Abstract
Background
In recent years, there has been an increase in numbers of individuals seeking laparoscopic surgical procedures for obesity. The current study compared the benefits and risks between laparoscopic and open Roux-en-Y gastric bypass (RYGBP) performed at the same center for more than 2,000 patients.
Methods
The study population consisted of 1,077 laparoscopic and 1,198 open RYGBP procedures performed between the years 1999 and 2002. Measurements included population characteristics, anthropometries, complications, and hospital stay.
Results
The laparoscopic RYGBP has both advantages and disadvantages. The disadvantages include a longer operative time and a higher incidence of fistulas, internal hernias, and small bowel obstruction. The advantages of the laparoscopic procedure are shorter hospital stay, lower incidence of wound infection, and fewer incisional hernias. Both procedures cause similar changes in body weight, but laparoscopic RYGBP is associated with less lean tissue loss during the early postoperative period.
Conclusion
Both laparoscopic and open RYGBP are effective in inducing massive weight loss. There are, however, differences in the benefits and risks between the two procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obesity has become a major health problem worldwide. Surgical procedures for the treatment of obesity have become increasingly popular because nonsurgical methods have shown low rates of success. In the United States, the surgical procedure of choice for the treatment of morbid obesity is the Roux-en-Y gastric bypass (RYGBP). The original gastric bypass, a loop gastrojejunostomy, was first reported in 1967 by Dr. Edward Mason [5]. The procedure has since undergone various modifications. In its current state, the RYGBP has demonstrated many years of safety and efficacy [18].
In 1994, Dr. Alan Wittgrove and colleagues [21] reported their experience with laparoscopic RYGBP in a small series. Since that time, other larger series have been reported [1, 2, 4, 6-11, 12-17, 19, 20]. Many authors have stressed the complexity and technical challenges of this procedure, as well as the long learning curve involved. Laparoscopic RYGBP is becoming the procedure of choice in the United States for the treatment of morbid obesity.
Whereas the advantages and disadvantages of the laparoscopic RYGBP have been reported [1, 2, 6-10, 12, 14, 17, 19], few comparative large-scale studies have analyzed the procedure’s benefits and risks. In our study, we compared the risks and benefits of laparoscopic and open RYGBP procedures in a population of more than 2,000 bariatric patients whose surgeries were performed at a single center.
Methods
Study population
The study population consisted of 2,275 morbidly obese patients who underwent silastic ring RYGBP at our center between the years 1999 and 2002. The mean age of the population was 44.3 ± 3.3 years. The mean weight was 138.4 ± 1.0 kg (range, 85-312 kg), and the average body mass index (BMI) was 50 ± 2 (range, 36-103). Approximately half the population (48.5%) suffered from supermorbid obesity (BMI > 50).
The gender distribution of the study population was 83% female and 17% male. The racial profiles of the patients were as follows: 65% white, 22% Hispanic, 7% black, and 7% Asian, American Indian, and other. The total number of comorbid diseases in the population was 3.6. The incidence rates for comorbidities were as follows: osteoarthritis (69%), diabetes (33%), back problems (36%), hypertension (43%), heart disease (11%), sleep apnea (46%) lipid abnormalities (44%), and gastrointestinal reflux disease (46%).
Roux-en-Y gastric bypass: open and laparoscopic
All the patients underwent the silastic ring RYGBP. An upper midline incision was used for the open RYGBP. The fascia was closed with a no. 1 looped PDS suture, and the skin was closed with a running 3-0 monocryl suture. For the laparoscopic procedure, 6 bladeless trocars were placed. The largest trocar site, dilated to accommodate the circular stapler, was closed with .a zero prolene suture. All skin incisions were closed with 4-0 vicryl suture. Steristrips were used for both laparoscopic and open incisions.
In all patients, a 2.5 - 3.0 cm transverse by 6.0 cm longitudinal pouch was created, based on the stomach’s lesser curvature, with preservation of the neurovascular bundle. Both the pouch and excluded stomach were oversewn with Vicryl suture after complete transection. A 6 cm nonsupported silastic ring was placed on the pouch approximately 1 cm from its distal point. The linear cutter stapler was used both to transect the small bowel and to perform a side-to-side jejunojejunostomy. The remaining enterotomy was closed with a running Vicryl suture in two layers. The Roux limb was brought up in a retrocolic, retrogastric fashion after creation of an opening in the transverse mesocolon. An anastomosis to the pouch was performed with a 21-mm Ethicon circular stapler in an end-to-side fashion. The opening in the small bowel, which had been created to place the circular stapler, was closed with the linear cutter stapler. All mesocolic and mesenteric defects were closed with running silk suture.
