Abstract
Background
Internal hernia (IH) is one of the critical complications after gastrectomy with Roux-en-Y reconstruction, which can be prevented by closing mesenteric defects. However, only few studies have investigated the incidence of IH after laparoscopic total gastrectomy (LTG) with Roux-en-Y reconstruction for gastric cancer till date. This study aimed to assess the efficacy of defect closure for the prevention of IH after LTG.
Methods
This multicenter, retrospective cohort study collected data from 714 gastric cancer patients who underwent LTG with Rou-en-Y reconstruction between 2010 and 2016 in 13 hospitals. We evaluated the incidence of postoperative IH by comparing closure and non-closure groups of Petersen’s defect, jejunojejunostomy mesenteric defect, and transverse mesenteric defect.
Results
The closure group for Petersen’s defect included 609 cases, while the non-closure group included 105 cases. The incidence of postoperative IH in the closure group for Petersen’s defect was significantly lower than it was in the non-closure group (0.5% vs. 4.8%, p < 0.001). The closure group for jejunojejunostomy mesenteric defect included 641 cases, while the non-closure group included 73 cases. The incidence of postoperative IH in the closure group of jejunojejunostomy mesenteric defect was significantly lower than that in the non-closure group (0.8% vs. 4.1%, p = 0.004). Out of 714 patients, 41 underwent retro-colic reconstruction. No patients in the transverse mesenteric defect group developed IH.
Conclusion
Mesenteric defect closure after LTG with Roux-en-Y reconstruction may reduce postoperative IH incidence. Endoscopic surgeons should take great care to prevent IH by closing mesenteric defects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic total gastrectomy (LTG) is a standard option for surgical treatment of gastric cancer due to its favorable postoperative recovery and precision due to the magnified operative view [1,2,3]. However, even though LTG has advantages, the minimal invasiveness of the laparoscopic approach can be nullified if severe postoperative complications, such as internal hernia (IH), occur.
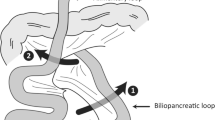
IH is one of the critical complications after gastrectomy with Roux-en-Y reconstruction and Roux-en-Y gastric bypass (RYGB). IH may occur through the Petersen’s defect, jejunojejunostomy mesenteric defect, or transverse colon mesenteric defect. The incidence of IH after laparoscopic gastrectomy for gastric cancer ranges from 1.4 to 22%, while the incidence of IH after RYGB ranges from 5 to 9% [4,5,6,7]. Previous studies associated laparoscopic surgery with an increased risk of postoperative IH because Roux-en-Y laparoscopic gastric bypass (LRYGB) and LTG have fewer adhesions than open RYGB and open total gastrectomy [7,8,9].
When IH occurs as a postoperative complication after gastrectomy or RYGB, the small bowel herniates through the mesenteric defects that are created during Roux-en-Y reconstruction. IH may cause small bowel strangulation with necrosis, perforation, and/or sepsis, which subsequently requires emergency surgery with extensive intestinal resection. Therefore, preventing postoperative IH is essential for both patients and surgeons.
Closing defects, such as Petersen’s defects or jejunojejunostomy mesenteric defects, is recommended to prevent IH after RYGB [10, 11]. As is the case with LRYGB, defect closure is effective for preventing IH after gastrectomy for gastric cancer with Roux-en-Y reconstruction [7, 12, 13]. However, only a few studies have investigated the incidence of IH after LTG by comparing closure and non-closure of these defects. Therefore, this retrospective study aimed to assess the efficacy of defect closure for the prevention of IH after LTG. For this study, we used a multicenter, large-scale cohort, which we used previously to compare linear and circular staplers for intracorporeal esophagojejunostomy during LTG [14].
Materials and methods
Patients and outcomes
From January 2010 to December 2016, patients with gastric cancer who underwent LTG with Roux-en-Y reconstruction were reviewed retrospectively at 13 hospitals that participated in the Kyoto Esophageal and Gastric Surgery Study Group. The inclusion criteria were as follows: gastric adenocarcinoma histologically diagnosed preoperatively, clinical stage I to III according to the Japanese Classification of Gastric Carcinoma [15], and LTG with Roux-en-Y reconstruction. The exclusion criteria were as follows: patients who had gastric cancer with 3 cm or more esophageal invasion and remnant gastric cancer or those who had no defect closure information. In this study, we analyzed IH that required surgical treatment (Grade IIIb or higher, according to the Clavien–Dindo classification) [16]. Patients were categorized into two groups for each defect: closure group and non-closure group. The IH incidence was compared between the two groups.
