Abstract
Lateral epicondylitis (LE) is a common disorder that causes pain on the outside of the elbow, as well as pain and weakness during gripping. In this prospective, randomized, controlled, assessor-blinded trial, we planned to investigate the effects of high-intensity laser therapy (HILT) in patients with LE and to compare these results with those of a brace and placebo HILT. Patients were randomly assigned to three treatment groups. The first group was treated with HILT. The second group (sham therapy group) received placebo HILT, while the third group (brace group) used the lateral counterforce brace for LE. The patients were assessed for grip strength, pain, disability, and quality of life. Outcome measurements and ultrasonographic examination of the patients were performed before treatment (week 0) and after treatment (after 4 and 12 weeks). HILT and brace groups showed significant improvements for most evaluation parameters (pain scores, grip strength, disability scores, and several subparts of the short-form 36 health survey (physical function, role limitations due to physical functioning, bodily pain, general health, and vitality)) after treatment (after 4 and 12 weeks). However, the improvements in evaluation parameters of the patients with LE in HILT and brace groups were not reflected to ultrasonographic findings. Furthermore, comparison of the percentage changes of the parameters after treatment relative to pretreatment values did not show a significant difference between HILT and brace groups. We conclude that HILT and splinting are effective physical therapy modalities for patients with LE in reducing pain and improving disability, quality of life, and grip strength.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lateral epicondylitis (LE) or tennis elbow is a common disorder that causes pain on the outside of the elbow, as well as pain and weakness during gripping. It has been found to occur in approximately 1.3–1.7 % of people between the third and sixth decades of life in studied populations [1, 2]. Physical strain may play a part in the development of LE, as the dominant arm is significantly more often affected than the nondominant arm. LE is usually self-limiting, and symptoms seem to resolve between 6 and 24 months in most patients [3].
To date, a standardized, universally accepted program for LE treatment has not been established. Various nonsurgical modalities have been described. In general, treatment can begin with patient education, application of commonly available treatments, physiotherapy, manual therapy, laser therapy, tennis elbow brace, exercises, massage, and local injection therapy, as well as oral or topical nonsteroidal anti-inflammatory drugs (NSAIDs) [4].
Laser treatment is a noninvasive and painless method that can be easily administered in therapy units for a wide range of conditions [5]. Effectiveness of low-level laser therapy (LLLT) in LE is controversial. One meta-analysis of LLLT for lateral epicondylitis found that LLLT was ineffective in the treatment of LE [6]. However, other two examinations of the literature based upon treatment protocol concluded a positive effect [7, 8].
Recently, the pulsed neodymium-doped yttrium aluminum garnet (Nd:YAG) laser, a form of high-intensity laser therapy (HILT), was introduced as a new treatment option. The superiority of HILT over LLLT is that HILT is able to reach and stimulate the larger and/or deeper areas; accordingly, during HILT therapy, significantly greater energy might be transferred into tissue compared to LLLT [9]. The effectiveness of HILT in LE is not yet clarified.
As a conservative treatment intervention, splinting is one of the most frequently used treatment modality for LE. Two popular methods of bracing include a forearm counterforce strap and a wrist extension splint. Although braces are commonly prescribed for lateral epicondylitis, controversy still exits regarding their effectiveness [10].
Clinical examination is generally accepted to be appropriate for the diagnosis of LE in most patients [11]. However, in patients with persistent pain and disability despite treatment, imaging methods including ultrasonography might be necessary. For this reason, ultrasonographic evaluation for injuries of the extensor tendon, nearby soft tissues, and/or the cortex of the lateral epicondyle may be valuable [12].
In this trial, we planned to investigate the effects of HILT in patients with LE and to compare (clinically and ultrasonographically) these results with those of a brace and sham HILT.