A percutaneous gastrostomy tube using a 16-Fr silastic Foley catheter was placed in the excluded stomach in all cases. Its position was marked with a silastic ring to allow future access to the excluded stomach, if necessary. All gastrostomy tubes were routinely removed in 10 to 14 days. The only difference in surgical technique between the laparoscopic and open procedures was the routine performance of a cholecystectomy with the open RYGBP.
All the patients underwent routine upper gastrointestinal tract radiography (UGI) in the postoperative period. The UGI for the laparoscopic patients was performed on postoperative day 1, whereas the UGI for the open patients was 10 to 14 days postoperatively. In both groups, the G-tube was removed if the UGI showed no leak and the patient was tolerating oral intake well at 10 to 14 days. Although differences in the timing of the routine UGI between the two procedures could have resulted in failure to detect an anastomotic leak, no patients had clinical signs suggesting that a leak was overlooked in the series, and there were no significant differences in the rates of leaks between the procedures (see Results section). At 1 year, all the patients (100%) underwent a repeat UGI to assess pouch size and to rule out gastrogastric fistula. Other diagnostic studies and procedures, such as a computed tomography (CT) scan and upper endoscopy, were performed on an individual basis, if symptoms warranted. The patients were followed for a minimum of 1 year postoperatively.
Procedure selection
Of the 2,275 patients, 1,198 had the open RYGBP and 1,077 patients had the laparoscopic procedure. The type of surgery to be performed was decided by both the operating surgeon and the patient. Some patients opted for the open procedure because of its known efficacy and safety. Others were scheduled for open RYGBP on the basis of multiple criteria such as a history of multiple previous upper abdominal operations or a BMI greater than 60. Patients with gallstones and a desire or need for cholecystectomy at the same time were treated with open RYGBP, as well. A cholecystectomy with the open RYGBP was standard procedure throughout the 3-year surgical period.
All patients not excluded by the preceding criteria were treated with laparoscopic RYGBP. Over the 3-year period, an increasingly greater number of laparoscopic procedures were performed each year as both patient and physician confidence in the procedure increased. Even patients with multiple previous operations, higher BMI, and revisions were treated via laparoscopy toward the end of the 3-year period.
Complications
The complications and benefits associated with each of the procedures studied involved the following: length of hospital stay, length of the operative procedure, changes in anthropometries, and incidence rates of short- and long-term surgical complications including liver laceration, incidental splenectomy, anastomotic leak, wound infection, gastrogastric fistula, small bowel obstruction/internal hernia, incisional hernia repair, silastic ring removed, and mortality. (Note that data were not available in this series for assessment of anastomotic stricture, although strictures did occur and were treated by endoscopy and balloon dilation without the need for surgical revision.) The incidence rates for complications are for those that occurred over a minimum of 1 year postoperatively, and represent the average complication rates associated with each of the procedures.
Anthropometrics
The anthropometric measurements for the laparoscopic and open RYGBP patients included height, weight, and BMI, determined before surgery, then 1, 3, 6, and 12 months postoperatively. In a subset population (n = 162) of laparoscopic and open procedure patients, changes in body composition were determined before and at 3 months after surgery. The subpopulation included females only to exclude the influence of sex hormone differences in changes in lean tissue and fat composition.
Body composition was measured using bioelectric impedance (Tanita) and included measurement of lean body tissue mass, fat mass, percentage of body fat, body weight, BMI, and total body water. The effects of the laparoscopic or open RYGBP procedures on lean tissue, fat mass, and total body weight were expressed as the percentage change from preoperative values.
Statistical analysis
Data are expressed as mean ± standard error of the mean. Statistical differences between the laparoscopic and open procedures for the various indices measured were determined using a one-way analysis of variance (ANOVA), followed by pairwise comparisons using Fisher’s protected least significant difference. Comparison of percentage changes over time for the population at large and the subset population was determined using a repeated measures ANOVA. Differences between complications rates of the procedures were determined using chi-square analyses. Statistical analysis was performed using biomedical software (Statview, SAS Institute).
