Abstract
Hypovitaminosis D has been reported to be common in chronic kidney disease (CKD) as well as in proteinuric disorders. We reviewed available evidence to assess clinically relevant effects of low vitamin D status and native vitamin D (NVD) therapy, in pediatric renal diseases. Online medical databases were searched for articles related to vitamin D status, associations of hypovitaminosis D and effects of NVD therapy in kidney disease. Hypovitaminosis D was associated with worse skeletal, cardiovascular, inflammatory, and renal survival outcomes in CKD. Low serum 25 hydroxy-vitamin D (25[OH]D) levels correlated positively with glomerular filtration rate and negatively with serum parathyroid (PTH) levels. However, to date, evidence of benefit of NVD supplementation is restricted mainly to improvements in serum PTH, and biochemical 25[OH]D targets form the basis of clinical practice recommendations for NVD therapy. In nephrotic syndrome (NS) relapse, studies indicate loss of 25[OH]D along with vitamin D binding protein in urine, and serum total 25[OH]D levels are low. Preliminary evidence indicates that free 25[OH]D may be a better guide to the biologically active fraction. NVD therapy in NS does not show consistent results in improving skeletal outcomes and hypercalciuria has been reported when total 25[OH]D levels were considered as indication for therapy. NVD formulations should be regularised, and therapy monitored adequately to avoid adverse effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D plays a vital role in maintaining bone health. In addition, effects on inflammation, infection, allergy, cardiovascular function, and cancer have been reported [1,2,3]. Hypovitaminosis D is common in kidney disorders, and a large number of studies have reported on its osseous and extra-osseous effects in these conditions [4, 5]. This review focusses on examining the clinical relevance of low vitamin D status, as well as outcomes of native vitamin D (NVD) supplementation in children with kidney disease.
Online medical databases, Medline, Pubmed, and Google scholar were searched for articles related to vitamin D status, associations of hypovitaminosis D, and effects of vitamin D therapy in kidney diseases. The available data is summarized and inferences drawn from this data are presented as conclusions after each section.
Vitamin D physiology
Vitamin D is sourced from sun exposure and from diet. The term “native vitamin D”, refers to ergocalciferol (D2) which is chiefly available from plant sources; and cholecalciferol (D3), available from animal dietary sources, and produced from 7-dehydrocholesterol in the skin.
A specific vitamin D binding globulin (DBP) and to a smaller extent, albumin, transport the vitamin D2 and D3 to the liver. These compounds are hydroxylated in the liver to 25 hydroxy D2 and 25 hydroxy D3 (25[OH]D or calcidiol) and subsequently in the kidneys by 1α hydroxylase enzyme, to the active forms: 1,25 dihydroxy D2 and 1,25 dihydroxy D3, (1,25[OH]2D or calcitriol) which activate vitamin D receptors (VDR). The enzyme 1α hydroxylase is also found in non-renal tissues, therefore conversion of calcidiol to calcitriol can occur at a smaller magnitude, extra-renally. It is hypothesized that the calcitriol produced in the kidneys has exocrine functions, whereas extra-renal production is responsible for autocrine and paracrine effects, and not released into the circulation [6, 7].
Circulating serum total 25[OH]D (the sum of 25[OH]D2 and 25[OH]D3) is considered to be the best biological marker of an individual’s vitamin D stores. This is the most abundant of all vitamin D metabolites in the serum, levels correlate with the amount of NVD substrate available, and are stable for 3–4 weeks in the absence of proteinuria [8, 9]. In contrast 1,25[OH]2D has a short half-life, is rapidly influenced by calcium and parathyroid hormone (PTH) levels, has thousand-fold lower circulating levels and there are greater challenges of assaying. The latter has limited use in certain conditions such as chronic kidney disease (CKD), hereditary phosphate losing disorders, vitamin D–resistant rickets, etc. [8, 10].
The largest component of measured serum 25[OH]D (85 to 90%) is bound to DBP, while 10 to 15% is more loosely bound to albumin, and a small fraction: 0.03 to 0.04%, circulates in the free state [8, 11].
The DBP gene is the most polymorphic gene known, and DBP levels and vitamin D binding capacity may be influenced by genotype and be different between races. Evidence suggests that like thyroid hormones, sex steroids and cortisol, vitamin D follows the “free hormone hypothesis”. This proposes that “only the non-bound or free fraction of hormones that otherwise circulate in blood bound to their carrier proteins is able to enter cells and exert their biologic effects” [8, 10, 11]. This hypothesis is supported by several reports: a patient with homozygous DBP mutation, had nearly undetectable levels of total 25[OH]D but free 25[OH]D, calcium, phosphate and PTH levels were normal. Similarly, DBP knockout mice did not reveal any evidence of vitamin D deficiency despite very low levels of total 25[OH]D [11].
However, it is of note that in the proximal renal tubular cell, DBP–25[OH]D complex can be directly reabsorbed from the glomerular filtrate through megalin and cubilin pathways [8, 11].
NVD assays
Measurements of total 25[OH]D use various methods, including immunoassays (most common), protein-binding assays, high-performance liquid chromatography–ultraviolet (HPLC–UV), or liquid chromatography–tandem mass spectrometry (LC–MS/MS) [8]. Until recently, assay variation contributed to the confusion surrounding efforts to define hypovitaminosis D. The vitamin D standardization program (VDSP) in 2010 developed a reference measurement system for harmonized reporting through standardization of the above assays. The gold standard reference measurement procedure utilizes separate serum measurements for D2 and D3 using isotope dilution LC–MS/MS, as it has least interference. Immunoassays, on the other hand, suffer from matrix and other metabolite interferences [12]. VDSP implementation has seen drastic improvements in performance of assays of several manufacturers; with acceptable specifications defined by limits for total coefficient of variation (CV%) ≤ 10% and mean bias ≤ 5% [13].
Free 25[OH]D levels can be estimated with a formula that entails measurements of total 25[OH]D, DBP and albumin levels, but this suffers from inaccuracies mainly due to complexities and uncertainties of DBP measurement. An enzyme-linked immunosorbent assay (ELISA) kit commercialized by Diasource is available to directly measure free 25[OH]D. While direct measurement is definitely the better approach in terms of performance [14, 15], the lack of a reference method, interferences from lipids, bilirubin, hemoglobin, and the underestimation of D2 concentrations remain some limitations [16]. Nonetheless, studies have shown directly measured free 25[OH]D assay to have considerable significance in populations with altered DBP and albumin levels [17, 18]; however, to date, it is only available as a research tool.
Several other biomarkers and vitamin D metabolites are being tested for clinical validity; all except serum 25[OH]D warrant standardization [19].
Section A: Vitamin D in CKD
CKD is associated with bone, cardiovascular, and inflammatory abnormalities, which influence long-term survival [4]. The deficiency of 1α hydroxylase enzyme causes reduction in conversion of 25[OH]D to the activated form: 1,25[OH]2D contributes to the development of CKD mineral bone disease (MBD) [20, 21]. In addition, total serum 25[OH]D levels, are commonly reported to be low [22,23,24,25,26].
