Abstract
The objective of this study was to compare the impact of peloid and low-level laser (LLLT) treatment in conjunction with a home exercise programme on short-term symptomatic pain, functional status and quality of life in individuals diagnosed with subacromial impingement syndrome (SIS). A total of 168 patients diagnosed with SIS were included in the study, with 56 receiving LLLT + exercise, 56 receiving peloidotherapy + exercise, and 56 receiving exercise only. Patients underwent clinical evaluations prior to treatment (first measurement), after treatment completion (second measurement), and one month post-treatment (third measurement). Pain was evaluated using the Visual Analog Scale (VAS). Functional status was evaluated using the Shoulder Pain and Disability Index (SPADI), and quality of life was evaluated using the Short Form 36 (SF-36). Active range of motion of the shoulder was measured by the same investigator using a goniometer. Statistically significant improvements in VAS, SPADI, SF-36, and ROM parameters were achieved after treatment and at 1 month follow-up compared to pretreatment in both active treatment groups (p < .05). The third group showed significant improvements in ROM and SF-36 physical components after treatment and 1 month later (p < .05). Low-level laser therapy or peloid therapy given in addition to home exercise therapy for SIS were found to have similar short-term effects on pain, functional status, quality of life and ROM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Shoulder pain ranks as the third most prevalent cause of musculoskeletal pain (Garving et al. 2017). It is estimated that between 44 and 65% of all shoulder pain visits are attributable to subacromial impingement syndrome (SIS) (Consigliere et al. 2018). Neer initially described SIS as the mechanical impingement of the rotator cuff tendons and associated tissue between the coracoacromial arch and greater tubercle of the humerus during overhead activities (Neer 2005). Impingement in the subacromial space can cause discomfort at the coracoacromial arch in SIS. This often results from the structures in the subacromial space (Mackenzie et al. 2015). SIS occurs due to degeneration and inflammation of anatomical structures within the subacromial space (Michener et al. 2009). The typical clinical symptom of SIS is pain, that focuses in the anterolateral acromial region and extends to the humerus (Dong et al. 2015).
While rest, anti-inflammatory medication, and cold therapy are the primary interventions for SIS treatment, physical therapy techniques can be employed in cases where there is no observable improvement. This treatment regimen may include approaches such as manipulating and mobilizing techniques, range of motion and strengthening exercises, electrotherapy, laser therapy, and deep as well as superficial heat remedies (Celik et al. 2009; Dogan et al. 2010; Kromer et al. 2009). Research indicates that 70–90% of individuals with SIS improve through the implementation of conservative treatment. Therefore, in cases where no major structural pathology exists, conservative treatment for a period of 3–6 months should be considered the primary treatment option for SIS (Garofalo et al. 2011).
Laser therapy is a painless and non-invasive technique that can be simply administered in physical therapy facilities (Dundar et al. 2015). Low- level laser therapy (LLLT) is a longstanding treatment option for patients experiencing shoulder pain. However, inconclusive findings regarding its effectiveness have led to controversy surrounding its application (Basford et al. 1999).
Peloids are naturally occurring substances that contain a wealth of inorganic and organic components, suitable for use in various therapeutic applications (Gomes et al. 2013). Peloids are used in thermotherapy due to their heating mechanism. The organic and chemical content of peloids is linked to their anti-inflammatory, analgesic, immunological, and chondroprotective effects (Maraver et al. 2021). Musculoskeletal disorders are frequently treated with peloids and this treatment was shown to positively impact pain, function, and quality of life. They are considered a significant area of treatment (Aksanyar et al. 2022).
To the best of our knowledge, no study in the existing literature compares the effectiveness of these two treatment modalities for SIS. Our study aimed to investigate the impact of LLLT and peloidotherapy on short-term pain, functional status, and quality of life among SIS patients.