Methods
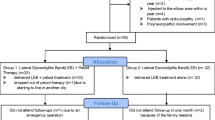
This prospective, randomized, controlled, assessor-blinded study was conducted in Physical Medicine and Rehabilitation Department of the university hospital between May 2013 and June 2014. Ninety-three patients (42 female/51 male; age range between 20 and 50 years) with the diagnosis of unilateral LE were enrolled in the study and assigned to three groups. Figure 1 summarizes the flowchart regarding patients’ enrollment.
Before inclusion, all subjects were examined by one of the authors to confirm the diagnosis of LE. Patients were diagnosed based on the following criteria for LE: (1) pain in the lateral elbow region (lasting less than 3 months), (2) local tenderness on palpation over the lateral epicondyle, (3) resisted wrist and/or middle finger extension produced typical pain at the origin on the lateral epicondyle, and (4) a positive Mill’s test [13]. Patients who fulfilled the above criteria were enrolled in the study.
Exclusion criteria were as follows: (1) fibromyalgia, (2) previous treatment for ipsilateral LE, (3) substantial rheumatoid arthritis, osteoarthritis, or inflammatory arthropathy affecting the elbow or wrist, (4) carpal tunnel syndrome, (5) cubital tunnel syndrome, (6) cervical radiculopathy, (7) previous elbow surgery, (8) previous radius/ulna fracture with resultant deformity of the affected extremity, (9) other elbow pathologies, (10) neurological deficit(s) in the ipsilateral upper limb, (11) systemic metabolic diseases, (12) other cervical/shoulder disorders, and (13) bilateral elbow pain.
All enrolled patients were instructed not to take any analgesic and/or NSAIDs during the treatment and control periods. All patients were informed about the study procedure, and they have given written consent to participate. This study was approved by the local ethical committee of the university.
Treatment groups
Patients were randomly assigned to three treatment groups (HILT group vs sham therapy group vs brace group). Randomization was allocated by using numbered envelopes method. HILT group (group 1) was treated with HILT. Sham therapy group (group 2) received placebo HILT. Patients in the brace group (group 3) used the lateral counterforce brace for LE. All enrolled patients were not treated with HILT before for any other disorders. The treatment modalities in all groups (HILT, placebo HILT, or brace) were started 1 day after initial assessment.
HILT (pulsed Nd:YAG laser therapy)
Patients received pulsed Nd:YAG laser treatment, produced by a HIRO 3 device (ASA Laser, Arcugnano, Italy). The apparatus provided pulsed emission (1064 nm), very high peak power (3 kW), a high level of fluency (energy density; 360–1780 mJ/cm2), a short duration (120–150 μs), a mean power of 10.5 W, a low frequency (10–40 Hz), a duty cycle of about 0.1 %, a probe diameter of 0.5 cm, and a spot size of 0.2 cm2 [9].
A standard handpiece endowed with fixed spacers was used to provide the same distance to the skin and perpendicularly to the zone to be treated with a laser beam diameter of 5 mm. Three phases of treatment were performed for every session. The total energy delivered to the patient during one session was 1275 J through three phases of treatment. The first phase involved fast manual scanning (100 cm2 per 30 s) of common extensor tendon (CET), soft tissues near the lateral epicondyle, and extensor muscles extending over forearm from lateral epicondyle (extensor carpi radialis longus and brevis, extensor carpi ulnaris, and extensor digitorum communis). Scanning was performed in both transverse and longitudinal directions. In this phase, a total energy dose of 625 J was administered. In the first phase, the laser fluency was set to three subphases of 510 mJ/cm2 (208 J), 810 mJ/cm2 (208 J), and 970 mJ/cm2 (209 J), for a total of 625 J. The second phase involved applying the handpiece with fixed spacers vertically to 90° on CET near the lateral epicondyle (trigger point inactivation phase). The second phase was carried out on CET with a fluency of 360 mJ/cm2 (6 J), 510 mJ/cm2 (9 J), and 610 mJ/cm2 (10 J) and a time of 6 s at each time, for a total of 25 J. The third phase involved slow manual scanning (100 cm2 per 60 s) of the same areas treated in the first phase until a total energy dose of 625 J was achieved (Table 1). The application time for one session was approximately 15 min with the total energy delivered to the patient during one session of 1275 J. The energy received in each phase and the total energy delivered to the patient during the treatment session were calculated by the device. HILT was applied once a day for 15 days during a period of 3 weeks. In group 2 (sham therapy group), the same treatment protocol was given, but the laser instrument was switched off during applications. All laser applications were performed by the same physiotherapist.