Surgical procedure
The patients were placed in the supine reverse Trendelenburg position with their legs spread apart. All patients received LTG with D1 + or D2 lymph node dissection, with splenectomy or pancreatic tail resection when required, according to the Japanese Gastric Cancer Treatment Guidelines [17]. The detailed lymphadenectomy during LTG procedures are described elsewhere [18,19,20]. Roux-en-Y reconstruction was performed for all patients. A jejunal loop was transected approximately 20 cm distal from the ligament of Treitz to make a Roux limb. Then, jejunojejunostomy was performed and a 40–50 cm long Roux limb was created. The esophagojejunostomy was performed using a linear or a circular stapler. The surgeon determined the reconstruction route, ante-colic or retro-colic, as well as whether to close Petersen’s defect/jejunojejunostomy mesenteric defects. In the closure group, Petersen’s defects were closed intracorporeally in all cases, while jejunojejunostomy mesenteric defects were closed intra- or extracorporeally according to the surgeon’s preference.
Statistical analysis
Continuous variables were analyzed using an unpaired t-test, and categorical variables were analyzed using Fisher’s exact test. All p-values were two-sided, and a p-value of less than 0.05 was considered statistically significant. Logistic regression analysis was used on multivariable analysis. JMP Statistical Software Version 13 (SAS Institute, Cary, NC, USA) was used to perform all the statistical analyses.
Results
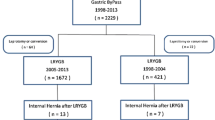
Figure 1 shows the flow diagram of the study design. A total of 714 patients were enrolled. For Petersen’s defect, the non-closure group comprised 105 patients, and the closure group comprised 609 patients. For jejunojejunostomy mesenteric defect, the non-closure group comprised 73 patients, and the closure group comprised 641 patients. The status of defect closure in each institute was shown in Supplemetary Table 1. Eight of the 13 institutes had at least one case without closure of Petersen's defect, while four institutes had cases without closure of jejunojejunostomy mesenteric defect.
Incidence of IH in patients with Petersen’s defects
Table 1 shows the patients’ characteristics of the patients. IH occurred in five cases (4.8%) in the non-closure group and three cases (0.5%) in the closure group. The incidence of IH was significantly lower in the closure group than in the non-closure group (p < 0.01). The follow-up period was shorter in the closure group (median: 923 days) than in the non-closure group (median: 1699 days) (Table 2). Table 3 shows the characteristics of patients who developed IH through Petersen’s defect. All patients that developed IH had received reconstruction via the ante-colic route. The median time to IH occurrence was 487 days (range: 108–507). All 8 patients underwent emergency surgery for IH repair without bowel resection. Laparoscopic approach was employed in four patients, while open approach in four patients. All patients recovered well without any postoperative complications and no patients required permanent total parenteral nutrition. Multivariable logistic regression analysis was performed to investigate whether non-closure was an independent risk factor of IH through Petersen’s defect. As shown in Supplemetary Table 2, non-closure of Petersen’s defect of was an independent risk factor of IH.
Incidence of IH in patients with jejunojejunostomy mesenteric defects
Table 4 shows the patients’ characteristics. IH occurred in three patients (4.1%) in the non-closure group and five patients (0.8%) in the closure group. The incidence of IH was significantly lower in the closure group than in the non-closure group (p < 0.01). The follow-up period was shorter in the closure group (median: 932 days) than in the non-closure group (median: 1630 days) (Table 5). Table 6 shows the characteristics of patients with jejunojejunostomy mesenteric defects who developed IH. Among this group, seven patients had received ante-colic reconstruction, and one patient had received retro-colic reconstruction. The median time to occurrence of IH was 604.5 days (range 7–1908). All patients underwent emergency surgery for IH repair without bowel resection. Laparoscopic approach was employed in six patients, while open approach in two patients. All patients recovered well without any postoperative complications and no patients required permanent total parenteral nutrition. Multivariable logistic regression analysis was also performed to investigate whether non-closure was an independent risk factor of IH through jejunojejunostomy mesenteric defect. As is the case with the aforementioned Petersen’s defect, non-closure of jejunojejunostomy mesenteric defect was an independent risk factor of IH (Supplemetary Table 3).
Incidence of IH in patients with transverse mesenteric defects
Forty-one patients, who received reconstruction via the retro-colic route, had transverse mesenteric defects, and no patients with transverse mesenteric defects developed IH.