Materials and methods
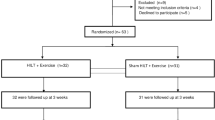
The research consisted of a hospital-based, prospective, randomized controlled study. Approval was granted by the Ethics Committee on 28th May 2018, allocated number 2019/0050 (28.05.2018, 2019/0050). The study included 180 individuals aged between 20 and 60 years who visited the physical therapy and rehabilitation outpatient clinic, were experiencing shoulder pain and received clinical and/or radiological diagnoses of SIS. The shoulder was examined by inspecting, palpating, and testing the passive and active range of motion. Further evaluation was conducted through provocation tests including Hawkins, Neer, and painful arch. All patients involved in the trial received detailed explanations and provided both written and verbal consent. The study was carried out in accordance with the principles of the Declaration of Helsinki.
Inclusion criteria
were age between 20 and 60 years, experiencing pain in shoulder range of motion reaching up to 150 degrees in any plane of motion, experiencing shoulder pain when raising the arm, forced movement of the arm above the head, testing positive for Jobe’s test indicating supraspinatus involvement or positive Hawkins test indicating SIS, experiencing pain in activities of daily living, exhibiting compliance and willingness to participate in treatments, and providing evaluation scores.
Exclusion criteria
for this study were previous shoulder girdle fracture, dislocation/subluxation of the glenohumeral joint, adhesive capsulitis, recent steroid injection into the shoulder within the last six months, continuous use of steroids or NSAIDs, acromioclavicular sprain or separation, and complete rupture of rotator cuff tendons as observed on MRI. Patients who had surgery on their neck or shoulder in the previous 12 months, neck pain that is consistent with radiculopathy, systemic inflammatory rheumatic disease, disseminated bacterial, viral, or fungal infections, malignancies, decompensated heart failure, a cardiac pacemaker, angina status, severe asthma, epilepsy, neurological deficits, or who were currently pregnant did not participate. Additionally, patients with positive drop arm test were also excluded.
Interventions
Participants were randomly allocated into three groups based on a randomized table. The first group received peloid application at 45 °C for 2 weeks, 5 days/week, 10 sessions total, 20 min each, on the shoulder where SIS was observed. A layer of peloid approximately 1.5-2 cm thick was applied to the shoulder, before wrapping it with a nylon bag and covering with a towel. After 20 min, the peloid layer was removed and the treated area was gently cleaned using soft cloths moistened with hot water, before concluding the session. Medicinal peloid was acquired from Köyceğiz in the Muğla province and contains a wealth of humic acid, as well as organic and inorganic matter (Fig. 1) (Karaarslan and Ordahan 2021). The patients in this group were administered a standard exercise programme for a duration of 2 weeks, together with peloidotherapy. The second group was administered LLLT for a span of two weeks, with five treatments a week for a total of ten sessions. With the patient seated comfortably in a chair, wearing protective eyewear and with their head turned away, LLLT was administered to the shoulder with SIS. The subacromial space, glenohumeral space, and adhesion site of the supraspinatus tendon were each treated with 100 Mw power output gallium-aluminium-arsenide (GaAIAs) diode laser (Chattanooga, Mexico, USA) emitting infrared light with a wavelength of 860 nm and frequency of 1 kHz, with a dose of 3.6 j/cm2. The laser probe was held perpendicular to the skin for 40 s in an area approximately 15–20 cm2. The total session duration was 120 s. Alongside LLLT, this group followed a standard exercise programme for two weeks. Patients assigned to the exercise group (group 3) received a two-week same standard exercise regimen as the other two groups consisting of 10 repetitions with 2 sets per day, lasting around 30 min daily. All patients received a standard home workout regimen comprising range-of-motion exercises (active and active-assisted), Codman exercises, stick exercises (in flexion, extension, abduction, adduction, and internal-external rotation directions), isometric strengthening (5–7 repetitions with a contraction time of 6–7 s), and self-stretching exercises for the inferior and posterior capsule (static stretching for 15–20 s, according to pain tolerance). Additionally, submaximal isotonic strengthening exercises were included. Exercises were arranged so as not to exceed the patient’s pain tolerance limit and patients were advised to use ice for 15 min if necessary. The physiatrist demonstrated the exercises to the patient and provided a printed guide including illustrated exercise descriptions. Compliance with the exercises was encouraged through face-to-face or telephone interviews. Participants with less than 75% compliance were excluded from the study.