Brace
Patients in the brace group (group 3) used the lateral counterforce brace for LE (Aurafix, Turkey) during the daytime for 4 weeks (Fig. 2). Brace removal was allowed only for bathing and sleeping.
Outcome measurements
The patients were assessed for grip strength, pain, disability, and quality of life. The same physician blinded to the randomization evaluated all the patients before treatment (week 0) and after treatment (after 4 and 12 weeks). Ninety-one patients completed the study. One male patient in HILT group and one male patient in brace group failed to complete the follow-up and dropped out of the study.
Outcome measures
We measured grip strength at 90° elbow flexion with a hand dynamometer (baseline hydraulic hand dynamometer, Irvington, NY, USA) and used the mean of three measurements [14].
Pain was assessed at rest and under strain by using a 10-cm-long visual analog scale (VAS) (0 means no pain while 10 means worst pain).
The Patient-Rated Tennis Elbow Evaluation (PRTEE) questionnaire was used to measure the changes in functional disability. The PRTEE questionnaire is a 15-item questionnaire specifically designed for patients with LE. The items investigate pain (five items) and the degree of difficulty in performing various activities (six specific and four usual activity items) due to the elbow problem over the preceding week. Each item has one response option (0 = no difficulty, 10 = unable to perform). The scores for the various items are used to calculate an overall scale score ranging from 0 (best score) to 100 (worst score) [15].
Quality of life was assessed by short-form 36 health survey (SF-36) [16].
Ultrasonographic evaluation
Ultrasonographic examination of the patients was performed before treatment (week 0) and after treatment (after 4 and 12 weeks) by a clinician with 4 years of experience in musculoskeletal ultrasonography, who was blind to the patients’ clinical data. Ultrasonographic examination was performed by using an Esoate Mylab 70 ultrasound machine with an 18–6-MHz linear array transducer. The ultrasonographic technique used in a previous study evaluating lateral epicondylitis with ultrasonography was accepted as reference [17]. The thickness/echogenicity of the CET and bony cortex of the lateral epicondyle were assessed during sonographic imaging (while patients were seated, elbows flexed and pronated). For measurement of the thickness of the CET, two lines were drawn; the first line was drawn between the peak point and lowermost point of lateral epicondyle. Then, the second line was drawn 90° perpendicular to the lower end of first line. The second line gave the thickness of the CET. The measurements were performed three times and the mean of these measurements was used for analysis (Fig. 3).
Statistical analysis
Descriptive statistics were expressed with mean ± standard deviation. A level of significance of P < 0.05 (two-tailed) was accepted for this study. Chi-square test was used to compare categorical variables (sex, occupation, side of involvement, dominant hand, CET echogenicity, bony cortex of the lateral epicondyle). Shapiro–Wilk test was used to analyze normality of the distribution of the data. Groups were compared with one-way ANOVA (for normally distributed data (pain at rest, pain under strain, CET thickness, all subgroups of SF-36); the Tukey test was used as a post hoc test) and Kruskal–Wallis (the data without normal distribution (grip strength, PRTEEQ); Mann–Whitney U test was used as a post hoc test). Cochran Q test (for categorical data), Wilcoxon (the data without normal distribution), and paired t test (for normally distributed data) were used to compare repeated measures/evaluations within each group. The mean values of the percentage changes calculated for the groups were compared by using the independent sample t test (for normally distributed data) and Mann–Whitney U test (the data without normal distribution). The correlations were evaluated with Spearman correlation tests. All analyses were performed using the SPSS for Windows 18.0 software program.
