Abstract
In the absence of a fragility fracture, osteoporosis is usually diagnosed from bone mineral density (BMD) measured by dual-energy X-ray absorptiometry (DXA). Osteoporosis is an increasingly prevalent disease, as is diabetes [in particular type 2 diabetes (T2D)], in part due to aging populations worldwide. It has been suggested that an increased risk of fracture may be another complication ensuing from longstanding diabetes. The purpose of this review is to concentrate on skeletal parameters and techniques readily available from DXA scanning, and their utility in routine clinical practice for predicting fracture risk. In addition to BMD, other applications and measures from DXA include trabecular bone score (TBS), skeletal geometry and DXA-based finite-element analysis, vertebral fracture assessment, and body composition. In type 1 diabetes (T1D), BMD and FRAXR (when secondary osteoporosis is included without BMD) only partially account for the excess risk of fracture in T1D. Consistent data exist to show that BMD and FRAXR can be used to stratify fracture risk in T2D, but do not account for the increased risk of fracture. However, several adjustments to the FRAX score can be made as proxies for T2D to inform the use of FRAX by primary care practitioners. Examples include using the rheumatoid arthritis input (as a proxy for T2D), lumbar spine TBS (to adjust FRAX probability) or an altered hip T-score (lowered by 0.5 units). These adjustments can improve fracture risk prediction in T2D and help to avoid systematically underestimating the risk of osteoporosis-related fractures in those with diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the absence of a fragility fracture, osteoporosis is usually diagnosed from bone mineral density (BMD) measured by dual-energy X-ray absorptiometry (DXA). Osteoporosis is defined as a BMD that is 2.5 or more standard deviations (SD) below the young adult mean population (T-score ≤ −2.5), with the proposed reference standard relying on BMD measured at the femoral neck with DXA and a uniform reference database (National Health and Nutrition Examination Survey [NHANES] III for white women aged 20–29 years) [1]. BMD measurement from DXA provides a robust estimate of fracture risk in the general population, increasing 1.4–2.6-fold for every SD decrease in BMD [2, 3].
Osteoporosis is an increasingly prevalent disease, in part due to aging populations worldwide [4]. Diabetes is also increasing globally, particularly type 2 diabetes (T2D) which predominates in older individuals and encompasses ninety percent of all diabetes cases, in large part as a consequence of the obesity epidemic. Between 1988–1994 and 2011–2012 there was a linear increase in the estimated prevalence of diabetes among US adults that reached 12–14 %, concordant with the observed increasing trend in obesity [5].
In addition to well-established micro- and macrovascular complications associated with long-term duration and poor control of diabetes, type 1 diabetes (TID), and more recently T2D, has been associated with increased fracture risk [6]. This is despite the fact that BMD is actually increased in T2D [7, 8], leading to the hypothesis that there are diabetes-associated alterations in skeletal properties which include an accumulation of advanced glycosylation end products (AGEs) in the organic bone matrix. AGE crosslinks lead to the formation of bone that is biochemically more brittle and may decrease bone formation on the whole by interfering with normal osteoblast development and function [9, 10]. The cortical component of bone appears to be compromised in T2D [11], while data are mixed regarding effects on trabecular bone mass and structure [12].
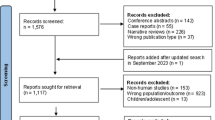
This review concentrates on skeletal parameters and techniques available from DXA. In addition to BMD, other applications and measures from DXA include trabecular bone score (TBS), bone geometry, vertebral fracture assessment (VFA), and body composition. A systemic search of PubMed to August 15, 2016) was performed using the keywords “osteoporosis”, “fracture risk”, “diabetes”, and “densitometry”. Inclusion criteria were epidemiological studies (cross-sectional, cohort or case control) that provided data on fracture risk in patients with T1D or T2D compared to a control group without diabetes. Information was used to address the following clinical questions: (1) Does the skeletal parameter (or technique) differ between those with and without diabetes? (2) Is the skeletal parameter (or technique) associated with fracture risk in those with diabetes? (3) Does the skeletal parameter (or technique) account for excess fracture risk in those with diabetes?
Bone Mineral Density
General Background
DXA is the most commonly used technique to diagnose osteoporosis, predict fracture risk, and monitor response to therapy. Denser tissue (i.e., bone) contains more electrons and therefore allows fewer X-rays to reach the detector. Differential attenuation of X-rays as they pass through body tissue can be analyzed to determine the amounts of bone and soft tissue, and allows for quantification of BMD. Radiation exposure to the patient is extremely small, and on the order of one day’s background.
Unfortunately, there are technical issues inherent in DXA that may affect accuracy. BMD measurements assume that bone is a uniform solid, and do not consider size, shape, and the distribution of bone material [13]. Furthermore, DXA-measured bone density does not allow for separation of the cortical or trabecular bone compartments. Substantial BMD measurement error can arise from nonuniform extraosseous fat, of potential relevance in patients with increased BMI [14–16]. Additionally, discordant change after bariatric surgery can affect longitudinal studies [17]. As well, aortic calcifications, vertebral compression fractures, osteophytes, and other degenerative changes may artificially increase BMD results [18, 19].
Greater body weight has historically been assumed to protect against skeletal mechanical incompetence largely based on DXA data that consistently show higher BMD in overweight and obese adults. A meta-analysis of nearly 400 000 individuals found a significant positive correlation between BMI and BMD (r = 0.33; 95 % CI 0.32–0.33) [20]. The same study found that the association between BMI and fracture risk was complex and differed across skeletal sites. Overall, higher BMI was associated with a reduced risk of all osteoporotic fractures. However, after adjustment for BMD, greater BMI was only protective for hip fractures.
Type 1 Diabetes
Studies have suggested that T1D is associated with alterations in bone turnover, (namely metabolic effects of poor metabolic control leading to increased bone resorption and bone loss in young adults, coupled with decreased bone formation retarding bone accumulation during growth), ultimately leading to the development of osteopenia [21, 22]. Indeed, reduced bone density in T1D as compared to normal controls has been demonstrated in a meta-analysis performed by Vestergaard [7]. A significant reduction in BMD z score (comparison of the subject’s BMD to the age-/sex-matched controls) was seen at the hip (mean ± SEM −0.37 ± 0.16) and at the lumbar spine (−0.22 ± 0.01). Meta-regression did not identify a consistent relationship between BMD and age, BMI, diabetes duration, or HbA1c. However, other studies have found the following factors may be associated with lower BMD in T1D: male gender, longer duration of disease, younger age at diagnosis, lower endogenous insulin or c-peptide levels, low BMI, and possibly the presence of chronic diabetes comorbidities or associated autoimmunity [23–28].
The decreased BMD reported in subjects with T1D only partially explains the observed higher fracture risk in these patients. T1D has also been found to be associated with a relative increased risk for hip fracture on the order of a 6.4–6.9-fold compared to individuals without diabetes [6, 7], which vastly exceeds the relative risk of 1.42 expected from the magnitude of the BMD reduction. Overall, the increase in fracture risk was higher, while BMD was lower in patients with T1D as compared to controls. Decreased BMD only partially accounts for the increased fracture risk in T1D, suggesting a multi-factorial etiology.
Longitudinal studies of BMD in T1D are sparse. Mastrandrea et al. reported on 63 women with T1D compared to 85 age-matched community control subjects at baseline [29] and after 2 years of follow-up [28]. After adjustment for age and BMI, baseline BMD values were significantly lower at the femoral neck and at the lateral spine in women greater than 20 years of age, as compared with the baseline BMD values of the controls. However, there was no significant difference in women younger than 20 years nor at the anteroposterior spine, forearm, or whole body. BMD at year 2 continued to be lower at the total hip, femoral neck, and whole body in women older than 20 years with T1D as compared to the control subjects, after adjusting for age, BMI, and oral contraceptive use. Lower BMD was also observed in T1D cases <20 years of age compared to control subjects, but these differences were not statistically significant. Percent change in BMD was not significantly different for any site or age, but the study may have been underpowered to detect such changes. The authors concluded that persistence of low BMD, as well as the failure to accrue bone density after age 20 years, might contribute to the increased incidence of osteoporotic hip fractures in postmenopausal women with T1D.
Strotmeyer et al. [30] studied 67 premenopausal women aged 35–55 years with T1D and 237 women without diabetes. Women with T1D were more likely to report a fracture after age 20 than non-diabetic women (33.3 vs. 22.6 %; age-adjusted odds ratio 1.89 [95 % CI 1.02–3.49]). T1D was associated with lower total hip BMD (0.890 vs. 0.961 g/cm2; p < 0.001), femoral neck BMD (0.797 vs. 0.847 g/cm2; p = 0.001), and whole body BMD (1.132 vs. 1.165 g/cm2; p < 0.01). Spine BMD was not significantly different between groups. Although self-reported fracture prevalence was higher in women with T1D than controls, the ability of BMD to stratify fracture risk in T1D was not reported.
