Abstract
Approaches to the cerebellar-pontine angle and petroclival region can be challenging due to intervening eloquent neurovascular structures and cerebellar retraction required to view this anatomic compartment with the standard retrosigmoid technique. As previously described [11], the extended retrosigmoid provides additional access to space ventral to the brainstem through mobilization of the sigmoid sinus. We report our further experience and modifications of this approach for neoplastic pathology. The standard craniotomy is utilized, and the burr holes are placed slightly beyond the transverse sinus as well as the transverse–sigmoid junction and down towards the foramen magnum, as low as possible. Another burr hole is placed over the cerebral hemisphere to facilitate the dural dissection below the bone flap and over the transverse and sigmoid sinuses. We then perform a standard retrosigmoid craniotomy with a craniotome and the transverse and sigmoid sinuses are skeletonized. Consequently, the sigmoid sinus can then mobilized anteriorly to provide an unobstructed view in line with the petrous bone, while exposure of the transverse sinus provides access to the tentorium. Fifteen patients (March 2006–July 2008) underwent this approach to manage neoplastic lesions, including five meningiomas, three schwannomas, one epidermoid, and four intra-axial metastatic lesions. The nine extra-axial lesions were predominantly in the cerebellar-pontine angle with extension medial to the seventh/eighth nerve complex to the petroclival region. Gross total resection was obtained in all patients. The primary complication due to the exposure was a clinically asymptomatic sigmoid sinus thrombosis in one patient. Requiring a fundamental change in the management of the venous sinuses, the extended retrosigmoid craniotomy permits mobilization of the sigmoid and transverse sinuses. In this process, the entire cerebellar-pontine angle extending from the tentorium to the foramen magnum can be visualized with minimal cerebellar retraction. This technical modification over the standard retrosigmoid approach may provide a useful advantage to neurosurgeons dealing with these complex lesions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lesions of the cerebellar-pontine angle and petroclival region can be surgically challenging to approach and resect. Whether arising extra-axially or intra-axially, these lesions can be difficult to access due to surrounding vascular and eloquent neural structures (i.e., brain stem) that have zero tolerance for retraction. In addition, the petrous bone anatomically limits access to the ventral most aspect of the brain stem/posterior fossa.
Since its description in the early 1900s, the retrosigmoid craniotomy/craniectomy has been the workhorse of neurosurgeons with regard to dealing with a wide variety of lesions in the posterior fossa. The traditional retrosigmoid approach involves an incision that provides soft tissue exposure from the asterion down inferiorly to the foramen magnum. The craniotomy/craniectomy commences with a burr hole placed at the transverse–sigmoid sinus junction and encompasses bone from just below the transverse sinus to the foramen magnum and extends from just lateral/posterior to the sigmoid sinus to 4 cm posteriorly. This approach typically leaves the major venous sinuses encased in bone, consequently relying on some cerebellar retraction for exposure [12].
Since this classical approach leaves the sinuses untouched with bone limiting the superior and antero-lateral extents of the exposure, its major limitation has been in accessing ventral to the brain stem (i.e., the petroclival suture) and superiorly to the tentorium. Numerous approaches have been developed to address these anatomical limitations. These approaches include anterior petrosectomy, posterior petrosectomy, translabyrinthine, and transcochlear approaches amongst other middle fossa techniques [1–4, 8, 10, 14, 18]. With their unique set of indications, these different approaches have their advantages and limitations. The overwhelming complication noted in these well-described approaches is the risk of cranial nerve injury.
The extended retrosigmoid craniotomy has been previously described in a handful of reports [11, 15–17]. This approach is most notably characterized by bony skeletonization of the sigmoid/transverse sinuses with an additional mastoidectomy. Initially described for acoustic tumors and vestibular neurectomies [15–17], it has also been employed for vascular lesions in the posterior fossa [11]. This technique affords access to regions that are difficult to visualize with the standard retrosigmoid approach. In this report, we describe a modified version of the extended retrosigmoid craniotomy (done primarily with a craniotome) and its use for neoplastic lesions of the cerebellar-pontine angle/petroclival region.
Operative technique
Pre-operative planning
All patients, in addition to standard pre-operative evaluation, undergo magnetic resonance imaging for intra-operative image guidance. Of particular importance to this technique, MR imaging that is performed also includes venography. This is done in order to rule out contralateral sinus occlusion prior to surgical manipulation of the sinus ipsilateral to the approach.
