Abstract
The effects of balneotherapy on chronic shoulder pain were studied. In this single-blind, randomized, follow-up study involving 46 patients with chronic shoulder pain, one group of patients received physiotherapy—exercise and transcutaneous electrical nerve stimulation—and the other group received balneotherapy in addition to physiotherapy for 4 weeks on 15 occasions. The following parameters were recorded before treatment (at week 0) and after treatment (at weeks 4, 7, and 13): Shoulder Pain and Disability Index (SPADI), the Short Form (36) Health Survey (SF-36) and EuroQuol-5D (EQ-5D) quality of life questionnaires, pain at rest and on movement on the visual analog scale (VAS), and active and passive range of motion. The SPADI pain, function, and total scores and the VAS scores at rest and on movement significantly improved in both groups after treatments. A greater improvement was observed in the balneotherapy group compared to the control group; regarding some parameters (VAS score on movement and SPADI function score at visit 2; VAS score at rest at visits 3 and 4), the difference between the groups was significant. The improvement of SF-36 and EQ-5D quality of life scores and the active range of motion was more pronounced in the balneotherapy group, the difference between the groups was not significant, except for EQ-5D at visit 2. Improvement of passive range of motion was not significant. Balneotherapy may have a beneficial effect on the clinical parameters and quality of life of patients with chronic shoulder pain. The number of patients should be increased.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Balneotherapy has been defined recently as the use of natural mineral waters, muds/peloids, and natural gases for therapy, prevention, and rehabilitation. The possible methods of use are immersion in mineral water, mud, and gases, drinking of mineral water, and inhalation of mineral waters and gases. Balneotherapy is traditionally used for the treatment of musculoskeletal disorders in many European and non-European countries [1]. The primary goal of balneotherapy is the treatment of degenerative musculoskeletal disorders. Based on the results of previous studies, balneotherapy has favorable effects on knee osteoarthritis [2, 3], chronic low back pain [4–6], hand osteoarthritis [7], and fibromyalgia [8].
In addition to low back and neck pain, shoulder disease (SD) is the third most common musculoskeletal disorder patients seek medical care for [9]. The estimated yearly incidence of SD in the USA is up to 7 %, its yearly prevalence in different countries is between 20 and 51 %, and lifetime prevalence is approximately 10 % in the average adult population [9, 10]. In 40 % of patients attending primary health care for a new episode of shoulder pain, symptoms can last even up to 12 months [9, 10].
The painful limitation of shoulder motion affects hand and arm motion as well; therefore, it significantly influences work performance and everyday activities as well as the quality of life. Therefore, the treatment of patients with shoulder pain has major social and health economic implications [10, 11].
The diagnosis and classification of SD is not uniform [9, 11]. Shoulder pain is caused by periarticular, glenohumeral, and regional (other than shoulder) disorders [10–12].
Biceps tendinitis is most often associated with other surrounding shoulder pathologies such as degenerative rotator cuff lesions and impingement syndrome as a secondary process. Primary tendinitis is rare and has been estimated to represent about 5 % of the cases [13].
Treating SD is a challenge also. The aim of the treatment is to decrease pain and increase function [10]. Several accepted conservative treatment options exist for shoulder pain. These include pharmacotherapy (analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), oral steroids, and steroid injections), physiotherapy (including exercise therapy and the application of physical modalities), mobilization, manipulation, and health education. In cases resistant for conservative therapy, hydrodilatation and surgery may be considered [10, 12].
Due to the diagnostic and classification difficulties, no uniform, specific treatment protocol exists [10, 12]. According to the meta-analysis of Gaujoux-Viala, efficacy of local steroid treatment is equal to that of NSAIDs in the acute and subacute stage of shoulder tendinitis: compared to other treatments (physiotherapy, wait and see, placebo), it decreases pain and improves function. However, this effect is confirmed only in studies with short term, and no long-term benefit was shown [14].
It is important to note that due to gastrointestinal side effects, pharmacological treatment (particularly NSAID therapy) has its limitations with significant financial and health economic consequences [15].
Several systematic reviews and meta-analyses have proven the pain-reducing and function-improving effect of exercise treatment in chronic shoulder pain [16–19]. The efficacy of transcutaneous electrical nerve stimulation (TENS) in shoulder pain is not proved [20].