Sex-specific decrease in BMD has also been reported in T1D. A 5-year prospective study revealed a longitudinal decrease in femoral neck BMD in 17 males with T1D (but not other skeletal sites), whereas no BMD change was detected among females with T1D (though the study was underpowered and did not formally assess for a sex interaction) [31]. However, another cross-sectional study looking at 25 females and 35 males with T1D identified a significant gender interaction (p = 0.0285) with reduced femoral shaft BMD in females only [25].
Leidig-Bruckner et al. [32] studied 398 consecutive diabetes patients from a single outpatient clinic, of whom 139 (71 men and 68 women) had T1D. Lumbar spine BMD and femoral neck BMD were significantly lower in those with fractures compared to those without fractures (p < 0.02 and p < 0.03, respectively), while age, BMI, diabetes duration, and HbA1c levels were similar. Most T1D patients with fractures had T-scores greater than −2.5 SD.
Overall, the increase in fracture risk in T1D, despite variations in BMD, gives credence to the hypothesis that factors independent of, or not accounted by BMD, contribute to the increased relative risk for fractures. BMD measurements are slightly lower in individuals with T1D, but this only partially account for the excess fracture risk. To date, no studies have been adequately powered to examine fracture prediction from BMD in T1D. Indeed, even data on the ability of BMD to stratify prior fracture status are sparse.
Type 2 Diabetes
Type 2 diabetes undoubtedly influences bone metabolism, but the effect of T2D on BMD is inconsistent across individual studies. There is robust evidence from meta-analyses for increased fracture risk in T2D [6, 7] despite normal or even high BMD at both the hip and spine [7, 8]. In the meta-analysis performed by Vestergaard [7], and in contrast with T1D, T2D was associated with an increased z score at the hip (mean ± SEM +0.27 ± 0.01) and at the lumbar spine (+0.41 ± 0.01). A meta-regression confirmed that BMI was strongly associated with hip BMD (regression coefficient ± SEM 0.40 ± 0.08) and lumbar spine BMD (0.34 ± 0.10) in T2D (but not age, duration of diabetes, or HbA1c) [7]. Of interest, the higher BMD in T2D persists after adjusting for BMI [33]. An updated meta-analysis by Ma et al. [8] included 15 observational studies containing over 3000 T2D subjects and 19,000 controls. BMD in T2D was significantly higher, with pooled mean differences of 0.04 (95 % CI 0.02–0.05) at the femoral neck, 0.06 (95 % CI 0.04–0.08) at the hip, and 0.06 (95 % CI 0.04–0.07) at the spine.
Vestergaard [7] reported an increased age-adjusted relative risk for hip fracture of 1.38 (95 % CI 1.25–1.53) in T2D compared to healthy controls. There was a borderline increase in wrist fracture risk, but not in non-vertebral and spine fractures. The meta-analysis from Janghorbani et al. [6] found a slightly stronger effect of T2D on hip fracture risk (summary RR = 1.7, 95 % CI 1.3–2.2), but most effect estimates for fractures at other sites were not statistically significant. Most subsequent studies have demonstrated increased age-adjusted rates of hip fracture. The expected relative risk of hip fracture in T2D based upon the magnitude of the BMD elevation is 0.7 (i.e., 30 % lower risk). This paradox highlights the difficulty in relying on BMD to assess fracture risk in T2D, and the importance of BMD-independent determinants of skeletal strength and/or fracture risk.
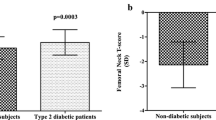
Combined results from three large prospective observational studies found that the fracture risk for any given femoral neck BMD T-score and age was increased in type 2 diabetic patients compared to those without diabetes [34]. For hip fracture, the mean difference in femoral neck T-scores comparing those with and without DM at the same fracture risk was approximately 0.5 SD (0.59, 95 % CI 0.31–0.87 in women, 0.38, 95 % CI 0.09–0.66 in men). Despite systematically higher fracture risk attributable to T2D, age-adjusted hazard ratios (HRs) per SD decrease in BMD predicted hip fracture and non-spine fracture equally well in those with and without T2D. For example, in women with T2D the HR was 1.88 (95 % confidence interval [CI], 1.43–2.48) for hip fracture and 1.52 (95 % CI 1.31–1.75) for non-spine fracture, versus 2.23 (95 % CI 2.06–2.41) for hip fracture and 1.53 (95 % CI 1.47–1.60) for non-spine fracture in women without T2D. Napoli et al. [35] demonstrated an increased risk of non-vertebral fracture for a given BMD in a study of 5994 men ≥65 years of age, 881 with diabetes. In this study, the multivariate-adjusted risk of non-vertebral fracture was found to be 30 % higher in men with diabetes for a given BMD (HR 1.30, 95 % CI 1.09–1.54). The effect of diabetes was no longer significant when additionally adjusted for falls in the prior year. Diabetic men receiving insulin treatment had nearly double the risk of fractures compared to those without diabetes, after adjustment for covariates, including age, race, clinic site, and total hip BMD (HR 2.46, 95 % CI 1.69–3.59).
de Liefde et al. [33] studied 6,655 men and women over the age of 55 from the Rotterdam Study, comparing subjects with T2D to those without diabetes. Subjects with T2D had higher BMD (even after adjustment for BMI and other covariates). They also had an increased non-vertebral fracture risk (HR 1.33, 95 % CI 1.00–1.77), although in a subset analysis this appeared to be restricted to those with treated diabetes. The ability of BMD to predict fracture risk in T2D was not reported.
Bonds et al. studied a racially diverse group of 93 676 women with clinically diagnosed T2D (n = 5285) at baseline in the Women’s Health Initiative Observational Cohort (a prospective study of postmenopausal women) and compared them with women without diagnosed diabetes (n = 88,120) [36], including a subsample of women with available baseline BMD scores. Women with T2D had higher hip and spine BMD as compared to the controls, but the increased risk of fracture remained after adjustment for BMD (HR 1.82, 95 % CI 0.90–3.64).
Leslie et al. [37] conducted an observational registry-based study of 62,413 older individuals (6.455 [10 %] with diabetes, mean age 66.5 years) with 4,218 sustaining one or more incident major osteoporotic fractures (hip, clinical spine, humerus, or forearm) and 1108 sustaining incident hip fractures during follow-up. Femoral neck BMD was significantly greater in those with diabetes (p < 0.001). For major osteoporotic fracture prediction, the adjusted HR per SD decrease in femoral neck T-score in those individuals without diabetes (1.68, 95 % CI 1.61–1.75) was similar to those with diabetes (1.60, 95 % CI 1.44–1.79; p-for-interaction 0.456). Each SD decrease in femoral neck T-score strongly predicted hip fracture in those without diabetes (HR 2.17, 95 % CI 1.98–2.38) and in those with diabetes (2.15, 95 % CI 1.75–2.6; p-for-interaction 0.956).
In summary, lower BMD is strongly predictive of fractures in those with T2D, just as it is in the general population, and remains an important and useful component of fracture risk assessment. However, the increased fracture risk associated with T2D is not fully captured by BMD that is paradoxically higher, even after adjustment for the BMI. Figure 1 illustrates a conceptual basis for diabetes-induced osteoporosis (DIO). Analogous to glucocorticoid-induced osteoporosis (GIO), there is a large component of fracture burden that is attributable to age-related osteoporosis. T2D upshifts the BMD–fracture relationship such that there is an increase in fracture risk above that predicted from BMD alone, resulting in the additional fracture burden attributable to T2D.
Conceptual framework for diabetes and fractures. The light gray region below the solid line indicates the fracture burden attributable to osteoporosis; the dark gray region between the dotted and solid lines indicates the additional fracture burden attributable to diabetes. Data are from Leslie et al. [68]
Skeletal Geometry
General Background
Most fractures occur in patients without a BMD T-score diagnosis in the osteoporotic range, and this indicates the presence of factors beyond BMD that compromise bone strength and predisposes individuals to fracture. Several studies have shown that variation in hip geometry affects fracture risk, in accordance with engineering principles [38]. Routinely available measurements of hip geometry through hip structural analysis (HSA) and related techniques are highlighted below and include hip axis length (HAL), neck-shaft angle, cross-sectional area (CSA), and cross-sectional moment of inertia (CSMI). Investigational, strength-based parameters derived from DXA-based finite-element analysis (FEA)/finite-element analysis of X-ray (FEXI) show promise but are not yet available as clinical tools [39–42].