Assessment parameters
Patients underwent evaluations prior to treatment (baseline measurement 1), following treatment (measurement 2) and one month post-treatment completion (measurement 3). During treatment, patients received instructions to take paracetamol only when necessary for pain relief, with a maximum daily limit of 2000 mg, unless they were on continuous medication for comorbid conditions. However, patients were advised to abstain from analgesics for 24 h before evaluations.
The Visual Analogue Scale (VAS) was used for pain assessment while the Shoulder Pain and Disability Index (SPADI) was used to evaluate functional status and Short Form 36 (SF-36) was used to assess quality of life. The active range of motion of the shoulder was assessed by measuring flexion, abduction, internal-external rotation, adduction and extended angles with a goniometer and the results were documented.
Range of motion
Flexion, abduction, internal and external rotation were assessed using a goniometer while in the supine position. Active movements were also recorded during the assessment. The goniometer was centred on the acromion for abduction with 90° flexion of the shoulder and elbow, on the greater tubercle for flexion, and on the olecranon for internal and external rotation.
Visual Analog Scale (VAS)
In this study, patients’ pain levels were evaluated using VAS. For the purpose of this study, a 10-centimetre line was drawn and divided into 10 intervals with 10 millimetres width. Patients were informed that 0 denoted no pain and 10 denoted the most severe pain. They were then asked to indicate on the scale the level of shoulder pain experienced at rest, during daily work activities, and at night. The distance between zero pain and the point indicated by the patient measures the level of pain experienced (Ritter et al. 2006).
Shoulder Pain and Disability Index (SPADI)
Functional assessment of patients used the Shoulder Pain and Disability Index (SPADI) for evaluation. SPADI is a scale that includes 5 questions about pain and 8 questions about disability and patients are asked to answer these questions on a numeric scale of 0–10 (Roach et al. 1991; Breckenridge and McAuley 2011; Angst et al. 2011). The pain and disability scores are calculated independently and together. Increased scores indicate more intense pain and disability (Roach et al. 1991; Angst et al. 2011; Williams et al. 1995). The study of the validity and reliability of the Turkish version of SPADI was carried out by Biçer et al. (Erol et al. 2008).
Short form 36 (SF-36)
Quality of life was evaluated using the Short Form 36 (SF-36) health survey. SF-36 is a 36-item questionnaire comprising of 8 domains designed to evaluate overall quality of life. The scale comprises eight subgroups, namely general health, physical functioning, physical condition, pain, life functions, social functions, emotional state and mental health, along with two summary scales; mental health and physical health. The measure is evaluated on a scale ranging from 0 to 100, where 0 denotes the poorest health status and 100 represents the optimal health status. This scale was specifically designed for application within the general population. The validity and reliability of the Turkish version of the scale was examined by Koçyiğit et al. (Kocyigit 1999).
Statistical analysis
IBM SPSS 26 package program (Armonk, NY, USA) was used to analyse the data. The significance level was assessed at 0.05. Examination of the skewness and kurtosis coefficients of the measurements for each variable for patients with SIS throughout the study was used to determine whether the values showed normal distribution. The results showed that the VAS, shoulder pain and disability scale, and the total SPADI scores and physical and mental component levels fell within ± 1.5, whereas range of motion measurement scores did not. The presence of normal distribution can be inferred when the skewness and kurtosis coefficients of the measured values fall between the range of ± 1.5 (Tabachnick 2013). The repeated measures ANOVA analysis, a parametric statistical method, was utilized to compare the measurements of VAS, shoulder pain and disability scale, total SPADI scores, and physical and mental component levels. In contrast, the Friedman test, a non-parametric statistical method, was used to compare the range of motion scores.
