Abstract
The aim of this study was to determine the association between type-2 diabetes mellitus (DM), BMD and fractures in 6,655 men and women aged 55 years and over from the Rotterdam Study. We compared subjects with type-2 DM to subjects without DM. Additionally, subset analyses were performed, dividing subjects on the basis of the glucose tolerance test into already treated DM, newly diagnosed DM, impaired glucose tolerance (IGT) and normal glucose tolerance (NGT, reference). Femoral neck and lumbar spine BMD were measured using DEXA. Nonvertebral fracture ascertainment was performed using an automated record system involving GPs and local hospitals. Although subjects with DM had higher BMD, they had an increased nonvertebral fracture risk: hazard ratio (HR) 1.33 (1.00–1.77). In subset analysis, the increased fracture risk appeared restricted to treated DM subjects only: HR 1.69 (1.16–2.46). Subjects with IGT had a higher BMD, but contrary to treated DM, they had a lower fracture risk: HR 0.80 (0.63–1.00). In conclusion, subjects with type-2 DM and IGT both have a higher BMD. Whereas, subjects with IGT have a decreased fracture risk, subjects with DM (primarily those with already established and treated DM) had an increased fracture risk, probably due to long-term complications associated with DM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well known that insulin plays an important role in glucose metabolism, since it is necessary for the transport of glucose into the cell. Failures in the insulin pathway result in diabetes mellitus (DM). DM is a metabolic disease characterized by hyperglycemia, resulting in a long-term damage, dysfunction and failure of various organs. The majority of subjects with DM can be divided into two types, where type-1 DM is caused by a deficiency of insulin secretion, and type-2 DM is the result of resistance to insulin and an inadequate compensatory insulin secretion response to glucose [1]. Besides the role of insulin in glucose metabolism, it is thought that insulin also has an anabolic effect on bone, resulting in a higher bone mineral density (BMD) [2,3]. Therefore, diabetes mellitus has become a topic of interest in bone research.
Previous studies have shown that subjects with type-1 DM, probably as a result of insulin deficiency, have a decreased BMD as compared with subjects without type-1 DM [4–6]. With regard to the association between BMD and type-2 DM, some conflicting results have been reported. We and others observed an increased BMD in subjects with type-2 DM [5,7–10].
On the other hand, some studies reported a decreased BMD in subjects with type-2 DM, whilst others reported no association at all [11–17]. Also, uncertainty exists concerning the association between type 2-DM and fractures. Previously, we reported a decreased risk of prevalent fractures in the preceding 5 years in subjects with DM [8]. This seems in line with the higher BMD found in type-2 DM in our study [8]. However, in the Study of Osteoporotic Fractures (SOF), an increased risk of incident fractures in women with known DM was observed [10]. The results obtained in the SOF study were supported by others, while opposite findings were also reported and some studies found no association at all [8, 10,18–22].
In the present study we compared BMD and incident nonvertebral fracture risk in a large prospective cohort study of men and women who were stratified according to different levels of insulin resistance.
Methods
The Rotterdam study
The Rotterdam Study is a prospective population-based cohort study of men and women aged 55 years and over and has the objective of investigating the incidence of, and risk factors for, chronic disabling diseases. Both the rationale and the study design have been described previously [23]. The focus of the Rotterdam Study is on neurologic, cardiovascular, ophthalmologic and locomotor diseases. All 10,275 inhabitants of Ommoord, a district in Rotterdam, the Netherlands, were invited to participate. Of these, 7,983 (4,878 women) participated in the study (resulting in a response rate of 78%). The Medical Ethics Committee of the Erasmus Medical Centre has approved the Rotterdam Study, and informed consent was obtained.
Measurements
Baseline home interview
Between 1990 and 1993, a baseline home interview on medical history, risk factors for chronic diseases and medication use, including the use of thiazides or loop diuretics, was taken by trained interviewers.