A systematic review and evidence-based Position Development Conference based upon the RAND/UCLA Appropriateness Method concluded that only HAL had potential for fracture risk assessment in clinical practice [38]. Two large retrospective registry-based studies from the Manitoba Bone Density Program examined skeletal geometry in the general population. The first study evaluated 50,420 women aged 40 years and older with hip geometry measures from DXA and FRAX scores, among whom 1020 hospitalized hip fractures were diagnosed during 319,137 person-years of follow-up [43]. Among the hip geometry measures, longer HAL showed a consistent association with greater hip fracture risk, and this was unaffected by adjustment for age and BMD or FRAX score (HR per SD 1.30, 95 %CI 1.22–1.38). Many other hip geometry measurements were also associated with hip fracture risk when adjusted for age alone, but no longer provided significant information after BMD adjustment. The HAL findings were further evaluated in an expanded cohort that included 4738 men in a subsequent study [44]. When adjusted for FRAX hip fracture probability, longer HAL increased hip fracture risk in men (p = 0.031) and in women (p < 0.001); this association was unaffected by sex (p interaction = 0.409). The authors proposed a simple adjustment to FRAX hip fracture probability: relative increase in hip fracture probability 4.7 % for every mm that HAL is above the sex-specific average, relative decrease in hip fracture probability 3.8 % for every mm that HAL is below the sex-specific average. However, this approach has not yet been replicated in other cohorts or in patients with diabetes. Although there is no reason to suspect that HAL differs in patients with diabetes, differences in fall mechanics and/or trochanteric fat padding may alter the usefulness of HAL in T1D or T2D.
A sophisticated engineering approach to skeletal strength assessment is DXA-based FEA/FEXI, which so far has also not yet been evaluated in diabetes [39–42, 45–47]. FEA solves mathematical models, based upon bone shape and density distribution embedded in the DXA images, to predict how the structure will react to stress when loaded. One DXA-derived FEA model has been shown to enhance the prediction of hip fracture compared with BMD alone: after adjusting for hip BMD, the odds ratio for femoral strength (OR 1.7, 95 % CI 1.2–2.4) and low-to-strength ratio (OR 1.4, 95 % CI 1.1–1.7) remained significantly greater than 1 [40].
Type 1 Diabetes
Unfortunately, there is a paucity of clinical studies specifically examining the geometric properties of bone strength in T1D. Maser et al. [26] investigated the association of age at onset of T1D with BMD, estimates of bone strength (cross-sectional area [CSA]) and bending strength (section modulus [SM]) in 60 adults (35 men and 25 women) with T1D. In covariate-adjusted models with CSA, SM or outer diameter as the dependent variable, age at diabetes onset (p < 0.01) and gender (p < 0.0001) showed significant associations without gender interaction. These findings suggested that earlier onset of T1D is associated with lower measures of bone strength.
A small study by Miazgowski et al. [24] compared the BMD, HAL, and CSA and cross-sectional moment of inertia (CSMI) in 36 men with T1D with age-, weight- and height-matched healthy controls. While men with T1D had lower spine BMD (p < 0.05), hip BMD and the hip geometry were not significantly different. BMD and hip strength parameters did not correlate with HbA1c.
To date, there have been no evaluations of hip geometry in T1D patients with fracture (prevalent or incident) as the outcome. Although skeletal geometry appears to be decreased in patients with T1D, there is insufficient information to determine whether bone geometry contributes to the excess fracture risk in T1D.
Type 2 Diabetes
As with T1D, there are few studies evaluating hip structure in T2D, and none with fracture as an outcome. Garg et al. [48] studied 5,924 postmenopausal women enrolled in the Women’s Health Initiative Observational Study (WHI-OS), of whom 427 had diagnosed T2D. Although BMD and many of the HSA-derived measures were higher in the women with T2D, after adjusting for multiple confounders (including total lean body weight) the differences disappeared. CSA and BMD normalized to lean body mass were lower in T2D women on insulin compared with controls, or non-insulin-treated women with T2D. The latter was suggested to represent altered adaptation of bone modeling and explain the higher fracture risk in patients with T2D, but no fracture data were provided to support this. In a cross-sectional study of 134 men and women with non-insulin requiring T2D, Moseley et al. [49] found that lean mass (but not fat mass) was positively correlated with BMD and HSA-derived measurements (CSA, SM, and buckling ratio).
Hamilton et al. [50] analyzed 3658 women (157 with T2D) with hip geometry and HSA data enrolled in the Canadian Multicentre Osteoporosis Study (CaMos). Based upon engineering beam theory, stresses were determined to be 4.5 % higher in women with T2D than in women without diabetes (11.03 ± 0.18 MPa versus 10.56 ± 0.04 MPa, p = 0.0093). Higher stresses indicate weaker geometry and the presence of an impaired skeletal load response.
In a cross-sectional analysis from the Study of Women’s Health Across the Nation (SWAN), Ishii et al. [51] studied 1887 women (including 81 with T2D) and found that despite the fact that women with T2D had greater BMD than controls at the femoral neck, they had lower composite strength indices relative to load (−0.20 SD, 95 % CI −0.38 to −0.03 SD for compression, −0.19 SD, 95 % CI −0.38 to −0.003 SD for bending, and −0.19 SD, 95 % CI −0.37 to −0.02 SD for impact). Homeostasis model-assessed insulin resistance (HOMA-IR) showed an inverse relationship with all three strength indices (adjusted for the same covariates).
Akeroyd et al. [45] studied 1137 men (12.5 % with T2D) and found no significant association between T2D and HSA-based geometry measurements of strength. However, other studies have shown the opposite, with a tendency toward increased bone strength in T2D but similar load-to-strength ratios due to greater weight in those with T2D [52].
As with T1D, the clinical utility of skeletal strength measurements derived from bone geometry for fracture prediction in T2D is unknown. We cannot comment on whether skeletal geometry is associated with increased fracture risk nor whether it accounts for excess fracture risk in T2D. Longitudinal cohort studies are needed to see whether these indices can help to understand and better predict risk for hip fracture in T2D.
Trabecular Bone Score (TBS)
General Background
The trabecular bone score (TBS) is a texture parameter that evaluates pixel gray-level variations in the spine DXA image and can be used to enhance fracture risk predictions independent of BMD [53]. TBS provides an indirect index of trabecular architecture [54]. A dense trabecular network that is associated with greater mechanical bone strength will produce many gray-level texture variations of small amplitude, resulting in a steep variogram slope. A low TBS value indicates fewer gray-level texture variations of larger amplitude and therefore a lower slope, suggesting worse bone structure. The original TBS software was optimized for women. Over time, there have been changes to the algorithm that have helped to improve performance in men and partially compensate for the effects of increased abdominal soft tissue that degrade image quality (reviewed in Leslie et al.) [55]. Due to persisting dependencies on abdominal soft tissue and BMI, the manufacturers discourage use of TBS in individuals with BMI < 15 or > 37 kg/m2.
In a large registry-based cohort of 29,407 women, Hans et al. [56] demonstrated that there was a significantly lower lumbar spine TBS as well as BMD in women with incident major osteoporotic, spine, and hip fractures (all p < 0.0001). Spine TBS and spine BMD predicted fractures equally well and the combination was superior to either measurement alone (p < 0.001). From the same database, the impact of TBS on the probability of fracture above that provided by the clinical risk factors utilized in FRAX was determined in 33,352 women aged 40–99 years [57]. When fully adjusted for FRAX risk variables, TBS remained a significant predictor of MOF excluding hip fracture (HR/SD 1. 18, 95 % CI 1.12–1.24), hip fracture (HR/SD 1.23, 95 % CI 1.09–1.38), and death (HR/SD 1.20, 95 % CI 1.14–1.26). Using these data, models were derived to adjust MOF and hip fracture probability accounting for TBS (that included an age interaction) with death considered as a competing event.
A recent meta-analysis by McCloskey et al. [59] confirmed that TBS predicted fracture risk independently of FRAX probability and examined their combined performance by adjusting the FRAX probability for TBS based upon the previous Manitoba cohort [57]. Data were collected on 17,809 subjects (59 % women, 41 % men) from 14 prospective population-based cohorts. Outcomes during follow-up (mean 6.7 years) comprised major osteoporotic fractures. Overall, the gradient of risk (GR; hazard ratio per SD decrease) of TBS for major osteoporotic fracture was 1.44 (95 % CI 1.35–1.53) when adjusted for age and time since baseline. When additionally adjusted for FRAX 10-year probability of major osteoporotic fracture, TBS remained a significant, independent predictor for fracture (GR 1.32, 95 % CI 1.24–1.41), with similar results in men and women. The authors concluded that TBS is a significant predictor of fracture risk independent of FRAX and supported the use of TBS as a potential adjustment for FRAX probability. Based upon these studies, the output of FRAX can now be adjusted for TBS through the online FRAX calculator (https://www.shef.ac.uk/FRAX/).
