Abstract
Purpose
To evaluate functional and radiological results in patients older than 50 years who underwent an anatomic anterior cruciate ligament (ACL) reconstruction with semitendinosus and gracilis tendons and to compare these results with those of patients younger than 40 years.
Methods
Thirty-six patients over the age of 50 years with a diagnosis of ACL complete lesion and 36 consecutive patients under 40 years were included in this prospective study. Follow-up included clinical evaluation using Lysholm, IKDC, and Tegner scores and a KT-1000 arthrometric evaluation. Bilateral weight-bearing radiographs were obtained before surgery and at final follow-up of five years to evaluate the degree of osteoarthritis. All patients were evaluated at a one year follow-up (T1) (range 13–17 months) and at final follow-up (T2) (range 60–72 months).
Results
No statistically significant difference was found between the two groups at the subjective and objective evaluations. At a KT-1000 arthrometric evaluation, the mean side to side maximum manual difference was 1.6 mm in the over 50 (group I) and 2.7 mm in the under 40 (group II) (p = 0.009). At 30 lb, the mean side to side difference was 1.7 mm in the over 50 group and 2.6 mm in the under 40 group (p = 0.040). No statistically significant increase in the degree of osteoarthritis was found at follow-up in the over 50 group.
Conclusions
The results of this study seems to confirm that ACL reconstruction in patients older than 50 years is a safe procedure with good to excellent subjective, objective, and radiological outcomes that are comparable to those for younger patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) tear is one of the most common sport injuries. In the USA, at least 200,000 ACL reconstructions (ACLRs) are performed each year, most often in young athletic patients [1].
Because the average age and life expectancy are rising, physical activity level in the elderly population is increasing and ACL injuries are becoming more frequent in middle-aged patients. Traditionally, these patients, who did not perform highly demanding activities, have been treated conservatively, since the benefits of the surgical procedure would not be balanced by the risks [2,3,4,5]. Recent studies seem to show that conservative treatment would result in an increased risk of residual instability and further injuries with remarkable modifications of activity levels and lifestyles [6,7,8,9]. Additionally, with subsequent instability episodes, patients may show an accelerated onset of degenerative joint changes [10]. ACLR has been regarded as critical for a good outcome and is commonly performed, particularly in those wishing to resume sports activities. Several studies have shown excellent results of ACLR in patients over 40 years old, including a greater return to sport activity [11]. Surgical treatment showed favorable outcomes in terms of joint stability and patient satisfaction, with comparable results to those observed in younger subjects [12,13,14,15,16]. This growing body of evidence has broadly changed the approach of the surgeons toward the management of the ACL-deficient knees in elderly patients, and various reports have recently focused on ACL reconstruction in patients aged 50 years or older. To the best of the authors’ knowledge, only few previous studies in literature reported similar results among middle-aged patients and young patients after ACLR [14, 17,18,19,20,21].
The aim of this study was to evaluate subjective, objective, and radiological results of ACL reconstruction in patients older than 50 years and to compare their results with subjective and objective outcomes of ACL reconstruction in patients under 40 years.
The primary hypothesis of this study was that age alone does not influence the outcome of ACLR and that subjective and objective outcomes in patients over 50 years are similar to those in younger patients.
Materials and methods
This prospective study evaluated a consecutive series of patients aged 50 years or more examined from January 2008 to December 2012 in the emergency department with a clinical and imaging (x-ray, magnetic resonance imaging (MRI)) diagnosis of ACL complete lesion.
The inclusion criteria applied were as follows: patients with a positive Lachman and Pivot shift test, patients aged more than 50 years, and any recurrent giving way episode as a manifestation of instability.
Exclusion criteria were as follows: severe associated ligamentous injuries, as documented by laxity tests positive other than Lachman and Pivot shift test or by imaging (x-ray, MRI) (e.g., posterior cruciate ligament, medial collateral ligament, lateral collateral ligament, posteromedial corner); cartilage damage (grade 3 or 4 according to Outerbridge classification) [22]; BMI > 29.9 (obesity); previous history of intra- or extra-articular ligament surgery in the involved or controlateral knee; reported rheumatological disorders; associated malalignment; time elapsed from injury to surgery of longer than 2 years; and no other medical comorbidities.