For inter-group analyses, the one-way ANOVA test was used for normally distributed variables, while the Kruskal Wallis H test was used for non-normally distributed variables. The chi-square test was employed for discontinuous variables and the one-way ANOVA test was used for continuous variables when comparing descriptive information between groups.
Sample size
The sample size for the study was calculated using G*Power 3.1.9. The effect size was determined to be 0.25, with a margin of error of 0.05 and a power value of 0.95, using parameters specific to the type of test. The study consisted of three groups with three measurements, and a total of 168 participants were included, guided by Kepekçi et al.‘s research (VAS score) (Kepekçi et al. 2018). Consistent with these findings, the study enrolled 168 patients with SIS, with equal numbers of participants (56 per group) assigned to the peloid, LLLT, and exercise interventions.
Results
The research was conducted with a sample of 168 participants with mean age of 49.38 ± 9.15 years. Due to pandemic conditions, 3 participants from the peloidotherapy group, 2 from the laser group, and 3 from the exercise group were unable to complete the treatment. As a result, 1 participant from the peloidotherapy group, 2 from the LLLT group, and 1 from the exercise group were excluded from the study for non-compliance with exercise. Demographic and clinical features of the patients are outlined in Table 1. There were no significant disparities between the groups with regards to their clinical and demographic characteristics at baseline (p > .05). No adverse effects were noted during treatment.
The peloid and LLLT treatments significantly reduced VAS scores for patients with SIS from pre-treatment through the end of treatment and one month afterward. The laser group also showed a significant decrease in VAS scores from the end of treatment to one month later (p < .05). However, the two treatments did not differ significantly (p > .05) according to the results in Table 2.
Patients diagnosed with SIS and treated with either peloid or LLLLT registered significant reductions in shoulder pain and disability levels. Additionally, their total scores on SPADI dropped considerably from pre-treatment to post-treatment and remained consistent one month later (p < .05). A noteworthy reduction in shoulder disability and total SPADI scores occurred from after treatment to 1 month post-treatment in the group (p < .05). However, there was no significant difference between the two treatment modalities (p > .05) (Table 3).
Significant increases in physical component levels of SF-36 were observed in the peloid and exercise group from before treatment to 1 month after treatment, as well as in the LLLT group from pre-treatment to post-treatment, 1 month after treatment, and from post-treatment to 1 month after treatment (p < .05). There was a significant increase in mental component levels in the peloid group between pre-treatment and post-treatment, as well as between post-treatment and 1 month post-treatment. The LLLT group also showed a significant increase in mental component levels between pre-treatment and post-treatment, as well as between post-treatment and 1 month post-treatment (p < .05). Conversely, the exercise group experienced no significant change (p > .05) (Table 4).
Shoulder abduction, internal rotation, and external rotation scores of patients diagnosed with SIS who received either peloid or LLLT treatment had a significant increase from pre-treatment to post-treatment and one month after treatment (p < .05). In the intervention group, the patients’ shoulder flexion and extension scores significantly increased from pre-treatment to 1 month after treatment. Additionally, their shoulder external rotation scores showed a significant increase from pre-treatment to post-treatment. Statistical analysis indicated that there was no significant difference between the two treatment methods (p > .05) (Table 5).
Discussion
The findings, which assessed the short-term efficacy of LLLT and peloidotherapy therapies for patients with SIS, demonstrated the effectiveness of both treatments in reducing pain, improving functional status, enhancing quality of life, and increasing ROM in the short term.