Type 1 Diabetes
Data on lumbar spine TBS in T1D are sparse. In a cross-sectional study by Neumann et al. [59], there was a borderline reduction in mean TBS between diabetic patients (60 females and 59 males, mean age 43.4 years) and non-diabetic, gender-, age- and BMI-matched controls (1.357 ± 0.129 vs. 1.389 ± 0.085, respectively, p = 0.075). The adjusted odds ratio (aOR) for lumbar spine TBS in the lowest tertile (vs. highest tertile reference) was significantly above 1 in the comparison between T1D patients and controls (aOR 2.59, 95 % CI 1.08–6.21, p = 0.033). In contrast, the aORs for BMD at the lumbar spine, femoral neck, or total hip did not differ between the two groups. T1D patients with prevalent fractures had significantly decreased TBS as compared to controls (1.309 ± 0.125 vs. 1.370 ± 0.127, p = 0.04). TBS and HbA1c were independently associated with prevalent fractures in T1D. A TBS cutoff of <1.42 captured prevalent fractures with 91.7 % sensitivity, 43.2 % specificity, and negative predictive value of 95.3 %. The high TBS cutoff in comparison with other studies probably reflects the relatively young age of the study subjects. The ROC curve showed that only TBS and total hip BMD significantly differentiated between diabetic patients with and without fractures (area under the curve [AUC] 0.63, 95 % CI 0.51–0.74, p = 0.048 and AUC 0.64, 95 % CI 0.51–0.78, p = 0.032, respectively). When lumbar spine TBS and total hip BMD values were combined, the AUC increased to 0.68 (95 % CI 0.55–0.81, p = 0.007), suggesting that TBS had additive value to BMD.
No studies to date have assessed the utility of lumbar spine TBS for fracture prediction in T1D. TBS does appear to differ in patients with T1D as compared to healthy controls and is independently associated with prevalent fractures. However, we cannot state whether TBS accounts for excess fracture risk in those with diabetes.
Type 2 Diabetes
In general, TBS has been found to be lower in patients with T2D as compared to controls without diabetes, even after adjustment for BMI [57, 60]. Leslie et al. [57] performed a retrospective cohort study of 29,407 women 50 years and older (2,356 with diabetes presumed to be predominantly T2D) using BMD results from a large clinical registry for the province of Manitoba, Canada. Diabetes was associated with higher BMD at all sites, but in contrast, lower lumbar spine TBS in both unadjusted and covariate-adjusted models (all p < 0.001). Lumbar spine TBS was found to be an equally strong BMD-independent predictor of fracture both in women with diabetes (adjusted hazard ratio 1.27, 95 % CI 1.10–1.46) and without diabetes (hazard ratio 1.31, 95 % CI 1.24–1.38). Overall fracture risk stratification from lumbar spine TBS (AUROC 0.63, 95 % CI 0.61 to 0.64) was similar to lumbar spine BMD (AUROC 0.64, 95 % CI 0.63 to 0.65), and neither showed a significant difference between women with and without diabetes. The effect of diabetes on fracture risk was reduced when lumbar spine TBS was added to prediction models with or without BMD measurements. This suggests that lumbar spine TBS captures some of the fracture risk associated with diabetes and that combining lumbar spine TBS with BMD may incrementally improve fracture prediction in older women with diabetes.
Other studies have confirmed that TBS is lower in T2D. Kim et al. [61] studied 1529 women (370 with T2D) and 1229 men (325 with T2D) age >50 years old. This cross-sectional study reported that TBS was significantly lower in the men with than those without diabetes (1.287 ± 0.005 vs. 1.316 ± 0.003, respectively, p < 0.001), which persisted after adjustment for age and BMI. Lower TBS seen in women with diabetes in unadjusted analysis did not persist after covariate adjustment (though it did in women younger than 65 years as in other studies). Conversely, BMD was increased in both women and men with diabetes in both adjusted and unadjusted models. In both groups, TBS was inversely associated with HbA1c, fasting plasma glucose, fasting insulin, and homeostatic model assessment: insulin resistance (HOMA-IR), even after adjusting for age and BMI.
Finally, Dhaliwal et al. [60] also performed a small retrospective cross-sectional study investigating TBS in 57 women with T2D and 43 controls without diabetes, ages 30–90 years old. Mean TBS was lower in T2D (1.228 ± 0.140 vs. 1.298 ± 0.132, p = 0.013), while mean BMD was higher (p = 0.001). Within the T2D group, TBS was higher in subjects with good glycemic control (HbA1c ≤ 7.5 %) compared to those with poor glycemic control (1.254 ± 0. 148 vs. 1.166 ± 0.094, p = 0.01).
In summary, several studies have shown that that spine and hip BMD is higher, but lumbar spine TBS is lower, in T2D as compared to controls without diabetes, in both women and men. In addition, TBS predicts MOF in postmenopausal women with and without diabetes. TBS scores in T2D are lower and are associated with fracture risk. Therefore, TBS appears to at least partially account for excess fracture risk in T2D though further work is needed to better understand the effects of abdominal obesity and BMI on TBS measurements in this population.
Vertebral Fracture Assessment (VFA)
General Background
Vertebral fracture assessment (VFA) by DXA is a rapid, low-radiation method for visualizing the thoracic and lumbar spine to detect vertebral fractures [62]. It has been established that the presence of morphometric vertebral fractures increases the risk of subsequent spinal or hip fractures, independently of BMD [63, 64]. Therefore, the value of VFA is to detect asymptomatic vertebral fractures in order to intervene and prevent subsequent clinical fractures (both vertebral and non-vertebral). There is clinical utility in selectively performing VFA at the time of DXA scanning in those with a sufficiently high pretest likelihood for having an asymptomatic vertebral fracture as the examination can be obtained at the same time as BMD measurement, at lower cost and radiation exposure than with conventional radiographs of the spine [65, 66]. VFA has good sensitivity (87–93 %) and specificity (93–95 %) for detecting moderate and severe vertebral fractures, but lower performance for identifying mild fractures (often of uncertain clinical significance) and in the presence of scoliosis or osteoarthritis [67].
Type 1 Diabetes
There is limited evidence for the use of VFA in fracture risk prediction in T1D. A cross-sectional study by Zhukouskaya et al. [31] assessed 82 TID patients (26 males and 56 females) and 82 controls. T1D patients had a higher prevalence of vertebral fractures (any grade) than controls (24.4 vs. 6.1 %, p = 0.002). Age, diabetes duration, age at diabetes diagnosis, HbA1c, lumbar spine and femoral neck z score, and prevalence of chronic complications were similar for patients with and without vertebral fracture. There was a significant association between T1D and vertebral fracture in the logistic regression models (adjusted OR 4.20, 95 % CI 1.40–12.70, p = 0.01). The study was underpowered for examining higher grade vertebral fractures. The authors concluded that there is a higher prevalence of morphometric vertebral fractures assessed by VFA. Other studies are needed to confirm this small study and prospectively determine whether VFA has the ability to predict clinical fractures in T1D (both subsequent vertebral fractures and/or other clinical fractures) and capture the excess fracture risk associated with this condition.
Type 2 Diabetes
There are no published studies examining VFA in T2D. There is no reason to doubt that vertebral fractures are not important to detect in T2D, as a previous study by Leslie et al. [68] demonstrated that prior vertebral fracture predicts future MOF and hip fracture equally well in women diabetes and without diabetes. However, it is also worth noting that VFA image quality is degraded in obese patients, especially with older generation DXA scanners, which may affect test performance. As with T1D, the ability of VFA to predict clinical fractures and capture the excess fracture risk in T2D remains uncertain.
Body Composition
General Background
Body mass index (BMI) is frequently used to assess for overweight and obesity. However, BMI may erroneously categorize risk in some individuals, as it does not account for body composition or fat distribution [69, 70]. DXA is a well-validated technique for body composition analysis [71]. More recently, methods have been developed to estimate visceral adipose tissue (VAT) from DXA, a metabolically active pathogenic fat depot that is implicated in insulin resistance and T2D. In a cross-sectional study using GE/Lunar VAT, it was shown that greater trochanteric soft tissue thickness, which may protect against hip fracture through reduced force transmission during sideways fall, could be estimated from conventional spine and hip DXA scans [72].