Thirty-six patients over 50 years underwent the inclusion criteria (group I); for each selected patient of group I, a randomized matched control patient aged less than 40 years, operated in the same time lapse and meeting the same inclusion and exclusion criteria (excluding age), was enrolled in this study (group II).
Group I consists of 28 men and eight women with a mean age of 54 years (range 50–62; SD = 3.69), while group II consists of 25 men and 11 women with a mean age of 32.5 years (range 20–40; SD = 2.73).
All patients reported ACL lesion during “high-risk pivoting sport”: in group I, 20 patients reported ACL lesion during football, ten patients during ski, four patients during basketball, and two patients during volleyball; in group II, 23 patients reported ACL lesion during football, eight patients during basketball, four patients during ski, and one patient during volleyball.
Informed consent was obtained from all individual participants included in the study.
All procedures performed in studies involving participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Surgical technique—ACL reconstruction
All the patients were operated with the same surgical technique by the same senior surgeon.
An arthroscopically assisted anatomic single-bundle two-incision technique using doubled semitendinosus and gracilis tendon (DGST) autografts was performed. Point of entry of the femoral tunnel was selected in the centre of the anatomical femoral footprint of ACL which was located midway between resident ridge and over the top position. The tibial tunnel was performed with a standard guide at 65°. The tendons were passed with an outside-in technique and manually tensioned before fixation. Cortical fixation to the bone was achieved in the femur with the Swing-Bridge device (Citieffe, Bologna, Italy) and in the tibia using the Evolgate device (Citieffe, Bologna, Italy). A tight fit of the graft in the bone tunnel was aimed for all patients.
Rehabilitation protocol
The post-operative protocol was the same for all patients of both groups. The knee was placed in a full extension brace for two weeks post-operatively. On the second day, partial weight-bearing was allowed as tolerated with crutches, and daily isometric and isotonic exercises were prescribed. Afterwards, progressive range-of-motion exercises were encouraged as well as isometric and isotonic exercises. At four weeks post-operatively, full weight-bearing without crutches and without a brace was permitted. From the second month post-operatively, a heavier muscle-strengthening program was prescribed, and a gradual return to athletic and sports-specific training was encouraged between four and six months. From the fifth month post-operatively, as soon as the trainer deemed the patient “ready to go,” full return to sports was allowed.
Follow-up
The first subjective data collection for all patients was performed at a mean time of 15 months (T1) (range 13–17 months).
A final evaluation was performed at a minimum of five year follow-up (T2) (mean 64 months, range 60–72 months for group I; mean 78 months, range 60–84 months for group II) by the same observer (F.I.), who was independent and not involved in the initial surgery. Activity level was assessed using Tegner scale [23]. The Lysholm score was used to evaluate the subjective functional status, while the clinical outcome was evaluated using the International Knee Documentation Committee (IKDC) rating system [24, 25]. All patients underwent a standard physical knee examination stability testing which was performed using the IKDC objective classification [26] and the KT-1000 arthrometer (Medmetric, San Diego, USA). Bilateral weight-bearing anteroposterior radiographs in full extension and lateral views were obtained and evaluated using the Fairbank scale [27], the Kellgren-Lawrence scale [28], and the IKDC grading system [24] for group I.
Statistical analysis
The Student t test and the Mann-Whitney test were used to analyze the data for patients in this series.
The evaluation of primary study outcomes (patient satisfaction, laxity scores, arthrometer) has been determined with a level of statistical significance set at 0.05 (95% interval of confidence). Data were analyzed with SPSS software version 22.0 (Armank NY IBM).
Results
All patients were reviewed at the final follow-up.
No complications such as joint infection, venous thromboembolism, or nerve injuries were detected; no further surgery was needed.
Data regarding subjective evaluations are summarized in Table 1
All subjective scores improved significantly from pre-operative evaluation to T1 evaluation (p < 0.05).
No statistically significant differences were found between the two age groups at Lysholm score, IKDC subjective score, and Tegner activity scale at T1 evaluation. Group I had a mean return to sport activity of 102 days while group II had a mean return to sport activity of 93 days (p > 0.05).
No statistically significant differences were found between the two age groups at Lysholm score, IKDC subjective score, and Tegner score at final follow-up (T2) (p > 0.05). At the final follow-up, in group I, 20 patients (56%) returned to the same pre-injury level of activity, 10 (28%) had 1 point less on the Tegner score, and 6 (16%) had 2 points less and in group II, only 22% had a reduced level of sports activity compared to pre-trauma status.