Patient positioning and soft tissue exposure
After induction of general anesthesia, central venous access is obtained and pre-cordial Dopplers are placed for early intra-operative detection of air embolism. In addition, patients with moderate to large extra-axial lesions undergo lumbar drain placement to facilitate intra-operative CSF drainage; drains are removed in the operating room at case completion. A lumbar drain is placed in those patients where (1) large tumors limit early access to the cisterns and (2) there is a small cisterna magna as appreciated on pre-operative MR scans (axial and sagittal slices). The lumbar drain can potentially assist also in the dissection of the dura over the sinus by relaxing the underlying brain. Patients are typically positioned parkbench. The patient’s head is then fixed in a Mayfield clamp, turned towards the contralateral shoulder, and slightly flexed such that the ipsilateral mastoid tip is the highest point in the operative field.
A hair shave is performed to expose the incision and Dandy’s point (for potential intra-operative intraventricular catheter placement). A C-shaped incision is marked from 2 cm superior to the pinna, curving posteriorly and ending two fingerbreadths below the mastoid tip. After incision, a standard retrosigmoid soft tissue dissection is performed—this has been described in detail in previous publications by our group [11]. The dissection is carried out to the extent that the bone is exposed from above the asterion superiorly, to the foramen magnum inferiorly, and from the mastoid process to several centimeters posterior to the sigmoid sinus.
Craniotomy
Bone dissection consists of two conceptual components: (1) standard retrosigmoid craniotomy with skeletonization of the transverse and sigmoid sinuses and (2) limited posterior mastoidectomy (if needed for exposure of the jugular bulb). We prefer to use a craniotome to perform all our posterior fossa craniotomies. Initial burr holes are placed encompassing the transverse sinus but slightly supratentorial as well as encompassing the transverse–sigmoid sinus junction but slightly supratentorial; final burr holes are placed over the sigmoid sinus near its termination at the jugular foramen and another burr hole over the cerebellar hemisphere (Fig. 1). We primarily use a craniotome to skeletonize the sinuses; a cutting burr is used for the limited posterior mastoidectomy. If there are any concerns intra-operatively with skeletonizing the sinuses using a craniotome, then a burr is employed. We then do careful epidural dissection with a penfield 3 instrument in order to separate carefully the dura as well as the transverse and sigmoid sinuses. The initial two cuts are the ones done over the cerebellar hemisphere with the footplate of the craniotome followed by the osteotomy extending along the length of the transverse sinus and the final osteotomy extending just posterior to the sigmoid sinus.
Illustration demonstrating placement of burr holes and use of craniotome to create bone flap and skeletonize the transverse/sigmoid sinuses. Burr holes are placed: (1) at the transverse–sigmoid junction, (2) on the sigmoid sinus towards the jugular bulb, (3) on the transverse sinus towards midline, and (4) over the cerebellar hemisphere
With the final osteotomies described above, the majority of the transverse and the sigmoid sinuses have been skeletonized through the use of the craniotome. As opposed to the other major venous sinuses that can be exposed with the craniotome, the sigmoid sinus has a tortuous course and is covered by compacted bone of variable thickness along the entire length of the sinus. As the sigmoid sinus terminates in its entry into the jugular foramen, its bony roof transitions from a compacted texture to a more trabeculated appearance as the mastoid process commences [9, 13]. While the craniotome can be effectively used to unroof the compacted bone, in order to expose the terminal end of the sigmoid sinus, a limited posterior mastoidectomy must also be done. During this step, the mastoid emissary vein is encountered where hemostasis is obtained with cauterization. The entire extent of this bony ledge is thinned until the sinus is more evident as a blue color visible through a thin eggshell rim of bone. The remaining bone overlying the terminal end of the sigmoid sinus is then removed with a diamond bit to expose the entire sigmoid sinus from its junction with the transverse sinus to the jugular bulb. This skeletonization of the sigmoid sinus entry into the jugular bulb is done selectively for cases located low along the posterior fossa.
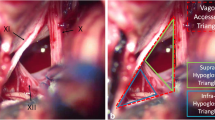
Dural opening
The bony dissection described above exposes the dura over the cerebellar hemisphere in addition to the entire length of the transverse and sigmoid sinuses. In order to take advantage of this bone opening and have access to the cisterna magna and lateralis, a cruciate or c-shaped dural opening is performed (Fig. 2). In the cruciate dural opening, the pedicles of two of the dural flaps are based on the sigmoid and transverse sinuses. The flap based on the sigmoid sinus is hooked with a 4-0 surgilon attached to a clamp in order to provide for dynamic/intermittent retraction. This allows for the sigmoid sinus to be retracted anteriorly in order to provide unobstructed access to cisterna lateralis and the cerebellar-pontine angle. In addition, the flap based on the transverse sinus provides for access to the space between the cerebellum and tentorium.