In some European and Asian countries, balneotherapy is traditionally and widely used in the treatment of chronic shoulder pain [1]. However, we have data only from one Turkish study showing the beneficial effects of hot mud packs in subacromial impingement syndrome [21]. The effect of mineral water bathing on chronic shoulder pain has not yet been studied.
Therefore, the aim of our study was to investigate the effects of balneotherapy on chronic shoulder pain. Our primary objective was to find out whether balneotherapy has an adjuvant beneficial effect on the clinical parameters of patients suffering from chronic shoulder pain compared to the control group. Our secondary objective was to evaluate the effect of clinical improvement on the quality of life from the baseline and compared to the control group.
Protocol and study parameters
Design
In this randomized, controlled, follow-up study, we evaluated the effects of balneotherapy plus exercise versus exercise alone on chronic shoulder pain in two patient groups. Both groups received TENS treatment, as probably a placebo for shoulder pain in lack of evidence.
Participants
This study was conducted at the Department of Rheumatology and Physiotherapy of the Józsefváros Municipal Health Service in Budapest (center 1) and at the Musculosceletal Rehabilitation Centre in Mezőkövesd (center 2), Hungary.
Patients with the following criteria were enrolled to the study: outpatients with chronic shoulder pain, men and women between 30 and 75 years of age, complaints present for at least 2 months, at least mild shoulder pain (25 on the visual analog scale (VAS) scale) on movement, and tenderness along the short or long head of the biceps brachii muscle possibly causing the complaints. Before enrollment, anteroposterior comparative shoulder X-ray and shoulder ultrasound examinations were performed.
Exclusion criteria were: acute shoulder pain; rotator cuff tear; glenohumeral disorders (inflammatory arthritis, osteoarthritis, osteonecrosis, cuff arthropathy, septic arthritis, adhesive capsulitis, glenohumeral instability), regional disorders (e.g., cervical radiculopathy, brachial neuritis, nerve entrapment syndrome, sternoclavicular arthritis, reflex sympathetic dystrophy, and neoplasms); shoulder pain probably caused by internal organ disease; previous shoulder surgery; previous shoulder fracture; complaints caused by obvious trauma; application of local steroid injection on the shoulder within 3 months prior to the study treatment and within 1 months prior to the study treatment on other body parts; balneotherapy within 2 months prior to the treatment; general contraindications of balneotherapy; TENS therapy was allowed up to 2 weeks prior to treatment; and exercises were allowed.
The study participants were patients under regular outpatient care recruited according to the study protocol by the rheumatologists of the Józsefváros Municipal Health Service in Budapest and the Musculosceletal Rehabilitation Centre in Mezőkövesd. Exercise therapy and TENS therapy were performed at the local Physiotherapy Department. Balneotherapy took place at the Budapest Spa Plc. Széchenyi Spa in Budapest and at the Zsóry Spa in Mezőkövesd. Study participants received written information, and they signed an informed consent form before the study. The study was approved by the Scientific and Research Ethics Committee (TUKEB).
Intervention
One group received individual, physiotherapist-led exercise therapy and TENS therapy for painful shoulder joint two to three times a week for 4 weeks on a total of 10 occasions, and the other group received the same treatment plus balneotherapy. Balneotherapy involved bathing in a 120-cm deep, 32 °C water for 4 weeks in a total of 15 sessions, for 30 min per occasion. During balneotherapy sessions, patients were allowed to move, swim, stand, and sit in the water. Both mineral waters contain a significant amount of sodium, calcium, hydrogen carbonate, and sulfate.
The therapists who supervised the exercise were trained. Exercise therapy was performed on the basis of an agreement reached prior to the study between the physiotherapists and was adjusted to the individual status of the patient. Exercises included passive mobilization, gradual introduction of active exercises (muscle strengthening and joint mobilization), and active joint exercises taking into account the patient's actual range of motion. Patients received educational material, which included advices and a series of exercises to be done at home for at least 5 days a week. TENS was applied on the anterior and posterior aspects of the joint for 15 min with a mean frequency of 100 Hz and with 15 mA amplitude.