LLLT has been employed to treat musculoskeletal disorders as it has analgesic, biostimulative, wound-healing, and lymphocyte activation effects (MF et al. 2022; Ozkaraoglu et al. 2020; Ahmed et al. 2022). Several academic studies indicated that low- level laser could be an effective intervention for SIS treatment. A meta-analysis conducted by Haslerud et al. demonstrated that laser therapy could have an analgesic impact on shoulder tendinopathy and may accelerate the healing process when combined with exercise or physical therapy modalities (Haslerud et al. 2015). Alfredo et al. concluded that low-dose laser therapy combined with exercise in SIS will provide pain reduction and faster functional recovery by controlling inflammation or stimulating tendon repair (Alfredo et al. 2021). Abrisham et al. conducted a study in which LLLT was implemented in conjunction with exercise in patients with SIS. The results indicated that this combined treatment proved to be more effective than exercise therapy alone in alleviating pain and improving range of motion in the shoulder (Abrisham et al. 2011). In a review of 78 randomized controlled trials, Bjordal and colleagues determined that LLLT has the potential to decrease pain in subacute and chronic tendinopathies provided that the dosage is appropriate to the treatment procedure and the location of the condition (Bjordal et al. 2001). Alternatively, Gomez et al. utilized high- level laser therapy in combination with exercise for patients afflicted with SIS. They determined that this intervention proved no more efficacious than the control group, subjected only to placebo laser therapy and exercise, in ameliorating pain or enhancing functionality for SIS patients (Aceituno-Gómez et al. 2019). In our study, similar to the literature, LLLT was found to be effective on pain, functional status, quality of life and ROM in patients with SIS. Consequently, low-level laser therapy can be considered a trustworthy and effective remedy in SIS treatment planning.
The impact of peloids involves a blend of mechanical, thermal and chemical influences. Thermal impacts manifest when peloids store heat adeptly and gradually transfer it to the skin’s surface. The high heat retention capacity of peloids leads to a slow heat loss, resulting in deep tissue heating. Inorganic (sulphur, sodium, magnesium chloride, sulphate, iodine, bromine, zinc and selenium) and organic (bitumen, pectin, cellulose, lignin, humin, sulphoglycolipids, humic, fulvic and ulmic acids) substances contained in peloid cause chemical effects. The absorption of these substances via the skin leads to vasodilation, relaxation of smooth muscles, inhibition of inflammation in Langerhans cells of the skin, prevention of arachidonic acid breakdown into prostaglandins, and inhibition of hyaluronidase activity, culminating in antioxidant, antiviral and anti-inflammatory outcomes (Odabasi et al. 2008; Fraioli et al. 2011). There is a paucity of research examining the effectiveness of peloidotherapy in treating patients with SIS. The findings of the study support the use of peloidotherapy for the treatment of SIS. The available research suggests that peloidotherapy can be an effective treatment for SIS. Kepekçi et al. conducted a study that administered peloid and exercise therapy to one group by a nurse in hospital, while the other group received the same treatment at home with supervision from the patient’s companion. The reduction in pain scores was considerably greater in the peloidotherapy group that received treatment in the hospital, as opposed to those who received the therapy at home (Kepekçi et al. 2018). A study by Şen et al. examined the impact of balneotherapy on patients with RDS. A total of 29 patients participated in a 15-session course of peloid therapy and exercise over three weeks. There were significant improvements in the patients’ pain and functional status following treatment and at the end of the third month (Sen et al. 2010). A randomized single-blind study was conducted by Tefner et al. to investigate the effectiveness of balneotherapy in patients diagnosed with chronic shoulder pain. Forty-six patients were divided into two groups. The first group underwent ten exercise and transcutaneous electrical nerve stimulation (TENS) sessions three times a week for four weeks, while the second group underwent fifteen exercise, TENS and balneotherapy sessions during the same period. Both groups exhibited significant improvements in their pain and disability scores. When comparing the two groups, the group receiving balneotherapy exhibited a more noticeable improvement in both pain and disability (Tefner et al. 2015). The findings of our study showed that peloidotherapy is effective and safe for the treatment of SIS, in line with the literature.