Results
Table 1 presents the characteristics of the 1,077 laparoscopic and the 1,198 open procedure patients. Both groups were similar with regard to age and gender distribution. The open RYGBP patients were significantly (p < 0.01) heavier than their laparoscopic cohort (132 vs 148 kg; BMI 48 vs 52). In spite of differences in body size, there were, however, no apparent differences in preoperative health status between the study groups. The total number of major co-morbidities (diabetes, heart disease, hypertension, sleep apnea, osteoarthritis, gastroesophageal reflux disease, obstructive airway disease) in the laparoscopic and open procedure groups did not differ significantly (3.5 vs 3.7, respectively; p > 0.05).
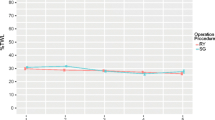
Among all the patients studied, the total length of hospital stay was significantly less for the laparoscopic than for the open procedure cases (Fig. 1). The patients who underwent laparoscopic surgery, on the average, were discharged from the hospital nearly a day before the open procedure patients (3.4 vs 4.3 days, respectively). The operative time for the laparoscopic RYGBP ranged between 90 min and 4 h during the learning curve for the procedure (first 100 cases). The average operating time for subsequent laparoscopic procedures was 95 min, which was only 10 min longer than for the open RYGBP (85 min).
Table 2 presents differences and similarities in the incidence rates between short- and long-term RYGBP surgical complications. The laparoscopic patients had a slightly greater risk, albeit nonsignificant, for anastomotic leak than the open procedure patients. The incidence rates (although low) for gastrogastric fistulas, small bowel obstructions, and internal hernias were significantly (p < 0.01) higher for the laparoscopic than for the open procedure patients. Alternatively, open RYGBP was associated with a higher incidence of incisional hernias requiring repair (p < 0.01) and a greater incidence of wound infection (p < 0.01). The 30-day postoperative rates of mortality did not significantly differ between the procedures in our series (0.1% vs 0.3%) respectively, for the laparoscopic and open RYGBP), although the absolute number of mortalities was greater for the open procedure (4 deaths vs 1 death). Other complications included a liver laceration in two laparoscopic patients, three incidental splenectomies attributable to iatrogenic injury for the open procedure, and three silastic ring erosions requiring surgical repair for two laparoscopic procedures and one open case.
Both RYGBP entry procedures resulted in similar percentage changes in total body weight at 1, 3, 6, and 12 months after surgery (Fig. 2). Changes in body weight for both procedure groups postoperatively averaged approximately 11% at 1 month, 23% at 3 months, 34% at 6 months, and 42% at 1 year after surgery, with no statistical differences (p > 0.05) between the groups at any of the measurement periods.
Figure 3A, B, and C illustrate the percentage changes in body weight, total fat mass, and total lean tissue at postoperative month 3 for a subset population of morbidly obese laparoscopic (n = 79) and open (n = 83) procedure patients. As can be seen, the percentage changes in body weight did not differ significantly between the laparoscopic and open procedure. However, individuals who underwent laparoscopic RYGBP lost significantly (p > 0.05) more fat (32% vs 28%) and less lean body tissue (8% vs 13%) than did their open procedure cohorts.
Discussion
The current research findings are based on the largest number of laparoscopic and open RYGBP patients from a single center reported to date. The study shows advantages and disadvantages for the utilization of laparoscopic procedures in performance of RYGBP.
One frequently reported disadvantage of laparoscopic RYGBP is that the surgery is longer than for the open procedure [6, 9, 12, 17]. The average operative time for our laparoscopic procedures was only 10 min longer than for the open procedure (95 vs 85 min). Other surgeons, using slightly differing RYGBP techniques, have reported somewhat greater differences in operative times between the procedures. Nguyen et al. [6, 9, 12] found that the laparoscopic RYGBP required approximately 30 min more time than the open RYGBP: 246 vs 194 min in one series [6] and 232 vs 201 min in another series [9]. Smith et al. [17] also reported an approximate 30-min longer operative time for the laparoscopic than for the open RYGBP procedure.
Increased operative time and the greater expense of surgical supplies and specialized equipment add to operative cost, posing another disadvantage with the use of the laparoscopic procedure. In our study, the extra cost of specialized equipment and surgical supplies for the laparoscopic procedure resulted in a higher operative cost, $2,600 for the laparoscopic vs $790 for the open procedure; (data not shown). Nguyen et al. [12], on examining the total cost of the procedure (operative time, supplies, and post-anesthesia) of their series, found that the operative cost for the laparoscopic RYGBP was higher than for the open RYGBP, but that the hospital service costs were significantly lower for the laparoscopic surgery. These investigators determined that the “total cost” of both procedures is nearly identical when the direct and indirect hospital costs for each of the procedures are computed.
