Abstract
Aims/hypothesis
Diabetes mellitus is associated with increased fracture risk in women but few studies are available in men. To evaluate the relationship between diabetes and prospective non-vertebral fractures in elderly men, we used data from the Osteoporotic Fractures in Men (MrOS) study.
Methods
The MrOS enrolled 5,994 men (aged ≥65 years). Diabetes (ascertained by self-report, the use of medication for diabetes or an elevated fasting glucose level) was reported in 881 individuals, 80 of whom were using insulin. Hip and spine bone mineral density (BMD) was measured using dual x-ray absorptiometry (DXA). After recruitment, the men were followed for incident non-vertebral fractures using a triannual (3 yearly) questionnaire for an average of 9.1 (SD 2.7) years. The Cox proportional hazards model was used to assess the incident risk of fractures.
Results
In models adjusted for age, race, clinic site and total hip BMD, the risk of non-vertebral fracture was higher in men with diabetes compared with normoglycaemic men (HR 1.30, 95% CI 1.09, 1.54) and was elevated in men using insulin (HR 2.46, 95% CI 1.69, 3.59). Men with impaired fasting glucose did not have a higher risk of fracture compared with normoglycaemic men (HR 1.04, 95% CI 0.89, 1.21). After multivariable adjustment, the risk of non-vertebral fracture remained higher only among men with diabetes who were using insulin (HR 1.74, 95% CI 1.13, 2.69).
Conclusions/interpretation
Men with diabetes who are using insulin have an increased risk of non-vertebral fracture for a given age and BMD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For many years, diabetic patients were not considered to be at risk of osteoporosis, based on reports of their higher bone mineral density (BMD) compared with healthy individuals. However, a 2001 analysis from the Study of Osteoporotic Fractures revealed that older women with type 2 diabetes had an increased risk of non-vertebral fractures [1], a finding confirmed in later studies [2, 3]. Two meta-analyses, which included data on more than one million participants, reported an OR of 1.4–1.7 for hip fractures in patients with type 2 diabetes [4, 5]. Insulin use appears to be associated with an increased fracture risk, possibly as a marker of long-standing diabetes [1]. The increased risk of fractures in women with diabetes may be partly explained by more frequent falls [1]. In addition, diabetic bone may be more fragile at a given BMD [6].
However, most of the available data for non-vertebral fracture have been collected in women or in studies that did not report sex-specific results. A meta-analysis of five studies showed an increased risk of hip fracture in men with type 2 diabetes (RR 2.8, 95% CI 1.2, 6.6) [4]. Results for non-vertebral fractures in men also suggested an increased risk, but this has not been clearly demonstrated [7–10]. Previous studies have been hampered by the small number of men included; most studies have not been able to adjust for BMD or falls.
Therefore, utilising data from the Osteoporotic Fractures in Men (MrOS) study, a large multicentre prospective observational study examining the incidence and predictors of fractures in older men, we evaluated: (1) the effect of diabetes or impaired fasting glucose (IFG) on the risk of non-vertebral fractures in elderly men, taking into account BMD and falls; and (2) the risk factors for fracture among older men with diabetes, including the effect of diabetes medications.
Methods
Participants
From March 2000 through April 2002, 5,994 men aged ≥65 years were enrolled in the baseline examination of the prospective MrOS study [11, 12]. Men were recruited from population-based listings in six areas of the USA: Birmingham, AL; Minneapolis, MN; Palo Alto, CA; the Monongahela Valley near Pittsburgh, PA; Portland, OR; and San Diego, CA. Men with a history of bilateral hip replacement and men who were unable to walk without the assistance of another person were excluded. The institutional review boards of each centre approved the study protocol, and written consent was obtained from all the participants.