At IKDC objective evaluation at the final follow-up for group I, 25 patients were categorized as A, ten patients were categorized as B, one patient was categorized as C, and no patients were categorized as D.
At IKDC objective evaluation at the final follow-up for group II, 23 patients were categorized as A, 11 patients were categorized as B, 2 patients were categorized as C, and no patients were categorized as D.
At objective evaluation, no statistically significant differences were found between the two groups at the final follow-up (p > 0.05).
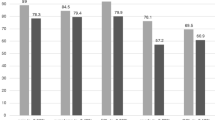
Specific data regarding Kt-1000 evaluation are shown in Fig. 1a–d
The mean side to side (S/S) difference at manual maximum (MM) KT-1000 evaluation was 1.6 mm (SD = 1.80) in patients of group II and 2.7 mm (SD = 2.25) in patients of group II. The mean side to side difference at 30 lb was 1.7 mm (SD = 1.96) in patients of group I and 2.6 mm (SD = 1.86) in patients of group II. There was a statistical significant difference between the two groups at S/SMMKT-1000 arthrometric evaluation (p = 0.009) and at 30 lb (p = 0.04).
Data regarding radiographic evaluation are summarized in Table 2
All patients in group I underwent pre- and post-operative x-rays.
At Fairbank classification, four patients (11%) were in grade I, 19 (53%) were in grade II, 13 (36%) were in grade III, and none were in grade IV.
At Kellgren-Lawrence scale, ten patients (28%) were included in grade I, 19 (53%) in grade II, seven (19%) in grade III, and none in grade IV.
The IKDC radiological evaluation showed two patients (6%) in grade A, 27 patients (75%) in grade B, seven (19%) in grade C, and no patients in grade D.
Comparing the final follow-up radiological evaluation with pre-operative images, no statistically significant for development of degenerative osteoarthritis (DOA) was detected (p > 0.05). Only three patients (8%) in group I increased from grade II to grade III at Kellgren-Lawrence scale; according to the Fairbank classification, three patients (8%) increased from grade II to grade III and two patients (6%) increased from grade I to grade II; and at IKDC radiological evaluation, three patients (8%) in group I increased from grade II to grade III (Table 2).
Discussion
The subjective and objective outcomes of patients of group I showed that in a middle-aged population with ACL tears, selected and motivated patients may have considerable recovery in function and stability after surgical reconstruction, with a good predictable return also to high-risk pivoting sports (football, basketball, ski, and volleyball), 100% returned to sport and 56% returned to pre-injury level. So, the primary hypothesis of this study was confirmed.
Despite the subjective and objective evaluations of group I are similar to those obtained in group II, suggesting that the outcome is not primarily age-related, older patients had a lower Tegner activity sport level compared to pre-injury status; however, all patients (100%) returned to sport activity. The younger patients were more pleased, even if not statistically different, to return at pre-injury level than the older patients, as reported in previous study [14]. Surgical treatment in our sample of patients of group I ensured favourable results in terms of patient satisfaction and return to sports without accelerating the development of DOA. No patients, moreover, have been submitted to re-intervention.
Although the management of older patients with ACL rupture remains controversial, in recent years, surgical treatment was recommended regardless of age. In some studies, a high rate of clinically and functionally satisfactory results has been reported in patients over 50 years undergoing surgery; conservative treatment, however, seems to suggest an increased risk of residual laxity and further injury. Ciccotti et al. [2] observed a satisfactory outcome in 83% of conservatively treated ACL-deficient knees in the population aged between 40 and 60 years, despite a recurrence rate of 37% and remarkable modification of activity levels and lifestyles.
In the literature, only few studies evaluated the outcomes of ACL reconstruction in patients over 50 years. These studies compared clinical and radiological results detected pre-operatively and that obtained after reconstruction. Data in the literature agree, highlighting a statistically significant functional and clinical improvement [20, 28,29,30,31,32,33].
One of most important factors to analyze is that despite all patients of group I return to sport activity, only 56% returned to pre-injury level; this result seems to be lower especially if compared to previous study [32].
Struewer et al. [34] evaluated clinical and radiological outcomes after isolated ACL reconstruction using either autologous bone patellar tendon bone autograft or DGST autograft in patients with a mean age of 49.4 years. At a medium follow-up of two years, all variables improved significantly for both groups compared to pre-operative values, with 76% of patients graded A or B according to the IKDC score and symptomatic DOA developing in approximately 30% of patients without significant inter-group differences.
