Abstract
Background
Internal hernia is a rare but a potentially fatal complication of laparoscopic Roux-En-Y gastric bypass (LRYGB). The aims of this study are to determine the impact of mesenteric defects closure on the incidence of internal hernia after LRYGB and to determine the symptoms, characteristics, and management of internal hernias after LRYGB.
Methods
A retrospective study for a total of 2093 LRYGB was carried out from 1998 to December 2013. Four hundred twenty-one patients were operated without closure of the mesenteric defects (group A). From January 2005 to December 2013, 1672 patients were operated with closure of the mesenteric defects at Petersen defect (PD) and at jejunojejunal anastomosis (J-J) defect (group B). The incidence of internal hernias was compared between the two periods.
Results
Out of the 2093 patients who underwent LRYGB, 20 patients (0.95%) developed a symptomatic internal hernia that required primary surgical intervention; 7 patients (1.66%) in group A all at J-J DEFECT versus 13 patients (0.78%) in (group B) 6 at (J-J DEFECT), 5 at PD, and 2 at PD, J-J DEFECT. This incidence was significantly lower in (group B) (p = 0.0021). The median interval between LRYGB and reoperation was 53 months in group A and 26 months in group B. A CT scan was performed in 8 patients, 40%, and showed signs of occlusion in all cases.
Conclusions
The closure of mesenteric defects during LRYGB is recommended because it is associated with a significant reduction in the incidence of internal hernia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity represents a major health problem worldwide [1, 2] and is associated with many major comorbidities [3,4,5]. Bariatric surgery has become the most popular therapeutic option for managing morbid obesity. Laparoscopic Roux-en-Y gastric bypass (RYGB) is one of the most performed bariatric/metabolic operations across the world, counting for 30.1% of all procedures. The RYGB remains and is considered by many surgeons as the gold standard. It represents the first most performed procedure in some European countries and in Latin America. Since 2016, in France, sleeve gastrectomy (SG) has been the most frequently performed bariatric procedure representing 64.9% of all procedures and laparoscopic Roux-en-Y gastric bypass (RYGB) became, with one anastomosis gastric bypass (OAGB), the second most frequently performed bariatric procedure at 14% [6]. In other countries, such as the USA, Canada, and Australia, SG also become the most frequently performed bariatric procedure [6]. Besides significant and lasting weight loss, it can improve or resolve obesity-related comorbidities (hypertension, diabetes, hypercholesterolemia, and obstructive sleep apnea) [7].
The advantages of laparoscopy compared to the open technique have been widely demonstrated. Nonetheless, the laparoscopic approach appears to be associated with a higher incidence of internal hernias, which is the most common late postoperative complication. According to studies, the incidence of internal hernias following Roux-en-Y gastric bypass with mesenteric defects closure ranges from 2 to 9%, depending on the loss of abdominal fat and the surgical techniques performed [8,9,10,11]. Possible sites of herniation include J-J defect, Petersen defect (PD), and transverse mesocolon defect. The interval between the surgical procedure and the onset of clinical presentation is highly variable [9, 11, 12]. The complications of internal hernias may include small-bowel obstructions, leading to gastric remnant dilatation, anastomotic leakage, and bowel ischemia with risk of perforation. The mortality rate associated with internal hernias after LRYGBP is 1.6% [8, 9].
The aims of this study are:
-
1)
To determine the impact of mesenteric defects closure on the incidence of internal hernia after (LRYGB);
-
2)
To determine the symptoms, characteristics, and management of internal hernia after (LRYGB).
Methods
This is a retrospective study of a total of 2093 LRYGB which were carried out at Nice University Hospital “L’Archet 2” at the Department of Gastrointestinal Surgery and Liver Transplantation.
The data were retrospectively analyzed from a prospectively collected database at our center for morbidly obese patients undergoing bariatric surgery, and included the following: age, gender, an interval of time elapsed between LRYGBP and internal hernia, BMI (at time of LRYGBP, as well as at incidence of internal hernia), weight loss, previous bariatric procedures, type of clinical presentation (acute versus chronic), symptoms and signs, contribution of imaging to diagnosis, closure of defects at time of LRYGB, surgical treatment (laparotomy versus laparoscopy, localization of internal hernia, reduction of internal hernia, and defect repair with or without bowel resection and associated procedures), postoperative complications, and mortality.
This study was carried out from 1998 to December 2013. A total of 421 patients were operated on without closure of the mesenteric defects (group A). From January 2005 to December 2013, 1672 patients were operated with closure of the mesenteric defects at Petersen defect (PD) and at J-J defect (Group B). The incidence of internal hernias was compared between two periods.