Adherence of patients to the treatment was registered in a checklist signed by the physicians on each occasion. The signed checklist of balneotherapy was controlled by the rheumatologists supervising the balneotherapy after the last balneotherapy session (one person in each center), and the signed checklist of the exercise and TENS was controlled at visit 2 (one person in each center). The patients were asked not to have any other concomitant treatments, and if they had, they were asked to report it at the visits.
Outcomes
Disease assessment was performed before treatment (week 0), after the last treatment session (week 4), then 3 and 10 weeks after the end of treatment (weeks 7 and 14, respectively). Disease assessments included, as the primary objective, the evaluation of the VAS pain scores on movement and at rest, and the completion of the Shoulder Pain and Disability Index (SPADI) questionnaire.
The SPADI was developed to measure current shoulder pain and disability [22, 23]. Initially, it was tested in a mix diagnosis group of patients reporting shoulder pain [22] and has since been used, among others, in rotator cuff disease [23]. The minimal clinically important difference has been reported to be 8 points, and the minimal detectable change (MDC 95 %) is 18 points [23]. The questionnaire is validated in Hungarian in chronic shoulder pain [24].
As secondary objective, the completion of the Short Form (36) Health Survey (SF-36) and EuroQol-5D quality of life questionnaires were performed. All questionnaires were self-reported. Active shoulder girdle range of motion and passive glenohumeral range of motion were measured by a goniometer and the results were recorded. The assessors were trained. Both assessors (each one in each center) carried out examinations on the basis of an agreement reached prior to the study.
In addition to the above, a detailed medical history was taken at each visit. At the same time, inclusion and exclusion criteria were checked, and possible side effects were recorded.
Randomization and blinding
The person randomizing the patients used a computer program for the randomization, and made a random number order. He received patient information via e-mail. Randomization was stratified by each center, separated. After randomization, an independent person assigned the patients to the appropriate group. The independent investigators blinded to the treatment on the basis of an agreement reached prior to the study examined the patients before treatment, at the end of treatment, and during the follow-up visits. As the patient cannot be blinded for the treatment, they were expressly asked not to tell the assessor in which group they were treated. The patients were examined by the same physician, which means one person in each center.
The independent physicians supervising the treatment were available during the treatments and they observed the possible side effects. The side effects of balneotherapy were supposed to be evaluated by the physicians supervising the treatments and finally by the rheumatologists working in the baths (one person in each center) by means of a list (a blank sheet) on which, in case of the emergence of any side effect, the emergence was indicated (description of the side effect). The side effects of physiotherapy were evaluated by the physicians and finally by the rheumatologists supervising the treatments (one person in each center) by means, again, of a list (a blank sheet) on which, in case of the emergence of any side effect, the emergence was indicated (description of the side effect). Statistical analysis was performed by an independent person.
Statistical analysis
Statistical analysis was performed by using IBM SPSS Statistics 20. Distribution was assessed by the Kolmogorov-Smirnov test. Nonparametric methods were used in statistical calculations, due to the sample size. Data were analyzed by Mann-Whitney test and Friedman test. Bonferroni correction was made; the level of significance was calculated by dividing 0.05 by the number of the independent variables in the tests. So, the level of significance given by Bonferroni correction was 0.025 for VAS pain scores on movement and at rest, for SPADI and for EuroQuol-5D quality of life questionnaires, the level of significance given by Bonferroni correction was 0.006 for SF-36 quality of life questionnaires, and 0.005 for clinical examination (active shoulder girdle range of motion and passive glenohumeral joint range of motion).
The effect sizes between the two groups were estimated with a 95 % confidence interval (CI). Regarding the Friedman test, the concordance was calculated and given by Kendall's coefficient (w). The results were evaluated by intention-to-treat analysis (ITT).
Results
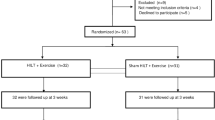
Fifty-four patients were assesed for eligibility, four patients did not meet inclusion criteria, and four patients declined to participate. Forty-six patients were randomized: 23 patients to the balneotherapy group (20 patients in center 1; 3 patients in center 2) and 23 patients to the control group (20 patients in center 1; 3 patients in center 2).
This study was conducted between December 2010 and June 2013. The patients were recruited continuously from December 2010 to March 2013. Participants attended visits at baseline at weeks 4, 7, and 13.