Dahm et al. [29] reported the outcomes of ACL reconstruction in a group of 34 patients aged over 50 years treated with two different surgical techniques. They reported three failures (8.6%) that required revision surgery. An arthrometric evaluation of the anteroposterior stability was not carried out.
Stein et al. [30] reassessed 19 patients, with a mean age of 54 years, at a medium follow-up of 24 months after ACL reconstruction performed with the patellar tendon or Achilles tendon. Reporting a success rate of 79% on the Lysholm score, they concluded that ACL reconstruction with allograft is a safe and minimally invasive procedure in patients over the age of 50 years.
At a mean follow-up of five years, Wolfson et al. [35] reported a high incidence of reoperation (38%) and residual instability (19%) in 32 patients with a mean age of 58.4 years at the time of operation. They concluded that the degree of patellofemoral arthritis, graded with the Outerbridge classification [22], may be associated with poor outcomes and should be considered in the decision for operative treatment.
Figueroa et al. [31] examined a series of 50 patients over the age of 50 years who underwent ACLR using hamstring autografts or allografts. At a mean follow-up of 53.17 months, they detected a mean post-operative Lysholm score of 93.7 and IKDC score of 90.96. Complications occurred in 6% of patients: 4% ACL re-ruptures and 2% infections. However, they did not perform an arthrometric evaluation of joint stability,
In the study conducted by Blith et al. [28], a side to side difference at manual maximum of 2.7 mm was reported along with a correlation between poor clinical results and advanced DOA.
A comparison of previous studies is showed in Table 3.
Results reported in these articles are similar to those of this study, especially with regard to the subjective evaluation.
Considering that all patients were performed with the same ACL reconstruction technique (DGST autografts), this uniformity of treatment allows a more objective comparison of the results obtained in the two age groups.
The evidence in the literature agreed emphasizing a clinical improvement and functional reconstruction in patients over 50 years compared to a pre-operative status, which is now recognized. Another study analyzed the outcomes of ACL reconstruction comparing a group of 20 patients aged over 50 years with 20 patients under 30 years [17]. In contrast to this study in which no difference was found between the age groups in the arthrometric evaluation, our results showed a greater stability in patients of group I compared to those in group II. Conteduca et al. [16] hypothesized that the increased stiffness in older patients could be due to a variety of physiological and pathological factors, such as different scar tissue formations, initial DOA, different hormonal patterns (especially in women), and loss of elasticity of tissue. In the literature, it has been widely reported that tendons and myotendinous junctions are modified with aging by changes in the underlying structure and mechanical properties becoming progressively stiffer. It can be thought that this could be the reason for the arthrometric differences found in this study. DOA development is a well-known consequence after ACL reconstruction [36]. However, it must also be considered that restoring knee stability could prevent further DOA progression from chronic knee instability following conservative treatment; this is due to a lower risk of subluxations or further injuries. In the present study, the pre- and post-operative comparison between the degree of radiographic DOA in patients older than 50 years using with Fairbank, Kellgren, and IKDC classifications did not show a statistically significant increase in the degree of arthritis at final follow-up. The radiographic results of our study in terms of DOA progression are comparable with those previously reported in literature [29, 37].
The main limitation of the study was the lack of pre-operative and final follow-up radiological evaluations of group II that did not allow to perform a comparison between groups; moreover, regarding the development of DOA, there were not considered concomitant meniscal lesions at surgery time. A long-term follow-up is required to analyze progression of DOA related to an over 50-year-old population and to compare with a younger population. Furthermore, another important limitation is that the data collection was performed at one year (T1) and at final follow-up (T2) without yearly follow-up. Finally, limitations of this study include the small number of patients.
In conclusion, the data of the present study seems to confirm that ACL reconstruction in patients older than 50 years who presented an isolated ACL injury, according to exclusion criteria, is a safe procedure with good to excellent results that are comparable to those for younger patients. Age itself is not a contraindication to ACL surgery; we consider clinical symptoms and functional requests to be more important. Moreover, although patients in our study are not large enough to make definitive conclusions, ACL reconstruction in patients over 50 years seems to not be related to development of early DOA of the knee.