Closure and reconstruction
The dura is closed with interrupted 4-0 surgilon sutures, and if watertight dural closure cannot be achieved, dural defects are supplemented with DuraGen (Integra, NJ, USA) and Fibrin Glue (Baxter AG, Vienna, Austria). In order to circumvent a potential route of CSF egress, the mastoid air cells are thoroughly waxed. Subsequently, the bone flap is replaced and secured with standard titanium plates and screws. The bony reconstruction is completed with the application of bone cement to the defect overlying the sigmoid sinus and any other palpable gaps only if considered necessary.
Case illustration
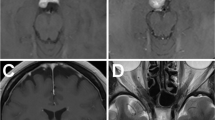
A 34-year-old right-handed female with a history of pseudotumor cerebri presented to our clinic with several months of headaches, vertigo, and diminished hearing on the left with gait imbalance. Pre-operative MRI demonstrated 3 cm × 2.5 × 3.3 cm homogenously contrast enhancing mass in the cerebellar-pontine angle with extension medial to the seventh/eighth nerve complex and slight extension into the internal auditory canal (Fig. 3a). MR venography demonstrated patent transverse/sigmoid sinuses bilaterally. The patient underwent an uneventful left-sided extended retrosigmoid craniotomy with lumbar drain placement and intra-operative neuro-monitoring. Post-operatively the patient was discharged home post-operative day 3 neurologically intact with post-resection imaging that demonstrated complete resection (Fig. 3b). Final pathology was WHO grade I meningioma.
a Pre-operative magnetic resonance imaging (T1-weighted with contrast) for case illustration (see text). Noted is an extra-axial homogeneously enhancing mass along the transverse–sigmoid sinus junction. b Post-operative MR scan from case illustration demonstration complete resection of previously described mass
Results
Between January 2006 and April 2008, we performed the extended retrosigmoid craniotomy on 15 patients with neoplastic lesions (Table 1). Over half of the procedures were done for extra-axial lesions (either meningioma or schwannoma), while the remainder of surgeries were for cerebellar lesions. The extra-axial lesions were primarily lateral to the seventh/eighth nerve complex; there were four patients with tumors primarily medial to the internal auditory canal in the cerebellar-pontine angle–petroclival/prepontine cistern region. For the intra-axial lesions where the extended retrosigmoid was employed, they were most often in the cerebellar hemisphere and came to the surface along the petrosal surface of the cerebellum—hence would have required a fair degree of retraction if a standard approach was utilized.
The most notable complication was sigmoid sinus thrombosis in one patient. This was clinically asymptomatic and discovered on routine post-operative imaging. The thrombus primarily involved the entire extent of the sigmoid sinus but did not extend into the transverse sinus. In a follow-up MRI 6 months later, the sinus had recanalized. Gross total resection (for metastatic lesions) or Simpson grade I/II resection was attained for all tumors.
Discussion
The resection of tumors in the cerebellar-pontine angle can be difficult due to intervening neurovascular structures and the need for cerebellar retraction. Approaches to this anatomical compartment include the standard retrosigmoid craniotomy/craniectomy and translabyrinthine/transcochlear trajectories, and trans-petrosal approaches (anterior and posterior petrosectomy) [1, 3, 5, 10, 17, 18]. Each of these techniques has its own unique set of advantages and disadvantages; for example, the translabyrinthine approach is associated with risk of damage to the hearing apparatus while the transcochlear approach is associated with facial nerve damage. In addition, each has its own set of indications.
We propose that the extended retrosigmoid craniotomy is a safe, simple technique that provides unobstructed access to the cerebellar-pontine angle extending from the tentorium to the foramen magnum. We describe a modification of this approach to a technique we had previously described [11] with the use of a craniotome to skeletonize the transverse and the sigmoid sinuses. Ultimately, in comparison with the standard retrosigmoid approach, this technique requires an adaptation in management of the sigmoid sinus and an understanding of its anatomy. This technique also incorporates a component of posterior petrosal approaches by skeletonizing the sigmoid sinus but does not require as much petrosal drilling (limiting the risk of cranial nerve injury) and a pre-sigmoid dural opening. This technique is efficient and can lead to an expeditious exposure with minimal morbidity in our preliminary experience.