Causes are postulated to be poor appetite, malnutrition, reduced sun exposure and food restrictions, which are common in CKD. Deficiency, with 25[OH]D levels < 20 ng/ml, was reported in 28% of 506 children with estimated glomerular filtration rate (GFR) 30 to 90 ml/min/1.73 m2 at enrolment in the CKiD study [27], while levels < 16 ng/ml were found in 2/3 of 500 European children with CKD stages 3–5 [28] and in 27% of 29 children with kidney transplant [29]. 25[OH]D levels are reported to be lower as kidney function declines and are more marked in children with glomerular and proteinuric diseases [23, 28, 30, 31].
NVD and bone parameters in CKD
In early CKD, low 25[OH]D levels have been associated with secondary hyperparathyroidism (HPTH) even in the presence of normal 1,25[OH]2D [24, 32]. Other studies indicate that 25[OH]D levels correlate positively with estimated GFR, 1,25[OH]2D, and NVD supplementation, while negative correlations are reported with serum PTH, CKD stage, and FGF23 levels [23, 28, 30, 33, 34]. Vitamin D deficient children have been reported to have reduced height [26], as well as lower bone mineral density (BMD) scores in CKD stages 2–5D [35].
Effect of NVD supplementation
Clinical outcomes of NVD therapy, such as effect on growth, fracture risk, or bone biopsy, have not been studied in children with CKD. Instead, surrogate biochemical outcomes are used, such as serum 25[OH]D and PTH levels, where changes after intervention may be observed in the short term. A prospective cohort study including 537 CKD children, demonstrated that fracture risk was independently associated with higher PTH levels [36]. Thus, one of the aims of management of CKD MBD is to control secondary HPTH, although optimum PTH levels at different CKD stages are debatable [37, 38].
Interventional studies in adult CKD have reported statistically significant increase in 25[OH]D levels and reduction of PTH levels after NVD supplementation; however, the clinical impact with regard to improvement in secondary HPTH appears to be low [39, 40]. The meta-analysis by Bover et al. included 974 non-dialysis CKD patients (9 randomised controlled trials (RCTs) and 5 observational studies). In the intervention arm, the pooled increase in 25[OH]D level was 20.6 ng/mL while decrease in PTH levels was only 10.5 pg/mL [40].
The effect of NVD supplementation on HPTH is reported to be related to NVD dose and to stage of CKD. Ennis et al. in a cross-sectional analysis of 14,289 patients, showed that in CKD 3–5, increasing levels of 25[OH]D up to 42–48 ng/ml with supplementation resulted in progressively lower PTH levels [41]. The beneficial effect of NVD was seen more in early CKD, and less in stages 4–5/5D where activated vitamin D compounds were needed to control PTH levels even after 25[OH]D levels were optimised [42,43,44,45,46,47].
Pediatric studies are all relatively small, but several also report significant rise in 25[OH]D levels and fall in PTH levels after NVD supplementation [32, 48, 49]. Shroff et al., in the only pediatric RCT of 40 children [50], reported that fewer patients treated with NVD developed HPTH, with significantly longer time to development of HPTH. Target 25[OH]D levels were achieved less in higher stages of CKD.
Significant adverse effects of NVD therapy have not been reported with therapeutic doses in the pediatric CKD literature. This is in contrast to treatment with activated vitamin D compounds (alphacalcidiol, calcitriol, paricalcitol, doxercalciferol) where complications such as hypercalcemia are more common [51, 52].
NVD and non-osseus effects in CKD
Several adult studies have associated vitamin D deficiency with poor cardiovascular outcomes and with increased markers of inflammation in CKD [53]. Pediatric reports are relatively few. Small studies have shown that in children with CKD, levels of 25[OH]D correlate negatively with surrogate indicators of cardiovascular morbidity like aortic pulse wave velocity (PWV) and aortic augmentation index (AI) [54, 55]. Left ventricular mass index correlates negatively with 25[OH]D levels and positively with PTH levels, blood pressure (BP) and AI [22, 56]. Altemose et al. [57], reporting on 580 children from the CKiD cohort, documented 1.9 times higher odds for being anemic in hypovitaminosis D, even after adjusting for several covariates including GFR and use of erythropoetin or hematinics. Levels of 25[OH]D correlated positively with anti-inflammatory and negatively with pro-inflammatory biomarkers in children on chronic hemodialysis [58].
Shroff et al. [59] reviewed 167 children from the ESCAPE cohort and showed that patients with 25[OH]D < 20 ng/ml had higher diastolic BP. The 5-year actuarial kidney survival was 50% with 25[OH]D levels < 20 ng/ml and 75% with levels above 20 ng/ml at baseline. Kidney survival increased 8.2% per 4 ng/ml increase in 25[OH]D levels (p = 0.03), independently of other confounders. Adult studies also indicate that higher 25[OH]D levels are associated with improved survival in CKD. In a meta-analysis of 10 studies and 6853 patients [60], relative risk of mortality for every 10 ng/mL rise in 25[OH]D was 0.86 (95% CI 0.82–0.91).
Effect of NVD supplementation
In vitro and animal studies have shown that NVD supplementation improves cardiovascular endpoints and reduces inflammatory biomarkers in CKD [53, 61]. In children, one small RCT [62] reported a significant decrease in erythropoietin dose in the group treated with NVD compared to control. There are no other studies in children that examine whether intervention with NVD or improvement in 25[OH]D levels improves any non-osseus parameters of CKD. A systemic review found NVD supplementation to be ineffective in lowering BP in otherwise healthy children [63].
In adult CKD, meta-analyses of available RCTs to date, show no consistent improvement in cardiovascular outcomes, anemia, immune function, health-related quality of life scores, hospitalisations or all-cause mortality, with NVD therapy [64,65,66].
Conclusions (A): NVD in CKD
-
a)
Utilization of NVD to maintain vitamin D sufficiency status is useful in early CKD, to prevent or treat secondary HPTH, and it is initially preferred over activated vitamin D compounds. Higher doses of NVD may be required in advanced CKD stages to achieve 25[OH]D target levels.
-
b)
In advanced CKD, NVD is often insufficient to control HPTH. In such cases, once target 25[OH]D levels are reached, activated forms of vitamin D (alphacalcidiol/calcitriol) may be required for control of HPTH and CKD MBD.
-
c)
NVD supplementation may be considered to maintain adequate 25[OH]D levels, as the latter has been associated with improved non-osseus outcomes as well as overall survival. However, direct interventional studies to support such use are not yet available.
Section B: Vitamin D in nephrotic syndrome and other proteinuric kidney diseases
As discussed previously, the majority of serum 25[OH]D (> 99%) circulates bound to proteins. DBP has a molecular weight similar to albumin, and both are lost in urine in proteinuric diseases. In gross proteinuria, urinary losses of DBP bound to 25[OH]D may overwhelm proximal tubular reabsorption capacity via megalin/cubilin pathways [9,10,11].
Free 25[OH]D is defined as circulating 25[OH]D which is bound to neither DBP nor albumin. Several studies indicate that in health, free and total 25[OH]D levels correlate closely, suggesting that there is no need for assessing free 25[OH]D levels separately. However, this correlation was lost in several disease states including nephrotic proteinuria [9, 10, 18]. There are no studies to date that indicate the level of proteinuria at which this dissociation may occur.