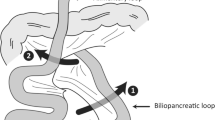
In the postoperative phase, the follow-up was carried out according to local institutional protocols: every 3 months the first year and every 6 months the second and third year. After 3 years, the follow-up was scheduled annually. In group A, the follow-up data at 5, 8, and 10 years after surgery were collected, respectively, for 70.2%, 52.4%, and 22.1% of patients. While in group B, the follow-up rate at 5, 8, and 10 years after surgery was 73%, 54.4%, and 26.4% of patients, respectively. A follow-up rate of 100% was recorded at least at the 20th and 24th month after surgery in group A and group B, respectively. LRYGB was defined as a procedure that was attempted and completed laparoscopically. Patients undergoing either open RYGB or conversion to open RYGB were excluded. Relevant surgical technique details of the standard laparoscopic technique for LRYGBP adopted at our center include the following: the ad hoc division of the greater omentum when too thick; the gastric pouch size of ≤ 30 mL, and the vertical orientation with the gastro-jejunostomy constructed over a 34-French bougie using handsewn gastro-jejunal anastomosis remained constant throughout the period of this study. The biliopancreatic limb was 50 cm from the ligament of Treitz without division of the mesentery, and the length of alimentary limb was 150 cm, the positioning of Roux en-Y was anterior to the transverse colon according to the antecolic technique and it was right-oriented with the cut end of the bowel pointing to the greater curvature of the stomach. The jejuno-jejunostomy was constructed using a linear cutting stapler and the common enterotomy was closed by hand sewing. This jejuno-jejunostomy results in a potential hernia defect in the small bowel mesentery called J-J defect. The closure of the mesenteric defect of the Roux-en-Y loop is performed with non-absorbable continuous sutures.
Statistical Analysis
Parametric or nonparametric data analysis was conducted depending upon the distribution of the variables. Continuous data are presented as the median. Qualitative variables were compared using the chi-square test, while quantitative variables were analyzed using Student’s t test. Two-sided P values were computed; P < 0.05 was considered statistically significant. All analyses were performed using MedCalc for Windows, version 10.2.0.0 (MedCalc Software, Belgium).
Results
Nice University Hospital “L’Archet 2” Department of Gastrointestinal Surgery and Liver Transplantation started bariatric surgery in 1998. Between 1998 and 2013, 3253 patients were operated for morbid obesity at Nice University Hospital “L’Archet 2” Department of Gastrointestinal Surgery and Liver Transplantation. A total of 2093 patients (64.34%) underwent LRYGB. Of these, 421 patients (20.11%) were operated without the closure of all defects (group A), 1672 patients (79.89%) were operated with the closure of all defects at Petersen defect (PD) and jejunojejunal anastomosis (J-J defect), using non-absorbable suture (group B). Out of the 2093 patients who underwent LRYGB, there were 421 patients—40 male patients (9.5%) and 381 female patients (90.5%) in (group A) and 1672 patients—536 male patients (32%) and 1136 female patients (68%) in (group B) (p = 0.001). The overall median age was 40 years (16–69): 42 years (18–69) in (group A) and 39 years (16–69) in (group B) (p = 0.001). Their preoperative body mass index (BMI) was 41 kg/m2 (21–64): 43 kg/m2 (21–64) in (group A) and 41 kg/m2 (35–55) in (group B) (p = 0.001) (Table 1, Fig. 1).
Internal Hernia
Out of the 2093 patients who underwent LRYGB, 20 patients (0.96%) developed a symptomatic internal hernia (IH) that required primary surgical intervention: 7 patients (1.66%) in group A, all at J-J DEFECT, versus 13 patients (0.78%) in group B, with 6 at J-J DEFECT (0.35%), 5 at PD (0.29%) and 2 at PD, J-J DEFECT (0.12%). This incidence was significantly lower in group B (p = 0.0021). The median age was 39 years (range = 20–64) (p = 0.98), and there were 18 females (90%) and 2 males (10%) (p = 0.75). The rest of the results are in Table 2 and Fig. 1.
Fourteen patients (70%) (5 in group A) were admitted to the emergency room. A CT scan was performed in 8 patients (40%) and showed signs of occlusion in all cases.
The surgery was performed by laparoscopy in 8 patients (40%) and by laparotomy or conversion in 12 patients (60%); there is a high prevalence of laparotomy or conversion according to the difficulty of access in laparoscopy because the adhesions and some of the operations were done by young general surgeons for the patient who was admitted by emergency. In all cases, the internal hernia was reduced, and all defects were closed. In only one patient in group A, the small bowel at J-J DEFECT was resected. There was no mortality and one patient had pneumonia with acute respiratory distress, which was treated medically.