Lean and fat mass differentially affect the skeleton. Ho-Pham et al. [73] performed a meta-analysis of 44 studies involving 20,226 men and women to examine the association between lean mass, fat mass, and BMD. The correlation between lean mass and femoral neck BMD was 0.39 (95 % CI 0.34–0.43), which was significantly higher than the correlation between fat mass and femoral neck BMD (0.28, 95 % CI 0.22–0.33). However, in postmenopausal women the effects of lean mass and fat mass on BMD were comparable.
Leslie et al. [74] examined skeletal health as a function of estimated total body lean and fat mass in 40,050 women and 3600 men age ≥50 years. Femoral neck BMD, femur strength index (SI), CSA, and CSMI were derived from DXA. Increasing lean mass was associated with near-linear increases in femoral BMD, CSA, and CSMI in both women and men. Increasing fat mass showed a small initial increase, followed by a plateau. Femoral SI was relatively unaffected by increasing lean mass, but was associated with a continuous linear decline with increasing fat mass, which should predict higher fracture risk. During follow-up, incident MOF were observed in 2505 women and 180 men (626 and 45 incident hip fractures, respectively). After adjustment for FRAX scores, there was no evidence found that showed lean mass, fat mass, or femoral SI affected prediction of MOF or hip fractures.
Although beyond the scope of the current review, sarcopenia, a reduction in muscle mass and muscle strength, or sarcopenic obesity, the co-occurrence of sarcopenia and obesity, are of interest as markers of frailty and fracture risk [75]. DXA can be used to directly measure and monitor appendicular lean mass, a component of several case definitions for sarcopenia [76, 77]. In a nested case–cohort study by Malkov et al. [76], 169 incident hip fractures were identified among 3079 participants over an average of 13.5 years. Lower DXA-derived subcutaneous fat was associated with fracture risk in men (fully adjusted HR 1.44 per SD decrease; 95 % CI 1.02–2.02) and in women (HR 1.39; 95 % CI 1.07–1.62). Lower appendicular lean mass (normalized for height2) was associated with fracture risk in women in unadjusted analysis (HR 1.80 per SD decrease; 95 % CI 1.42–2.27) but not in the fully adjusted model (HR 1.04; 95 % CI 0.66–1.63). In men, lower appendicular lean mass (kg/m2) was paradoxically protective against fracture (fully adjusted model HR er SD decrease 0.58; 95 % CI 0.36–0.91). The counterintuitive effect of appendicular lean mass was only seen when hip BMD was included in the model. Other studies have reported an additive effect of sarcopenia and osteopenia in men (but not women), though sarcopenia alone did not increase fracture risk [78]. This is an important and evolving area of research.
Type 1 Diabetes
There are few studies published examining the role of body composition in fracture risk in T1D. In a small study, Abd El Dayem et al. [79] studied 47 patients with T1D along with 30 age- and sex-matched controls. Lean body mass and lean/fat ratio were found to be lower in patients with T1D, while total fat mass, abdominal fat percentage, soft tissue fat mass percentage, and fat/lean ratio were higher in T1D as compared to the controls. How much this absolute and relative reduction in lean mass contributes to the excess fracture risk in T1D is uncertain.
Type 2 Diabetes
Body composition and fat distribution, particularly abdominal adiposity, are strongly associated with metabolic morbidities, including T2D, and may play a causal role in their development [79–81]. Leslie et al. [82] studied 30,252 women without previously diagnoses diabetes to determine the association between fat measurements from DXA of the lumbar region or hip and the risk for a subsequent diagnosis of diabetes, which occurred in 1252 (4.1 %) of the women. A new diagnosis of diabetes was strongly associated with greater abdominal fat even when adjusted for age, BMI, and other comorbidities (adjusted HR 1.43; 95 % CI 1.35–1.52 per SD increase), whereas hip fat did not independently predict diabetes. Those in the highest abdominal fat quintile had 3.56 (95 % CI 2.67–4.75) times the risk for subsequent diabetes diagnosis (adjusted for BMI and other covariates) compared to those in the lowest (reference) quintile. Cross-sectional analyses from the same dataset suggest that the difference in spine and hip tissue thickness from regional DXA scans may provide an index of relative abdominal adiposity [82]. Women had significantly lower mean spine-hip thickness differences than men, even after adjustment for the effects of age and BMI. Both men and women with previously diagnosed diabetes had significantly greater mean spine-hip thickness differences before and after adjustment for age and BMI.
Moseley et al. [83] conducted a cross-sectional analysis of 78 men and 56 women with T2D, average age 56 years. Body composition and BMD were measured with DXA. Magnetic resonance imaging (MRI) was used to measure total abdominal, visceral, and subcutaneous fat. Women had significantly higher BMIs than men (BMI 34.4 ± 5.0 kg/m2 vs. 32.6 ± 4.1 kg/m2, p < 0.05), while men had significantly larger waist to hip ratios compared with women (1.0 ± 0.1 vs. 0.8 ± 0.1, p < 0.05) and significantly more lean mass. All measures of fat mass (abdominal total, subcutaneous, and visceral) were significantly higher in women. Lean mass was found to be positively associated with total body, hip, femoral neck, and hip BMD in both sexes. Fat mass, abdominal total, and subcutaneous fat were associated with total body and hip BMD in women. In sex-adjusted generalized linear models, lean mass was positively associated with BMD at the total body, total hip, and femoral neck; fat mass was significantly associated with BMD at the total body and total hip.
Intra-abdominal fat is closely linked to the metabolic syndrome and its complications, including T2D [84, 85]. Strong positive associations have been observed between VAT and T2D. In a study by Rothney et al. [86], a cross-sectional analysis of relationships between DXA-derived VAT (GE/Lunar iDXA [GE Healthcare, Madison, WI]) and cardiometabolic indicators, including T2D, was conducted in 939 subjects (541 women and 398 men). Sex-specific, age-adjusted multivariable regression analysis demonstrated that DXA VAT was significantly associated with increased odds of cardiometabolic indicators, including impaired fasting glucose and T2D (p < 0.001). After additional adjustment for BMI and waist circumference, the OR per SD increase in VAT for T2D was 2.07 (95 %CI 0.73–5.87) for women and 2.25 (95 %CI 1.21–4.19) for men.
Although interesting, none of the preceding studies have examined whether body composition or VAT was a predictor of fracture in T2D. It remains to be seen whether sarcopenia or sarcopenic obesity can identify bone fragility and fracture risk in individuals with T2D. We cannot comment on whether body composition accounts for excess fracture risk in those with diabetes.
Fracture Prediction Tools
General Background
The WHO fracture risk assessment tool (FRAX) is a computer-based algorithm (http://www.shef.ac/uk/FRAX) primarily intended for use in primary care [87, 88].
FRAX calculates fracture probability from easily obtained clinical risk factors: age, sex, body mass index, prolonged use of glucocorticoids, current smoking, alcohol intake of three or more units per day, a parental history of hip fracture, secondary osteoporosis, rheumatoid arthritis, prior fragility fracture, and (optionally) femoral neck BMD or T-score. Probabilities for MOF and hip fracture over 10 years are generated and have been shown to improve fracture prediction over T-score alone. Diabetes is not currently a primary entry variable in FRAX.
The Garvan fracture risk calculator (www.garvan.org.au/bone-fracture-risk) was constructed using information on women and men from the Dubbo Osteoporosis Epidemiology Study (DOES) [89, 90]. Five- and ten-year fracture probability nomograms were constructed using inputs of age, sex, femoral neck BMD (or weight), history of prior fractures after age 50 years (none to 3+), and falls in the previous 12 months (none to 3+). Diabetes is not an input, and no studies have evaluated the Garvan calculator in subjects with T1D or T2D.
The QFracture score (www.qfracture.org) was derived from a cohort including more than one million women and more than one million men age 30–85 years with 24,350 incident osteoporotic fractures in women (9302 hip fractures) and 7934 osteoporotic fractures in men (5424 hip fractures) [91]. It provides outputs for any osteoporotic fracture (hip, wrist, or spine) and hip fracture over a user-selected follow-up period from 1 to 10 years. This algorithm includes T1D or T2D as a direct input, in addition to age, sex, ethnicity, height, weight, smoking status, alcohol consumption, previous fracture, parental osteoporosis or hip fracture, living in a nursing or care home, history of falls, and a number of comorbidities and medications.