Diabetes and IFG status
Participants attended a baseline clinic visit and up to five follow-up visits. Their baseline diabetes status was ascertained using fasting glucose levels, a self-reported diagnosis of diabetes and the medication inventory (described below). In men without self-reported diabetes or use of diabetes medications, we used ADA criteria. These men were considered to have normoglycaemia if their fasting glucose level was <5.6 mmol/l and considered to have IFG if their fasting glucose level was between 5.6 and 6.9 mmol/l [13]. Men with a fasting glucose ≥7 mmol/l and/or self-reported diabetes and/or the use of medications to treat diabetes were considered to have diabetes. Patients using insulin were analysed separately. At the follow-up visits, the men were queried regarding a history of diabetes, and a new medication inventory was obtained. Diabetes and insulin use status were updated based on these reports. Fasting glucose level data were not available for follow-up visits. HbA1c was not measured in the MrOS study.
Ascertainment of fracture
As previously described, after recruitment, men were followed for incident fracture with a triannual (3 yearly) questionnaire administered by mail or telephone [14]. The average follow-up for fractures was 9.1 (SD 2.7) years. Reports of fracture were followed up by the study staff to determine the date, a description of how the fracture occurred and whether there was any trauma associated with the fracture. Fractures were centrally adjudicated by a physician review of the medical records and x-ray reports without any knowledge of the individual’s diabetes status. We included only confirmed non-spine fractures. We included fractures regardless of the trauma level. High-trauma fractures are associated with a low bone density in men and women [15], and the exclusion of fractures resulting from excess trauma has been reported to underestimate the contribution of osteoporosis to fractures [16].
Covariates
Questionnaire and medication inventory
At baseline, information on demographic and anthropometric variables, personal and family medical history, lifestyle, functional status, visual and neuromuscular function and frailty, as well as cognitive data, was obtained by self-report, interview or examination by trained and certified staff [12]. Data on age and race/ethnicity (white, black, Asian, Hispanic, Native Hawaiian/Pacific Islander, American Indian/Alaskan Native or multiracial) were collected.
Physical activity was assessed with the Physical Activity Scale for the Elderly (PASE) [17] together with questions on daily sedentary activity (sometimes/often sit >4 h/day). Additional questions included specific common medical conditions (e.g. diabetes mellitus, hypothyroidism, heart attack and stroke), a personal history of fracture at ≥50 years of age and a maternal history of hip fracture. Participants were asked at the baseline and follow-up visits about falls in the previous 12 months. General health status was self-rated as excellent/good vs fair/poor/very poor. Participants were asked about their mood during the previous 4 weeks to assess for depression. Lifestyle risk factors included smoking (current, past, never) and dietary intake of calcium and vitamin D. Functional status was assessed by summing the amount of difficulty (on a 0–3 scale) related to five instrumental activities of daily living: difficulty with walking 2–3 blocks outside on level ground, climbing ten steps without resting, preparing meals, doing heavy housework and shopping for groceries or clothes (overall score range 0–15) [18].
The Block 98 semiquantitative food frequency questionnaire (Block Dietary Data Systems, Berkeley, CA, USA) was specifically modified for the MrOS study to capture the most important sources of calcium and vitamin D in older men in the USA. The nutrient composition was calculated using the US Department of Agriculture Database for Standard Reference, Version 12, and the 1994–1996 Continuing Survey of Food Intake by Individuals database (www.ars.usda.gov). For this analysis, we used the usual daily intake of calcium (mg) and vitamin D (IU) from the participants’ diet and supplements.
The participants were instructed to bring to their clinic visit all prescription medications taken in the past 30 days, and specially trained study coordinators recorded these medications. The Iowa Drug Information Service Drug Vocabulary (College of Pharmacy, University of Iowa, Iowa City, IA, USA) was used to identify the ingredient(s) in the medications [18]; these data were stored in an electronic medications inventory database (San Francisco Coordinating Center, San Francisco, CA, USA). Specific classes of medications of interest, including diabetes medications, were centrally coded by trained staff. This medication inventory was also obtained at follow-up visits.
Functional assessment
Measurements taken on examination included anthropometry, cognitive function, visual function, neuromuscular function and BMD. Body weight (kg; in indoor clothing without shoes) was recorded with a calibrated balance beam or electronic scale. Height (cm) was measured using a wall-mounted Harpenden stadiometer (Holtain, Crymych, UK). The Modified Mini-Mental State examination (scored from 0 to 100) was conducted to assess cognitive function [19]. We assessed contrast sensitivity (vision contrast test system; Visitech Consultants, Dayton, OH, USA).