Results
No adverse event was observed during HILT, sham therapy, and/or brace therapy in the study. There were no statistically significant differences in the demographic features and pre-treatment evaluation parameters of the patients between groups. Demographic features of HILT group, sham therapy group, and brace group are given in Table 2. Pretreatment values for evaluation parameters of the groups are shown in Table 3.
The occupation of the patients were as follows: eight office workers, seven sales/marketing personnel, two heavy work workers, three unemployed, five full-time homemakers, one part-time worker, and four farmers in HILT group; nine office workers, six sales/marketing personnel, two heavy work workers, three unemployed, six full-time homemakers, two part-time workers, and three farmers in sham therapy group; and seven office workers, seven sales/marketing personnel, three heavy work workers, two unemployed, five full-time homemakers, two part-time workers, and four farmers in brace group. Distribution of the patients according to occupation did not show a significant difference between the groups (P > 0.05).
HILT group and brace group showed significant improvements for pain (VAS) scores, grip strength, PRTEEQ scores and physical function, role limitations due to physical functioning, bodily pain, general health, and vitality subparts of SF-36 at the evaluations 4 and 12 weeks after treatment (Tables 4 and 6). However, there were no statistically significant improvements in any evaluation parameter in sham therapy group after treatment (Table 5). Since HILT group and brace group showed significant improvements for most evaluation parameters (for brace group, see Table 6), we compared the percentage changes of parameters after 4 and 12 weeks relative to pretreatment values in both groups. Comparison of the percentage changes of all parameters both after 4 and 12 weeks relative to pretreatment values did not show a significant difference between HILT and brace groups (Table 7).
Compared to the baseline measurements, the CET thicknesses did not change significantly after treatment (after 4 and 12 weeks) in any group (Tables 3, 4, and 5). Further, the changes in CET thickness were also similar between the HILT and brace groups (Table 6). Also, cortical irregularities of the lateral epicondyle or echogenicity of the CET did not change significantly during follow-up. Comparison of the CET echogenicity and presence or absence of erosion in bony cortex of the lateral epicondyle of the three groups showed that there were no statistically significant differences between groups after treatment (data not shown). There was no correlation between ultrasonographic findings (CET thicknesses, echogenicity of the extensor tendon, and cortical irregularities of the lateral epicondyle) and clinical evaluations in the study (Table 8).
Discussion
The main findings of this study were as follows: (1) HILT and brace groups showed significant improvements for most evaluation parameters (pain (VAS) scores, grip strength, PRTEEQ scores and physical function, role limitations due to physical functioning, bodily pain, general health, and vitality subparts of SF-36) after treatment (both after 4 and 12 weeks). (2) Improvements in pain scores, grip strengths, and PRTEEQ scores of the patients with LE in HILT and brace groups were not reflected to ultrasonographic findings. (3) Comparison of the percentage changes of all parameters both after 4 and 12 weeks relative to pretreatment values did not show a significant difference between HILT and brace groups.
LLLT is a conservative treatment choice for patients with LE. Trials on the effectiveness of LLLT in LE have shown conflicting results. Earlier studies about the effectiveness of LLLT on LE showed that LLLT is not effective in improving pain, grip strength, and global improvement on the short term in lateral epicondylitis [6, 18–23]. However, according to the results of other studies and a meta-analysis, LLLT may have some beneficial effects on pain reduction and grip strength increase [7, 8, 24–26]. Contradictory results may be considered to be due to different treatment protocols regarding variables such as dose, duration, and frequency [27].