Impairment in daily activities was assessed using a questionnaire adapted from the Stanford Health Assessment Questionnaire. Lower limb disability was calculated by the average scores for rising, walking, bending and getting out of a car. The score ranged from 0 to 3, where 0 indicated no impairment and 3 indicated no ability to do the activities. Falling frequency was recorded as “never,” “less than once a month,” and “more than once a month.” Smoking habits were coded as “current,” “former” and “never.” To have information about previous fractures, participants were asked if they had experienced at least one nonvertebral fracture in the preceding 5 years.
Clinical examination
Subsequently, participants were invited to the research center for clinical examination. Height and weight were measured with indoor clothing and no shoes. Body mass index (BMI) was calculated as weight in kg/height in m2. Visual acuity of both eyes was measured at a 3-m distance using the Lighthouse Distance Acuity Test. To evaluate best-corrected visual acuity, optimal refraction was obtained subjectively after objective autorefraction [24]. The best visual acuity of one of the eyes was used to compare the visual acuity between subjects. In serum of the participants, creatinine was measured using standard laboratory methods.
Classification of type-2 diabetes mellitus
At the research center, all participants, except those on anti-diabetic medication, underwent an oral glucose tolerance test (OGTT) with a 37.5% oral glucose solution (75 g of glucose) in a non-fasting state. Both before and 2 h after the glucose solution was administered, blood samples were drawn by venepuncture and the serum glucose levels were measured in both samples using the glucose hexokinase method. Serum insulin levels were measured by radioimmunoassay (MedGenix Diagnostics, Brussels, Belgium) in the post-load serum only. Subjects were classified as having DM if they used anti-diabetic medication or when the pre-load or post-load serum glucose levels were at or above 11.1 mmol/l. Subjects with serum glucose levels (pre- or post-load) lower than 11.1 mmol/l were classified as non-diabetics. To restrict the analysis to subjects with type-2 DM, those who reported having DM at or before the age of 30 were excluded.
Sub-stratification for level of insulin resistance
To determine the effect of different levels of insulin resistance and the effects of long-term DM with its associated complications, subset analyses were performed. The following four groups were defined: subjects with already treated DM, subjects with newly diagnosed DM, subjects with impaired glucose tolerance (IGT), having a pre-load or post-load serum glucose level from 7.8 mmol/l to 11.1 mmol/l, and subjects with normal glucose tolerance (NGT), who had a serum glucose level lower than 7.8 mmol/l. These classifications are based on World Health Organization (WHO) criteria [25–27].
BMD measurement
BMD of the femoral neck and lumbar spine was measured by dual-energy X-ray absorptiometry (DEXA), using a Lunar DPX-L densitometer (Lunar Radiation Corporation, Madison, WI, USA) as described previously [28].
Follow-up procedure
All events, including nonvertebral fractures and death were reported by general practitioners (GPs) in the research area (covering 80% of the cohort) by means of a computerized system. Information from GPs outside the research area was obtained by regular checking of patient records by research physicians. All reported events were verified by two trained research physicians, who independently reviewed and coded the information. Subsequently, all coded events were reviewed by a medical expert for final classification. Subjects were followed from their baseline visit until either death, first nonvertebral fracture or until January 1, 2000, whichever occurred first.
Population for analyses of type-2 diabetes mellitus
Of all 7,983 participants from the Rotterdam Study, 177 (2.2%) were excluded from the analyses since no informed consent was obtained for follow-up data registration. Data on the use of anti-diabetic medication and data of pre-load or post-load OGTT were available for 6,655 individuals, of which 5,754 subjects had data available on femoral neck and lumbar spine BMD. According to the glucose tolerance test, 807 subjects were classified as having DM. However, to restrict the analyses to type-2 DM, 15 subjects with an onset of diabetes at or before the age of 30 were excluded, leaving 792 subjects with DM for the analyses.
Population for subset analyses of level of insulin resistance
The numbers and percentages of subjects with treated DM, subjects with newly diagnosed DM, subjects with IGT and subjects with NGT are shown in Fig. 1. Half of the subjects with DM were newly diagnosed at the beginning of the study.
No information on the use of anti-diabetic medication was available for 14 subjects with DM. Therefore, these subjects could not be separated into one of the groups for the subset analyses and were excluded in these analyses. Of the 6,641 individuals in the subset analyses, there were data available of femoral neck and lumbar spine BMD for 5,746 subjects.