Type 1 Diabetes
T1D is considered as one of the causes of secondary osteoporosis in the FRAX algorithm but not as a primary entry variable. As such, it is given the same weight as other causes of secondary osteoporosis (modeled after rheumatoid arthritis) and only increases fracture probability when BMD is not included in the FRAX calculation [92]. As such, FRAX may partially account for the excess fracture risk in T1D, but would underestimate the high relative risk for hip fractures referred to earlier. No studies have directly assessed the performance of FRAX (with or without BMD) for predicting fracture in T1D.
Type 2 Diabetes
Several studies have evaluated the predictive performance of FRAX in patients with diabetes. These studies showed that for a given FRAX probability, there is an increased risk of fracture in diabetics as compared to non-diabetics [34, 93]. Schwartz et al. compared the results of three prospective observational studies of older community-dwelling adults comprised of 9,449 women (770 with T2D) and 7,436 men (1199 with T2D) [34]. For a given FRAX probability, women and men with T2D had a higher observed fracture risk. Despite systematically higher fracture risk attributable to T2D, FRAX predicted hip and non-spine fractures equally well in those with and without T2D (all p-for-interaction >0.10). These findings were echoed in a subsequent study of 3518 patients with diagnosed diabetes (predominantly T2D) from a large clinical cohort in Manitoba, Canada [93]. Diabetes was confirmed to be a risk factor for subsequent MOF (adjusted HR 1.61, 95 % CI 1.42–1.83) or hip fracture (adjusted HR 6.27, 95 % CI 3.62–10.87 aged < 65 years; 2.22, 95 % CI 1.71–2.90 aged ≥ 65 years). FRAX was able to stratify fracture risk in those with diabetes (AUC for MOF 0.67, 95 % CI 0.63–0.70; AUC for hip fracture 0.77, 95 % CI 0.72–0.81), only slightly less well than in those without diabetes. However, FRAX underestimated MOF and hip fracture risk in those with diabetes, even after accounting for competing mortality. The results indicated that FRAX score is useful for the assessment of fracture risk in older adults with diabetes. However, interpretation of the FRAX score in an older patient must take into account the higher fracture risk associated with diabetes.
In a related analysis from the Manitoba database based upon 62,413 individuals 40 years and older (6455 [10 %] with diabetes), diabetes and the FRAX risk factors were independently associated with major osteoporotic fractures and hip fractures [37]. Importantly, diabetes did not significantly modify the effect of individual FRAX risk factors with the exception of age, which exerted a stronger effect on hip fracture, risk in younger as compared to older individuals. For example, major osteoporotic fractures showed a similar relationship to a 10-year increase in age in those without diabetes (HR 1.43) versus those with diabetes (HR 1.39, p interaction 0.781), rheumatoid arthritis (1.43 vs. 1.74, p interaction 0.325) and prior fracture (1.62 vs. 1.72, p interaction 0.588) when adjusted for BMD. When BMD was excluded, an increase in BMI of 5 kg/m2 was similarly protective against major osteoporotic fracture in those without diabetes (HR 0.83) and those with diabetes (HR 0.79, p interaction 0276). The absence of statistically significant interactions between diabetes status and risk factors for predicting MOF implies a simple additive effect of diabetes to the major osteoporotic fracture probability derived from FRAX clinical risk factors.
In summary, the FRAX algorithm underestimates fracture risk in individuals with T2D though individual FRAX risk factors are still important and perform similar to the general population. Importantly, FRAX provided significant fracture discrimination in the diabetes population, similar to the general population even if fracture risk is underestimated. Factors contributing to this underestimation include the higher BMD observed in T2D, greater risk for falls, and alterations in material strength.
Several methods have been proposed to inform the use of FRAX by primary care practitioners in order to accommodate the average effect of T2D despite its absence as an input variable in FRAX. One such method is to use rheumatoid arthritis in the calculation as a proxy for T2D, as the effect appears to be very similar to that of T2D (Fig. 2). Another option is to adjust FRAX score for TBS. A clinical case example illustrated in Table 1 demonstrates the potential changes in a 65-year-old obese female (BMI 30.5 kg/m2) with T2D, a prior fracture, femoral neck T-score of −2.0, and lumbar spine TBS of 1.160. The FRAX calculation without modification yields a 10-year major osteoporotic fracture risk of 17 % and hip fracture risk is 2.6 %. When rheumatoid arthritis is used as a proxy in the calculation, MOF risk is increased to 22 % and hip fracture risk to 3.6 %. When Adjusted for TBS, MOF risk is 20 %, and hip fracture risk 3.4 %. Finally, when BMD is adjusted downwards by 0.5 SD (i.e., T-score −2.5), MOF risk is 21 % and hip fracture risk 4.4 %. This may have clinical implications for treatment. These proposed fracture risk adjustments clearly do not capture the complexities and nuances of T2D, which, as noted earlier, will be influenced by disease-specific factors including duration, control, insulin use, and end-organ complications. However, this approach is consistent with FRAX itself, which dichotomizes complex risk factors as a simple tool for primary care practitioners, not osteoporosis experts or researchers, to provide an adjunct (not a replacement) for clinical judgement [94].

Reprinted with permission [95]
Comparative effects of type 1 diabetes, type 2 diabetes, and inflammatory arthropathy (rheumatoid arthritis or SLE) versus no other risk factors on 10-year probability for major osteoporotic fracture (upper panel) and hip fracture (lower panel) with QFracture®-2013
Conclusions
Table 2 summarizes the evidence reviewed above for the effect of various DXA-derived skeletal parameters on fracture risk in T1D, and whether they can be used to account for the excess fracture risk. BMD is lower in those with T1D, but only partially accounts for the excess risk in those with T1D. It is uncertain whether bone geometry, TBS, VFA, or body composition differs between those with and without diabetes, and whether these are associated with increased fracture risk. As well, it is uncertain whether these parameters account for excess fracture risk in T1D. FRAX does differ between those with and without T1D (lower BMD and through the secondary osteoporosis input), but likely only partially accounts for excess risk of fracture.
Table 3 summarizes the evidence reviewed above for the effect of various DXA-derived skeletal parameters on fracture risk in T2D. BMD tends to be higher in those with versus without diabetes and is associated with an increased fracture risk, but this clearly cannot account for the excess risk of fracture in T2D. TBS also differs between those with and without diabetes, is associated with increased fracture risk, and may partially account for excess risk of fracture. It is uncertain whether FRAX does differ between those with and without T2D (through higher BMI and BMD), but this does not account for the excess fracture risk. It remains uncertain whether bone geometry, VFA, or body composition differs between those with and without T2D, is associated with increased fracture risk, or can account for the excess risk in T2D.
In summary, diabetes mellitus is characterized by a significant increase in fracture risk that is only partially reflected by the BMD reductions seen in T1D and is underestimated in T2D where BMD is increased. While BMD from DXA still stratifies fracture risk in those with diabetes, additional measures that can be obtained from DXA help to identify patients at increased risk of fracture. Incorporating this additional information into risk prediction models may help to avoid systematically underestimating the risk of osteoporosis-related fractures in subjects with diabetes.