The participants were asked to stand from a chair without using their arms; those who were unable to do a single chair stand were classified as ‘unable’ to complete the test. All men who were able to complete the single chair stand were asked to complete the repeated chair stand test. The ability and time required to complete five stands without using the arms were recorded. If the men were unable to do five chair stands, used their arms during the test, were unable to complete the test or refused to do the repeated chair stand test, they were also classified as ‘unable’. Grip strength (kg) was measured twice using a hand-held dynameter (Jamar, Sammons Preston Rolyan, Bolingbrook, IL, USA) in both the right and left arms; the average of the readings for the right and left was used in the analysis.
Frailty was evaluated using five components, similar to the criteria proposed by Fried et al [20]: weight loss between baseline and the second examination (~3.4 years), weakness (low grip strength), poor energy (based on the answer to the question ‘Do you feel full of energy?’), slowness (a slow walking speed) and low physical activity (using the PASE). Those with three or more components were categorised as frail, with two components as pre-frail, with one component intermediate, and with zero components as robust [21].
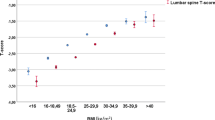
Dual energy x-ray absorptiometry
The total body, lumbar spine (L1–L4) and total femur area BMD, and the body composition (total body lean mass and total body fat mass), were measured at baseline and for up to three follow-up visits using dual energy x-ray absorptiometry (DXA). The same scanner model was used at all six sites and at all visits (QDR 4,500 W; Hologic, Bedford, MA, USA). Standardised procedures for positioning the participants and analysing the scans were followed for all scans. All DXA operators were centrally certified based on an evaluation of their scanning and analysis techniques. Cross-calibration studies performed before the baseline MrOS visit found no linear differences across the scanners, and the maximum percentage difference in mean total spine BMD between scanners was 1.4% [22]. Participants’ scans were not corrected for cross-machine differences, but statistical models were adjusted for clinic site. Participants’ DXA results were corrected as needed for longitudinal changes in machine performance, based on regular scans of Hologic spine and whole-body phantoms at each site.
Biochemistry
Baseline fasting morning serum was collected and stored at −70°C. Glucose was measured using a hexokinase method using previously unthawed serum (Northwest Lipid Metabolism and Diabetes Research Laboratories, Seattle, WA, USA). The interassay CV for glucose based on blind duplicates was <3%. Serum creatinine was measured on previously thawed specimens using a Roche COBAS Integra 800 automated analyser (Roche Diagnostics, Indianapolis, IN, USA), using a variation of the Jaffe colorimetric method. The assay was calibrated daily, and interassay and intra-assay CVs were 5.3%. Estimated GFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [23].
Statistical analysis
The characteristics of the cohort are presented separately by baseline diabetes status. The Cox proportional hazards model was used to assess the association between diabetes and the time after baseline to a first non-spine fracture during 9.1 (2.7) years of follow-up. The primary analysis included diabetes compared with no diabetes as the reference group; a secondary analysis included diabetes with insulin use, diabetes without insulin use, and IFG, compared with participants with normoglycaemia as the reference group. Diabetes status was entered into these models as a time-dependent covariate. Total hip BMD and number of falls in the previous year were also modelled as time-dependent covariates. Other variables were entered as baseline measurements.
All models included an adjustment for age, race and clinic site. Total hip BMD and history of falls were added separately to this model to assess their influence on the relationship between diabetes and fractures. In the first analysis (diabetes compared with no diabetes), the addition of falls almost completely attenuated the association between diabetes and non-spine fracture, and a larger multivariable model was not developed. In the second analysis, the addition of falls to the model did not fully attenuate the relationship between diabetes with insulin use and fracture risk.