Patients participated in at least 80 % of the treatment sessions. During the follow-up period, one patient in the balneotherapy group required periarticular steroid therapy for increasing pain at visit 3 and therefore this patient was excluded from the study. Due to issues with compliance, one patient in the balneotherapy group and four patients in the control group did not attend visit 4. No side effects were observed during the treatment period or the follow-up period. All patient data were analyzed according to the intent-to-treat principle (Fig. 1). The statistical analysis performed was planned; no other statistical analysis was performed.
At the beginning of the study, the demographic characteristics and measured parameters of the two groups were comparable. This study included 17 male and 29 female patients. The average age was 59.7 ± 8.3 and 57.4 ± 11.1 years in the balneotherapy and control groups, respectively.
Tenderness was noted in all patients along the initial segment of the long head of the biceps brachii muscle. In 30 of the 46 patients (17 patients in the balneotherapy group and 13 patients in the control group), ultrasonography confirmed tendovaginitis of the long head of the biceps brachii muscle. Ultrasound examination showed rotator cuff tendinopathy in 12 patients (nine patients in the balneotherapy group and three patients in the control group), and chronic subacromial bursitis and/or subdeltoid bursitis in 13 patients (five patients in the balneotherapy group and eight patients in the control group). Physical examination revealed impingement syndrome in 17 patients (eight patients in the balneotherapy group and nine patients in the control group). Out of these patients, ultrasonography showed rotator cuff tendinopathy in six patients (four patients in the balneotherapy group and two patients in the control group), chronic subacromial bursitis and/or deltoid bursitis in six patients (one patients in the balneotherapy group and five patients in the control group), and long head tendinopathy of the biceps brachii muscle in nine patients (seven patients in the balneotherapy group and two patients in the control group; Table 1).
The SPADI total pain, total disability, and total scores significantly improved from baseline to the end of treatment in both groups, and further improvement was observed during the follow-up period. The improvement was greater in the balneotherapy group. A significant difference was seen between the two groups in the SPADI total disability score at visit 2 (Table 2).
Shoulder pain at rest and on movement significantly improved from baseline to the end of treatment in both groups, and further improvement was observed during the follow-up period. Pain decreased more pronounced in the balneotherapy group than in the control group. A significant difference in pain at rest was seen between the two groups at visits 3 and 4 and in pain on movement at visit 2 (Table 2).
The role limitations due to physical health, energy/fatigue, and pain domains measured by the SF-36 quality of life questionnaire significantly improved in both groups. This improvement was greater in the balneotherapy group compared to the control group. The difference was not significant. Physical functioning, emotional well being, and general health improved significantly in the balneotherapy group only; the difference between the two groups was not significant. The improvement of the role limitations due to emotional problems and social functioning was not significant in any of the groups (Table 3).
The EuroQuol-5D (EQ-5D) index and VAS general health score of the EuroQol-5D quality of life questionnaire significantly improved in both groups. Improvement was more pronounced in the balneotherapy group. The difference between the two groups was not significant except for EQ-5D index at visit 2 (Table 4).
Active anteflexion and active retroflexion significantly improved in both groups. Active abduction and active outer rotation improved significantly in the balneotherapy group only. The improvement of the active adduction was not significant in any of the groups. The difference in the active range of motion was not significant between the two groups at any visits (Table 5). Regarding the passive glenohumeral joint range of motion, the improvement was not significant in any of the groups after treatment (Table 5).
Discussion
Our study showed that balneotherapy may have a beneficial effect on the clinical parameters and quality of life of patients with chronic shoulder pain.
Previous reports have demonstrated the beneficial effects of exercise therapy [16–19]. In our study, this benefit is observed in the changes of the control group. According to the results of our study, balneotherapy combined with exercises and TENS provided better results regarding pain, shoulder function, and quality of life than exercises plus TENS, notwithstanding the statistical power of the study was low.
Despite the fact that balneotherapy is a widely used therapeutic method in the treatment of chronic shoulder pain, our study is the first randomized, controlled study, which evaluated the efficacy of mineral water treatment in patients with chronic shoulder pain.