References
Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ 3rd, Khaltaev N (2008) A reference standard for the description of osteoporosis. Bone 42(3):467–475
Johnell O, Kanis JA, Oden A et al (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20(7):1185–1194
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ (Clin Res Ed.) 312(7041):1254–1259
Cole ZA, Dennison EM, Cooper C (2008) Osteoporosis epidemiology update. Curr Rheumatol Rep 10(2):92–96
Menke A, Casagrande S, Geiss L, Cowie CC (2015) Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA 314(10):1021–1029
Janghorbani M, Van Dam RM, Willett WC, Hu FB (2007) Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol 166(5):495–505
Vestergaard P (2007) Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes–a meta-analysis. Osteoporos Int 18(4):427–444
Ma L, Oei L, Jiang L et al (2012) Association between bone mineral density and type 2 diabetes mellitus: a meta-analysis of observational studies. Eur J Epidemiol 27(5):319–332
Kume S, Kato S, Yamagishi S et al (2005) Advanced glycation end-products attenuate human mesenchymal stem cells and prevent cognate differentiation into adipose tissue, cartilage, and bone. J Bone Miner Res 20(9):1647–1658
Sanguineti R, Storace D, Monacelli F, Federici A, Odetti P (2008) Pentosidine effects on human osteoblasts in vitro. Ann N Y Acad Sci 1126:166–172
Burghardt AJ, Issever AS, Schwartz AV et al (2010) High-resolution peripheral quantitative computed tomographic imaging of cortical and trabecular bone microarchitecture in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab 95(11):5045–5055
Pritchard JM, Giangregorio LM, Atkinson SA et al (2012) Association of larger holes in the trabecular bone at the distal radius in postmenopausal women with type 2 diabetes mellitus compared to controls. Arthritis Care Res 64(1):83–91
Petit MA, Paudel ML, Taylor BC et al (2010) Bone mass and strength in older men with type 2 diabetes: the Osteoporotic Fractures in Men Study. J Bone Miner Res 25(2):285–291
Bolotin HH, Sievanen H, Grashuis JL (2003) Patient-specific DXA bone mineral density inaccuracies: quantitative effects of nonuniform extraosseous fat distributions. J Bone Miner Res 18(6):1020–1027
Hangartner TN, Johnston CC (1990) Influence of fat on bone measurements with dual-energy absorptiometry. Bone Miner 9(1):71–81
Yu EW, Thomas BJ, Brown JK, Finkelstein JS (2012) Simulated increases in body fat and errors in bone mineral density measurements by DXA and QCT. J Bone Miner Res 27(1):119–124
Yu EW, Bouxsein ML, Roy AE et al (2014) Bone loss after bariatric surgery: discordant results between DXA and QCT bone density. J Bone Miner Res 29(3):542–550
Dawson-Hughes B, Dallal GE (1990) Effect of radiographic abnormalities on rate of bone loss from the spine. Calcif Tissue Int 46(4):280–281
Greenspan SL, Maitland LA, Myers ER, Krasnow MB, Kido TH (1994) Femoral bone loss progresses with age: a longitudinal study in women over age 65. J Bone Miner Res 9(12):1959–1965
Johansson H, Kanis JA, Oden A et al (2014) A meta-analysis of the association of fracture risk and body mass index in women. J Bone Miner Res 29(1):223–233
Kayath MJ, Tavares EF, Dib SA, Vieira JG (1998) Prospective bone mineral density evaluation in patients with insulin-dependent diabetes mellitus. J Diabetes Complicat 12(3):133–139
Krakauer JC, McKenna MJ, Buderer NF, Rao DS, Whitehouse FW, Parfitt AM (1995) Bone loss and bone turnover in diabetes. Diabetes 44(7):775–782
Miazgowski T, Czekalski S (1998) A 2-year follow-up study on bone mineral density and markers of bone turnover in patients with long-standing insulin-dependent diabetes mellitus. Osteoporos Int 8(5):399–403
Miazgowski T, Pynka S, Noworyta-Zietara M, Krzyzanowska-Swiniarska B, Pikul R (2007) Bone mineral density and hip structural analysis in type 1 diabetic men. Eur J Endocrinol/Eur Fed Endocr Soc 156(1):123–127
Hamilton EJ, Rakic V, Davis WA et al (2012) A five-year prospective study of bone mineral density in men and women with diabetes: the Fremantle Diabetes Study. Acta Diabetol 49(2):153–158
Maser RE, Kolm P, Modlesky CM, Beck TJ, Lenhard MJ (2012) Hip strength in adults with type 1 diabetes is associated with age at onset of diabetes. J Clin Densitom 15(1):78–85
Joshi A, Varthakavi P, Chadha M, Bhagwat N (2013) A study of bone mineral density and its determinants in type 1 diabetes mellitus. J osteoporos 2013:397814
Mastrandrea LD, Wactawski-Wende J, Donahue RP, Hovey KM, Clark A, Quattrin T (2008) Young women with type 1 diabetes have lower bone mineral density that persists over time. Diabetes Care 31(9):1729–1735
Liu EY, Wactawski-Wende J, Donahue RP, Dmochowski J, Hovey KM, Quattrin T (2003) Does low bone mineral density start in post-teenage years in women with type 1 diabetes? Diabetes Care 26(8):2365–2369
Strotmeyer ES, Cauley JA, Orchard TJ, Steenkiste AR, Dorman JS (2006) Middle-aged premenopausal women with type 1 diabetes have lower bone mineral density and calcaneal quantitative ultrasound than nondiabetic women. Diabetes Care 29(2):306–311
Zhukouskaya VV, Eller-Vainicher C, Vadzianava VV et al (2013) Prevalence of morphometric vertebral fractures in patients with type 1 diabetes. Diabetes Care 36(6):1635–1640
Leidig-Bruckner G, Grobholz S, Bruckner T, Scheidt-Nave C, Nawroth P, Schneider JG (2014) Prevalence and determinants of osteoporosis in patients with type 1 and type 2 diabetes mellitus. BMC Endocr Disord 14:33
de Liefde II, van der Klift M, de Laet CE, van Daele PL, Hofman A, Pols HA (2005) Bone mineral density and fracture risk in type-2 diabetes mellitus: the Rotterdam Study. Osteoporos Int 16(12):1713–1720
Schwartz AV, Vittinghoff E, Bauer DC et al (2011) Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA 305(21):2184–2192
Napoli N, Strotmeyer ES, Ensrud KE et al (2014) Fracture risk in diabetic elderly men: the MrOS study. Diabetologia 57(10):2057–2065
Bonds DE, Larson JC, Schwartz AV et al (2006) Risk of fracture in women with type 2 diabetes: the Women’s Health Initiative Observational Study. J Clin Endocrinol Metabol 91(9):3404–3410
Leslie WD, Morin SN, Lix LM, Majumdar SR (2014) Does diabetes modify the effect of FRAX risk factors for predicting major osteoporotic and hip fracture? Osteoporos Int 25(12):2817–2824
Broy SB, Cauley JA, Lewiecki ME, Schousboe JT, Shepherd JA, Leslie WD (2015) Fracture risk prediction by non-BMD DXA measures: the 2015 iscd official positions part 1: hip geometry. J Clin Densitom 18(3):287–308
Pisharody S, Phillips R, Langton CM (2008) Sensitivity of proximal femoral stiffness and areal bone mineral density to changes in bone geometry and density. Proc Inst Mech Eng [H] 222(3):367–375
Naylor KE, McCloskey EV, Eastell R, Yang L (2013) Use of DXA-based finite element analysis of the proximal femur in a longitudinal study of hip fracture. J Bone Miner Res 28(5):1014–1021
Vaananen SP, Grassi L, Flivik G, Jurvelin JS, Isaksson H (2015) Generation of 3D shape, density, cortical thickness and finite element mesh of proximal femur from a DXA image. Med Image Anal 24(1):125–134
Ferdous Z, Luo Y (2015) Study of hip fracture risk by DXA-based patient-specific finite element model. Bio-Med Mater Eng 25(2):213–220
Leslie WD, Lix LM, Morin SN et al (2015) Hip axis length is a FRAX- and bone density-independent risk factor for hip fracture in women. J Clin Endocrinol Metab 100(5):2063–2070
Leslie WD, Lix LM, Morin SN et al (2016) Adjusting hip fracture probability in men and women using hip axis length: the Manitoba bone density database. J Clin Densitom 19(3):326–331
Akeroyd JM, Suarez EA, Bartali B et al (2014) Differences in skeletal and non-skeletal factors in a diverse sample of men with and without type 2 diabetes mellitus. J Diabetes Complicat 28(5):679–683
Yang L, Palermo L, Black DM, Eastell R (2014) Prediction of incident hip fracture with the estimated femoral strength by finite element analysis of DXA Scans in the study of osteoporotic fractures. J Bone Miner Res 29(12):2594–2600
Yang L, Peel N, Clowes JA, McCloskey EV, Eastell R (2009) Use of DXA-based structural engineering models of the proximal femur to discriminate hip fracture. J Bone Miner Res 24(1):33–42
Garg R, Chen Z, Beck T et al (2012) Hip geometry in diabetic women: implications for fracture risk. Metab Clin Exp 61(12):1756–1762