NVD in nephrotic syndrome
In pediatric nephrotic syndrome (NS), reports have documented urinary DBP loss, with low levels of serum DBP and total 25[OH]D during and after NS relapse [67,68,69]. However, unlike in CKD, this had no association with abnormalities of corrected calcium, phosphate, alkaline phosphatase (ALP) or PTH [69,70,71]. The total 25[OH]D levels returned to levels similar to healthy controls after ≥ 3 months of attaining remission in steroid sensitive nephrotic syndrome (SSNS) [70, 72].
In contrast, free 25[OH]D levels, were found to be similar to healthy controls both in NS remission and relapse [18], and this may explain why corrected calcium, phosphate, ALP and PTH levels do not change significantly in SSNS, despite markedly low total 25[OH]D. Only total and not free 25[OH]D correlated significantly and negatively with urinary protein:creatinine ratios (Spearman’s rank correlation coefficient, rs = − 0.42, p < 0.001 and 0.04, p = 0.6), while total 25[OH]D had a stronger correlation with serum albumin levels than free 25[OH]D (rs = 0.64, p < 0.001 and 0.21, p = 0.13) [18].
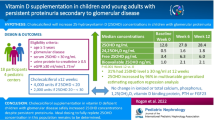
Effect of NVD supplementation
Children with NS are usually treated with steroids, and glucocorticoid-induced osteoporosis (GIO) is a considerable concern, especially if the patient is frequently relapsing or steroid dependent. The question is whether treatment with NVD will improve bone health in such patients.
In patients with SSNS on steroid therapy, two small RCTs over 2–3 months [73, 74], and a longitudinal study over 1.5 years [75] reported better BMD or bone mineral content (BMC) in groups treated with NVD and calcium; however, 25[OH]D levels were not measured in these studies. A subsequent RCT [71] showed no change in BMD or BMC over 6 months, despite marked improvements in serum total 25[OH]D status in the supplemented group.
An RCT by Rooney et al. [76] failed to show benefit of calcium and NVD supplementation on lumbar BMD in GIO of rheumatological diseases.
In NS, hypercalciuria was detected in 50% of patients who received NVD supplementation of 60,000 IU weekly for 4 weeks. All patients in the intervention arm were in relapse and had low total serum 25[OH]D (median 7.0, interquartile range 3–16.7) ng/ml at recruitment. These levels rose to a median of 54.45 (interquartile range 46.45–87.75) ng/ml after supplementation, when the patients were in remission [71]. The question arises of whether total 25[OH]D is a valid target for supplementation, given the evidence of DBP–25[OH]D complex loss in urine and low serum DBP levels in NS [67,68,69]. Free 25[OH]D levels were not checked in this study.
Studies in DBP knockout mice show that despite the absent DBP and very low levels of serum total 25[OH]D, these mice do not develop evidence of vitamin D deficiency unless they are fed an NVD-deficient diet. Extrapolating from this, it appears that DBP binding serves as a reservoir for vitamin D compounds [11]. Thus, in gross proteinuric conditions, where DBP levels are expected to be low, although calcium and NVD supplementation may not specifically treat GIO, achieving daily dietary reference intakes (DRI) for these compounds should be considered, to maintain bone health, as suggested in the forthcoming IPNA clinical practice recommendations, as well as other recent guidelines [77, 78].
NVD in other proteinuric diseases
Several studies of children and adult CKD have indicated lower total 25[OH]D levels in patients with proteinuria, with levels correlating positively with serum albumin and negatively with degree of protein loss [25, 27, 28, 30, 79]. A large population-based adult study revealed increasing prevalence of albuminuria with decreasing 25[OH]D levels [80].
These studies are cross-sectional in nature, therefore causality of the association cannot be proven, and the low total 25[OH]D may simply be an effect of increased urinary losses of protein-bound 25[OH]D. Serum or urinary DBP, free or bioavailable serum 25[OH]D levels have not been studied in these conditions. Pending further evidence, it may be logical to consider the use of NVD therapy above DRI, in such situations, if there is associated evidence of hypovitaminosis D such as low corrected calcium, phosphate and high ALP and PTH.
Experimental data suggests that NVD and VDR activators reduce proteinuria, possibly by suppressing the renin–angiotensin–aldosterone system [81]. In glomerular diseases like IgA and diabetic nephropathy, adult studies have indicated improvement in levels of proteinuria with VDR activator therapy [82,83,84]. However, no such evidence is available in children or with NVD supplementation. There are also no studies examining other non-osseus effects of NVD therapy in proteinuric disorders. Although it is attractive to consider that infection-related NS relapses may be reduced with NVD therapy, Banerjee et al. [71] failed to find any effect of NVD supplementation on relapse frequency; however, their study was not adequately powered to examine this effect.
Conclusions (B): NVD in NS and other proteinuric diseases
-
a)
In proteinuric conditions, serum total 25[OH]D levels may not reflect the biologically active fraction, and preliminary evidence suggests that free 25[OH]D may be a better guide. However, easy-to-use validated assays and further supporting evidence are required before this can become a clinically useful tool.
-
b)
In NS, although calcium and NVD supplementation does not specifically treat GIO, maintaining DRI for calcium and NVD is suggested to optimise bone health. Total serum 25[OH]D may be targeted in SSNS, ideally when in remission for over 3 months.
-
c)
In children, as yet there is no evidence that NVD supplementation reduces proteinuria or has any other positive influence on non-osseous outcomes in proteinuric diseases.
Section C: NVD therapy in kidney disease
Therapeutic targets
Ideally, the levels of 25[OH]D targeted should be sufficient to maintain both osseus and non-osseus functions of vitamin D. However, data for such optimum levels is lacking, particularly for non-osseus outcomes, and guidelines are available to address biochemical bone parameters only. In otherwise healthy children, the level at which bone accrual may be optimum, with effective absorption of calcium from the gut and maintenance of normal ALP and PTH levels, is suggested to be > 20 ng/ml in a recent global consensus [77]. This target is generally accepted for children with kidney disease and normal kidney function. It is recognised that in CKD, higher levels (> 30 ng/ml) are required to prevent secondary HPTH [37, 41, 85] (Table1).
NVD supplements
NVD supplements are available in the form of ergocalciferol (D2) and cholecalciferol (D3). Studies in adults suggest that D3 is superior to D2 in raising both total and free 25[OH]D levels and in lowering serum PTH [86, 87]. An RCT in adults on HD, comparing high-dose monthly vitamin D2 versus D3, also reported that the latter resulted in higher 25[OH]D levels [88]. We could not find any studies comparing D2 to D3 supplementation in children with kidney disease. Pediatric studies to date have not demonstrated any difference between D2 and D3 supplements, whether given daily, weekly, or as single bolus doses [89,90,91]. Pediatric guidelines suggest that either D2 or D3 in daily dose regimens can be used; however, since D3 has a longer half-life, it is preferred if using intermittent dosing schedules [37, 77]. Calcefediol, an extended-release derivative of 25[OH]D3 has recently been approved; however, there are no pediatric data available as yet.
NVD doses and monitoring
The specific dose required in an individual patient to raise 25[OH]D levels from a certain baseline to target levels is not known. Evidence-based pediatric guidelines that are not specific for kidney disease, recommend minimum daily intakes of 400 IU in infancy and 400–600 IU in older children. For treatment of rickets or low 25[OH]D status, the recommended daily doses are up to 2000 IU for infants or 3000 IU for older children; for 12 weeks. For reasons of improved compliance, intermittent doses of 50,000 to 60,000 IU weekly may be given to children over 1 year of age, with total cumulative dose remaining the same [77, 78]. These guidelines are usually followed also for non-CKD renal diseases. Since complications occur more frequently with mega-dose Stoss regimens, such treatment is best avoided [37].