To develop a multivariable model, additional variables were selected for initial inclusion in the model based on risk factors for fracture previously identified in the MrOS cohort [14]. The initial variables, in addition to history of diabetes, age, race, clinic site, total hip BMD and falls in the previous year, were: history of fracture at age ≥50 years; maternal hip fracture; calcium intake; vitamin D intake; current use of oral corticosteroids, loop diuretics, selective serotonin reuptake inhibitors, tricyclic antidepressants or thiazolidinediones (TZDs); current smoker; history of stroke, thyroid dysfunction or heart attack; self-rated health compared with others; difficulty with instrumental activities of daily living; BMI; hours per day sitting upright; physical activity (PASE score); estimated GFR; grip strength; inability to stand up from a chair without using the arms; contrast sensitivity; score on Teng’s Modified Mini-Mental State examination; frailty status; and being downhearted for most of the time. Variables were retained if their removal changed the coefficient for insulin-using diabetes mellitus by ≥10% compared with the minimally adjusted model. A Wald test was used to determine whether the HR for insulin-using diabetes was statistically different from the HR for non-insulin-using diabetes in the multivariable model for non-spine fracture.
A Cox proportional hazards model was used to assess risk factors for non-spine fracture among diabetic men only. The variables were identified in advance and included key demographics (age, race/ethnicity), factors associated with fracture risk in other populations (total hip BMD, falls) and diabetes-related factors (diabetes medications, fasting glucose level). All the variables were retained in the model. All analyses were conducted using SAS Version 9.13 (SAS Institute, Cary, NC, USA).
Results
The baseline characteristics of the MrOS participants according to diabetes status are reported in Table 1. Among a total of 5,994 study participants, 2,027 individuals had impaired fasting glucose (IFG) and 881 had diabetes, 80 of whom were on insulin treatment. Ninety per cent of the participants were white. The median age was approximately 73.5 years, with an average baseline BMI in the overweight range in all groups. Total hip BMD was also higher in diabetic men and was progressively lower in men with IFG and in men with normal glucose levels. Men with diabetes had a lower physical performance for grip strength and chair stand. Men using insulin reported more falls than other men and were more likely to report a history of fractures.
Table 2 presents the incidence of non-vertebral fractures by diabetes status. Among 3,086 men with a normal fasting glucose level, 459 had at least one non-vertebral fracture during the average follow-up of 9.1 years. During the same follow-up, 107 diabetic men without insulin use and 20 men using insulin developed at least one non-vertebral fracture. The incidence rate of non-vertebral fracture was similar for normoglycaemic men (1.74 per 100 person-years), those with IFG (1.62 per 100 person-years) and those with diabetes who were not using insulin (1.69 per 100 person-years), but was higher in those using insulin (3.56 per 100 person-years).
Adjusting for age, race and clinic site, diabetic men did not have an increased risk of non-vertebral fractures compared with men without diabetes (HR 1.12, 95% CI 0.94, 1.34). However, with additional adjustment for total hip BMD, diabetes was associated with an increased risk of fracture (HR 1.30, 95% CI 1.09, 1.54). In a model that was additionally adjusted for a history of falls, however, the relationship between diabetes and fracture was no longer significant (HR 1.08, 95% CI 0.91, 1.29).
When the men were categorised by insulin use and by diabetes status, men using insulin had a higher risk of all non-vertebral fractures (HR 2.24, 95% CI 1.53, 3.27) despite their higher BMD, compared with normoglycaemic men (Table 3). Diabetic men who were not treated with insulin did not have a higher risk of fracture (HR 0.98, 95% CI 0.80, 1.20), nor did men with IFG (HR 0.95, 95% CI 0.81, 1.10). In a model also controlling for total hip BMD, men with diabetes who were not using insulin had a modestly increased risk of non-vertebral fractures compared with men who were normoglycaemic, but the increased risk was not statistically significant (HR 1.18, 95% CI 0.96, 1.44). The addition of total hip BMD (Table 3, Model 3) did not appreciably alter the relationship between insulin use and fracture risk (HR 2.46, 95% CI 1.69, 3.59). We therefore added an adjustment for fall risk (Table 3, Model 4) and found that the association between insulin-using diabetes and fracture risk was attenuated but still significantly elevated (HR 1.98, 95% CI 1.34, 2.15).
In other multivariable models (Table 3, Model 5) additionally adjusted for BMI and other covariates associated with bone loss and fracture, the risk of non-vertebral fracture remained elevated only among men with insulin-treated diabetes (HR 1.74, 95% CI 1.13, 2.69). No effect was found in men not using insulin or in men with IFG. The HRs for diabetes with insulin use (HR 1.74, 95% CI 1.13, 2.69) and for diabetes without insulin use (HR 1.00, 95% CI 0.80, 1.25) were statistically different (Wald test p value 0.017).