Until now, only one uncontrolled Turkish balneotherapy study has been published about evaluating the effects of hot mud packs on shoulder pain. In this study, Sen et al. enrolled 29 patients suffering from subacromial impingement syndrome for at least 3 months. Patients received 45 °C mud packs on their painful shoulders for 30 min once a day for 15 days. A significant improvement in pain was observed during rest, night, and activity as well as in joint function [21].
The treatment of chronic shoulder pain has not been established yet. Evidence exist that exercise decreases pain and improves function in chronic periarticular shoulder pain [16–19]. However, little data is available concerning the effect of electrical therapy [20].
Kromer et al. published in 2009 that moderate evidence exists that physiotherapist-led exercises and surgery have similar efficacy in the treatment of impingement syndrome in the long term. These data indicate the importance of conservative therapy before surgery. Home-based exercise program is as effective as combined physiotherapy (exercise: centering training, mobilization; electric therapy) in the short and long term. Also, there is moderate evidence that manual therapy combined with exercise is superior in pain relief compared to exercise alone. Moderate evidence exists that passive treatments (ultrasound, magnetotherapy, and laser) are not effective compared to placebo [18].
Marinko et al. meta-analyzed on 17 randomized controlled trials (RCTs) involving patients with painful shoulder. Exercise had positive effects on pain and function compared to other treatments. However, the change in range of motion was inconclusive [17].
The systematic review of Hanratty et al. published in 2012 included 16 RCTs involving 1,162 patients. Strong evidence was shown that exercise improved pain and function in subacromial impingement syndrome in the short term. There is moderate evidence that exercise has positive effects on mental status in the short term and improves physical function in the long term. Based on the results of the meta-analysis of six studies, the authors concluded that exercise had small positive effect on rotator cuff muscle strength in the short term and small positive effect on long-term function [16].
TENS therapy is widely used in the treatment of rheumatic conditions (e.g., chronic low back pain and osteoarthritis of the knee) and nonrheumatic disorders (e.g., diabetic neuropathy and cancer pain); the efficacy of TENS is still controversial [25].
In a study involving 40 patients with rotator cuff tendinitis, Eyigor et al. found that although intra-articular steroid decreased pain and improved function more pronouncedly compared to TENS therapy especially in the first weeks of treatment, TENS therapy alone was also effective in improving activity, function, and quality of life in the long term [20].
Several authors have studied the effect of mechanism of balneotherapy on musculoskeletal diseases. The mechanical and heat effects of hydrotherapy predominate during balneotherapy as well [26]. The gate control theory of pain acting via heat receptors and mechanoreceptors has been described [27]. Under hydrostatic pressure, circulation becomes centralized, which via the stretching of the volume receptors leads to increased diuresis, and finally to decrease of joint swelling and edemas [26, 28]. During immersion, circulation of the deep muscle structures and oxygen supply of the tissues increase, which may facilitate the healing of muscle, joint, or bone injuries [29]. Data exist that during water immersion, neuromuscular function is modified compared to the non-immersed control; however, some results are inconsistent [30, 31].
Several authors have studied the role and the mechanism of heat therapy in decreasing pain and inflammation [26, 32, 33]. In response to heat, elasticity of collagen-rich tissues increases, muscle spasm decreases (which presumably reduce pain), and joint function improves [26]. Heat may also be able to influence the hypothalamic adrenal axis, and may increase serum cortisol, adrenocorticotropic hormone, and beta-endorphin levels, which is followed by pain reduction in fibromyalgia syndrome [34].
In our study, water temperature was in the thermoneutral zone; therefore probably the mechanical effects were predominant. Inferring from other studies, balneotherapy modified the level of inflammatory mediators (e.g., interleukin-1 alpha, leukotriene B4, prostaglandin E2, tumor necrosis factor alpha, insulin-like growth factor 1, and transforming growth factor beta) [26, 35], and had a positive effect on the markers of antioxidant status [36–38] and cartilage degradation (e.g., adiponectin and matrix metallopeptidase 3) [26, 39].
Mineral water may also have a specific chemical effect. Several authors have described the significantly better effects of balneotherapy on pain, mobility, and quality of life compared to hydrotherapy in knee [40–42] and hand osteoarthritis [7] and chronic low back pain [4–6].