The findings of our study should be interpreted with a number of limitations in mind. The most significant constraint to our study is the brief follow-up duration. Additionally, the research being completed solely at one centre may impede the generalisation of results. The implementation of exercise therapy as a home program, rather than under the supervision of a physiotherapist in a hospital setting, may have impacted patient compliance and decreased the effectiveness of the exercise.
In addition, this research constitutes the first randomized controlled trial that compares the efficacy of peloid and LLLT treatment among patients diagnosed with SIS.
Conclusion
For the conservative management of SIS, both peloidotherapy and LLLT exhibit comparable favourable outcomes on pain, functional status, quality of life, and ROM. The efficacy of peloidotherapy and LLLT in SIS over the long run needs confirmation with extensive follow-up studies.
References
Abrisham SM, Kermani-Alghoraishi M, Ghahramani R, Jabbari L, Jomeh H, Zare M (2011) Additive effects of low-level laser therapy with exercise on subacromial syndrome: a randomised, double-blind, controlled trial. Clin Rheumatol 30(10):1341–1346. https://doi.org/10.1007/s10067-011-1757-7
Aceituno-Gómez J, Avendaño-Coy J, Gómez-Soriano J, García-Madero VM, Ávila-Martín G, Serrano-Muñoz D, González-González J, Criado-Álvarez JJ (2019) Efficacy of high-intensity laser therapy in subacromial impingement syndrome: a three-month follow-up controlled clinical trial. Clin Rehabil 33(5):894–903. https://doi.org/10.1177/0269215518824691
Ahmed I, Mohseni Bandpei MA, Gilani SA, Ahmad A, Zaidi F (2022) Correlation analysis between Pain Intensity, Functional Disability and Range of Motion using low-level laser therapy in patients with discogenic lumbar Radiculopathy: a cross-sectional study. J Lasers Med Sci 13:e26. https://doi.org/10.34172/jlms.2022.26
Aksanyar B, Yılmaz H, Karaarslan F, Yılmaz R, Karpuz S (2022) Comparison of the effectiveness of peloid and paraffin treatment for symptomatic hand osteoarthritis in women: a single-blind randomized controlled study. Int J Biometeorol 66(9):1841–1851. https://doi.org/10.1007/s00484-022-02324-z
Alfredo PP, Bjordal JM, Junior WS, Marques AP, Casarotto RA (2021) Efficacy of low-level laser therapy combined with exercise for subacromial impingement syndrome: a randomised controlled trial. Clin Rehabil 35(6):851–860. https://doi.org/10.1177/0269215520980984
Angst F, Schwyzer HK, Aeschlimann A, Simmen BR, Goldhahn J (2011) Measures of adult shoulder function: disabilities of the arm, shoulder, and Hand Questionnaire (DASH) and its short version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and elbow surgeons (ASES) society standardized shoulder assessment form, constant (Murley) score (CS), simple shoulder test (SST), Oxford Shoulder score (OSS), shoulder disability questionnaire (SDQ), and western Ontario shoulder instability index (WOSI). Arthritis Care Res (Hoboken) 63(Suppl 11):S174–188. https://doi.org/10.1002/acr.20630
Basford JR, Sheffield CG, Harmsen WS (1999) Laser therapy: a randomized, controlled trial of the effects of low-intensity nd:YAG laser irradiation on musculoskeletal back pain. Arch Phys Med Rehabil 80(6):647–652. https://doi.org/10.1016/s0003-9993(99)90167-3
Bjordal JM, Couppe C, Ljunggren AE (2001) Low level laser therapy for tendinopathy. Evidence of a dose–response pattern. Phys Therapy Reviews 6(2):91–99. https://doi.org/10.1179/108331901786166569