Interventional studies in children with kidney disease have used D2 or D3, in widely variable doses and frequencies, varying from megadoses of 300,000 to 600,000 IU [49, 92] to 60,000 IU weekly for 4 weeks [71] to 2000 IU/day [93]. However, although median 25[OH]D levels increased significantly, the above-mentioned target levels were not achieved in all children with these doses.
It is recognized that higher doses may be required in CKD. Shroff et al. administered D2 supplements to children with CKD, in a modified DOQI protocol [50, 85], which varied according to age and baseline levels (Table 2), and reported that after intensive therapy, target levels of > 30 ng/ml were achieved in 80%, which fell to 60% on maintenance therapy.
Achievement of target levels was less in higher stages of CKD, where even higher doses may be required. In patients with low vitamin D status, Kari et al. administered 2000 IU NVD daily for 3 months, and only 9% of patients achieved levels > 30 ng/ml [93]; whereas doses of 3000 to 4000 IU daily were able to achieve target levels in > 70% patients in two recent RCTs [31, 94].
The doses of NVD used in studies or recommended in guidelines are not generally scaled to body weight or surface area. However, nephrocalcinosis occurred more frequently in smaller children after excessive intake in a recent case series [95]. Pharmakokinetic simulation modelling has suggested that weight-based dosing may improve attainment of target levels and avoid toxicity due to overdose [96].
Screening for hypovitaminosis D is suggested in at-risk patients, every 6–12 months. Continued monitoring of levels at regular intervals while on treatment (Table 2) is required to guide further therapy, along with monitoring for toxicity (hypercalcemia, hyperphosphatemia or hypercalciuria) [37]. Adverse effects are more likely during high dose intensive replacement/loading regimens, and monitoring is more important during this time.
Toxicity of NVD
Pediatric studies using therapeutic doses of NVD reported increase in FGF23 in CKD [31, 97] while calcium, phosphate, and ALP levels were largely unchanged.
However, hypercalciuria was reported in > 50% of patients receiving NVD in NS, when supplementation was guided by total and not free 25[OH]D levels [71].
A meta-analysis of adverse effects of long-term (≥ 24 weeks) NVD supplementation in adult studies revealed increased risks of hypercalcemia and hypercalciuria [98].
Hypervitaminosis usually occurs due to ingestion of excess vitamin D supplements [94, 98]. Vitamin D toxicity is manifested as hypercalcemia, hypercalciuria and suppressed PTH levels. This may cause further complications like pancreatitis, nephrocalcinosis, nephro-urolithiasis, and kidney function impairment. There may be no early symptoms, and biochemical monitoring only can pick up early toxicity. Symptoms, when they occur, maybe be non-specific, like anorexia, vomiting, constipation, polyuria, polydipsia, and dehydration. Rare life-threatening conditions like arrhythmias or encephalopathy have also been reported [99, 100].
In the general population, 25[OH]HD levels > 50 ng/ml are associated with increased mortality, while symptomatic toxicity is associated with 25[OH]D levels above 100 ng/ml [37]. Guidelines suggest that vitamin D supplements are stopped before 25[OH]D levels of 50 ng/ml to prevent toxicity [37, 77].
The availability and formulations of vitamin D preparations are very variable even within countries and regions, and can often be bought as over-the-counter medications. The supplements are available in the form of very concentrated drops, syrups, powders, and capsules, as single products or in combination with calcium and other micronutrients. Popular media have generated a perceived need for NVD supplementation for a myriad of conditions and for general well-being. However, globally, there are now several reports of concentration errors during manufacturing, errors in labelling, and of inappropriate or wrongly administered doses [95, 101,102,103,104,105]. Public education, review and standardisation of formulations are required to safeguard against such mishaps. Caregivers administering these medications should be adequately counselled and treatment monitored to avoid toxicity. Availability without prescription should not be allowed for the more concentrated or high dose formulations.
Conclusions (C): NVD therapy in kidney disease
-
1.
Patients who have high risk of hypovitaminosis D, including patients with hypocalcemia, HPTH, CKD, proteinuria, osteoporosis or clinical rickets, should be screened for vitamin D status.
-
2.
In such patients, vitamin D sufficiency targets, i.e. total 25[OH]D levels of > 20 ng/ml in non-CKD and > 30 ng/ml in CKD, but < 50 ng/ml (in absence of gross proteinuria) should be achieved with NVD therapy (Table 1). Treatment is started as per available guidelines, but subsequently titrated according to levels of 25[OH]D achieved, as well as serum and urinary calcium and PTH status.
-
3.
Supplements containing D2 or D3 may be used; the latter is preferred when using weekly intermittent therapy. Megadose Stoss therapy is to be avoided.
-
4.
Regulations for standardization and labelling of formulations, parental guidance and monitoring are required, and concentrated or high dose preparations should only be available by prescription.
Summary
Although there is much discussion as well as published guidelines regarding NVD therapy in CKD, the issues surrounding proteinuric renal diseases are more nebulous.
In children with CKD, observational studies associate low 25[OH]D status with poorer osseous and non-osseous outcomes. However, evidence of benefit of NVD therapy is restricted only to biochemical improvements in 25[OH]D and PTH levels. Recent evidence-based guidelines aim to optimize NVD therapy to attain vitamin D sufficiency status.
In NS and other hypoalbuminemic/proteinuric conditions, serum total 25[OH]D levels may not reflect the biologically active fraction. Very few studies have correlated outcomes to free 25[OH]D levels. Until commercial assays and further studies examining free 25[OH]D are available, total 25[OH]D levels may be used to guide therapy when the proteinuria has remitted for ≥ 3 months; or NVD supplementation (above DRI) may be indicated in the presence of effects of true hypovitaminosis D, such as low corrected calcium, phosphate and high ALP and PTH levels.
Further research is required to assess the benefits of NVD therapy on clinical outcomes. The limitations of available assays in certain clinical situations needs to be recognized. NVD formulations should be regularised, and therapy monitored and supervised adequately to avoid toxicities which can cause acute systemic illness as well as long-lasting kidney impairment.