Author contribution
All authors were fully involved in the study and preparation of the manuscript and that the material within has been and will not be submitted for publication elsewhere.
References
Evans S, Shaginaw J, Bartolozzi A (2014) ACL reconstruction—it’s all about timing. Int J Sports PhysTher 9(2):268–273
Ciccotti MG, Lombardo SJ, Nonweiler B, Pink M (1994) Non-operative treatment of ruptures of the anterior cruciate ligament in middle-aged patients. Results after long-term follow-up. J Bone Joint Surg Am 76(9):1315–1321
Buss DD, Min R, Skyhar M, Galinat B, Warren RF, Wickiewicz TL (1995) Nonoperative treatment of acute anterior cruciate ligament injuries in a selected group of patients. Am J Sports Med 23(2):160–165. https://doi.org/10.1177/036354659502300206
Johnson RJ, Beynnon BD, Nichols CE, Renstrom PA (1992) The treatment of injuries of the anterior cruciate ligament. J Bone Joint Surg Am 74(1):140–151
Ventura A, Legnani C, Terzaghi C, Borgo E (2012) Single- and double-bundle anterior cruciate ligament reconstruction in patients aged over 50 years. Arthroscopy 28(11):1702–1709. https://doi.org/10.1016/j.arthro.2012.04.146
Fitzgerald GK, Axe MJ, Snyder-Mackler L (2000) A decisionmaking scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc 8(2):76–82. https://doi.org/10.1007/s001670050190
Strehl A, Eggli S (2007) The value of conservative treatment in ruptures of the anterior cruciate ligament (ACL). J Trauma 62(5):1159–1162. https://doi.org/10.1097/TA.0b013e31805006e7
Conteduca F, Ferretti A, Mariani PP, Puddu G, Perugia L (1991) Chondromalacia and chronic anterior instabilities of the knee. Am J Sports Med 19(2):119–123. https://doi.org/10.1177/036354659101900205
Fu FH, Bennett CH, Lattermann C, Ma CB (1999) Current trends in anterior cruciate ligament reconstruction. Part 1: biology and biomechanics of reconstruction. Am J Sports Med 27(6):821–830. https://doi.org/10.1177/03635465990270062501
Louboutin H, Debarge R, Richou J, Selmi TA, Donell ST, Neyret P, Dubrana F (2009) Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee 16(4):239–244. https://doi.org/10.1016/j.knee.2008.11.004
Legnani C, Terzaghi C, Borgo E, Ventura A (2011) Management of anterior cruciate ligament rupture in patients aged 40 years and older. J Orthop Traumatol 12(4):177–184. https://doi.org/10.1007/s10195-011-0167-6
Barber FA, Elrod BF, McGuire DA, Paulos LE (1996) Is an anterior cruciate ligament reconstruction outcome age dependent? Arthroscopy 12(6):720–725
Bohnsack M, Ruhmann O, Luck K, Wirth CJ (2002) The influence of age on the outcome of anterior cruciate ligament reconstruction. Z Orthop Ihre Grenzgeb 140(2):194–198. https://doi.org/10.1055/s-2002-31540.
Brandsson S, Kartus J, Larsson J, Eriksson BI, Karlsson J (2000) A comparison of results in middle-aged and young patients after anterior cruciate ligament reconstruction. Arthroscopy 16(2):178–182
Viola R, Vianello R (1999) Intra-articular ACL reconstruction in the over-40-year-old patient. Knee Surg Sports Traumatol Arthrosc 7(1):25–28. https://doi.org/10.1007/s001670050116.