Breckenridge JD, McAuley JH (2011) Shoulder Pain and Disability Index (SPADI). J Physiother 57(3):197. https://doi.org/10.1016/s1836-9553(11)70045-5
Celik D, Atalar AC, Sahinkaya S, Demirhan M (2009) The value of intermittent ultrasound treatment in subacromial impingement syndrome. Acta Orthop Traumatol Turc 43(3):243–247. https://doi.org/10.3944/aott.2009.243
Consigliere P, Haddo O, Levy O, Sforza G (2018) Subacromial impingement syndrome: management challenges. Orthop Res Rev 10:83–91. https://doi.org/10.2147/orr.S157864
Dogan SK, Ay S, Evcik D (2010) The effectiveness of low laser therapy in subacromial impingement syndrome: a randomized placebo controlled double-blind prospective study. Clin (Sao Paulo) 65(10):1019–1022. https://doi.org/10.1590/s1807-59322010001000016
Dong W, Goost H, Lin XB, Burger C, Paul C, Wang ZL, Zhang TY, Jiang ZC, Welle K, Kabir K (2015) Treatments for shoulder impingement syndrome: a PRISMA systematic review and network meta-analysis. Med (Baltim) 94(10):e510. https://doi.org/10.1097/md.0000000000000510
Dundar U, Turkmen U, Toktas H, Ulasli AM, Solak O (2015) Effectiveness of high-intensity laser therapy and splinting in lateral epicondylitis; a prospective, randomized, controlled study. Lasers Med Sci 30(3):1097–1107. https://doi.org/10.1007/s10103-015-1716-7
Erol Ö, Özçakar L, Çeliker R (2008) Shoulder rotator strength in patients with stage I-II subacromial impingement: relationship to pain, disability, and quality of life. J Shoulder Elbow Surg 17(6):893–897. https://doi.org/10.1016/j.jse.2008.05.043
Fraioli A, Serio A, Mennuni G, Ceccarelli F, Petraccia L, Fontana M, Grassi M, Valesini G (2011) A study on the efficacy of treatment with mud packs and baths with Sillene mineral water (Chianciano Spa Italy) in patients suffering from knee osteoarthritis. Rheumatol Int 31(10):1333–1340. https://doi.org/10.1007/s00296-010-1475-5
Garofalo R, Conti M, Massazza G, Cesari E, Vinci E, Castagna A (2011) Subcoracoid impingement syndrome: a painful shoulder condition related to different pathologic factors. Musculoskelet Surg 95 Suppl 1S25–29. https://doi.org/10.1007/s12306-011-0142-7
Garving C, Jakob S, Bauer I, Nadjar R, Brunner UH (2017) Impingement Syndrome of the shoulder. Deutsches Ärzteblatt International 114(45):765–776. https://doi.org/10.3238/arztebl.2017.0765
Gomes C, Carretero MI, Pozo M, Maraver F, Cantista P, Armijo F, Legido JL, Teixeira F, Rautureau M, Delgado R (2013) Peloids and pelotherapy: historical evolution, classification and glossary. Appl Clay Sci 75:28–38. https://doi.org/10.1016/j.clay.2013.02.008
Haslerud S, Magnussen LH, Joensen J, Lopes-Martins RA, Bjordal JM (2015) The efficacy of low-level laser therapy for shoulder tendinopathy: a systematic review and meta-analysis of randomized controlled trials. Physiother Res Int 20(2):108–125. https://doi.org/10.1002/pri.1606
Karaarslan F, Ordahan B (2021) Efficacy of peloidotherapy in unilateral plantar fasciitis: a pilot study. Turk J Phys Med Rehabil 67(4):473–481. https://doi.org/10.5606/tftrd.2021.6494
Kepekçi M, Taspınar Ö, Barut Y, Geçmen İ (2018) Subakromiyal Sıkışma Sendromlu Hastalarda Peloidoterapinin Etkinliği. Uludağ Üniversitesi Tıp Fakültesi Dergisi 45(1):23–27. https://doi.org/10.32708/uutfd.457747
Koçyiğit H, Aydemir O, Fişek G, Ölmez N, Memiş A (1999) Reliability and validity of the Turkish version of short Form-36 (SF-36). İlaç ve Tedavi Dergisi 12:102–106