Discussion
A large-scale, multicenter, retrospective cohort study was conducted to investigate the incidence of postoperative IH after LTG. In this study, we separately analyzed the efficacy of defect closure for Petersen’s defect and jejunojejunostomy mesenteric defect. The incidence of IH was significantly lower in the closure group than in the non-closure group for both mesenteric defects. The incidence of IH was 2.2% in all patients, 1.1% for Petersen’s defect, and 1.1% for jejunojejunostomy mesenteric defect.
Defect closure is known to decrease the incidence of IH after gastrectomy. Kojima et al. and Hosoya et al. reported no incidence of IH in patients with defect closures [21, 22]. In our study, the occurrence of IH was found not only in the non-closure group but also in the closure group. In the closure group, three patients with Petersen’s defects, and five patients with jejunojejunostomy mesenteric defects developed IH after LTG. The occurrence of IH in the closure group may have been due to insufficient closure of the defects. Routine closure of all mesenteric defects with running non-absorbable sutures is recommended for the prevention of IH [6, 12]. Our results also support this recommendation. However, because we did not collect data on suturing methods in this study (i.e., running or interrupted, absorbable or non-absorbable sutures), we could not conclude how defects should be closed.
Laparoscopic surgery for gastrectomy and Roux-en Y gastric bypass is increasing globally [5, 23, 24]. However, several studies have reported that the incidence of IH is significantly higher after laparoscopic surgery than after open surgery due to the reduction of intra-abdominal adhesions in laparoscopic surgery [25, 26]. The incidence of IH after LTG was 2.2% in this study, which was lower than the previous studies [7, 12, 27]. Moreover, Kelly et al. suggested that IH may occur early in the postoperative period because of the reduction in intra-abdominal adhesions [13]. In this study, two patients developed IH within one month of their surgery.
Retro-colic route reconstruction is a risk factor for IH of transverse mesenteric defects. Transverse mesenteric defects created by retro-colic route reconstruction is one of the most common sites of IH [22, 28]. Therefore, ante-colic route reconstruction may be more favorable. However, the size of Petersen’s defects is affected by the reconstruction route and tends to be wider in ante-colic route reconstruction. Cruz-Munoz et al. reported that all patients with Petersen’s defect hernias had undergone ante-colic route reconstruction [28]. Surgeons should, therefore, consider the route of Roux limb reconstruction and should know the pitfalls of the ante-colic and retro-colic routes. In our study, 41 patients were reconstructed using the retrocolic route, and no patients developed IH through transverse mesenteric defects.
The length of the follow-up period may also affect the incidence of IH. The median follow-up period was 948 days in this study. The follow-up period was longer in the non-closure group than in the closure group for both Petersen’s defects and jejunojejunostomy mesenteric defects. This difference is partly because our practice gradually shifted from non-closure to closure in the middle of this study, as IH after LTG was being reported over time. Although the shorter follow-up period of the closure group would account for the lower incidence of IH in the closure group, 14 out of 16 patients developed IH within 2 years in our study. The other two patients, who developed IH after more than two years, were in the closure group. Previous studies have reported that IH occurs mostly within two years of surgery [13, 21, 22, 27]. Therefore, we considered that our follow-up period was sufficient to observe IH, even though it was shorter in the closure group compared to the non-closure group.
In our study, two patients with defect closure had early postoperative IH through jejunojejunostomy mesenteric defect, which occurred on a postoperative day 7 and day 10 (Table 6). Although the detailed causes of IH were unclear due to the unavailability of data on suturing methods (continuous or interrupted), types of thread (absorbable or non-absorbable), and surgeon profiles, it is reasonable to assume that these complications resulted from insufficient closure. Taking our results of multivariable analyses into account that non-closure of Petersen’s and/or jejunojejunostomy mesenteric defects was an independent risk factor for IH, laparoscopic surgeons should pay close attention to the sufficient closure of these defects.
Our study had several limitations. First, this study suffers from inherent limitations due to its retrospective nature. It was impossible to acquire data regarding the detailed procedures of defect closures, or surgeon experience, which may have affected the occurrence of IH. Second, confounders were not adjusted due to the limited number of IH cases. Third, because the closure and non-closure group ratios varied among 13 institutes in this study, there was a potential inter-institutional bias. For both Petersen's defect and jejunojejunostomy mesenteric defect, we confirmed no inter-institutional bias in the occurrence of IH in cases with defect closure (data not shown). On the other hand, the five cases of IH without closure of Petersen’s defect were all from the same institute, and the possibility of an inter-institutional bias cannot be denied (data not shown). However, there was no IH after surgeons changed their practice of non-closure into closure of the defects at that institute, suggesting that defect closure has a preventive effect on IH. Despite these limitations, we were able to show the effectiveness of defect closure in our multicenter study with a substantial sample size of 714 LTG patients and strengthen the evidence of previous studies regarding the prevention of IH.