LLLT is based on the belief that laser radiation, and possibly monochromatic light, are able to alter cellular and tissue function in a manner dependent on the characteristics of light itself [28]. Since LLLT works at low irradiation intensities (low energy doses), it is assumed that any biologic effects are secondary to the direct effects of photonic radiation and are not the result of thermal processes. However, HILT uses higher-intensity laser irradiation and causes minor and slow light’s absorption by chromophores, which has been utilized. So that, some thermal processes in the target tissue may be triggered by HILT [29, 30].
A form of HILT, pulsed Nd:YAG laser therapy, has been used for a variety of diseases. Effectiveness of pulsed Nd:YAG laser therapy in pain control has been shown in ankle pain [31], subacromial impingement syndrome [32], low back pain [30, 33], and knee osteoarthritis [34, 35]. To the best of our knowledge, no study has investigated the effectiveness of HILT in patients with LE. The results of this study revealed that pulsed Nd:YAG laser therapy (HILT) is as effective as brace therapy in the treatment of these patients with respect to decreased pain and disability and improved quality of life.
The analgesic effect of HILT is based on multiple mechanisms of action, including its ability to slow the transmission of the pain stimulus and to increase the production of morphine-mimetic substances in the body [9]. LLLT may have a direct effect on nerve fibers, which could inhibit Aδ- and C-fiber transmission [36]. Also, LLLT may increase blood flow and cell metabolism [37]. We believe that the main difference between HILT and LLLT is the intensity of laser therapy. So, we may hypothesize that HILT may also have these therapeutics effects of LLLT more strongly. In addition, we may hypothesize that by applying HILT over LE, some photothermal energy may be transferred into tissue. Moreover, the photochemical and photothermic effects of HILT may stimulate collagen production within tendons and increase blood flow, vascular permeability, and cell metabolism and thus help to repair damaged tendon and remove the painful stimulus.
Traditional nonoperative therapy for lateral epicondylitis is directed toward control of inflammation, enhancement of microscopic and macroscopic tissue healing, reconditioning of the extremity, and alteration of abusive force patterns. Among conservative treatment interventions, splinting is one of the most frequently used modalities for treating lateral epicondylitis [38]. However, studies on the effectiveness of splinting in LE also have shown conflicting results. Cochrane database systematic review found that no definitive conclusions can be drawn concerning effectiveness of orthotic devices for the treatment of LE [39]. But, in a meta-analysis, Borkholder et al. reported one Sackett level 1b study and ten Sackett level 2b studies that offer early positive, but not conclusive, supporting the effectiveness of splinting lateral epicondylitis [38]. Lateral counterforce braces work by reducing the level of tension in the forearm extensors. Several trials have shown that elbow straps or sleeve orthoses have superior results in terms of relief of pain and grip strength compared with a placebo orthosis or wrist splints [40, 41] However, a meta-analysis did not find one type of brace to be better than the others [6]. In our study, patients in the brace group (group 3) used the lateral counterforce brace for LE. Significant improvements were obtained for pain (VAS) scores, grip strength, PRTEEQ scores and physical function, role limitations due to physical functioning, bodily pain, general health, and vitality subparts of SF-36 after treatment (both after 4 and 12 weeks) in this group. According to the results of the current study, lateral counterforce brace for LE is not superior to HILT therapy.
Ultrasonography has been usually used as a convenient imaging method for the diagnosis and follow-up of soft tissue disorders. From this point, we tried to observe whether we could quantify the changes also by using CET thickness measurements. However, there was no correlation between ultrasonographic findings (CET thicknesses, echogenicity of the extensor tendon, and cortical irregularities of the lateral epicondyle) and clinical findings (pain scores, disability, and quality of life) in the study. Previously, in three different studies, authors investigated whether ultrasonographic findings were associated with clinical findings of the patients with LE or not. Clarke et al. [42] found no correlation with clinical findings and thickness of the tendon in patients with LE. Zeisiq et al. [43] followed up the patients with LE after intertendinous injection therapy but could not indicate a relationship with ultrasonographic findings and clinical results. Gunduz et al [17] compared the therapeutic effects of physical therapy modalities, local corticosteroid injection, and extracorporeal shock wave treatment in LE. They found that ultrasonographic findings did not change in the first 6 months of these treatment methods. Also, our ultrasonographic findings were in line with the previous studies [17, 42, 43]. The absence of the correlation can be due to the shortness of evaluation period. Longer follow-up (more than 3 months up to 1 year) of the patients with ultrasonography may reveal a correlation between ultrasonographic findings and clinical findings. Therefore, the changes would be ensuing later than the third month posttreatment.