Anatomically, the sigmoid sinus is characterized by a tortuous course distinguishing it from the other venous sinuses. With the traditional retrosigmoid approach and posterior petrosal approaches, the initiation of the sigmoid sinus traditionally has been marked by the asterion. Anatomic studies have disproven the accuracy of this superficial bony landmark [6]; consequently, image guidance has played an increasing role in determining the sigmoid–transverse junction [7]. Formed by the confluence of the transverse sinus with the superior petrosal sinus, from its origination, the sigmoid sinus then changes its vertical trajectory to terminate medial to the mastoid cavity in the jugular foramen. Hence, the more terminal aspect of the sinus is superficially covered by the mastoid process. Consequently, in order to expose the sigmoid sinus in its entirety, a partial posterior mastoidectomy can be performed to expose the sinus as it enters the jugular foramen if this is necessary for low-lying lesions.
In comparison with traditional neurosurgical approaches to the cerebellar-pontine angle, the extended retrosigmoid approach has the added advantage of additional working angle [11]. With this technique, the bony ledge overlying the sigmoid sinus which limits the anterior extent of visualization is removed. In addition, the craniotomy is extended superiorly to the transverse sinus. As a result, the working corridor for the surgeon has now expanded so that anteriorly it is line with the petrous bone and superiorly extends to the cerebellar surface of the tentorium. Subsequently, this approach may reduce the need for cerebellar retraction most especially in tumors that are large or that extend superiorly towards the tentorium.
With exposure and manipulation of the sinus, the surgeon is rewarded by additional working space; however, this comes with the risk of intra-operative venous obstruction. Intra-operatively, one must be aware for signs of venous outflow congestion (i.e., cerebellar edema); under such circumstances, the stay sutures on the sigmoid sinus must be relaxed temporarily. Manipulation of the sinus is further associated with the potential development of venous sinus thrombosis. As evident in our series and previously published reports, the post-operative diagnosis of venous sinus thrombosis is rare.
The primary limitation of this approach is the potential for venous sinus injury. Our experience and previously published literature [11, 15, 16] demonstrates zero incidences of hemorrhagic contusions but one patient with clinically silent but radiographically evident sigmoid sinus thrombosis. As the patient was clinically asymptomatic—indicating adequate venous outflow through the contralateral transverse/sigmoid sinus—the patient was followed up with serial imaging to ensure that the thrombus did not propagate towards the torcula herophili. This risk highlights the importance in obtaining pre-operative MR venography in order to rule out contralateral sinus thrombosis—this would be a relative contraindication to this approach.
Recognizing the potential advantages and limitations of this approach in comparison with other cranial base approaches, we feel that the extended retrosigmoid craniotomy can be utilized to treat (1) extra-axial lesions in the cerebellar-pontine angle that do not extend medial to the trigeminal nerve and (2) intra-axial lesions of the brainstem, cerebellar peduncle, and cerebellar hemisphere that present a surface to the subarachnoid space. Otherwise, a clear contraindication to this approach is occlusion of the contralateral transverse–sigmoid sinuses and a potential contraindication would be utilizing this exposure in older patients with poor quality dura.
Conclusions
We describe our experience with a modification to the extended retrosigmoid approach which we had previously reported [11] for neoplastic lesions in the posterior fossa. This new modification has made the surgical craniotomy more efficient and equally safe. Among the different surgical approaches to the cerebellar-pontine angle, the extended retrosigmoid may represent the most effective technique for maximizing the surgeons’ working angle. In comparison with the standard retrosigmoid craniotomy, the extended technique provides additional working room in the cerebellar-pontine angle and enhanced access to regions medial to the seventh/eighth nerve complex and ventral to the brainstem. This approach does have the primary risk of venous injury/congestion. This approach should be considered an option for lesions in this anatomic compartment and should be considered in the armamentarium of neurosurgical skull base surgeons.