There is hardly any data about the transcutaneous absorption of mineral water components [43]. It has already been reported that hydro- and balneotherapy have beneficial effects on anxiety, depression, and mood. It may also play a role in the alterations of pain experience and in the improvement of quality of life [44].
TENS uses analgesic currents, and while its mechanism of action is not completely understood, it is thought that it serves to release endogenous opiates in specific areas of the central nervous system [45].
Since no uniform diagnostic and classification criteria exist, we established arbitrary criteria. Based on the inclusion and exclusion criteria, the X-ray and ultrasound examinations made the establishment of relatively homogeneous patient groups. This study is considered to be a pilot study. According to its results, with sample size calculation and determination of the main criteria for a future study, the expansion of the number of the patients would be promising.
Limitation of the study
A single-blind method was used; therefore, the patients knew which treatment they received. Being all self-reported questionnaires, the assessor was the patient and blinding of assessor was not possible and the influence of the placebo effect could be increased. The lack of blinding of therapists may overestimate the treatment effect. The procedure evaluating the side effects might be able to underestimate it in both groups. In spite of the fact that concomitant treatments were not reported, it is difficult to evaluate it. Continuous outcome can lead to a significant placebo effect. Being a small study, the treatment effect might be overestimated. The effect of balneotherapy and hydrotherapy cannot be distinguished in our study. Expansion of the number of patients would be promising.
Conclusions
As primary objective of the pilot study, we have shown that balneotherapy combined with exercise and TENS therapy may provide significantly better results than exercise and TENS alone on the clinical parameters of patients suffering from chronic shoulder pain with a possible improvement in the quality of life of patients as well. Based on our results, we can conclude that balneotherapy may be a possible therapeutic option in the treatment of chronic shoulder pain. The number of patients should be increased.
References
Gutenbrunner C, Bender T, Cantista P, Karagülle Z (2010) A proposal for a worldwide definition of health resort medicine, balneology, medical hydrology and climatology. Int J Biometeorol 54:495–507
Harzy T, Ghani N, Akasbi N, Bono W, Nejjari C (2009) Short- and long-term therapeutic effects of thermal mineral waters in knee osteoarthritis: a systematic review of randomized controlled trials. Clin Rheumatol 28:501–507
Forestier R, Desfour H, Tessier JM, Françon A, Foote AM, Genty C, Rolland C, Roques CF, Bosson JL (2009) Spa therapy in the treatment of knee osteoarthritis: a large randomised multicentre trial. Ann Rheum Dis 69:660–665
Balogh Z, Ordögh J, Gász A, Német L, Bender T (2005) Effectiveness of balneotherapy in chronic low back pain—a randomized single-blind controlled follow-up study. Forsch Komplementarmed Klass Naturheilkd 12:196–201
Kulisch A, Bender T, Németh A, Szekeres L (2009) Effect of thermal water and adjunctive electrotherapy on chronic low back pain: a double-blind, randomized, follow-up study. J Rehabil Med 41:73–79
Tefner IK, Németh A, Lászlófi A, Kis T, Gyetvai G, Bender T (2012) The effect of spa therapy in chronic low back pain: a randomized controlled, single-blind, follow-up study. Rheumatol Int 32:3163–3169
Kovács C, Pecze M, Tihanyi Á, Kovács L, Balogh S, Bender T (2012) The effect of sulphurous water in patients with osteoarthritis of hand. Double-blind, randomized, controlled follow-up study. Clin Rheumatol 31:1437–1442