In a separate model that included only men with a diagnosis of diabetes at baseline (Table 4), factors that were associated with an increased risk of fractures included lower total hip BMD (HR 1.69, 95% CI 1.38, 2.06), falls in the previous 12 months (HR 1.61, 95% CI 1.06, 2.44) and sulfonylurea use (HR 1.66, 95% CI 1.09, 2.51). Hispanic, but not black or Asian, men had a significantly elevated risk relative to white men. The use of TZDs or metformin did not affect the risk of fractures. In this model, a significantly increased risk of fractures was not observed among insulin users. Baseline fasting glucose level was also no longer associated with fracture risk.
Discussion
Our findings suggest that older men with diabetes mellitus have an increased risk of non-vertebral fractures compared with normoglycaemic men, adjusting for age and total hip BMD. However, diabetic men receiving insulin treatment had nearly double the risk of fractures compared with those without diabetes after adjustment for covariates available in the MrOS study. In diabetic men who were not using insulin, the fracture rate was not increased during an average 9 year follow-up. IFG did not affect the fracture rate. Factors associated with an increased risk of fractures included lower total hip BMD, recent falls and sulfonylurea use.
A few previous studies have estimated the RR for non-vertebral or all clinical fractures associated with diabetes in men. The Rotterdam study reported that although men with diabetes had a higher BMD, they had an increased risk of non-vertebral fractures in unadjusted models (crude HR 1.61 [95% CI 1.05–2.46]), although the relationship was not significant after adjustment for age, BMI, BMD and other factors (HR 1.64 [0.93–2.90]) [8]. The Malmo study of middle-aged men (43.7 ± 6.6 years old) found an increased risk of low-energy fractures with diabetes (adjusted RR 2.38 [1.65–3.42]) [9]. Melton et al reported that men with diabetes had an increased risk of any fractures in models adjusted for age (RR 1.4 [1.3–1.6]) [10]. In the Tromso study, where vitamin D supplements and physical exercise were commonly seen, type 2 diabetes was not significantly associated with the risk of non-vertebral fracture in men (adjusted RR 1.21 [0.6–2.47]) [7].
In our study, men with diabetes had a higher risk of fracture at a given age and BMD, consistent with previous findings in this cohort and others [24]. These results suggest that BMD and FRAX (the fractures risk algorithm developed by the WHO) may underestimate the fracture risk in diabetic men. In this cohort of older men, the increased risk of fracture with diabetes, considering all diabetic men as a group, was accounted for by worse physical performance and increased falls. Functional limitations and lower limb strength have been reported in diabetic patients, which can be a consequence of increased muscle protein breakdown and fat infiltration [25–27]. However, in diabetic men who were using insulin, an increased risk of fracture persisted even after taking into account physical performance, falls and other fracture-related risk factors. Some previous studies have also reported an increased risk of fracture in those using insulin. Most of these studies combined men and women together in their analyses [7, 10, 28], but one Italian study reported an increased risk in men separately [29].
Our findings are consistent with several potential mechanisms of increased fracture risk in individuals with diabetes. First, patients receiving insulin have a higher propensity for hypoglycaemic events, which could increase the risk of falls. Those taking insulin may also have more severe disease or a longer disease duration and are thus likely to have microvascular involvement and peripheral neuropathy, which increases the prevalence of chronic gait/balance impairments and subsequently falls. Not unexpectedly, we found that diabetic men using insulin reported more falls than healthy men, similar to reports in diabetic women [2]. Insulin users are usually more likely to have chronic hyperglycaemia, which may impair bone quality in the diabetic skeleton [30]. In fact, although areal BMD may be higher in patients with type 2 diabetes compared with healthy individuals, a previous study in the MrOS cohort found that the bone structure of diabetic patients may have an overall decreased strength and lowered resistance to fractures [31]. In addition, high glucose levels produce a larger concentration of advanced glycation end-products in the bone, which have been associated with low bone strength in post mortem studies [32] and with fracture in diabetic patients [33]. Therefore, with compromised bone quality, low-trauma events may increase fracture risk.