References
Al-Mefty O, Fox JL, Smith RR (1988) Petrosal approach for petroclival meningiomas. Neurosurgery 22:510–517
Al-Mefty O, Ayoubi S, Smith RR (1991) The petrosal approach: indications, technique, and results. Acta Neurochir Suppl (Wien) 53:166–170
Baldwin HZ, Miller CG, van Loveren HR et al (1994) The far lateral/combined supra- and infratentorial approach. A human cadaveric prosection model for routes of access to the petroclival region and ventral brain stem. J Neurosurg 81:60–68
Baldwin HZ, Spetzler RF, Wascher TM et al (1995) The far lateral-combined supra- and infratentorial approach: clinical experience. Acta Neurochir (Wien) 134:155–158
Cho CW, Al-Mefty O (2002) Combined petrosal approach to petroclival meningiomas. Neurosurgery 51:708–716, discussion 716–708
Day JD, Tschabitscher M (1998) Anatomic position of the asterion. Neurosurgery 42:198–199
Gharabaghi A, Rosahl SK, Feigl GC et al (2008) Surgical planning for retrosigmoid craniotomies improved by 3D computed tomography venography. Eur J Surg Oncol 34:227–231
Heros RC (1986) Lateral suboccipital approach for vertebral and vertebrobasilar artery lesions. J Neurosurg 64:559–562
Katsuta T, Rhoton AL Jr, Matsushima T (1997) The jugular foramen: microsurgical anatomy and operative approaches. Neurosurgery 41:149–201, discussion 201–142
Kawase T, Toya S, Shiobara R et al (1985) Transpetrosal approach for aneurysms of the lower basilar artery. J Neurosurg 63:857–861
Quinones-Hinojosa A, Chang EF, Lawton MT (2006) The extended retrosigmoid approach: an alternative to radical cranial base approaches for posterior fossa lesions. Neurosurgery 58:ONS-208–ONS-214, discussion ONS-214
Rhoton AL Jr (2000) The cerebellopontine angle and posterior fossa cranial nerves by the retrosigmoid approach. Neurosurgery 47:S93–S129
Rhoton AL Jr (2000) Jugular foramen. Neurosurgery 47:S267–S285
Sekhar LN, Kalia KK, Yonas H et al (1994) Cranial base approaches to intracranial aneurysms in the subarachnoid space. Neurosurgery 35:472–481, discussion 481–473
Shelton C, Alavi S, Li JC et al (1995) Modified retrosigmoid approach: use for selected acoustic tumor removal. Am J Otol 16:664–668
Silverstein H, Norrell H, Smouha E et al (1989) Combined retrolab-retrosigmoid vestibular neurectomy. An evolution in approach. Am J Otol 10:166–169
Silverstein H, Nichols ML, Rosenberg S et al (1995) Combined retrolabyrinthine-retrosigmoid approach for improved exposure of the posterior fossa without cerebellar retraction. Skull Base Surg 5:177–180
Spetzler RF, Daspit CP, Pappas CT (1992) The combined supra- and infratentorial approach for lesions of the petrous and clival regions: experience with 46 cases. J Neurosurg 76:588–599
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Nader Sanai, Phoenix, USA
In this concise report, Dr. Quinones-Hinojosa and colleague review their experience with the extended retrosigmoid craniotomy for both intra- and extra-axial tumors of the posterior fossa. While this technique was originally described in the context of vascular skull-based lesions, its application to large posterior fossa masses is emblematic of an emerging trend in neurosurgical oncology adapting vascular surgery techniques for brain tumors. The study findings support the utility of this approach, demonstrating maximal resection with minimal morbidity.
Nicholas B. Levine, Raymond Sawaya, Houston, Texas, USA
Raza et al. describe a variant of the retrosigmoid technique, which includes tailoring the craniotomy to allow for more exposure of the transverse and sigmoid sinuses. In the authors’ hands, this provides better visualization by eliminating the boney overhang which may prevent retraction of the dura and sinuses, thereby limiting the operative corridor and requiring retraction of the cerebellum. The technique is promoted for both intra- and extra-axial neoplastic lesions. One patient developed sigmoid sinus thrombosis due to the increased exposure of the sinus. Although asymptomatic in this series, this can lead to pseudotumor cerebri and other neurologic sequelae. The authors mention that the petrous bone limits ventral access to the brain stem, a well-known anatomic limitation which has led to the use of posterior petrosectomies by skull base surgeons. The authors briefly discuss the limitations of petrous approaches. The extended retrosigmoid approach provides an alternative to formal skull base approaches.
Rights and permissions
About this article
Cite this article
Raza, S.M., Quinones-Hinojosa, A. The extended retrosigmoid approach for neoplastic lesions in the posterior fossa: technique modification. Neurosurg Rev 34, 123–129 (2011). https://doi.org/10.1007/s10143-010-0284-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-010-0284-3