Statistical analysis
At first, analyses were performed comparing all subjects with type-2 DM to subjects without DM. To define differences in baseline characteristics between subjects with DM and without DM, we used a chi-square test for categorical variables and a student- t -test for continuous variables.
Differences in BMD, as measured at the femoral neck and lumbar spine were evaluated using analysis of variance (ANOVA). Analyses were performed crude, adjusting for age and gender and finally for age, gender, BMI, lower-limb disability, smoking, and use of either loop or thiazide diuretics at baseline. Because the prevalence of the use of hormonal replacement therapy or systemic corticosteroids at baseline was low, we did not adjust for them in the analyses. Analyses were repeated stratifying for gender.
To investigate the relation between type-2 DM and nonvertebral fractures, a Cox proportional hazard regression model was used. To express these associations, hazard ratios were calculated with the corresponding 95% confidence intervals. In the analyses, only nonvertebral fractures, including hip and wrist fractures, were studied. First the analyses were performed crude, then adjusted for age and gender, and finally adjustments were made for age, gender, BMI, smoking, serum creatinine, visual acuity, falling frequency and lower limb disability. In addition, analyses were repeated with an additional adjustment for femoral neck BMD.
Following the analyses in which we compared subjects with and without DM, we performed the same analyses using a different classification. Subjects with DM were sub-classified into subjects with previously known and newly diagnosed diabetes, whereas, subjects without DM were sub-classified into subjects with IGT and with NGT, using the latter category as reference. In addition, we repeated these analyses stratifying for gender. SPSS 11.0 for windows was used for all analyses.
Results
Type-2 diabetes mellitus
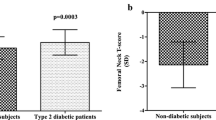
The baseline characteristics of subjects with and without type-2 DM are shown in Table 1. Men and women were equally distributed between groups. As expected, subjects with DM were significantly older, had a higher BMI and more comorbidity as compared with subjects without DM. The post-load serum insulin level in subjects with DM was considerably higher. Fig. 2 shows mean values of BMD, as measured at femoral neck and lumbar spine according to diabetic status, with adjustment for the full model. We did not include the use of hormonal replacement therapy or systemic corticosteroids in this full model, because of the low prevalence, and adjustment did not influence the results. At both sites, after adjustment for potential confounders, BMD was substantially higher in subjects with DM as compared with subjects without DM. Similar significant results were observed when analyses were repeated stratifying for gender (data not shown).
The fracture-risk analyses are based on follow-up data collected from baseline (1990–1993) until January 1, 2000, with an average follow-up period of 6.8 years (SD 2.3 years). During follow-up, 771 subjects suffered at least one nonvertebral fracture. In total, 25 (8.1%) men and 79 (16.4%) women with DM suffered at least one nonvertebral fracture, including nine (2.9%) hip and two (0.6%) wrist fractures in men and 28 (5.8%) hip and 23 (4.8%) wrist fractures in women. In contrast, 143 (6.0%) men and 525 (5.1%) women without DM suffered at least one nonvertebral fracture, including 41 (1.7%) hip and 21 (0.9%) wrist fractures in men and 137 (3.9%) hip and 158 (4.5%) wrist fractures in women.
In the fracture-risk analyses—in which subjects with type-2 DM, men and women combined are compared with subjects without DM, subjects with DM had an increased risk of overall nonvertebral fractures, despite their higher BMD values (Table 2). There was also a similar but nonsignificant trend observed for the hip and wrist fracture risks. When we stratified by gender, we observed a comparable trend as well, although some analyses were not significant, especially in men, due to the low fracture numbers when stratified (Table 2).
Level of insulin resistance
In order to evaluate the effect of different levels of insulin resistance and long-term DM, we repeated all these analyses by comparing subjects with treated DM, subjects with newly diagnosed DM, subjects with IGT and subjects with NGT.