In addition, other factors related to type 2 diabetes such as the microvascular and macrovascular complications, oxidative stress, renal dysfunction, elevated renal calcium loss and persistent inflammation present in type 2 diabetes may further impair bone health and increase fracture risk. Interestingly, in the Blue Mountain Study in Australia, which was specifically designed to determine the risk factors for eye disease in diabetic patients, the risk of fractures in insulin users was strongly influenced by retinopathy: their poor vision caused an increased risk of falls [34]. Poor vision may also be a marker for a longer duration of diabetes, more severe diabetes or poorer glycaemic control. In the Blue Mountain Study, insulin users had a 2.7 RR of dying (95% CI 1.7, 4.4) during a 5 year follow-up [34].
In our effort to identify the variables contributing to the higher risk of fracture among MrOS men with insulin-treated diabetes, we considered a range of risk factors for fracture that are also associated with diabetes, including more frequent falls, poorer physical performance and vision, reduced renal function and a history of cardiovascular events. However, these risk factors accounted for only a small portion of the association between insulin-treated diabetes and fracture risk in our models.
Risk factors for fracture in men with diabetes, considered as a separate group, included lower BMD and more frequent falls. In the same subgroup, an increased risk of fractures was observed in those treated with sulfonylureas, medications known to cause hypoglycaemic events and in turn falls [35]. Fracture risk appeared to be similarly elevated with insulin use, but the association was not statistically significant and, with limited numbers of participants in this category, the CIs were wide.
Our results suggest that diabetic patients and caregivers should pay more attention to preventive measures to avoid falls, particularly in patients treated with insulin and sulfonylureas. Our study did not find any protective effect of metformin on fractures, a finding confirmed by other authors [7, 10]. There was also no increased risk with TZD use. Reports from clinical trials have found an increased fracture risk with TZD use in women but not men [36]. As already reported [8], patients with IFG did not have an increased risk of fractures, implying that mild hyperglycaemia does not predict bone health.
In our study, we have investigated for the first time risk of fractures in a well-characterised cohort of elderly men with a long follow-up, one notable study strength. We lack information, however, on diabetes duration, HbA1c levels and peripheral nerve function. Without HbA1c or OGTT data, diabetes may have been underdiagnosed. Diabetes was determined by fasting glucose levels as well as self-report, but some men with undiagnosed diabetes may have been misclassified as not having diabetes. However, self-report is considered to be a valid method to detect diabetes [37, 38]. Study participants were community-dwelling volunteers who were ambulatory and mainly white, and our results may not be applicable to the broader population of older men. Finally, we cannot exclude that diabetic patients on insulin could have been affected by long-standing type 1 diabetes. We think that this is very unlikely since, in general, type 1 diabetes is a rare condition that dramatically increases the risk of cardiovascular diseases, and only 40% of patients survive more than 40 years of disease [39–41]. Men with type 1 diabetes who do survive to older age are often in poor health. Many are no longer living in the community, and those who are would be unlikely to volunteer for a study such as the MrOS.
Our findings indicate that the risk of non-vertebral fracture is 30% higher in men with diabetes for a given BMD. Men who take insulin have more than double the risk of fractures. Taken together with previous findings in women, our findings highlight the importance of diabetes as a risk factor for fractures, and underscore the importance of preventive measures for diabetic patients receiving insulin.