In our study, the IH occurrence rate, through Petersen’s defects and jejunojejunostomy mesenteric defects after LTG, was lower in patients who underwent defects closure than in those who did not. Since IH sometimes result in critically serious conditions, endoscopic surgeons should take great care to prevent IH by closing defects after LTG. Further studies are necessary to clarify the optimal methods of closing defects, including the type of thread and suturing method.
References
Kim HS, Kim BS, Lee IS, Lee S, Yook JH (2013) Comparison of totally laparoscopic total gastrectomy and open total gastrectomy for gastric cancer. J Laparoendosc Adv Surg Tech A 23:323–331
Katai H, Mizusawa J, Katayama H, Kunisaki C, Sakuramoto S, Inaki N, Kinoshita T, Iwasaki Y, Misawa K, Takiguchi N, Kaji M, Okitsu H, Yoshikawa T, Terashima M (2019) Single-arm confirmatory trial of laparoscopy-assisted total or proximal gastrectomy with nodal dissection for clinical stage I gastric cancer: Japan clinical oncology group study JCOG1401. Gastric Cancer 22:999–1008
Hyung WJ, Yang HK, Han SU, Lee YJ, Park JM, Kim JJ, Kwon OK, Kong SH, Kim HI, Lee HJ, Kim W, Ryu SW, Jin SH, Oh SJ, Ryu KW, Kim MC, Ahn HS, Park YK, Kim YH, Hwang SH, Kim JW, Cho GS (2019) A feasibility study of laparoscopic total gastrectomy for clinical stage I gastric cancer: a prospective multi-center phase II clinical trial, KLASS 03. Gastric Cancer 22:214–222
Iannelli A, Facchiano E, Gugenheim J (2006) Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg 16:1265–1271
Marema RT, Perez M, Buffington CK (2005) Comparison of the benefits and complications between laparoscopic and open Roux-en-Y gastric bypass surgeries. Surg Endosc 19:525–530
Paroz A, Calmes JM, Giusti V, Suter M (2006) Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity: a continuous challenge in bariatric surgery. Obes Surg 16:1482–1487
Kang KM, Cho YS, Min SH, Lee Y, Park KB, Park YS, Ahn SH, Park DJ, Kim HH (2019) Internal hernia after gastrectomy for gastric cancer in minimally invasive surgery era. Gastric Cancer 22:1009–1015
Higa KD, Ho T, Boone KB (2003) Internal hernias after laparoscopic Roux-en-Y gastric bypass: incidence, treatment and prevention. Obes Surg 13:350–354
Capella RF, Iannace VA, Capella JF (2006) Bowel obstruction after open and laparoscopic gastric bypass surgery for morbid obesity. J Am Coll Surg 203:328–335
Rosas U, Ahmed S, Leva N, Garg T, Rivas H, Lau J, Russo M, Morton JM (2015) Mesenteric defect closure in laparoscopic Roux-en-Y gastric bypass: a randomized controlled trial. Surg Endosc 29:2486–2490
Stenberg E, Szabo E, Agren G, Ottosson J, Marsk R, Lonroth H, Boman L, Magnuson A, Thorell A, Naslund I (2016) Closure of mesenteric defects in laparoscopic gastric bypass: a multicentre, randomised, parallel, open-label trial. Lancet 387:1397–1404
Kimura H, Ishikawa M, Nabae T, Matsunaga T, Murakami S, Kawamoto M, Kamimura T, Uchiyama A (2017) Internal hernia after laparoscopic gastrectomy with Roux-en-Y reconstruction for gastric cancer. Asian J Surg 40:203–209
Kelly KJ, Allen PJ, Brennan MF, Gollub MJ, Coit DG, Strong VE (2013) Internal hernia after gastrectomy for cancer with Roux-Y reconstruction. Surgery 154:305–311
Murakami K, Obama K, Tsunoda S, Hisamori S, Nishigori T, Hida K, Kanaya S, Satoh S, Manaka D, Yamamoto M, Kadokawa Y, Itami A, Okabe H, Hata H, Tanaka E, Yamashita Y, Kondo M, Hosogi H, Hoshino N, Tanaka S, Sakai Y (2020) Linear or circular stapler? A propensity score-matched, multicenter analysis of intracorporeal esophagojejunostomy following totally laparoscopic total gastrectomy. Surg Endosc 34:5265–5273
Japanese Gastric Cancer Association (2011) Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 14:101–112
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Japanese Gastric Cancer Association (2017) Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 20:1–19