Guidelli GM, Tenti S, De Nobili E, Fioravanti A (2012) Fibromyalgia syndrome and spa therapy: myth or reality? Clin Med Insights Arthritis Musculoskelet Disord 5:19–26
van der Heijden GJ (1999) Shoulder disorders: a state-of-the-art review. Baillieres Best Pract Res Clin Rheumatol 13:287–309
Croft P, Pope D, Silman A (1996) The clinical course of shoulder pain: prospective cohort study in primary care. Primary Care Rheumatology Society Shoulder Study Group. BMJ 313:601–602
Brox JI (2003) Regional musculoskeletal conditions: shoulder pain. Review. Best Pract Res Clin Rheumatol 17:33–56
Baring T, Emery R, Reilly P (2007) Management of rotator cuff disease: specific treatment for specific disorders. Review. Best Pract Res Clin Rheumatol 21:279–294
Elser F, Braun S, Dewing CB, Giphart JE, Millett PJ (2011) Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy 27:581–592
Gaujoux-Viala C, Dougados M, Gossec L (2009) Efficacy and safety of steroid injections for shoulder and elbow tendonitis: a meta-analysis of randomised controlled trials. Ann Rheum Dis 68:1843–1849
Smalley WE, Griffin MR, Fought RL, Ray WA (1996) Excess costs from gastrointestinal disease associated with nonsteroidal anti-inflammatory drugs. J Gen Intern Med 11:461–469
Hanratty CE, McVeigh JG, Kerr DP, Basford JR, Finch MB, Pendleton A, Sim J (2012) The effectiveness of physiotherapy exercises in subacromial impingement syndrome: a systematic review and meta-analysis. Semin Arthritis Rheum 42:297–316
Marinko LN, Chacko JM, Dalton D, Chacko CC (2011) The effectiveness of therapeutic exercise for painful shoulder conditions: a meta-analysis. J Shoulder Elbow Surg 20:1351–1359
Kromer TO, Tautenhahn UG, de Bie RA, Staal JB, Bastiaenen CH (2009) Effects of physiotherapy in patients with shoulder impidgement syndrome: a systematic review of the literature. J Rehabil Med 41:870–880
Kuhn JE (2009) Exercise in the treatment of rotator cuff impidgement: a systematic review and a synthesized evidence-based rehabilitation protocol. J Shoulder Elbow Surgery 18:138–160
Eyigor C, Eyigor S, Kivilcim Korkmaz O (2010) Are intra-articular corticosteroid injections better than conventional TENS in treatment of rotator cuff tendinitis in the short run? A randomized study. Eur J Phys Rehabil Med 46:315–324
Sen U, Karagulle M, Erkorkmaz U (2010) The efficacy of balneotherapy in the patients with subacromial impingement syndrome. Turkiye Klinikleri Tip Bilimleri Dergisi 30:906–913
Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y (1991) Development of a Shoulder Pain and Disability Index. Arthritis Care Res 4:143–149
Breckenridge JD, McAuley JH (2011) Shoulder Pain and Disability Index (SPADI). J Physiother 57:197
Kovács Cs, Tefner IK, Bender T, Hodosi K (2013) A váll fájdalmának és funkciójának értékelésére alkalmas SPADI kérdőív hazai adaptálása és validálása. Balneológia, Gyógyfürdőügy, Gyógyidegenforgalom 2:99 P
Nnoaham KE, Kumbang J (2008) Transcutaneous electrical nerve stimulation (TENS) for chronic pain. Cochrane Database Syst Rev 16(3), CD003222
Fioravanti A, Cantarini L, Guidelli GM, Galeazzi M (2011) Mechanisms of action of spa therapies in rheumatic diseases: what scientific evidence is there? Review. Rheumatol Int 31:1–8
Melzack R, Wall PD (1965) Pain mechanism: a new theory. Science 150:971–979
O'Hare JP, Heywood A, Summerhayes C, Lunn G, Evans JM, Walters G, Corrall RJ, Dieppe PA (1985) Observations on the effect of immersion in bath spa water. Brit Med J 291:1747–1751
Becker BE (2009) Aquatic therapy: scientific foundations and clinical rehabilitation applications. PM R 1:859–872
Pöynönen T, Avela J (2002) Effect of head out water immersion on neuromuscular function of the plantarflexor muscles. Aviat Space Environ Med 73:1215–1218
Kalpakcioglu B, Candir F, Bernateck M, Gutenbrunner C, Fischer MJ (2009) Does local immersion in thermo-neutral bath influence surface EMG measurements? Results of an experimental trial. J Elektromyogr Kinesiol 19:550–553
