wien) 162:1081–1087
Flanders TM, Blue R, Roberts S, McShane BJ, Wilent B, Tambi V, Petrov D, Lee JYK (2018) Fully endoscopic microvascular decompression for hemifacial spasm. J Neurosurg 13:813–819
McGahan BG, Albonette-Felicio T, Kreatsoulas DC, Magill ST, Hardesty DA, Prevedello DM (2021) Simultaneous endoscopic and microscopic visualization in microvascular decompression for hemifacial spasm. Oper Neurosurg (Hagerstown) 21:540–548
Attabib N, Kaufmann AM (2007) Use of fenestrated aneurysm clips in microvascular decompression surgery. Technical note and case series. J Neurosurg 106:929–931
Ichikawa T, Agari T, Kurozumi K, Maruo T, Satoh T, Date I (2011) “Double-stick tape” technique for transposition of an offending vessel in microvascular decompression: technical case report. Neurosurgery 68:377–382
Jha RT, Kumar J, Pressman E, Agazzi S (2019) Arterial sling decompression for hemifacial spasm. World Neurosurg 132:134
Kim JY, Jung S, Song TW, Kim IY, Moon KS, Jung TY, Jang WY (2019) The cornerstone technique of microvascular decompression for hemifacial spasm with vertebral artery offender. World Neurosurg 126:e94–e100
Masuoka J, Matsushima T, Kawashima M, Nakahara Y, Funaki T, Mineta T (2011) Stitched sling retraction technique for microvascular decompression: procedures and techniques based on an anatomical viewpoint. Neurosurg Rev 34:373–379
Nonaka Y, Hayashi N, Matsumae M, Fukushima T (2019) Wedge-technique for transposition of the vertebral artery in microvascular decompression for hemifacial spasm: technical nuances and surgical outcomes. Acta Neurochir (Wien) 161:1435–1442
Rawlinson JN, Coakham HB (1988) The treatment of hemifacial spasm by sling retraction. Br J Neurosurg 2:173–178
Lin J, Zhang Y, Peng R, Ji X, Luo G, Luo W, Wang M, Zhu M, Sun X, Zhang Y (2019) Preoperative imaging and microscopic navigation during surgery can avoid unnecessarily opening the mastoid air cells through craniotomy using the retrosigmoid approach. World Neurosurg 121:e15–e21
Acknowledgements
We thank Ms. Satomi Fujimura, Ms. Yasuko Noda, and Ms. Kayoko Kutsuwa for their assistance with data collection and illustrations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
.The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Inoue, T., Goto, Y., Shitara, S. et al. Indication for a skull base approach in microvascular decompression for hemifacial spasm. Acta Neurochir 164, 3235–3246 (2022). https://doi.org/10.1007/s00701-022-05397-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05397-2