Currently, there is no a standardized, universally accepted program for LE treatment, and also, both treatment methods (HILT and brace) are noninvasive and painless and easy for use. So that, we wanted to investigate the effects of HILT in patients with LE and to compare these results with those of a brace or placebo HILT. Also, there is no universally accepted treatment protocol concerning number of session, duration, frequency, and dose for both HILT and brace therapies. Since both treatment groups used different regimens of treatment, HILT was applied once a day for 15 days (15 min daily) during a period of 3 weeks, while brace groups used lateral counterforce brace for a longer time (4 weeks and only removed during sleep and bathing). This may also show that HILT has an advantage in treatment duration (only 15 min a day) compared to brace therapy (during all day and removed during sleeping). If we could apply both treatment modalities with the same duration (4 weeks), we might find statistically significant differences between the groups.
The main limitations of this study are the relatively small study population and the lack of long-term (>3 months up to 1 year) follow-up results. Another limitation is that there was not any group treated with both HILT and brace therapy together. If we had such a group, we could discuss the additional effect of HILT in LE.
There are conflicting results regarding the treatment (LLLT and splinting) of LE. As a result, it is concluded that pulsed Nd:YAG laser treatment (HILT) and splinting are an effective physical therapy modality for patients with LE in reducing pain and improving disability, quality of life, and grip strength. The results of the present study are encouraging, but further studies with larger samples, longer follow-up, and possible comparisons with other conservative interventions or placebo control groups are needed to make more valid conclusion.
References
Bharti A, Avasthi S, Solanki K, Kumar S, Swaroop A, Sengar GK (2010) Clinical assessment of functional outcome in lateral epicondylitis managed by local infiltration of autologous blood. Internet J Med Update 5(1):20–24
Shiri R, Viikari-Juntura E, Varonen H, Heliovaara M (2006) Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol 164(11):1065–74
Smidt N, Lewis M, van der Windt DA, Hay EM, Bouter LM, Croft P (2006) Lateral epicondylitis in general practice: course and prognostic indicators of outcome. J Rheumatol 33(10):2053–2059
Luk JK, Tsang RC, Leung HB (2014) Lateral epicondylalgia: midlife crisis of a tendon. Hong Kong Med J 20:145–51
Brown AW, Weber DC (2000) Physical agent modalities. In: Braddom RL (ed) Physical medicine and rehabilitation. WB Saunders, Harcourt Health Sciences Company, London, pp 440–458
Bisset L, Paungmali A, Vicenzino B, Beller E (2005) A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med 39:411–422
Bjordal JM, Lopes-Martins RA, Joensen J, Couppe C, Ljunggren AE, Stergioulas A, Johnson MI (2008) A systematic review with procedural assessments and meta-analysis of low level laser therapy in lateral elbow tendinopathy (tenis elbow). BMC Musculoskelet Disord 9:75–90
Tumilty S, Munn J, McDonough S, Hurley DA, Basford JR, Baxter GD (2010) Low level laser treatment of tendinopathy: a systematic review with meta-analysis. Photomed Laser Surg 28(1):3–16
Zati A, Valent A (2006) Laser therapy in Medicine. In: Medica M (ed) Terapia Elsica: Nuove Tecnologie in Medicina Riabilitatiya, p 162–185