References
Chang SW, Lee HC (2019) Vitamin D and health - the missing vitamin in humanSs. Pediatr Neonatol 60:237–244. https://doi.org/10.1016/j.pedneo.2019.04.007
Chiodini I, Gatti D, Soranna D, Merlotti D, Mingiano C, Fassio A et al (2021) Vitamin D status and SARS-CoV-2 infection and COVID-19 clinical outcomes. Front Public Health 9:736665. https://doi.org/10.3389/fpubh.2021.736665
Liu D, Meng X, Tian Q, Cao W, Fan X, Wu L et al (2021) Vitamin D and multiple health outcomes: an umbrella review of observational studies, randomized controlled trials, and Mendelian randomization studies. Adv Nutr 23:nmab142. https://doi.org/10.1093/advances/nmab142
Dusso AS, Bauerle KT, Bernal-Mizrachi C (2021) Non-classical Vitamin D actions for renal protection. Front Med (Lausanne) 8:790513. https://doi.org/10.3389/fmed.2021.790513
Cannata-Andía JB, Martín-Carro B, Martín-Vírgala J, Rodríguez-Carrio J, Bande-Fernández JJ, Alonso-Montes C et al (2021) Chronic kidney disease-mineral and bone disorders: pathogenesis and management. Calcif Tissue Int 108:410–422. https://doi.org/10.1007/s00223-020-00777-1
Holick MF (2011) Chapter 2: photobiology of vitamin D. In: Feldman D, Pike JW, Adams M (eds) Vitamin D, 3rd edn. Academic Press, Cambridge, MA, pp 13–22
Christakos S, Dhawan P, Verstuyf A, Verlinden L, Carmeliet G (2016) Vitamin D: metabolism, molecular mechanism of action, and pleiotropic effects. Physiol Rev 96:365–408. https://doi.org/10.1152/physrev.00014.2015
Herrmann M, Farrell CL, Pusceddu I, Fabregat-Cabello N, Cavalier E (2017) Assessment of vitamin D status - a changing landscape. Clin Chem Lab Med 55:3–26. https://doi.org/10.1515/cclm-2016-0264
Bikle DD, Malmstroem S, Schwartz J (2017) Current controversies: are free vitamin metabolite levels a more accurate assessment of vitamin D status than total levels? Endocrinol Metab Clin North Am 46:901–918. https://doi.org/10.1016/j.ecl.2017.07.013
Alonso MA, Mantecón L, Santos F (2019) Vitamin D deficiency in children: a challenging diagnosis! Pediatr Res 85:596–601. https://doi.org/10.1038/s41390-019-0289-8
Bikle DD, Schwartz J (2019) Vitamin D binding protein, total and free vitamin D levels in different physiological and pathophysiological conditions. Front Endocrinol (Lausanne) 10:317. https://doi.org/10.3389/fendo.2019.00317
Makris K, Bhattoa HP, Cavalier E, Phinney K, Sempos CT, Ulmer CZ et al (2021) Recommendations on the measurement and the clinical use of vitamin D metabolites and vitamin D binding protein - a position paper from the IFCC Committee on bone metabolism. Clin Chim Acta 517:171–197. https://doi.org/10.1016/j.cca.2021.03.002
Altieri B, Cavalier E, Bhattoa HP, Pérez-López FR, López-Baena MT, Pérez-Roncero GR et al (2020) Vitamin D testing: advantages and limits of the current assays. Eur J Clin Nutr 74:231–247. https://doi.org/10.1038/s41430-019-0553-3
Schwartz JB, Lai J, Lizaola B, Kane L, Markova S, Weyland P, Terrault NA, Stotland N, Bikle D (2014) A comparison of measured and calculated free 25[OH] vitamin D levels in clinical populations. J Clin Endocrinol Metab 99:1631–1637. https://doi.org/10.1210/jc.2013-3874
Lopez-Molina M, Santillan C, Murillo M, Valls A, Bosch L, Bel J, Granada ML (2018) Measured free 25-hydroxyvitamin D in healthy children and relationship to total 25-hydroxyvitamin D, calculated free 25-hydroxyvitamin D and vitamin D binding protein. Clin Biochem 61:23–27. https://doi.org/10.1016/j.clinbiochem.2018.08.007
Malmstroem S, Rejnmark L, Imboden JB, Shoback DM, Bikle DD (2017) Current assays to determine free 25-hydroxyvitamin D in serum. J AOAC Int 100:1323–1327. https://doi.org/10.5740/jaoacint.17-0085
Schwartz JB, Gallagher JC, Jorde R, Berg V, Walsh J, Eastell R et al (2018) Determination of free 25[OH]D concentrations and their relationships to total 25[OH]D in multiple clinical populations. J Clin Endocrinol Metab 103:3278–3288. https://doi.org/10.1210/jc.2018-00295
Banerjee S, Basu S, Akhtar S, Sinha R, Sen A, Sengupta J (2020) Free vitamin D levels in steroid-sensitive nephrotic syndrome and healthy controls. Pediatr Nephrol 35:447–454. https://doi.org/10.1007/s00467-019-04433-1
Sempos CT, Heijboer AC, Bikle DD, Bollerslev J, Bouillon R, Brannon PM et al (2018) Vitamin D assays and the definition of hypovitaminosis D: results from the First International Conference on Controversies in Vitamin D. Br J Clin Pharmacol 84:2194–2207. https://doi.org/10.1111/bcp.13652
Santos F, Díaz-Anadón L, Ordóñez FA, Haffner D (2021) Bone disease in CKD in children. Calcif Tissue Int 108:423–438. https://doi.org/10.1007/s00223-020-00787-z
Lalayiannis AD, Crabtree NJ, Fewtrell M, Biassoni L, Milford DV, Ferro CJ et al (2020) Assessing bone mineralisation in children with chronic kidney disease: what clinical and research tools are available? Pediatr Nephrol 35:937–957. https://doi.org/10.1007/s00467-019-04271-1
Ali S, Saber M, Kassem M (2021) The impact of bone mineral biomarkers on cardiac dysfunction in predialysis chronic kidney disease children. Int J Pediatr 2021:4708452. https://doi.org/10.1155/2021/4708452
Kari JA, El Desoky SM, El-Morshedy SM, Habib HS (2012) Vitamin D insufficiency and deficiency in children with chronic kidney disease. Ann Saudi Med 32:473–478. https://doi.org/10.5144/0256-4947.2012.473
Stein DR, Feldman HA, Gordon CM (2012) Vitamin D status in children with chronic kidney disease. Pediatr Nephrol 27:1341–1350. https://doi.org/10.1007/s00467-012-2143-7
Solarin AU, Nourse P, Gajjar P (2019) Vitamin D status of children with moderate to severe chronic kidney disease at a tertiary pediatric center in Cape Town. Saudi J Kidney Dis Transpl 30:781–794. https://doi.org/10.4103/1319-2442.265453
Seeherunvong W, Abitbol CL, Chandar J, Zilleruelo G, Freundlich M (2009) Vitamin D insufficiency and deficiency in children with early chronic kidney disease. J Pediatr 154:906-911.e1. https://doi.org/10.1016/j.jpeds.2008.12.006
Kumar J, McDermott K, Abraham AG, Friedman LA, Johnson VL, Kaskel FJ et al (2016) Prevalence and correlates of 25-hydroxyvitamin D deficiency in the chronic kidney disease in children (CKiD) cohort. Pediatr Nephrol 31:121–129. https://doi.org/10.1007/s00467-015-3190-7
Doyon A, Schmiedchen B, Sander A, Bayazit A, Duzova A, Canpolat N et al (2016) 4C Study Consortium. Genetic, environmental, and disease-associated correlates of vitamin D status in children with CKD. Clin J Am Soc Nephrol 11:1145–1153. https://doi.org/10.2215/CJN.10210915