Moseley KF, Dobrosielski DA, Stewart KJ, Sellmeyer DE, Jan De Beur SM (2011) Lean mass predicts hip geometry in men and women with non-insulin-requiring type 2 diabetes mellitus. J Clin Densitom 14(3):332–339
Hamilton CJ, Jamal SA, Beck TJ et al (2013) Evidence for impaired skeletal load adaptation among Canadian women with type 2 diabetes mellitus: insight into the BMD and bone fragility paradox. Metab Clin Exp 62(10):1401–1405
Ishii S, Cauley JA, Crandall CJ et al (2012) Diabetes and femoral neck strength: findings from the hip strength across the menopausal transition study. J Clin Endocrinol Metab 97(1):190–197
Hadjidakis DJ, Raptis AE, Sfakianakis M, Mylonakis A, Raptis SA (2006) Bone mineral density of both genders in Type 1 diabetes according to bone composition. J Diabetes Complicat 20(5):302–307
McCloskey EV, Oden A, Harvey NC et al (2015) Adjusting fracture probability by trabecular bone score. Calcif Tissue Int 96(6):500–509
Silva BC, Broy SB, Boutroy S, Schousboe JT, Shepherd JA, Leslie WD (2015) Fracture risk prediction by non-BMD DXA measures: the 2015 ISCD official positions part 2: trabecular bone score. J Clin Densitom 18(3):309–330
Leslie WDBN (2016) Spine bone texture and the trabecular bone score (TBS). In: Preedy VBPaVR (ed) Biomarkers in disease methods, discoveries and applications. Springer, New York
Hans D, Goertzen AL, Krieg MA, Leslie WD (2011) Bone microarchitecture assessed by TBS predicts osteoporotic fractures independent of bone density: the Manitoba study. J Bone Miner Res 26(11):2762–2769
Leslie WD, Aubry-Rozier B, Lamy O, Hans D (2013) TBS (trabecular bone score) and diabetes-related fracture risk. J Clin Endocrinol Metab 98(2):602–609
McCloskey EV, Oden A, Harvey NC et al (2016) A meta-analysis of trabecular bone score in fracture risk prediction and its relationship to FRAX. J Bone Miner Res 31(5):940–948
Neumann T, Lodes S, Kastner B et al (2016) Trabecular bone score in type 1 diabetes-a cross-sectional study. Osteoporos Int 27(1):127–133
Dhaliwal R, Cibula D, Ghosh C, Weinstock RS, Moses AM (2014) Bone quality assessment in type 2 diabetes mellitus. Osteoporos Int 25(7):1969–1973
Kim JH, Choi HJ, Ku EJ et al (2015) Trabecular bone score as an indicator for skeletal deterioration in diabetes. J Clin Endocrinol Metab 100(2):475–482
Ferrar L, Jiang G, Adams J, Eastell R (2005) Identification of vertebral fractures: an update. Osteoporos Int 16(7):717–728
Strotmeyer ES, Cauley JA, Schwartz AV et al (2005) Nontraumatic fracture risk with diabetes mellitus and impaired fasting glucose in older white and black adults: the health, aging, and body composition study. Arch Intern Med 165(14):1612–1617
Crans GG, Genant HK, Krege JH (2005) Prognostic utility of a semiquantitative spinal deformity index. Bone 37(2):175–179
Rosen HN, Vokes TJ, Malabanan AO et al (2013) The official positions of the international society for clinical densitometry: vertebral fracture assessment. J Clin Densitom 16(4):482–488
Chou SH, Vokes TJ, Ma SL, Costello M, Rosen HR, Schousboe JT (2014) Simplified criteria for selecting patients for vertebral fracture assessment. J Clin Densitom 17(3):386–391
Lewiecki EM, Laster AJ (2006) Clinical review: clinical applications of vertebral fracture assessment by dual-energy x-ray absorptiometry. J Clin Endocrinol Metab 91(11):4215–4222
Leslie WD, Lix LM, Prior HJ, Derksen S, Metge C, O’Neil J (2007) Biphasic fracture risk in diabetes: a population-based study. Bone 40(6):1595–1601
Gelber RP, Gaziano JM, Orav EJ, Manson JE, Buring JE, Kurth T (2008) Measures of obesity and cardiovascular risk among men and women. J Am Coll Cardiol 52(8):605–615
Storti KL, Brach JS, FitzGerald SJ, Bunker CH, Kriska AM (2006) Relationships among body composition measures in community-dwelling older women. Obesity (Silver Spring, Md.) 14(2):244–251
Albanese CV, Diessel E, Genant HK (2003) Clinical applications of body composition measurements using DXA. J Clin Densitom 6(2):75–85
Schacter GI, Leslie WD (2015) Spine-hip thickness difference measured by dual-energy X-ray absorptiometry is associated with diabetes mellitus in women and men. J Clin Densitom 18(4):512–518
Ho-Pham LT, Nguyen UD, Nguyen TV (2014) Association between lean mass, fat mass, and bone mineral density: a meta-analysis. J Clin Endocrinol Metab 99(1):30–38
Leslie WD, Orwoll ES, Nielson CM et al (2014) Estimated lean mass and fat mass differentially affect femoral bone density and strength index but are not FRAX independent risk factors for fracture. J Bone Miner Res 29(11):2511–2519
Cauley JA (2015) An overview of sarcopenic obesity. J Clin Densitom 18(4):499–505
Malkov S, Cawthon PM, Peters KW et al (2015) Hip fractures risk in older men and women associated with DXA-derived measures of thigh subcutaneous fat thickness, cross-sectional muscle area, and muscle density. J Bone Miner Res 30(8):1414–1421
Cawthon PM (2015) Assessment of lean mass and physical performance in sarcopenia. J Clin Densitom 18(4):467–471
Chalhoub D, Cawthon PM, Ensrud KE et al (2015) Risk of nonspine fractures in older adults with sarcopenia, low bone mass, or both. J Am Geriatr Soc 63(9):1733–1740
Abd El Dayem SM, El-Shehaby AM, Abd El Gafar A, Fawzy A, Salama H (2011) Bone density, body composition, and markers of bone remodeling in type 1 diabetic patients. Scand J Clin Lab Investig 71(5):387–393
Direk K, Cecelja M, Astle W et al (2013) The relationship between DXA-based and anthropometric measures of visceral fat and morbidity in women. BMC Cardiovasc Disord 13:25
Porter SA, Massaro JM, Hoffmann U, Vasan RS, O’Donnel CJ, Fox CS (2009) Abdominal subcutaneous adipose tissue: a protective fat depot? Diabetes Care 32(6):1068–1075
Leslie WD, Ludwig SM, Morin S (2010) Abdominal fat from spine dual-energy X-ray absorptiometry and risk for subsequent diabetes. J Clin Endocrinol Metab 95(7):3272–3276
Moseley KF, Dobrosielski DA, Stewart KJ, De Beur SM, Sellmeyer DE (2011) Lean mass and fat mass predict bone mineral density in middle-aged individuals with noninsulin-requiring type 2 diabetes mellitus. Clin Endocrinol 74(5):565–571
von Eyben FE, Mouritsen E, Holm J et al (2003) Intra-abdominal obesity and metabolic risk factors: a study of young adults. Int J obes Related Metab Disord 27(8):941–949
Jensen MD (2008) Role of body fat distribution and the metabolic complications of obesity. J Clin Endocrinol Metab 93(11 Suppl 1):S57–S63
Rothney MP, Catapano AL, Xia J et al (2013) Abdominal visceral fat measurement using dual-energy X-ray: association with cardiometabolic risk factors. Obesity (Silver Spring, Md.) 21(9):1798–1802
Kanis JA (2008) Assessment of osteoporosis at the primary health-care level. Technical Report. WHO Collaborating Centre for Metabolic Bone Disease, University of Sheffield, UK
Kanis JA, Oden A, Johansson H, Borgstrom F, Strom O, McCloskey E (2009) FRAX and its applications to clinical practice. Bone 44(5):734–743
Nguyen ND, Frost SA, Center JR, Eisman JA, Nguyen TV (2007) Development of a nomogram for individualizing hip fracture risk in men and women. Osteoporos Int 18(8):1109–1117
Langsetmo L, Nguyen TV, Nguyen ND et al (2011) Independent external validation of nomograms for predicting risk of low-trauma fracture and hip fracture. CMAJ Can Med Assoc J 183(2):E107–E114
Hippisley-Cox J, Coupland C (2009) Predicting risk of osteoporotic fracture in men and women in England and Wales: prospective derivation and validation of QFractureScores. BMJ (Clin Res Ed.) 339:b4229
Hough FS, Pierroz DD, Cooper C, Ferrari SL (2016) MECHANISMS IN ENDOCRINOLOGY: Mechanisms and evaluation of bone fragility in type 1 diabetes mellitus. Eur J Endocrinol/Eur Fed Endocr Soc 174(4):R127–R138
Giangregorio LM, Leslie WD, Lix LM et al (2012) FRAX underestimates fracture risk in patients with diabetes. J Bone Min Res 27(2):301–308
Kanis JA, Hans D, Cooper C et al (2011) Interpretation and use of FRAX in clinical practice. Osteoporos Int 22(9):2395–2411
Lecka-Czernik B, Fowlkes J (eds) (2016) Diabetic bone disease: basic and translational research and clinical applications. Springer International Publishing, Switzerland
Conflict of interest
G. Isanne Schacter and William D. Leslie declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schacter, G.I., Leslie, W.D. DXA-Based Measurements in Diabetes: Can They Predict Fracture Risk?. Calcif Tissue Int 100, 150–164 (2017). https://doi.org/10.1007/s00223-016-0191-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-016-0191-x