Abbreviations
- BMD:
-
Bone mineral density
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration
- DXA:
-
Dual energy x-ray absorptiometry
- IFG:
-
Impaired fasting glucose
- MrOS:
-
Osteoporotic Fractures in Men
- PASE:
-
Physical Activity Scale for the Elderly
- TZDs:
-
Thiazolidinediones
References
Schwartz AV, Sellmeyer DE, Ensrud KE et al (2001) Older women with diabetes have an increased risk of fracture: a prospective study. J Clin Endocrinol Metab 86:32–38
Bonds DE, Larson JC, Schwartz AV et al (2006) Risk of fracture in women with type 2 diabetes: the Women's Health Initiative Observational Study. J Clin Endocrinol Metab 91:3404–3410
Nicodemus KK, Folsom AR (2001) Type 1 and type 2 diabetes and incident hip fractures in postmenopausal women. Diabetes Care 24:1192–1197
Janghorbani M, van Dam RM, Willett WC, Hu FB (2007) Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol 166:495–505
Vestergaard P (2007) Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes—a meta-analysis. Osteoporos Int 18:427–444
Isidro ML, Ruano B (2010) Bone disease in diabetes. Curr Diabetes Rev 6:144–155
Ahmed LA, Joakimsen RM, Berntsen GK, Fonnebo V, Schirmer H (2006) Diabetes mellitus and the risk of non-vertebral fractures: the Tromso study. Osteoporos Int 17:495–500
de Liefde I, van der Klift M, de Laet CE, van Daele PL, Hofman A, Pols HA (2005) Bone mineral density and fracture risk in type-2 diabetes mellitus: the Rotterdam Study. Osteoporos Int 16:1713–1720
Holmberg AH, Johnell O, Nilsson PM, Nilsson J, Berglund G, Akesson K (2006) Risk factors for fragility fracture in middle age. A prospective population-based study of 33,000 men and women. Osteoporos Int 17:1065–1077
Melton LJ 3rd, Leibson CL, Achenbach SJ, Therneau TM, Khosla S (2008) Fracture risk in type 2 diabetes: update of a population-based study. J Bone Miner Res 23:1334–1342
Blank JB, Cawthon PM, Carrion-Petersen ML et al (2005) Overview of recruitment for the Osteoporotic Fractures in Men study (MrOS). Contemp Clin Trials 26:557–568
Orwoll E, Blank JB, Barrett-Connor E et al (2005) Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study – a large observational study of the determinants of fracture in older men. Contemp Clin Trials 26:569–585
American Diabetes Association (2012) Standards of medical care in diabetes – 2012. Diabetes Care 35(Suppl 1):S11–S63
Lewis CE, Ewing SK, Taylor BC et al (2007) Predictors of non-spine fracture in elderly men: the MrOS study. J Bone Miner Res 22:211–219
Mackey DC, Lui LY, Cawthon PM et al (2007) High-trauma fractures and low bone mineral density in older women and men. JAMA 298:2381–2388
Sanders KM, Pasco JA, Ugoni AM et al (1998) The exclusion of high trauma fractures may underestimate the prevalence of bone fragility fractures in the community: the Geelong Osteoporosis Study. J Bone Miner Res 13:1337–1342
Washburn RA, Smith KW, Jette AM, Janney CA (1993) The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol 46:153–162
Pahor M, Chrischilles EA, Guralnik JM, Brown SL, Wallace RB, Carbonin P (1994) Drug data coding and analysis in epidemiologic studies. Eur J Epidemiol 10:405–411
Teng EL, Chui HC (1987) The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry 48:314–318
Fried LP, Tangen CM, Walston J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol 56:M146–M156
Ensrud KE, Ewing SK, Cawthon PM et al (2009) A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriatr Soc 57:492–498
Ray WA, Griffin MR, Schaffner W, Baugh DK, Melton LJ 3rd (1987) Psychotropic drug use and the risk of hip fracture. N Engl J Med 316:363–369
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Schwartz AV, Vittinghoff E, Bauer DC et al (2011) Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA 305:2184–2192
De Rekeneire N, Resnick HE, Schwartz AV et al (2003) Diabetes is associated with subclinical functional limitation in nondisabled older individuals: the Health, Aging, and Body Composition study. Diabetes Care 26:3257–3263
Barzilay JI, Cotsonis GA, Walston J et al (2009) Insulin resistance is associated with decreased quadriceps muscle strength in nondiabetic adults aged > or =70 years. Diabetes Care 32:736–738
Schafer AL, Vittinghoff E, Lang TF et al (2010) Fat infiltration of muscle, diabetes, and clinical fracture risk in older adults. J Clin Endocrinol Metab 95:E368–E372