Ebbert K, Chow J, Krempien J, Matsuda-Abedini M, Dionne J (2015) Vitamin D insufficiency and deficiency in pediatric renal transplant recipients. Pediatr Transplant 19:492–498. https://doi.org/10.1111/petr.12527
Denburg MR, Kalkwarf HJ, de Boer IH, Hewison M, Shults J, Zemel BS et al (2013) Vitamin D bioavailability and catabolism in pediatric chronic kidney disease. Pediatr Nephrol 28:1843–1853. https://doi.org/10.1007/s00467-013-2493-9
Iyengar A, Kamath N, Reddy HV, Sharma J, Singhal J, Uthup S et al (2022) Determining the optimal cholecalciferol dosing regimen in children with CKD: a randomized controlled trial. Nephrol Dial Transplant 37:326–334. https://doi.org/10.1093/ndt/gfaa369
Menon S, Valentini RP, Hidalgo G, Peschansky L, Mattoo TK (2008) Vitamin D insufficiency and hyperparathyroidism in children with chronic kidney disease. Pediatr Nephrol 23:1831–1836. https://doi.org/10.1007/s00467-008-0842-x
Cho HY, Hyun HS, Kang HG, Ha IS, Cheong HI (2013) Prevalence of 25[OH] vitamin D insufficiency and deficiency in pediatric patients on chronic dialysis. Perit Dial Int 33:398–404. https://doi.org/10.3747/pdi.2011.00246
Niculescu DA, Deacu LG, Caragheorgheopol A, Popescu N, Ghemigian A, Procopiuc C et al (2021) Combined effects of vitamin D status, renal function and age on serum parathyroid hormone levels. Front Endocrinol (Lausanne) 12:657991. https://doi.org/10.3389/fendo.2021.657991
Denburg MR, Tsampalieros AK, de Boer IH, Shults J, Kalkwarf HJ, Zemel BS et al (2013) Mineral metabolism and cortical volumetric bone mineral density in childhood chronic kidney disease. J Clin Endocrinol Metab 98:1930–1938. https://doi.org/10.1210/jc.2012-4188
Denburg MR, Kumar J, Jemielita T, Brooks ER, Skversky A, Portale AA et al (2016) Fracture burden and risk factors in childhood CKD: results from the CKiD cohort study. J Am Soc Nephrol 27:543–550. https://doi.org/10.1681/ASN.2015020152
Shroff R, Wan M, Nagler EV, Bakkaloglu S, Fischer DC, Bishop N et al (2017) European Society for Paediatric Nephrology Chronic Kidney Disease Mineral and Bone Disorders and Dialysis Working Groups. Clinical practice recommendations for native vitamin D therapy in children with chronic kidney disease Stages 2–5 and on dialysis. Nephrol Dial Transplant 32:1098–1113. https://doi.org/10.1093/ndt/gfx065
Shroff R, Wan M, Nagler EV, Bakkaloglu S, Cozzolino M, Bacchetta J et al (2017) European Society for Paediatric Nephrology Chronic Kidney Disease Mineral and Bone Disorders and Dialysis Working Groups. Clinical practice recommendations for treatment with active vitamin D analogues in children with chronic kidney disease stages 2–5 and on dialysis. Nephrol Dial Transplant 32:1114–1127
Kandula P, Dobre M, Schold JD, Schreiber MJ Jr, Mehrotra R, Navaneethan SD (2011) Vitamin D supplementation in chronic kidney disease: a systematic review and meta-analysis of observational studies and randomized controlled trials. Clin J Am Soc Nephrol 6:50–62. https://doi.org/10.2215/CJN.03940510
Bover J, Gunnarsson J, Csomor P, Kaiser E, Cianciolo G, Lauppe R (2021) Impact of nutritional vitamin D supplementation on parathyroid hormone and 25-hydroxyvitamin D levels in non-dialysis chronic kidney disease: a meta-analysis. Clin Kidney J 14:2177–2186. https://doi.org/10.1093/ckj/sfab035
Ennis JL, Worcester EM, Coe FL, Sprague SM (2016) Current recommended 25-hydroxyvitamin D targets for chronic kidney disease management may be too low. J Nephrol 29:63–70. https://doi.org/10.1007/s40620-015-0186-0
Al-Aly Z, Qazi RA, González EA, Zeringue A, Martin KJ (2007) Changes in serum 25-hydroxyvitamin D and plasma intact PTH levels following treatment with ergocalciferol in patients with CKD. Am J Kidney Dis 50:59–68. https://doi.org/10.1053/j.ajkd.2007.04.010
Zisman AL, Hristova M, Ho LT, Sprague SM (2007) Impact of ergocalciferol treatment of vitamin D deficiency on serum parathyroid hormone concentrations in chronic kidney disease. Am J Nephrol 27:36–43. https://doi.org/10.1159/000098561
Bhan I, Dobens D, Tamez H, Deferio JJ, Li YC, Warren HS et al (2015) Nutritional vitamin D supplementation in dialysis: a randomized trial. Clin J Am Soc Nephrol 10:611–619. https://doi.org/10.2215/CJN.06910714
Mieczkowski M, Żebrowski P, Wojtaszek E, Stompór T, Przedlacki J, Bartoszewicz Z et al (2014) Long-term cholecalciferol administration in hemodialysis patients: a single-center randomized pilot study. Med Sci Monit 20:2228–2234. https://doi.org/10.12659/MSM.892315
Gravesen E, Hofman-Bang J, Lewin E, Olgaard K (2013) Ergocalciferol treatment and aspects of mineral homeostasis in patients with chronic kidney disease stage 4–5. Scand J Clin Lab Invest 73:107–116. https://doi.org/10.3109/00365513.2012.744464
Marckmann P, Agerskov H, Thineshkumar S, Bladbjerg EM, Sidelmann JJ, Jespersen J, Nybo M, Rasmussen LM, Hansen D, Scholze A (2012) Randomized controlled trial of cholecalciferol supplementation in chronic kidney disease patients with hypovitaminosis D. Nephrol Dial Transplant 27:3523–3531. https://doi.org/10.1093/ndt/gfs138
Sawires H, Fadel F, Hussein A, Helmy R (2021) Native vs. active vitamin D in children with chronic kidney disease: a cross-over study. Pediatr Nephrol 36:443–450. https://doi.org/10.1007/s00467-020-04721-1
Hari P, Gupta N, Hari S, Gulati A, Mahajan P, Bagga A (2010) Vitamin D insufficiency and effect of cholecalciferol in children with chronic kidney disease. Pediatr Nephrol 25:2483–2488. https://doi.org/10.1007/s00467-010-1639-2
Shroff R, Wan M, Gullett A, Ledermann S, Shute R, Knott C et al (2012) Ergocalciferol supplementation in children with CKD delays the onset of secondary hyperparathyroidism: a randomized trial. Clin J Am Soc Nephrol 7:216–223. https://doi.org/10.2215/CJN.04760511
Palmer SC, McGregor DO, Craig JC, Elder G, Macaskill P, Strippoli GF (2009) Vitamin D compounds for people with chronic kidney disease requiring dialysis. Cochrane Database Syst Rev (4):CD005633. https://doi.org/10.1002/14651858.CD005633.pub2
Palmer SC, McGregor DO, Craig JC, Elder G, Macaskill P, Strippoli GF (2009) Vitamin D compounds for people with chronic kidney disease not requiring dialysis. Cochrane Database Syst Rev (4):CD008175. https://doi.org/10.1002/14651858.CD008175