The baseline characteristics of subjects with treated DM, newly diagnosed DM, IGT and NGT are shown in Table 3. Subjects with treated DM were older and had more comorbidity than subjects with newly diagnosed DM, IGT or NGT. Subjects with IGT had less comorbidity than subjects with newly diagnosed DM, but more comorbidity than subjects with NGT. Insulin levels, not measured in subjects with anti-diabetic medication, were the highest in subjects with newly diagnosed DM and the lowest in subjects with NGT.
Table 4 shows average femoral neck and lumbar spine BMD values according to the level of insulin resistance, using subjects with NGT as a reference. Subjects with treated DM and newly diagnosed DM had a substantially higher BMD measurement at both sites compared with subjects with NGT, independent of potential confounders. The BMD in subjects with IGT was lower than the BMD in treated DM, but it was higher compared with subjects with NGT. Analyses stratified by gender yielded similar results (data not shown).
The fracture risks in subjects with treated DM, newly diagnosed DM and IGT as compared with subjects with NGT are shown in Table 5. The increased fracture risk, which was observed in the overall analyses, appeared to be restricted to subjects with treated DM. Subjects with newly diagnosed DM were not at an increased risk for any of the investigated fracture types. In contrast, subjects with IGT have a 20–40% decreased fracture risk independent of potential confounders and BMD. Results did not substantially differ when stratifying for gender (data not shown).
Discussion
The results of our study confirm earlier observations that subjects with type-2 DM have a higher BMD. Despite this higher BMD, an increased fracture risk was observed. More detailed analyses revealed that the increase in fracture risk was restricted to subjects with already established and treated DM only. Subjects with IGT also had a higher BMD, but in contrast to subjects with treated DM, these subjects had a significantly decreased fracture risk.
To our knowledge, this is the first study that investigates the association between BMD, fracture risk and different levels of insulin resistance. The different levels of insulin resistance in the subgroups in our study are reflected by the different levels of serum insulin. Tripathy et al. also observed a progressive increase in insulin resistance between subjects with NGT, IGT, mild DM and DM, which supports that our sub-classifications indeed reflect different levels of insulin resistance [29].
Recent literature suggests that an association between insulin levels, BMD and fractures might exist [2,30–32]. It is hypothesized that insulin has an anabolic effect on bone formation by interacting with the IGF-1 receptor, which is present on osteoblasts in bone, resulting in higher bone mass, which consequently might result in a reduced fracture risk [2,3].
In our BMD analyses, we indeed observed a higher BMD in subjects with DM, with the highest BMD in subjects with DM and subjects with IGT, while the lowest BMD was observed in subjects with NGT. These BMD results were independent of several confounders such as age, gender, BMI, lower limb disability, smoking, and use of either loop or thiazide diuretics, suggesting that these factors did not play an important role in explaining the observed association. Aortic calcifications and osteoarthritis could have influenced BMD measurements at the lumbar spine. However, this would not explain the higher BMD at the femoral neck.
Our BMD results of subjects with type-2 DM confirm other studies [5,7–10]. Some other investigators observed different BMD results in subjects with DM [11–17]. For instance, Levin et al. reported a decreased BMD in adult onset diabetes [11]. However, they did not describe which criteria were used to separate adult onset diabetes from juvenile onset. It is likely that they included subjects with type-1 DM in the adult onset DM group, considering the age distribution and the percentage of insulin-treated subjects.
The results of BMD in subjects with newly diagnosed DM and subjects with IGT could not be compared with other studies, because to our knowledge no other study has yet investigated these associations.
In the analyses, we observed that the increased fracture risk found in subjects with DM was restricted to subjects with already established and treated DM only. This result suggests that an association exists between the duration of the disease and the risk of fractures.
One explanation for this observed increased fracture risk in treated DM is that, due to long-term DM, subjects with established and treated DM suffer more from disease-related complications, such as poor balance and vision, cardiovascular disease and peripheral neuropathy, which might increase falling frequency [33]. In our fracture-risk analyses, we did adjust for falling frequency. However, this variable was only measured at baseline, and, therefore, the confounding effect could not be entirely ruled out.