Garg R, Adamson GJ, Dawson PA, Shankwiler JA, Pink MM (2010) A prospective randomized study comparing a forearm strap brace versus a wrist splint for the treatment of lateral epicondylitis. J Shoulder Elbow Surg 19(4):508–12
Nirschl RP (1992) Elbow tendinosis/tennis elbow. Clin Sports Med 11:851–871
Struijs PA, Spruyt M, Assendelft WJ, van Dijk CN (2005) The predictive value of diagnostic sonography for the effectiveness of conservative treatment of tennis elbow. AJR 185:1113–1118
Bhargava AS, Eapen C, Kumar SP (2010) Grip strength measurements at two different wrist extension positions in chronic lateral epicondylitis-comparison of involved vs. uninvolved side in athletes and non athletes: a case-control study. Sports Med Arthrosc Rehabil Ther Technol 2:22
Puh U (2010) Age-related and sex-related differences in hand and pinch grip strength in adults. Int J Rehabil Res 33(1):4–11
Cacchio A, Necozione S, MacDermid JC, Rompe JD, Maffulli N, di Orio F, Santilli V, Paoloni M (2012) Cross-cultural adaptation and measurement properties of the italian version of the Patient-Rated Tennis Elbow Evaluation (PRTEE) questionnaire. Phys Ther 92(8):1036–45
Wang G, Gao Q, Hou J, Li J (2014) Effects of Temperature on chronic trapezius myofascial pain syndrome during dry needling therapy. Evid Based Complement Alternat Med 2014:638268
Gunduz R, Malas FU, Borman P, Kocaoglu S, Ozcakar L (2012) Physical therapy, corticosteroid injection, and extracorporeal shock wave treatment in lateral epicondylitis Clinical and ultrasonographical comparison. Clin Rheumatol 31:807–812
Stasinopoulos DI, Johnson MI (2005) Effectiveness of low-level laser therapy for lateral elbow tendinopathy. Photomed Laser Surg 23:425–30
Basford JR, Sheffield CG, Kathryn RC (2000) Laser therapy: a randomized, controlled trial of the effects of low intensity Nd:YAG laser irradiation on lateral epicondylitis. Arch Phys Med Rehabil 81:1504–10
Haker E, Lundeberg T (1990) Laser treatment applied to acupuncture points in lateral humeral epicondylalgia. A double-blind study. Pain 43:243–7
Maher S (2006) Clinical question: is low-level laser therapy effective in the management of lateral epicondylitis? Phys Ther 86:1161–7
Krasheninnikoff M, Ellitsgaard N, Rogvi-Hansen B, Zeuthen A, Harder K, Larsen R, Gaardbo H (1994) No effect of low power laser in lateral epicondylitis. Scand J Rheumatol 23:260–3
Borman P, Seckin U, Calıskan Z, Yucel M (2000) Comparison of the efficacy of ultrasound and laser in the treatment of lateral epicondylitis. J Rheum Med Rehab 11:265–8
Oken O, Kahraman Y, Ayhan F, Canpolat S, Yorgancioglu ZR, Oken OF (2008) The short-term efficacy of laser, brace, and ultrasound treatment in lateral epicondylitis: a prospective, randomized, controlled trial. J Hand Ther 21(1):63–7, quiz 68
Stergioulas A (2007) Effects of low-level laser and plyometric exercises in the treatment of lateral epicondylitis. Photomed Laser Surg 25(3):205–13
Lam LK, Cheing GL (2007) Effects of 904-nm low-level laser therapy in the management of lateral epicondylitis: a randomized controlled trial. Photomed Laser Surg 25(2):65–71
Emanet SK, Altan LI, Yurtkuran M (2010) Investigation of the effect of GaAs laser therapy on lateral epicondylitis. Photomed Laser Surg 28(3):397–403
Basford JR (1995) Low intensity laser therapy:stil not an established clinical tool. Laser Surg Med 16:331–42