The hospital costs of the laparoscopic procedure are likely to be lower than for the open RYGBP, in part because of a shortened length of hospital stay. Our study found that the length of hospital stay for laparoscopic patients was nearly 1 day less than for patients who had undergone open RYGBP procedure, (3.4 vs 4.2 days). Other investigators, likewise, have reported an approximate 1-day difference in the length of hospital stay between the procedures [1, 2, 7, 9, 17, 19].
In our series, the open and laparoscopic procedures differed in the type and frequency of postgastric bypass complications. According to the data, 7 of the 1,077 laparoscopic patients developed a gastrogastric fistula, and 16 of the laparoscopic patients had small bowel obstructions or internal hernias requiring surgical repair. None of the open procedure patients experienced a fistula or a small bowel obstruction. Other investigators [1, 7, 17] have, likewise, reported higher incidences of small bowel obstruction and internal hernias with the laparoscopic than with the open RYGBP. Podnos et al. [14], in a meta-analysis of data from 8 studies involving 2,771 open RYGBP patients and 10 studies involves 3,464 laparoscopic RYGBP patients, found that the laparoscopic procedure is associated with a higher frequency of early and late bowel obstructions and stomal stenosis.
The meta-analysis of open vs laparoscopic RYGBP studies by Podnos et al. [14] further showed that, in contrast to the laparoscopic procedure, patients having the open RYGBP experience a higher frequency of incidental splenectomies and have a greater incidence of wound infections and incisional hernias. In our series, we also found among the open procedure RYGBP patients higher incidences of wound infection (12% vs 6%), splenectomies (0.3% vs 0%) and incisional hernias requiring surgical repair (1.2% vs 0.2%). Studies also have reported a higher mortality rate for the open than for the laparoscopic RYGBP [7, 14]. In our series, there were no statistically significant differences in mortality rates between the procedures (0.1% vs 0.3%), although a greater total number of open procedure patients died during the 30-day postoperative period. According to our findings, 1 of the 1,077 laparoscopic patients died 30 days after RYGBP. The cause of this death (a perforated appendix) was unrelated to the surgery. Among the 1,198 open procedure patients, 4 died: one succumbed to pulmonary emboli; another had an intracranial hemorrhage; a third patient died of cardiac arrest; and only one patient died of an event related to the surgical procedure (an anastomotic leak).
Possible causes for the higher mortality rates associated with the open than with the laparoscopic RYGBP reported for other series [7, 14], along with the longer hospital stay found in our series and observed by others [1, 2, 7, 9, 17, 19], are unclear. The RYGBP performed as an open procedure apparently causes greater trauma than if performed laparoscopically. Blood loss during the open procedure is reported to be threefold that during laparoscopic RYGBP, resulting in a significantly greater need for blood replacement through transfusion [7, 9]. Time spent in the intensive care unit after open RYGBP also is found to be substantially more than when the surgery is performed laparoscopically [7, 9]. Hypoxia, atelectasis, and the suppression of respiratory functions are more prevalent among open than among laparoscopic patients [10], possibly at least, partly because of the greater need for pain control among open procedure patients [10, 19]. The open procedure also is associated with significantly higher production of norepinephrine, adrenocorticotropic hormone (ACTH), C-reactive protein, and interleukin-6 than the RYGBP procedure, suggesting greater operative injury [8].
Differences in preoperative body size also could have contributed to the longer hospital stay among our open than among our laparoscopic RYGBP patients. The open procedure patients in our series were significantly larger than their laparoscopic counterparts. However, both procedure groups had similar numbers of major comorbidities, suggesting that preoperative health status was similar. Furthermore, in other studies comparing open and laparoscopic RYGBP [11], body size was found not to be a significant predictor of complication rates or surgical outcome.
Changes in body size during all periods postoperatively up to 1 year were nearly identical for the open and laparoscopic patients. Because of preoperative differences in body size between the procedure groups, changes in body size after surgery were expressed as a percentage change in total body weight. Several investigators have, likewise, found nearly identical changes in body size 1 year after the laparoscopic and open RYGBP procedures, with values expressed as a percentage change in excess body weight or as absolute changes in BMI [1, 7, 9, 17, 19]. Such findings would be expected because the RYGBP operation is the same regardless of the mode of access.