Kromer TO, Tautenhahn UG, de Bie RA, Staal JB, Bastiaenen CH (2009) Effects of physiotherapy in patients with shoulder impingement syndrome: a systematic review of the literature. J Rehabil Med 41(11):870–880. https://doi.org/10.2340/16501977-0453
Mackenzie TA, Herrington L, Horlsey I, Cools A (2015) An evidence-based review of current perceptions with regard to the subacromial space in shoulder impingement syndromes: is it important and what influences it? Clin Biomech (Bristol Avon) 30(7):641–648. https://doi.org/10.1016/j.clinbiomech.2015.06.001
Maraver F, Armijo F, Fernandez-Toran MA, Armijo O, Ejeda JM, Vazquez I, Corvillo I, Torres-Piles S (2021) Peloids as thermotherapeutic agents. Int J Environ Res Public Health 18(4):1965. https://doi.org/10.3390/ijerph18041965
Michener LA, Walsworth MK, Doukas WC, Murphy KP (2009) Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil 90(11):1898–1903. https://doi.org/10.1016/j.apmr.2009.05.015
Neer CS 2 (2005) nd Anterior acromioplasty for the chronic impingement syndrome in the shoulder. 1972. J Bone Joint Surg Am 87 (6):1399. https://doi.org/10.2106/JBJS.8706.cl
Odabasi E, Turan M, Erdem H, Tekbas F (2008) Does mud pack treatment have any chemical effect? A randomized controlled clinical study. J Altern Complement Med 14(5):559–565. https://doi.org/10.1089/acm.2008.0003
Oliveria MF, Johnson DS, Demchak T, Tomazoni SS, Leal-Junior EC (2022) Low-intensity LASER and LED (photobiomodulation therapy) for pain control of the most common musculoskeletal conditions. Eur J Phys Rehabil Med 58(2):282–289. https://doi.org/10.23736/s1973-9087.21.07236-1
Ozkaraoglu DK, Tarakci D, Algun ZC (2020) Comparison of two different electrotherapy methods in low back pain treatment. J Back Musculoskelet Rehabil 33(2):193–199. https://doi.org/10.3233/bmr-181199
Ritter PL, González VM, Laurent DD, Lorig KR (2006) Measurement of pain using the visual numeric scale. J Rheumatol 33(3):574–580
Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y (1991) Development of a shoulder pain and disability index. Arthritis Care Res 4(4):143–149. https://doi.org/10.1002/art.1790040403
Sen U, Karagülle M, Erkorkmaz Ü (2010) The efficacy of Balneotherapy in the patients with Subacromial Impingement Syndrome. Türkiye Klinikleri Tip Bilimleri Dergisi 30(3):906. https://doi.org/10.5336/medsci.2008-8589
Tabachnick BG, Fidell LS (2013) Using multivariate statistics (6th Edition). Pearson Education, Los Angeles
Tefner IK, Kovács C, Gaál R, Koroknai A, Horváth R, Badruddin RM, Borbély I, Nagy K, Bender T (2015) The effect of balneotherapy on chronic shoulder pain. A randomized, controlled, single-blind follow-up trial. A pilot study. Clin Rheumatol 34(6):1097–1108. https://doi.org/10.1007/s10067-013-2456-3
Williams JW Jr., Holleman DR Jr., Simel DL (1995) Measuring shoulder function with the Shoulder Pain and Disability Index. J Rheumatol 22(4):727–732
Funding
The authors have no relevant financial or non-financial interests to disclose. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Agir, F.C., Karpuz, S., Yilmaz, R. et al. Comparison of the efficacy of low intensity laser and peloid therapy in patients with subacromial impingement syndrome. Int J Biometeorol 68, 1507–1517 (2024). https://doi.org/10.1007/s00484-024-02660-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-024-02660-2