Satoh S, Okabe H, Kondo K, Tanaka E, Itami A, Kawamura J, Nomura A, Nagayama S, Watanabe G, Sakai Y (2009) Video. A novel laparoscopic approach for safe and simplified suprapancreatic lymph node dissection of gastric cancer. Surg Endosc 23:436–437
Okabe H, Obama K, Kan T, Tanaka E, Itami A, Sakai Y (2010) Medial approach for laparoscopic total gastrectomy with splenic lymph node dissection. J Am Coll Surg 211:e1-6
Okabe H, Satoh S, Inoue H, Kondo M, Kawamura J, Nomura A, Nagayama S, Hasegawa S, Itami A, Watanabe G, Sakai Y (2007) Esophagojejunostomy through minilaparotomy after laparoscopic total gastrectomy. Gastric Cancer 10:176–180
Hosoya Y, Lefor A, Ui T, Haruta H, Kurashina K, Saito S, Zuiki T, Sata N, Yasuda Y (2011) Internal hernia after laparoscopic gastric resection with antecolic Roux-en-Y reconstruction for gastric cancer. Surg Endosc 25:3400–3404
Kojima K, Inokuchi M, Kato K, Motoyama K, Sugihara K (2014) Petersen’s hernia after laparoscopic distal gastrectomy with Roux-en-Y reconstruction for gastric cancer. Gastric Cancer 17:146–151
Kodera Y, Fujiwara M, Ohashi N, Nakayama G, Koike M, Morita S, Nakao A (2010) Laparoscopic surgery for gastric cancer: a collective review with meta-analysis of randomized trials. J Am Coll Surg 211:677–686
Kim W, Kim HH, Han SU, Kim MC, Hyung WJ, Ryu SW, Cho GS, Kim CY, Yang HK, Park DJ, Song KY, Lee SI, Ryu SY, Lee JH, Lee HJ (2016) Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: short-term outcomes from a multicenter randomized controlled trial (KLASS-01). Ann Surg 263:28–35
Cho M, Pinto D, Carrodeguas L, Lascano C, Soto F, Whipple O, Simpfendorfer C, Gonzalvo JP, Zundel N, Szomstein S, Rosenthal RJ (2006) Frequency and management of internal hernias after laparoscopic antecolic antegastric Roux-en-Y gastric bypass without division of the small bowel mesentery or closure of mesenteric defects: review of 1400 consecutive cases. Surg Obes Relat Dis 2:87–91
de la Cruz-Munoz N, Cabrera JC, Cuesta M, Hartnett S, Rojas R (2011) Closure of mesenteric defect can lead to decrease in internal hernias after Roux-en-Y gastric bypass. Surg Obes Relat Dis 7:176–180
Miyagaki H, Takiguchi S, Kurokawa Y, Hirao M, Tamura S, Nishida T, Kimura Y, Fujiwara Y, Mori M, Doki Y (2012) Recent trend of internal hernia occurrence after gastrectomy for gastric cancer. World J Surg 36:851–857
Yoshikawa K, Shimada M, Kurita N, Sato H, Iwata T, Higashijima J, Chikakiyo M, Nishi M, Kashihara H, Takasu C, Matsumoto N, Eto S (2014) Characteristics of internal hernia after gastrectomy with Roux-en-Y reconstruction for gastric cancer. Surg Endosc 28:1774–1778
Funding
Operating support grants from Kyoto University supported this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Katsuhiro Murakami, Kazutaka Obama, Seiichiro Kanaya, Seiji Satoh, Dai Manaka, Michihiro Yamamoto, Yoshio Kadokawa, Atsushi Itami, Hiroshi Okabe, Hiroaki Hata, Eiji Tanaka, Yoshito Yamashita, Masato Kondo, Hisahiro Hosogi, Shigeru Tsunoda, Shigeo Hisamori, Tatsuto Nishigori, and Yoshiharu Sakai have no conflicts of interest or financial ties to disclose.
Ethical approval
The Kyoto University ethics committee and all the hospitals involved approved this multicenter, retrospective, comparative study (R1276). This study was conducted in accordance with the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This paper was based on a previous communication to the 91st Annual Meeting of the Japanese Gastric Cancer Association.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Murakami, K., Obama, K., Kanaya, S. et al. Mesenteric closure after laparoscopic total gastrectomy with Roux-en-Y reconstruction is effective for prevention of internal hernia: a multicenter retrospective study. Surg Endosc 36, 4181–4188 (2022). https://doi.org/10.1007/s00464-021-08744-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08744-z