Querfeld U (2013) Vitamin D and inflammation. Pediatr Nephrol 28:605–610. https://doi.org/10.1007/s00467-012-2377-4
Patange AR, Valentini RP, Du W, Pettersen MD (2012) Vitamin D deficiency and arterial wall stiffness in children with chronic kidney disease. Pediatr Cardiol 33:122–128. https://doi.org/10.1007/s00246-011-0101-y
Conkar S, Mir S, Dogan E, Ülger Tutar Z (2018) Association of Vitamin D deficiency with increased pulse wave velocity and augmentation index in children with chronic kidney disease. Iran J Kidney Dis 12:275–280
Patange AR, Valentini RP, Gothe MP, Du W, Pettersen MD (2013) Vitamin D deficiency is associated with increased left ventricular mass and diastolic dysfunction in children with chronic kidney disease. Pediatr Cardiol 34:536–542. https://doi.org/10.1007/s00246-012-0489-z
Altemose KE, Kumar J, Portale AA, Warady BA, Furth SL, Fadrowski JJ et al (2018) Vitamin D insufficiency, hemoglobin, and anemia in children with chronic kidney disease. Pediatr Nephrol 33:2131–2136. https://doi.org/10.1007/s00467-018-4020-5
Youssef DM, Elshal AS, Abo Elazem AA (2012) Assessment of immune status in relation to vitamin D levels in children on regular hemodialysis. Saudi J Kidney Dis Transpl 23:267–273
Shroff R, Aitkenhead H, Costa N, Trivelli A, Litwin M, Picca S et al . . . ESCAPE Trial Group (2016) Normal 25-hydroxyvitamin D levels are associated with less proteinuria and attenuate renal failure progression in children with CKD. J Am Soc Nephrol 27:314–322. https://doi.org/10.1681/ASN.2014090947
Pilz S, Iodice S, Zittermann A, Grant WB, Gandini S (2011) Vitamin D status and mortality risk in CKD: a meta-analysis of prospective studies. Am J Kidney Dis 58:374–382. https://doi.org/10.1053/j.ajkd.2011.03.020
Brito RBO, Rebello JF, Grabulosa CC, Pinto W, Morales A Jr, Elias RM et al (2020) 25-vitamin D reduces inflammation in uremic environment. Sci Rep 10:128. https://doi.org/10.1038/s41598-019-56874-1
Rianthavorn P, Boonyapapong P (2013) Ergocalciferol decreases erythropoietin resistance in children with chronic kidney disease stage 5. Pediatr Nephrol 28:1261–1266. https://doi.org/10.1007/s00467-013-2431-x
Abboud M (2020) Vitamin D supplementation and blood pressure in children and adolescents: a systematic review and meta-analysis. Nutrients 12:1163. https://doi.org/10.3390/nu12041163
Banerjee D, Chitalia N, Ster IC, Appelbaum E, Thadhani R, Kaski JC et al (2021) Impact of vitamin D on cardiac structure and function in chronic kidney disease patients with hypovitaminosis D: a randomized controlled trial and meta-analysis. Eur Heart J Cardiovasc Pharmacother 7:302–311. https://doi.org/10.1093/ehjcvp/pvz080
Agarwal R, Georgianos PI (2016) Con: nutritional vitamin D replacement in chronic kidney disease and end-stage renal disease. Nephrol Dial Transplant 31:706–713. https://doi.org/10.1093/ndt/gfw080 (Erratum.In:NephrolDialTransplant.202136:566-567)
Zoccali C, Mallamaci F (2016) Moderator’s view: vitamin D deficiency treatment in advanced chronic kidney disease: a close look at the emperor’s clothes. Nephrol Dial Transplant 31:714–716. https://doi.org/10.1093/ndt/gfw081
Grymonprez A, Proesmans W, Van Dyck M, Jans I, Goos G, Bouillon R (1995) Vitamin D metabolites in childhood nephrotic syndrome. Pediatr Nephrol 9:278–281. https://doi.org/10.1007/BF02254183
Barragry JM, France MW, Carter ND, Auton JA, Beer M, Boucher BJ et al (1977) Vitamin-D metabolism in nephrotic syndrome. Lancet 2:629–632. https://doi.org/10.1016/s0140-6736(77)92498-9
Weng FL, Shults J, Herskovitz RM, Zemel BS, Leonard MB (2005) Vitamin D insufficiency in steroid-sensitive nephrotic syndrome in remission. Pediatr Nephrol 20:56–63. https://doi.org/10.1007/s00467-004-1694-7
Banerjee S, Basu S, Sengupta J (2013) Vitamin D in nephrotic syndrome remission: a case-control study. Pediatr Nephrol 28:1983–1989. https://doi.org/10.1007/s00467-013-2511-y
Banerjee S, Basu S, Sen A, Sengupta J (2017) The effect of vitamin D and calcium supplementation in pediatric steroid-sensitive nephrotic syndrome. Pediatr Nephrol 32:2063–2070. https://doi.org/10.1007/s00467-017-3716-2
Biyikli NK, Emre S, Sirin A, Bilge I (2004) Biochemical bone markers in nephrotic children. Pediatr Nephrol 19:869–873. https://doi.org/10.1007/s00467-004-1537-6
Bak M, Serdaroglu E, Guclu R (2006) Prophylactic calcium and vitamin D treatments in steroid-treated children with nephrotic syndrome. Pediatr Nephrol 21:350–354. https://doi.org/10.1007/s00467-005-2118-z
Choudhary S, Agarwal I, Seshadri MS (2014) Calcium and vitamin D for osteoprotection in children with new-onset nephrotic syndrome treated with steroids: a prospective, randomized, controlled, interventional study. Pediatr Nephrol 29:1025–1032. https://doi.org/10.1007/s00467-013-2720-4
Gulati S, Sharma RK, Gulati K, Singh U, Srivastava A (2005) Longitudinal follow-up of bone mineral density in children with nephrotic syndrome and the role of calcium and vitamin D supplements. Nephrol Dial Transplant 20:1598–1603. https://doi.org/10.1093/ndt/gfh809
Rooney M, Bishop N, Davidson J, Beresford MW, Pilkington C, Donagh JM et al (2019) British Society for Paediatric and Adolescent Rheumatology UK. The prevention and treatment of glucocorticoid-induced osteopaenia in juvenile rheumatic disease: a randomised double-blind controlled trial. EClinicalMedicine 12:79–87. https://doi.org/10.1016/j.eclinm.2019.06.004
Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K et al (2016) Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab 101:394–415. https://doi.org/10.1210/jc.2015-2175
Gupta P, Dabas A, Seth A, Bhatia VL, Khadgawat R, Kumar P et al (2022) Indian Academy of Pediatrics revised (2021) guidelines on prevention and treatment of vitamin D deficiency and rickets. Indian Pediatr 59:142–158
Isakova T, Gutiérrez OM, Patel NM, Andress DL, Wolf M, Levin A (2011) Vitamin D deficiency, inflammation, and albuminuria in chronic kidney disease: complex interactions. J Ren Nutr 21:295–302. https://doi.org/10.1053/j.jrn.2010.07.002
de Boer IH, Ioannou GN, Kestenbaum B, Brunzell JD, Weiss NS (2007) 25-Hydroxyvitamin D levels and albuminuria in the Third National Health and Nutrition Examination Survey (NHANES III). Am J Kidney Dis 50:69–77. https://doi.org/10.1053/j.ajkd.2007.04.015