A second explanation is glycation of collagen in bone. Hyperglycemia instigates a higher concentration of advanced glycation end products in collagen, which might cause a decrease in bone strength, resulting in an increased fracture risk [34–36]. Given the fact that glycation might increase with the duration of the disease, this would explain that especially subjects with already established and treated DM have an increase in fracture risk.
In contrast to subjects with already treated DM, we observed a significantly decreased fracture risk in subjects with IGT, which is in line with the hypothesis that insulin has an anabolic effect on bone, resulting in a lower fracture risk. Subjects with IGT already have an increased insulin resistance, displayed by a higher serum insulin concentration compared with subjects with NGT, but they do not yet suffer as much from disease-related complications as subjects with DM do. In addition, one could hypothesize that the level and the duration of hyperglycemia is less than in subjects with treated DM, which might result in less glycation of collagen in bone than in subjects with already treated DM.
However, if the increased BMD is the most important factor for the reduced fracture risk, we expected that adjustment for BMD would have had a large effect on this risk [2,3]. However, the fracture risk was only mildly affected by the adjustment for BMD, suggesting that insulin might also have other effects that influence bone fragility. Therefore, further studies are needed to establish the effect of hyperinsulinemia on bone quality.
The increased fracture risk results seen in our study are in agreement with findings of other previous studies [10,18–20]. A study of The Nord-Trøndelag Health Survey reported an increased hip fracture risk in women with type-2 DM known for more than 5 years [18]. Schwartz et al., in the SOF study, reported an increase of nonvertebral fracture risk in women with DM, both insulin and non-insulin treated [10]. On the other hand, some studies found other results than ours [8, 21,22]. We previously reported a decreased risk of prevalent nonvertebral fractures, occurring in the preceding 5 years before the baseline visit, in subjects with DM [8]. However, it is very likely that these subjects who were thought to have DM had IGT instead of DM, at the time they suffered a fracture. Therefore, the results of the previous study are not in contrast to the findings of the present study. Health et al., studying fractures occurring before diagnosis of DM, observed a decreased fracture risk in subjects with DM as well [21]. In contrast, they also reported a decreased fracture risk after the diagnosis. However, they did not adjust for BMI and did not investigate the association between the duration of the disease and the fracture risk.
Although our study is a large population-based study, we did not perform a fasting OGTT but used the 2-h post-glucose level as recommended by the WHO [25]. It appears that the 2-h post-load glucose is the best indicator of the presence of DM [37–39]. There is also evidence that a non-fasting OGTT provides similar results as a fasting OGTT [40]. When we performed in 69 participants both the fasting and non-fasting OGTT, glucose levels were comparable [38]. Furthermore, the prevalence of DM in this population is equivalent with the prevalence in the Dutch population [41]. Nevertheless, it could still be possible that some subjects were misclassified, but this is equally likely with subjects with NGT, which would only result in an underestimation of the observed effects.
In conclusion, the results of our study confirm earlier observations that subjects with type-2 DM have a higher BMD. Despite this higher BMD, an increased fracture risk was observed. More detailed analyses revealed that the increase in fracture risk was restricted to subjects with already established and treated DM. Subjects with IGT had a higher BMD as well, but in contrast to subjects with treated DM, these subjects had a significantly lower fracture risk. The results suggest that insulin can affect BMD and fracture risk, but in the long-term, the fracture risk increases, probably due to complications and general comorbidity as a result of long-term DM.