Conteduca F, Caperna L, Ferretti A, Iorio R, Civitenga C, Ponzo A (2013) Knee stability after anterior cruciate ligament reconstruction in patients older than forty years: comparison between different age groups. Int Orthop 37(11):2265–2269. https://doi.org/10.1007/s00264-013-2050-y
Osti L, Papalia R, Del Buono A, Leonardi F, Denaro V, Maffulli N (2011) Surgery for ACL deficiency in patients over 50. Knee Surg Sports Traumatol Arthrosc 19(3):412–417. https://doi.org/10.1007/s00167-010-1242-x
Desai N, Björnsson H, Samuelsson K, Karlsson J, Forssblad M (2014) Outcomes after ACL reconstruction with focus on older patients: results from The Swedish National Anterior Cruciate Ligament Register. Knee Surg Sports Traumatol Arthrosc 22(2):379–386. https://doi.org/10.1007/s00167-013-2803-6
Mall NA, Frank RM, Saltzman BM, Cole BJ, Bach BR (2016) Results after anterior cruciate ligament reconstruction in patients older than 40 years, how do they compare with younger patients? A systematic review and comparison with younger populations. Sports Health 8(2):177–181. https://doi.org/10.1177/1941738115622138
Blyth MJ, Gosal HS, Peake WM, Bartlett RJ (2003) Anterior cruciate ligament reconstruction in patients over the age of 50 years: 2-8 year follow-up. Knee Surg Sports Traumatol Arthrosc 11:204–211
Baker CL Jr, Jones JC, Zhang J (2014) Long-term outcomes after anterior cruciate ligament reconstruction in patients 60 years and older. Orthop J Sports Med 2(12):2325967114561737. https://doi.org/10.1177/2325967114561737
Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg Br 43-B:752–757
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res (198):43–49
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10(3):150–154. https://doi.org/10.1177/036354658201000306
Hefti F, Muller W, Jakob RP, Staubli HU (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1(3–4):226–234
Fairbank TJ (1948) Knee joint changes after meniscectomy. J Bone Joint Surg Br 30B(4):664–670
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Blyth MJ, Gosal HS, Peake WM, Bartlett RJ (2003) Anterior cruciate ligament reconstruction in patients over the age of 50 years: 2- to 8-year follow-up. Knee Surg Sports Traumatol Arthrosc 11(4):204–211. https://doi.org/10.1007/s00167-003-0368-5
Dahm DL, Wulf CA, Dajani KA, Dobbs RE, Levy BA, Stuart MA (2008) Reconstruction of the anterior cruciate ligament in patients over 50 years. J Bone Joint Surg Br. 90(11):1446–1450. https://doi.org/10.1302/0301-620X.90B11.21210
Stein DA, Brown H, Bartolozzi AR (2006) Age and ACL reconstruction revisited. Orthopedics 29(6):533–536
Noyes FR, Barber-Westin SD (1997) Arthroscopic-assisted allograft anterior cruciate ligament reconstruction in patients with symptomatic arthrosis. Arthroscopy 13(1):24–32
Figueroa D, Figueroa F, Calvo R, Vaisman A, Espinoza G, Gili F (2014) Anterior cruciate ligament reconstruction in patients over 50 years of age. Knee 21(6):1166–1168. https://doi.org/10.1016/j.knee.2014.08.003
Trojani C, Sane JC, Coste JS, Boileau P (2009) Four-strand hamstring tendon autograft for ACL reconstruction in patients aged 50 years or older. Orthop Traumatol Surg Res 95(1):22–27. https://doi.org/10.1016/j.otsr.2008.05
Struewer J, Ziring E, Oberkircher L, Schüttler KF, Efe T (2013) Isolated anterior cruciate ligament reconstruction in patients aged fifty years: comparison of hamstring graft versus bone-patellar tendon-bone graft. Int Orthop 37(5):809–817. https://doi.org/10.1007/s00264-013-1807-7
Wolfson TS, Epstein DM, Day MS, Joshi BB, McGee A, Strauss EJ, Jazrawi LM (2013) Outcomes of anterior cruciate ligament reconstruction in patients older than 50 years of age. Bull Hosp Jt Dis 2014 72(4):277–283
Cinque ME, Dornan GJ, Chahla J, Moatshe G, LaPrade RF (2017) High rates of osteoarthritis develop after anterior cruciate ligament surgery: an analysis of 4108 patients. Am J Sports Med:363546517730072. https://doi.org/10.1177/0363546517730072
Toanen C, Demey G, Ntagiopoulos PG, Ferrua P, Dejour D (2017) Is there any benefit in anterior cruciate ligament reconstruction in patients older than 60 years? Am J Sports Med 45(4):832–837. https://doi.org/10.1177/0363546516678723
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent was obtained from all individual participants included in the study.
All procedures performed in studies involving participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Iorio, R., Iannotti, F., Ponzo, A. et al. Anterior cruciate ligament reconstruction in patients older than fifty years: a comparison with a younger age group. International Orthopaedics (SICOT) 42, 1043–1049 (2018). https://doi.org/10.1007/s00264-018-3860-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3860-8