Lucisano S, Buemi M, Passantino A, Aloisi C, Cernaro V, Santoro D (2013) New insights on the role of vitamin D in the progression of renal damage. Kidney Blood Press Res 37:667–678. https://doi.org/10.1159/000355747
de Zeeuw D, Agarwal R, Amdahl M, Audhya P, Coyne D, Garimella T et al (2010) Selective vitamin D receptor activation with paricalcitol for reduction of albuminuria in patients with type 2 diabetes (VITAL study): a randomised controlled trial. Lancet 376:1543–1551. https://doi.org/10.1016/S0140-6736(10)61032-X
de Borst MH, Hajhosseiny R, Tamez H, Wenger J, Thadhani R, Goldsmith DJ (2013) Active vitamin D treatment for reduction of residual proteinuria: a systematic review. J Am Soc Nephrol 24:1863–1871. https://doi.org/10.1681/ASN.2013030203
Deng J, Zheng X, Xie H, Chen L (2017) Calcitriol in the treatment of IgA nephropathy with non-nephrotic range proteinuria: a meta-analysis of randomized controlled trials. Clin Nephrol 87:21–27
KDOQI Work Group (2009) KDOQI Clinical Practice Guideline for Nutrition in Children with CKD: 2008 update. Executive summary Am J Kidney Dis 53(3 Suppl 2):S11-104. https://doi.org/10.1053/j.ajkd.2008.11.017
Balachandar R, Pullakhandam R, Kulkarni B, Sachdev HS (2021) Relative efficacy of vitamin D2 and vitamin D3 in improving vitamin D status: systematic review and meta-analysis. Nutrients 13:3328. https://doi.org/10.3390/nu13103328
Shieh A, Chun RF, Ma C, Witzel S, Meyer B, Rafison B et al (2016) Effects of high-dose vitamin D2 versus D3 on total and free 25-hydroxyvitamin D and markers of calcium balance. J Clin Endocrinol Metab 101:3070–3078. https://doi.org/10.1210/jc.2016-1871
Daroux M, Shenouda M, Bacri JL, Lemaitre V, Vanhille P, Bataille P (2013) Vitamin D2 versus vitamin D3 supplementation in hemodialysis patients: a comparative pilot study. J Nephrol 26:152–157. https://doi.org/10.5301/jn.5000123
Gallo S, Phan A, Vanstone CA, Rodd C, Weiler HA (2013) The change in plasma 25-hydroxyvitamin D did not differ between breast-fed infants that received a daily supplement of ergocalciferol or cholecalciferol for 3 months. J Nutr 143:148–153. https://doi.org/10.3945/jn.112.167858
Thacher TD, Fischer PR, Obadofin MO, Levine MA, Singh RJ, Pettifor JM (2010) Comparison of metabolism of vitamins D2 and D3 in children with nutritional rickets. J Bone Miner Res 25:1988–1995. https://doi.org/10.1002/jbmr.99
Gordon CM, Williams AL, Feldman HA, May J, Sinclair L, Vasquez A et al (2008) Treatment of hypovitaminosis D in infants and toddlers. J Clin Endocrinol Metab 93:2716–2721. https://doi.org/10.1210/jc.2007-2790
Kari JA, Baghdadi OT, El-Desoky S (2013) Is high-dose cholecalciferol justified in children with chronic kidney disease who failed low-dose maintenance therapy? Pediatr Nephrol 28:933–937. https://doi.org/10.1007/s00467-012-2407-2
Kari JA, Eldesoky SM, Bagdadi OT (2012) Vitamin D insufficiency and treatment with oral vitamin D3 in children with chronic kidney disease. Saudi Med J 33:740–744
Nadeem S, Tangpricha V, Ziegler TR, Rhodes JE, Leong T, Xiang Y, Greenbaum LA (2022) Randomized trial of two maintenance doses of vitamin D in children with chronic kidney disease. Pediatr Nephrol 37:415–422. https://doi.org/10.1007/s00467-021-05228-z
Lin TH, Lu HJ, Lin CH, Lee MD, Chang BP, Lin CC et al (2022) Nephrocalcinosis in children who received high dose Vitamin D. Pediatr Nephrol. https://doi.org/10.1007/s00467-022-05512-6
Wan M, Green B, Iyengar AA, Kamath N, Reddy HV, Sharma J, Singhal J, Uthup S, Ekambaram S, Selvam S, Rait G, Shroff R, Patel JP (2022) Population pharmacokinetics and dose optimisation of colecalciferol in paediatric patients with chronic kidney disease. Br J Clin Pharmacol 88:1223–1234. https://doi.org/10.1111/bcp.15064
Lerch C, Shroff R, Wan M, Rees L, Aitkenhead H, Kaplan Bulut I et al (2018) 4C study consortium; ESPN CKD-MBD working group. Effects of nutritional vitamin D supplementation on markers of bone and mineral metabolism in children with chronic kidney disease. Nephrol Dial Transplant 33:2208–2217. https://doi.org/10.1093/ndt/gfy012
Malihi Z, Wu Z, Stewart AW, Lawes CM, Scragg R (2016) Hypercalcemia, hypercalciuria, and kidney stones in long-term studies of vitamin D supplementation: a systematic review and meta-analysis. Am J Clin Nutr 104:1039–1051. https://doi.org/10.3945/ajcn.116.134981
Lim K, Thadhani R (2020) Vitamin D Toxicity. J Bras Nefrol 42:238–244. https://doi.org/10.1590/2175-8239-JBN-2019-0192
Tripty N, Tushar J, Sunil J (2021) Vitamin D intoxication presenting as subacute encephalopathy-a case report. Child Neurol Open 8:2329048X211008075. https://doi.org/10.1177/2329048X211008075
Garg S, Sabri D, Kanji J, Rakkar PS, Lee Y, Naidoo N et al (2013) Evaluation of vitamin D medicines and dietary supplements and the physicochemical analysis of selected formulations. J Nutr Health Aging 17:158–161. https://doi.org/10.1007/s12603-012-0090-4
LeBlanc ES, Perrin N, Johnson JD, Ballatore A, Hillier T (2013) Over-the-counter and compounded vitamin D: is potency what we expect? JAMA Intern Med 173:585. https://doi.org/10.1001/jamainternmed.2013.3812
Wan M, Patel A, Patel JP, Rait G, Jones SA, Shroff R (2021) Quality and use of unlicensed vitamin D preparations in primary care in England: retrospective review of national prescription data and laboratory analysis. Br J Clin Pharmacol 87:1338–1346. https://doi.org/10.1111/bcp.14521
Verkaik-Kloosterman J, Seves SM, Ocké MC (2017) Vitamin D concentrations in fortified foods and dietary supplements intended for infants: implications for vitamin D intake. Food Chem 221:629–635. https://doi.org/10.1016/j.foodchem.2016.11.128
Khadgawat R, Ramot R, Chacko KM, Marwaha RK (2013) Disparity in cholecalciferol content of commercial preparations available in India. Indian J Endocrinol Metab 17:1100–1103. https://doi.org/10.4103/2230-8210.122638
Author information
Authors and Affiliations
Contributions
Conception and outline was by S Banerjee. S Banerjee and JS focused on review of clinical evidence, and S Basu on physiology and biochemical components. All authors contributed to writing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Banerjee, S., Sengupta, J. & Basu, S. The clinical relevance of native vitamin D in pediatric kidney disease. Pediatr Nephrol 38, 945–955 (2023). https://doi.org/10.1007/s00467-022-05698-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05698-9