Discussion
LRYGB has largely replaced the open approach due to improved outcomes in postoperative pain, length of stay, and preoperative morbidity. Nonetheless, at the beginning of laparoscopic surgery, the incidence of conversion is closely related to surgeon learning curve. Roux-en-Y reconstruction of the alimentary tract creates defects in the mesentery and potential internal hernia sites. In the retrocolic technique, the alimentary limb was placed posterior to the transverse colon into the lesser sac by way of a defect created in the transverse mesocolon. Therefore, three mesenteric defects are produced: the mesocolic defect where the alimentary limb traverses the mesocolon into the lesser sac, Petersen defect between the mesentery of the alimentary limb and the transverse mesocolon, and J-J defect at the jejunojejunostomy between the mesenteries of the alimentary limb and the biliopancreatic limb and common channel. In the antecolic technique, which is used in our center, two mesenteric defects are created: Petersen defect and J-J defect. Like the open operation, the Roux limb was done and Petersen defect and J-J defect were not routinely closed in early experience with LRYGB. However, unlike the open approach, the laparoscopic approach resulted in a higher incidence of internal hernia ranging from 0 to 11% which is thought to be due to decreased adhesion formation [13]. In this study, there is a relatively high conversion or laparotomy rate (14.7% in group A and 3.7% in group B) in group A during the initial stages of RYGB at our center.
Small bowel obstruction has been reported to occur in 2.5 to 9.7% of patients after RYGB [2, 10, 14,15,16,17,18]. The most frequent reasons for the obstructions are adhesive disease and internal hernias [19, 20].
Here, we compared the impact of the closure of the mesenteric defects on the incidence of symptomatic internal hernia before and after starting to close all defects. We found the incidence of symptomatic internal hernia to be 0.96% after LRYGB, with a statistically significant lower incidence (0.87%) when all of the defects were closed compared to 1.66% without all defects being closed (p = 0.0021).
In this study, there is no internal hernia at PD in group A (100% of IH rate at J-J DEFECT), which was not closed, however there were incidences (0.35%) of internal hernia at PD in group B which were closed (IH rate 46.1% at J-J DEFECT; 38.4% at PD; 15.3% at PD + J-J DEFECT). However, this is not significant (p = 0.6). Several complications related to closure of the mesenteric defects after LRYGB are reported in literature as small bowel obstruction because of internal hernia, kinking of the small bowel, and hematoma. Furthermore, in some studies, it appears that internal hernia after LRYGB occurs because of incomplete closure of the mesenteric defects or with its failure. Consistent with our data, most studies have shown decreased rates of internal hernia with closure of defects and most authors have advocated closure of the mesenteric defects [21,22,23]. How should we close the mesenteric defects in a continuous or interrupted suture? And which type of suture used has been debated in the literature? Many argue that the closure should be performed using continuous non-absorbable suture [24]—with some series showing a decrease in internal hernia rates in consecutive patients when closed with permanent suture [24, 25]. Some studies found no difference in internal hernia rates between continuous versus interrupted sutures [9].
The most common symptom was vague postprandial abdominal pain, 14 patients (70%) were followed by abdominal pain associated with nausea (8 (17.8%)). One of the studies shows abdominal pain as the most common symptom of internal hernia (53.4%) 13. There is some variation in the location of the abdominal pain between the epigastric, periumbilical, and left hypochondriac, and there is also variation in the type: acute and chronic The most common symptom was vague postprandial abdominal pain (14 patients (70%)), followed by abdominal pain associated with nausea (2 (10%)) and abdominal pain associated with nausea and vomiting (3 (15%)). Two patients (10%) presented with acute abdominal pain, and one patient (5%) presented with peritonitis and an acute surgical compression and who the small bowel at J-J DEFECT was resected for him. In our study, 14 patients (70%) were admitted to the emergency room. All on-call surgeons must consider internal hernia in patients who have abdominal pain in the emergency room especially if he has a history of gastric bypass (Table 3).
In this study, Petersen defect and J-J defect are closed using a continuous purse-string non-absorbable braided suture (Ethibond Excel ®-EthiconTM). This study did not show a statistically significant difference in the rate of internal hernias following LYRGB in age, gender, BMI, and excess weight loss; a high clinical index of suspicion for internal herniation should always be maintained in any LRYGB patient who presents with abdominal pain and/or clinical signs and symptoms of small bowel obstruction. A laparoscopic approach can be undertaken to reduce the hernia contents and close all defects. In this study,
This study has some limitations, such as the rate of symptomatic internal hernias, internal hernias that were incidentally repaired during other operations, and those that were not included, and we were unable to follow patients who may have been lost to follow-up and treated elsewhere for an internal hernia. Regardless, there is no reason to suspect a difference between the two groups, which is the group with the higher number of patients with all defects closed, when compared to the group without all defects closed presented to outside hospitals.