Bazelier MT, Gallagher AM, van Staa TP et al (2012) Use of thiazolidinediones and risk of osteoporotic fracture: disease or drugs? Pharmacoepidemiol Drug Saf 21:507–514
Monami M, Cresci B, Colombini A et al (2008) Bone fractures and hypoglycemic treatment in type 2 diabetic patients: a case-control study. Diabetes Care 31:199–203
Huang S, Kaw M, Harris MT et al (2010) Decreased osteoclastogenesis and high bone mass in mice with impaired insulin clearance due to liver-specific inactivation to CEACAM1. Bone 46:1138–1145
Petit MA, Paudel ML, Taylor BC et al (2010) Bone mass and strength in older men with type 2 diabetes: the Osteoporotic Fractures in Men Study. J Bone Miner Res 25:285–291
Yamaguchi T, Sugimoto T (2011) Bone metabolism and fracture risk in type 2 diabetes mellitus. Endocr J 58:613–624 (Review)
Schwartz AV, Garnero P, Hillier TA et al (2009) Pentosidine and increased fracture risk in older adults with type 2 diabetes. J Clin Endocrinol Metab 94:2380–2386
Ivers RQ, Cumming RG, Mitchell P, Peduto AJ, Blue Mountains Eye Study (2001) Diabetes and risk of fracture: The Blue Mountains Eye Study. Diabetes Care 24:1198–1203
Cefalu CA, Cefalu WT (2005) Controlling hypoglycemia in type 2 diabetes: which agent for which patient? J Fam Pract 54:855–862
Kahn SE, Zinman B, Lachin JM et al (2008) Rosiglitazone associated fractures in type 2 diabetes: an analysis from ADOPT. Diabetes Care 31:845–851
Schneider AL, Pankow JS, Heiss G, Selvin E (2012) Validity and reliability of self-reported diabetes in the atherosclerosis risk in communities study. Am J Epidemiol 176:738–743
Margolis KL, Lihong Q, Brzyski R et al (2008) Women Health Initiative Investigators. Validity of diabetes self-reports in the Women's Health Initiative: comparison with medication inventories and fasting glucose measurements. Clin Trials 5:240–247
Sun JK, Keenan HA, Cavallerano JD et al (2011) Protection from retinopathy and other complications in patients with type 1 diabetes of extreme duration: the Joslin 50-year medalist study. Diabetes Care 34:968–974
Bain SC, Gill GV, Dyer PH, Jones AF et al (2003) Characteristics of type 1 diabetes of over 50 years duration (the Golden Years Cohort). Diabet Med 20:808–811
Laing SP, Swerdlow AJ, Slater SD et al (2003) Mortality from heart disease in a cohort of 23,000 patients with insulin-treated diabetes. Diabetologia 46:760–765
Acknowledgements
The authors wish to thank C. C. Dant of Medcom Consulting for his expert assistance preparing this manuscript. The authors represent the Osteoporotic Fractures in Men (MrOS) research group.
Funding
The Osteoporotic Fractures in Men (MrOS) study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute on Aging (NIA), the National Center for Research Resources (NCRR) and NIH Roadmap for Medical Research under the following grant numbers: U01 AR45580, U01 AR45614, U01 AR45632, U01 AR45647, U01 AR45654, U01 AR45583, U01AG18197, U01-AG027810, and UL1 RR024140. Glucose measurements were supported by a grant from the American ADA (1-04-JF-46, Strotmeyer ES).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
NN was involved in the concept, in data interpretation and in writing the manuscript. KEE and ESS were involved in the concept and design of the study, the acquisition and interpretation of data and the critical review of the paper for important intellectual content. ARH, DES, TLD, EB-C, DCB, DMB, ESO and SRC took part in the acquisition and interpretation of the data and in revising the article for important intellectual content. LP was involved in data acquisition and analysis and in revising the article. AVS is the guarantor of the study and made substantial contributions to the conception and design of the study, to the analysis and interpretation of the data, and to revising the article critically for important intellectual content. All authors gave their approval of the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Napoli, N., Strotmeyer, E.S., Ensrud, K.E. et al. Fracture risk in diabetic elderly men: the MrOS study. Diabetologia 57, 2057–2065 (2014). https://doi.org/10.1007/s00125-014-3289-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-014-3289-6