Oosterveld FG, Rasker JJ (1994) Treating arthritis with locally applied heat or cold. Semin Arthritis Rheum 24:82–90
Bender T, Karagülle Z, Bálint GP, Gutenbrunner C, Bálint PV, Sukenik S (2005) Hydrotherapy, balneotherapy, and spa treatment in pain management. Rheumatol Int 25:220–224
Bellometti S, Galzigna L (1999) Function of the hypothalamic adrenal axis in patients with fibromyalgia syndrome undergoing mud-pack treatment. Int J Clin Pharmacol Res 19:27–33
Ardiç F, Ozgen M, Aybek H, Rota S, Cubukçu D, Gökgöz A (2007) Effects of balneotherapy on serum IL-1, PGE2 and LTB4 levels in fibromyalgia patients. Rheumatol Int 27:441–446
Ekmekcioglu C, Strauss-Blasche G, Holzer F, Marktl W (2002) Effect of sulfur baths on antioxidative defense systems, peroxide concentrations and lipid levels in patients with degenerative osteoarthritis. Forsch Komplementarmed Klass Naturheilkd 9:216–220
Bender T, Bariska J, Vághy R, Gomez R, Kovács I (2007) Effect of balneotherapy on the antioxidant system—a controlled pilot study. Arch Med Res 38:86–89
Dogliotti G, Galliera E, Iorio E, De Bernardi Di Valserra M, Solimene U, Corsi MM (2011) Effect of immersion in CO2-enriched water on free radical release and total antioxidant status in peripheral arterial occlusive disease. Int Angiol 30:12–17
Fioravanti A, Cantarini L, Bacarelli MR, de Lalla A, Ceccatelli L, Blardi P (2011) Effects of spa therapy on serum leptin and adiponectin levels in patients with knee osteoarthritis. Rheumatol Int 31:879–882
Bálint GP, Buchanan WW, Adám A, Ratkó I, Poór L, Bálint PV, Somos E, Tefner I, Bender T (2007) The effect of the thermal mineral water of Nagybaracska on patients with knee joint osteoarthritis—a double blind study. Clin Rheumatol 26:890–894
Yurtkuran M, Yurtkuran M, Alp A, Nasircilar A, Bingöl U, Altan L, Sarpdere G (2006) Balneotherapy and tap water therapy in the treatment of knee osteoarthritis. Rheumatol Int 27:19–27
Sherman G, Zeller L, Avriel A, Friger M, Harari M, Sukenik S (2009) Intermittent balneotherapy at the Dead Sea area for patients with kneeosteoarthritis. Isr Med Assoc J 11:88–93
Shani J, Barak S, Levi D, Ram M, Schachner ER, Schlesinger T, Robberecht H, Van Grieken R, Avrach WW (1985) Skin penetration of minerals in psoriatics and guinea-pigs bathing in hypertonic salt solutions. Pharmacol Res Commun 17:501–512
Dubois O, Salamon R, Germain C, Poirier MF, Vaugeois C, Banwarth B, Mouaffak F, Galinowski A, Olié JP (2010) Balneotherapy versus paroxetine in the treatment of generalized anxiety disorder. Complement Ther Med 18:1–7
Sluka KA, Walsh D (2003) Transcutaneous electrical nerve stimulation: basic science mechanisms and clinical effectiveness. J Pain 4:109–121
Acknowledgments
We would like to thank Ms. Katalin Hodosi (Institute for Internal Medicine, Medical and Health Science Centre, University of Debrecen, Debrecen, Hungary) for the statistical analysis and Ms. Dorottya Molnar and Mrs. Krisztina Acs-Lenart (Musculoskeletal Rehabilitation Center, Mezőkövesd) for their physiotherapy work. Géza Bálint is warmly acknowledged for his useful comments and suggestions.
Conflict of interest
Regarding material costs, this study was sponsored by the Foundation for the Patients of Musculosceletal Rehabilitation Center of Mezőkövesd (Mozgásszervi Rehabilitációs Központ Betegeiért Alapítvány, Mezőkövesd).
Author information
Authors and Affiliations
Corresponding author
Additional information
Ildikó Katalin Tefner and Csaba Kovács contributed equally to this work.
Rights and permissions
About this article
Cite this article
Tefner, I.K., Kovács, C., Gaál, R. et al. The effect of balneotherapy on chronic shoulder pain. A randomized, controlled, single-blind follow-up trial. A pilot study. Clin Rheumatol 34, 1097–1108 (2015). https://doi.org/10.1007/s10067-013-2456-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-013-2456-3