References
Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (1997). Diabetes Care 20:1183–1197
Yano H, Ohya K, Amagasa T (1994) Effects of insulin on in vitro bone formation in fetal rat parietal bone. Endocr J 41:293–300
Mohan S, Richman C, Guo R, Amaar Y, Donahue LR, Wergedal J, Baylink DJ (2003) Insulin-like growth factor regulates peak bone mineral density in mice by both growth hormone-dependent and -independent mechanisms. Endocrinology 144:929–936
Kayath MJ, Tavares EF, Dib SA, Vieira JG (1998) Prospective bone mineral density evaluation in patients with insulin-dependent diabetes mellitus. J Diabetes Complications 12:133–139
Christensen JO, Svendsen OL (1999) Bone mineral in pre- and postmenopausal women with insulin-dependent and non-insulin-dependent diabetes mellitus. Osteoporos Int 10:307–311
Tuominen JT, Impivaara O, Puukka P, Ronnemaa T (1999) Bone mineral density in patients with type 1 and type 2 diabetes. Diabetes Care 22:1196–1200
Bauer DC, Browner WS, Cauley JA, Orwoll ES, Scott JC, Black DM, Tao JL, Cummings SR (1993) Factors associated with appendicular bone mass in older women. The Study of Osteoporotic Fractures Research Group. Ann Intern Med 118:657–665
van Daele PL, Stolk RP, Burger H, Algra D, Grobbee DE, Hofman A, Birkenhager JC, Pols HA (1995) Bone density in non-insulin-dependent diabetes mellitus. The Rotterdam Study. Ann Intern Med 122:409–414
Lunt M, Masaryk P, Scheidt-Nave C, Nijs J, Poor G, Pols H, Falch JA, Hammermeister G, Reid DM, Benevolenskaya L, Weber K, Cannata J, O’Neill TW, Felsenberg D, Silman AJ, Reeve J (2001) The effects of lifestyle, dietary dairy intake and diabetes on bone density and vertebral deformity prevalence: the EVOS study. Osteoporos Int 12:688–698
Schwartz AV, Sellmeyer DE, Ensrud KE, Cauley JA, Tabor HK, Schreiner PJ, Jamal SA, Black DM, Cummings SR (2001) Older women with diabetes have an increased risk of fracture: a prospective study. J Clin Endocrinol Metab 86:32–38
Levin ME, Boisseau VC, Avioli LV (1976) Effects of diabetes mellitus on bone mass in juvenile and adult-onset diabetes. N Engl J Med 294:241–245
Ishida H, Seino Y, Matsukura S, Ikeda M, Yawata M, Yamashita G, Ishizuka S, Imura H (1985) Diabetic osteopenia and circulating levels of vitamin D metabolites in type 2 (noninsulin-dependent) diabetes. Metabolism 34:797–801
Giacca A, Fassina A, Caviezel F, Cattaneo AG, Caldirola G, Pozza G (1988) Bone mineral density in diabetes mellitus. Bone 9:29–36
Weinstock RS, Goland RS, Shane E, Clemens TL, Lindsay R, Bilezikian JP (1989) Bone mineral density in women with type II diabetes mellitus. J Bone Miner Res 4:97–101
Okuno Y, Nishizawa Y, Sekiya K, Hagiwara S, Miki T, Morii H (1991) Total and regional bone mineral content in patients with non-insulin dependent diabetes mellitus. J Nutr Sci Vitaminol (Tokyo) 37 [Suppl]:S43–49
Wakasugi M, Wakao R, Tawata M, Gan N, Koizumi K, Onaya T (1993) Bone mineral density measured by dual energy X-ray absorptiometry in patients with non-insulin-dependent diabetes mellitus. Bone 14:29–33
Sosa M, Dominguez M, Navarro MC, Segarra MC, Hernandez D, de Pablos P, Betancor P (1996) Bone mineral metabolism is normal in non-insulin-dependent diabetes mellitus. J Diabetes Complications 10:201–205
Forsen L, Meyer HE, Midthjell K, Edna TH (1999) Diabetes mellitus and the incidence of hip fracture: results from the Nord-Trondelag Health Survey. Diabetologia 42:920–925
Ivers RQ, Cumming RG, Mitchell P, Peduto AJ (2001) Diabetes and risk of fracture: The Blue Mountains Eye Study. Diabetes Care 24:1198–1203
Nicodemus KK, Folsom AR (2001) Type 1 and type 2 diabetes and incident hip fractures in postmenopausal women. Diabetes Care 24:1192–1197
Heath H 3rd, Melton LJ 3rd, Chu CP (1980) Diabetes mellitus and risk of skeletal fracture. N Engl J Med 303:567–570