Conclusion
In conclusion, internal hernia is a potentially life-threatening complication that can present at any time, ranging from a few weeks to several years after LRYGB. A high index of suspicion must be maintained since symptoms may be nonspecific and imaging may be negative. The antecolic approach is the Roux-limb “right-oriented,” systematic closure of the defects with tight non-absorbable continuous sutures.
References
Marema RT, Perez M, Buffington CK. Comparison of the benefits and complications between laparoscopic and open Roux-en-Y gastric bypass surgeries. Surg Endosc. 2005;19:525–30.
Hwang RF, Swartz DE, Felix EL. Causes of small bowel obstruction after laparoscopic gastric bypass. Surg Endosc. 2004;18:1631–5.
Calle EE, Rodriguez C, Walker-Thurmond K, et al. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–38.
Calle EE, Teras LR, Thun MJ. Obesity and mortality. N Engl J Med. 2005;353:2197–9.
Nguyen NT, Goldman C, Rosenquist CJ, et al. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg. 2001;234:279–89.
Angrisani L, Santonicola A, Iovino P, et al. Worldwide survey 2016. Obes Surg. 2018;28(12):3783–94.
Noria S, Grantcharov T. Biological effects of bariatric surgery on obesity-related comorbidities. Can J Surg. 2013;56(1):47–57.
Higa KD, Ho T, Boone KB. Internal hernias after laparoscopic Roux en-Y gastric bypass: incidence, treatment and prevention. Obes Surg. 2003;13:350–4.
Ahmed AR, Rickards G, Husain S, et al. Trends in internal hernia incidence after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2007;17(12):1563–6.
Iannelli A, Facchiano E, Gugenheim J. Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2006;16(10):1265–71. Review
Iannelli A, Buratti MS, Novellas S, et al. Internal hernia as a complication of laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2007;17(10):1283–6.
Aghajani E, Jacobsen HJ, Nergaard BJ, et al. Internal hernia after gastric bypass: a new and simplified technique for laparoscopic primary closure of the mesenteric defects. J Gastrointest Surg. 2012;16(3):641–5.
McNeal S, Breland M, Stahl R, et al. Internal hernia after laparoscopic Roux-en-Y gastric bypass. Obeid A1. J Gastrointest Surg. 2014;18(2):250–5; discussion 255–6. https://doi.org/10.1007/s11605-013-2377-0.
Capella RF, Iannace VA, Capella JF. Bowel obstruction after open and laparoscopic gastric bypass surgery for morbid obesity. J Am Coll Surg. 2006;203:328–35.
Nelson LG, Gonzalez R, Haines K, et al. Spectrum and treatment of small bowel obstruction after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2006;2:377–83. discussion
Champion JK, Williams M. Small bowel obstruction and internal hernias after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2003;13:596–600.
Eckhauser A, Torquati A, Youssef Y, et al. Internal hernia: postoperative complication of Roux-en-Y gastric bypass surgery. Am Surg. 2006;72:581–4; discussion 584–585
Gumbs AA, Duffy AJ, Chandwani R, et al. Jejunojejunal anastomotic obstruction following laparoscopic Roux-en-Y gastric bypass due to non-absorbable suture: a report of seven cases. Obes Surg. 2006;16:12–5.
Husain S, Ahmed AR, Johnson J, et al. Small-bowel obstruction after laparoscopic Roux-en-Y gastric bypass: etiology, diagnosis, and management. Arch Surg. 2007;142:988–93.
Rogula T, Yenumula PR, Schauer PR. A complication of Roux-en-Y gastric bypass: intestinal obstruction. Surg Endosc. 2007;21:1914–8.
Miyashiro L, Fuller W, Ali M. Favorable internal hernia rate is achieved using retrocolic, retrogastric alimentary limb in laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2010;6:158–64.
Abasbassi M, Pottel H, Deylgat B, et al. Small bowel obstruction after antecolic antegastric laparoscopic Roux-en-Y gastric bypass without division of small bowel mesentery: a single center, 7 year review. Obes Surg. 2011;21:1822–7.
De la Cruz-Munoz CC, Cuesta M, Hartnett S, et al. Closure of mesenteric defect can lead to decrease in internal hernias after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2011;7:176–80.
Coleman MH, Awad ZT, Pomp A, et al. Laparoscopic closure of the Petersen mesenteric defect. Obes Surg. 2006;16:770–2.
Carmody B, DeMaria EJ, Jamal M, et al. Internal hernia after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2005;1:543–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Amor, I.B., Kassir, R., Debs, T. et al. Impact of Mesenteric Defect Closure During Laparoscopic Roux-en-Y Gastric Bypass (LRYGB): a Retrospective Study for a Total of 2093 LRYGB. OBES SURG 29, 3342–3347 (2019). https://doi.org/10.1007/s11695-019-04000-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04000-5