Ohshiro T, Calderhead R (1991) Development of low reactive-level laser therapy and its present status. J Clin Laser Med Surg 9:267–275
Fiore P, Panza F, Cassatella G, Russo A, Frisardi V, Solfrizzi V, Ranieri M, Di Teo L, Santamato A (2011) Short-term effects of high-intensity laser therapy versus ultrasound therapy in the treatment of low back pain: a randomized controlled trial. Eur J Phys Rehabil Med 47(3):367–73
Saggini R, Bellomo RG, Cancelli F (2009) Hilterapia and chronic ankle pain syndromes. Abstract from Energy for Health. Int J İnf Sci Cult 3:37–38
Santamato A, Solfrizzi V, Panza F, Tondi G, Frisardi V, Leggin BG, Ranieri M, Fiore P (2009) Short-term effects of high-intensity laser therapy versus ultrasound therapy in the treatment of people with subacromial impingement syndrome: a randomized clinical trial. Phys Ther 89:643–652
Alayat MSM, Atya AM, Ali MME, Shosha TM (2014) Long-term effect of high-intensity laser therapy in the treatment of patients with chronic low back pain: a randomized blinded placebo-controlled trial. Lasers Med Sci 29(3):1065–73
Stiglić-Rogoznica N, Stamenković D, Frlan-Vrgoc L, Avancini-Dobrović V, Vrbanić TS (2011) Analgesic effect of high intensity laser therapy in knee osteoarthritis. Coll Antropol 35(2):183–5
Kheshie AR, Alayat MSM, Ali MME (2014) High-intensity versus low-level laser therapy in the treatment of patients with knee osteoarthritis: a randomized controlled trial. Lasers Med Sci 29(4):1371–6
Chow R, Armati P, Laakso EL, Bjordal JM, Baxter GD (2011) Inhibitory effects of laser irradiation on peripheralmammalian nerves and relevance to analgesic effects: a systematic review. Photomed Laser Surg 29(6):365–81
Kujawa J, Zavodnik L, Zavodnik I, Buko V, Lapshyna A, Bryszewska M (2004) Effect of low-intensity (3.75–25 J/cm2) near-infrared (810 nm) laser radiation on red blood cell ATPase activities and membrane structure. J Clin Laser Med Surg 22(2):111–7
Borkholder CD, Hill VA, Fess EE (2004) The efficacy of splinting for lateral epicondylitis: a systematic review. J Hand Ther 17(2):181–99
Struijs PA, Smidt N, Arola H, Dijk vC, Buchbinder R, Assendelft WJ (2002) Orthotic devices for the treatment of tennis elbow. Cochrane Database Syst Rev (1):CD001821
Jafarian FS, Demneh ES, Tyson SF (2009) The immediate effect of orthotic management on grip strength of patients with lateral epicondylosis. J Orthop Sports Phys Ther 39:484–489
Ahmad Z, Siddiqui N, Malik SS, Abdus-Samee M, Tytherleigh-Strong G, Rushton N (2013) Lateral epicondylitis: a review of pathology and management. Bone Joint J 95-B(9):1158–64
Clarke AW, Ahmad M, Curtis M, Connell DA (2010) Lateral elbow tendinopathy: correlation of ultrasound findings with pain and functional disability. Am J Sports Med 38(6):1209–14
Zeisiq E, Fahlstorm M, Olberg L, Alfredson H (2010) A two year sonographic follow-up after intratendinous injection therapy in patients with tennis elbow. Br J Sports Med 44:584–587
Conflict of interest
The authors report no conflict of interest.
Source of funding
No funding was received for this study
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dundar, U., Turkmen, U., Toktas, H. et al. Effectiveness of high-intensity laser therapy and splinting in lateral epicondylitis; a prospective, randomized, controlled study. Lasers Med Sci 30, 1097–1107 (2015). https://doi.org/10.1007/s10103-015-1716-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-015-1716-7