Some investigators have reported similar changes in weight loss between the laparoscopic and open procedures 1 year after RYGBP, but their findings have shown significantly greater weight loss for the laparoscopic patients in the earlier postoperative periods [8]. Our study, in contrast, found identical percentage changes in weight between the procedure groups during all observation periods up to 1 year. However, in the early postoperative period, we did find more favorable body composition changes with the laparoscopic than with the open procedure.
In a subset population of patients, changes in body weight and body composition were followed over the first 3 postoperative months, a period previously reported to be associated with the greatest loss of lean body tissue after RYGBP [3]. Individuals who underwent the laparoscopic procedure showed no greater loss in total body weight than those who had the open RYGBP. Nonetheless, changes in body weight for the laparoscopic patients were associated with significantly greater loss of body fat and less loss of lean body tissue.
The preferential loss of fat mass and reduced loss of lean body tissue with the laparoscopic procedure, as compared with the open procedure, likely resulted from a faster rate of postsurgery recovery. Several studies have reported faster rates of total recovery or return to activities after laparoscopic RYGBP [1, 2, 7, 10, 19]. Levels of physical activity as well as social functions and overall feelings of well-being also reported to be higher in the early postoperative periods for individuals having the laparoscopic procedure [2, 7].
In summary, we have found in more than 2,000 RYGBP patients from the same center that the laparoscopic procedure has both advantages and disadvantages. The disadvantages include a longer operative time and a higher incidence of fistulas, internal hernias, and small bowel obstruction. The advantages of the laparoscopic procedure are a shorter hospital stay and reduced incidences of wound infection, incisional hernias, and mortality. Both procedures cause similar changes in body weight, but laparoscopic RYGBP is associated with less lean tissue loss during the early postoperative period. We conclude that both laparoscopic and open RYGBP are effective in inducing massive weight loss. There are, however, differences in the benefits and risks between the procedures.
References
A Courcoulas Y Perry P Buenaventura J Luketich (2003) ArticleTitleComparing the outcomes after laparoscopic versus open gastric bypass: a matched paired analysis Obes Surg 13 341–346 Occurrence Handle10.1381/096089203765887624 Occurrence Handle12841890
BL Fisher (2004) ArticleTitleComparison of recovery time after open and laparoscopic gastric bypass and laparoscopic adjustable banding Obes Surg 14 67–72 Occurrence Handle10.1381/096089204772787310 Occurrence Handle14980036
M Gordon (1993) ArticleTitleMetabolic changes after Roux-en-Y gastric bypass: a preliminary report Obes Surg 3 425–428 Occurrence Handle10.1381/096089293765559151 Occurrence Handle10757957
KD Higa KB Boone T Ho (2000) ArticleTitleComplications of the laparoscopic Roux-en-Y gastric bypass: 1,040 patients - What have we learned? Obes Surg 10 509–513 Occurrence Handle10.1381/096089200321593706 Occurrence Handle1:STN:280:DC%2BD3M7ks1WjtQ%3D%3D Occurrence Handle11175957
EE Mason C Ito (1967) ArticleTitleGastric bypass in obesity Surg Clin North Am 47 1345–1351 Occurrence Handle1:STN:280:CCeD1M3nt1Q%3D Occurrence Handle6073761
NT Nguyen NW Fleming A Singh SJ Lee CD Goldman BM Wolfe (2001) ArticleTitleEvaluation of core temperature during laparoscopic vs open gastric bypass Obes Surg 11 570–575 Occurrence Handle10.1381/09608920160557039 Occurrence Handle1:STN:280:DC%2BD3MrkslOiuw%3D%3D Occurrence Handle11594097
NT Nguyen C Goldman CJ Rosenquist A Arango CJ Cole SJ Lee BM Wolfe (2001) ArticleTitleLaparoscopic versus open gastric bypass: a randomized study outcomes, quality of life, and costs Ann Surg 234 279–291 Occurrence Handle10.1097/00000658-200109000-00002 Occurrence Handle1:STN:280:DC%2BD3MvotVymtA%3D%3D Occurrence Handle11524581