Melchior TM, Sorensen H, Torp-Pedersen C (1994) Hip and distal arm fracture rates in peri- and postmenopausal insulin-treated diabetic females. J Intern Med 236:203–208
Hofman A, Grobbee DE, de Jong PT, van den Ouweland FA (1991) Determinants of disease and disability in the elderly: the Rotterdam Elderly Study. Eur J Epidemiol 7:403–422
Klaver CC, Wolfs RC, Vingerling JR, Hofman A, de Jong PT (1998) Age-specific prevalence and causes of blindness and visual impairment in an older population: the Rotterdam Study. Arch Ophthalmol 116:653–658
Diabetes mellitus. Report of a WHO Study Group (1985) World Health Organ Tech Rep Ser 727:1–113
Prevention of diabetes mellitus. Report of a WHO Study Group (1994) World Health Organ Tech Rep Ser 844:1–100
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15:539–553
Burger H, de Laet CE, van Daele PL, Weel AE, Witteman JC, Hofman A, Pols HA (1998) Risk factors for increased bone loss in an elderly population: the Rotterdam Study. Am J Epidemiol 147:871–879
Tripathy D, Carlsson M, Almgren P, Isomaa B, Taskinen MR, Tuomi T, Groop LC (2000) Insulin secretion and insulin sensitivity in relation to glucose tolerance: lessons from the Botnia Study. Diabetes 49:975–980
Reid IR, Evans MC, Cooper GJ, Ames RW, Stapleton J (1993) Circulating insulin levels are related to bone density in normal postmenopausal women. Am J Physiol 265:E655–659
Stolk RP, Van Daele PL, Pols HA, Burger H, Hofman A, Birkenhager JC, Lamberts SW, Grobbee DE (1996) Hyperinsulinemia and bone mineral density in an elderly population: The Rotterdam Study. Bone 18:545–549
Barrett-Connor E, Kritz-Silverstein D (1996) Does hyperinsulinemia preserve bone? Diabetes Care 19:1388–1392
Schwartz AV, Hillier TA, Sellmeyer DE, Resnick HE, Gregg E, Ensrud KE, Schreiner PJ, Margolis KL, Cauley JA, Nevitt MC, Black DM, Cummings SR (2002) Older women with diabetes have a higher risk of falls: a prospective study. Diabetes Care 25:1749–1754
Paul RG, Bailey AJ (1996) Glycation of collagen: the basis of its central role in the late complications of ageing and diabetes. Int J Biochem Cell Biol 28:1297–1310
Vashishth D, Gibson GJ, Khoury JI, Schaffler MB, Kimura J, Fyhrie DP (2001) Influence of nonenzymatic glycation on biomechanical properties of cortical bone. Bone 28:195–201
Wang X, Shen X, Li X, Agrawal CM (2002) Age-related changes in the collagen network and toughness of bone. Bone 31:1–7
Modan M, Halkin H, Karasik A, Lusky A (1984) Effectiveness of glycosylated hemoglobin, fasting plasma glucose, and a single post-load plasma glucose level in population screening for glucose intolerance. Am J Epidemiol 119:431–444
Stolk RP, Orchard TJ, Grobbee DE (1995) Why use the oral glucose tolerance test? Diabetes Care 18:1045–1049
Haeckel R, Wosniok W, Raber R, Janka HU (2003) Detecting type 2 diabetes by a single post-challenge blood sample. Clin Chem Lab Med 41:1251–1258
Coustan DR, Widness JA, Carpenter MW, Rotondo L, Pratt DC, Oh W (1986) Should the fifty-gram, one-hour plasma glucose screening test for gestational diabetes be administered in the fasting or fed state? Am J Obstet Gynecol 154:1031–1035
Ruwaard D, Feskens EJ (1993) Diabetes Mellitus. In Ruwaard D, Kramers PGN (eds) (1993) Volksgezondheid Toekomst Verkenning: De Gezondheidstoestand van de Nederlandse bevolking in de periode 1950–2010. Sdu Uitgeverij Plantijnstraat, Den Haag, pp 303–308
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Liefde, I.I., van der Klift, M., de Laet, C.E.D.H. et al. Bone mineral density and fracture risk in type-2 diabetes mellitus: the Rotterdam Study.. Osteoporos Int 16, 1713–1720 (2005). https://doi.org/10.1007/s00198-005-1909-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-005-1909-1