NT Nguyen CD Goldman HS Ho RC Gosselin A Singh BM Wolfe (2002) ArticleTitleSystemic stress response after laparoscppic and open gastric bypass J Am Coll Surg 194 557–567 Occurrence Handle10.1016/S1072-7515(02)01132-8 Occurrence Handle12022597
NT Nguyen HS Ho LS Palmer BM Wolfe (2000) ArticleTitleA comparison study of laparoscopic versus open gastric bypass for morbid obesity J Am Coll Surgeons 191 149–157 Occurrence Handle10.1016/S1072-7515(00)00276-3 Occurrence Handle1:STN:280:DC%2BD3cvgvFKitw%3D%3D
NT Nguyen SL Lee C Goldman N Fleming A Arango R McFall BM Wolfe (2001) ArticleTitleComparison of pulmonary function and postoperative pain after laparoscopic versus open gastric bypass: a randomized trial J Am Coll Surg 192 469–477 Occurrence Handle10.1016/S1072-7515(01)00822-5 Occurrence Handle1:STN:280:DC%2BD3M3ivFSktg%3D%3D Occurrence Handle11294404
NT Nguyen R Rivers BM Wolfe (2003) ArticleTitleFactors associated with operative outcomes in laparoscopic gastric bypass J Am Coll Surg 197 548–557 Occurrence Handle10.1016/S1072-7515(03)00648-3 Occurrence Handle14522321
NT Nguyen BM Wolfe (2002) ArticleTitleLaparoscopic versus open gastric bypass Semin Laparosc Surg 9 86–93 Occurrence Handle10.1053/slas.2002.126330 Occurrence Handle12152151
T Olbers H Lonroth M Fageyik-Olsen L Lundell (2003) ArticleTitleLaparoscopic gastric bypass: development of technique, respiratory function, and long-term outcome Obes Surg 13 364–370 Occurrence Handle10.1381/096089203765887679 Occurrence Handle12841895
YD Podnos JC Jimenez SE Wilson CM Stevens NT Nguyen (2003) ArticleTitleComplications after laparoscopic gastric bypass: a review of 3,464 cases Arch Surg 138 957–961 Occurrence Handle12963651
PR Schauer S Ikramuddin W Gourash R Ramanathan J Luketich (2000) ArticleTitleOutcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity Ann Surg 232 515–529 Occurrence Handle10.1097/00000658-200010000-00007 Occurrence Handle1:STN:280:DC%2BD3M%2Fhs1eitA%3D%3D Occurrence Handle10998650
C See PL Carter D Elliott P Mullenix W Eggebroten C Porter D Watts (2002) ArticleTitleAn institutional experience with laparoscopic gastric bypass complications seen in the first year compared with open gastric bypass complications during the same period Am J Surg 183 533–538 Occurrence Handle10.1016/S0002-9610(02)00829-2 Occurrence Handle12034387
SC Smith CB Edwards GN Goodman RC Halversen SC Simper (2004) ArticleTitleOpen vs laparoscopic Roux-en-Y gastric bypass: comparison or operative morbidity and mortality Obes Surg 14 73–76 Occurrence Handle10.1381/096089204772787329 Occurrence Handle14980037
HJ Sugerman (2001) ArticleTitleBariatric surgery for severe obesity J Assoc Acad Minor Phys 12 129–136 Occurrence Handle1:STN:280:DC%2BD387hs1yhsA%3D%3D Occurrence Handle11851201
A Westling S Gustavsson (2001) ArticleTitleLaparoscopic vs open Roux-en-Y gastric bypass: a prospective randomized trial Obes Surg 11 284–292 Occurrence Handle1:STN:280:DC%2BD38%2FhslSrsg%3D%3D Occurrence Handle11433902
AC Wittgrove GW Clark (2000) ArticleTitleLaparoscopic gastric bypass, Roux-en-Y in 500 patients: technique and results, with 3- to 60-month follow-up Obes Surg 10 233–239 Occurrence Handle10.1381/096089200321643511 Occurrence Handle1:STN:280:DC%2BD3cvotFOlsQ%3D%3D Occurrence Handle10929154
AC Wittgrove GW Clark LJ Tremblay (1994) ArticleTitleLaparoscopic gastric bypass, Roux-en-Y: preliminary report of five cases Obes Surg 4 353–357 Occurrence Handle10.1381/096089294765558331 Occurrence Handle10742801
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marema, R.T., Perez, M. & Buffington, C.K. Comparison of the benefits and complications between laparoscopic and open Roux-en-Y gastric bypass surgeries. Surg Endosc 19, 525–530 (2005). https://doi.org/10.1007/s00464-004-8907-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-004-8907-9