Abstract
Purpose of Review
Recently, the American Diabetes Association updated the 2024 guidelines for Standards of Care in Diabetes and recommend that a T-score of − 2.0 in patients with diabetes should be interpreted as equivalent to − 2.5 in people without diabetes. We aimed to evaluate the most recent findings concerning the bone mineral density (BMD)-derived T-score and risk of fractures related to osteoporosis in subjects with diabetes.
Recent Findings
The dual-energy X-ray absorptiometry (DXA) scan is the golden standard for evaluating BMD. The BMD-derived T-score is central to fracture prediction and signifies both diagnosis and treatment for osteoporosis. However, the increased fracture risk in diabetes is not sufficiently explained by the T-score, complicating the identification and management of fracture risk in these patients.
Summary
Recent findings agree that subjects with type 2 diabetes (T2D) have a higher T-score and higher fracture risk compared with subjects without diabetes. However, the actual number of studies evaluating the direct association of higher fracture risk at higher T-score levels is scant. Some studies support the adjustment based on the 0.5 BMD T-score difference between subjects with T2D and subjects without diabetes. However, further data from longitudinal studies is warranted to validate if the T-score treatment threshold necessitates modification to prevent fractures in subjects with diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes (T2D) and osteoporosis are two common and chronic diseases in the elderly population. The increased risk of fractures in subjects with type 1 diabetes (T1D) and T2D has been investigated for more than 30 years [1]. It is well established that the increased fracture risk exceeds what can be rationalized by a slightly lower bone mineral density (BMD) in T1D [1,2,3] and a paradoxically normal or higher BMD in subjects with T2D compared with subjects without diabetes [1]. However, BMD is an important tool in fracture risk stratification, and this far, the estimation of BMD by the dual-energy x-ray absorptiometry (DXA) remains the golden standard for diagnosing osteoporosis—also in subjects with T1D and T2D [4].
Conventional antiresorptive treatments are reported as effective in subjects with diabetes as in subjects without diabetes [5, 6]. However, the likelihood of being diagnosed with and treated for osteoporosis may be lower in those with diabetes [7, 8], which may be due to a relatively higher BMD. Numerous alternatives for assessing the fracture risk in subjects with diabetes have been suggested including novel measures and technologies such as the DXA-derived measures trabecular bone score (TBS) and hip structural analysis (HSA), high-resolution peripheral quantitative computed tomography (HRpQCT) measures, and microindentation, as well as stratifying according to more clinical characteristics by the fracture risk assessment tool (FRAX).
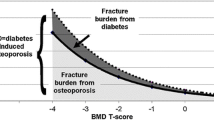
In 2011, Schwartz et al. assembled a review combining results from three prospective observational studies on fractures in subjects with and without diabetes [4]. The review concluded that at a given T-score or age, the 10-year probability of a hip or non-spine fracture was higher in subjects with T2D. Moreover, they concluded that the fracture risk in subjects without diabetes at T-score − 2.5 was similar to that of a subject with T2D at T-score − 2.0. These findings established the current debate suggesting an adjusted diagnostic and treatment threshold of T-score − 2.0 in subjects with diabetes.
The meta-analysis by Schwartz et al. [4] included only studies of subjects with T2D, and thus, the suggestion of a revised T-score cut-off was addressed to this group. However, the risk of fracture, hip fracture in particular, is vastly increased in subjects with T1D as well [9]. Due to the discrepancy of T-scores and fracture risk in T1D, secondary osteoporosis as a consequence of T1D has been incorporated into the FRAX tool [10]. Nonetheless, in Denmark and other countries, the T-score is the primary tool for evaluating the diagnosis of and treatment for osteoporosis. Mostly, FRAX is only recommended as a supplement if the clinician considers not to treat in spite of a low BMD [11, 12]; however, some countries have incorporated FRAX in the evaluation of treatment as well [13]. Unclarity remains upon the exact association between BMD T-score and fractures in T1D; however, on behalf of the Bone and Diabetes Working Group of IOF, Ferrari et al. have recommended a cut-off value at T-score − 2.0 in both T1D and T2D [14]. Most recently, the American Diabetes Association updated the 2024 guidelines for Standards of Care in Diabetes and recommended that a T-score of − 2.0 in people with diabetes should be interpreted as equivalent to − 2.5 [15].
In cohort studies and the aforementioned meta-analysis, the estimated fracture risk and BMD level is investigated in persons with and without diabetes. However, we speculated that the diabetes population may be significantly heterogeneous and so, we aimed to investigate 1) if and how the BMD level varies within the diabetes population and 2) whether the BMD in the full diabetes population is representative of the subpopulation that suffers osteoporotic fractures. To illuminate further the considerations of lowering the treatment and diagnostic T-score threshold for osteoporosis in persons with diabetes, we pose the following research question: at which BMD T-score do persons with diabetes suffer an osteoporotic fracture and does it differ from the background population?
We conducted a systematic review, exploring the recent evidence within the last 3 years including information on the BMD, T-score, and fracture risk in subjects with diabetes.
Methods
We conducted a systematic review based on the latest 3 years of findings applying a PIRO (Population, Index test, Reference standard and Outcomes) approach using the search string ((“diabetes mellitus”[MeSH Terms] OR “diabet*”[Text Word]) AND (“bone densit*”[Text Word] OR “bone mineral densit*”[Text Word] OR “bone density”[MeSH Terms] OR “absorptiometry, photon”[MeSH Terms] OR “absoptiometr*”[Text Word] OR “bone mineral content*”[Text Word] OR “BMC”[Text Word] OR “BMD”[Text Word] OR “dual-energy-x-ray”[Text Word] OR “dual-energy-x-ray”[Text Word] OR “dual-energy-x-ray”[Text Word] OR “dual-energy-x-ray”[Text Word] OR “dual-energy-x-ray”[Text Word]) AND (“osteoporo*”[Text Word] OR (“osteoporosis, postmenopausal”[MeSH Terms] OR “osteoporosis”[MeSH Terms]) OR (“fractures, bone”[MeSH Terms] OR “fractur*”[Text Word]) OR (“bone fragil*”[Text Word] OR “bone disease”[Text Word] OR “bone competence”[Text Word] OR “fracture risk”[Text Word]) OR (“fractures, bone”[MeSH Terms] OR “fractur*”[Text Word]))) AND (2020/1/1:2023/4/13[pdat]) in PubMed filtering results from 2020 to April 13 2023 with an updated search September 20 2023 and repeated the search in Embase using a database adapted search string (see supplemental material).
After removing duplicates, the combined results were evaluated for in- or exclusion by 2 independent blinded researchers (I.B. and R.V.). Conflicts were discussed and resolved between the two researchers, and in case of doubt, a third researcher (J.S-L.) was consulted for the final decision.
We only considered studies presenting clinical data on adult subjects with diabetes (either type 1 or type 2) including a control group in comparison. In addition, case-only studies (i.e., studies only presenting data on subjects with a fracture) were excluded and only studies with estimates (primary or secondary) on BMD, Z-scores, or T-scores and any fractures, and analysis of the association were considered for inclusion. All included studies were graded using the critical appraisal tools Newcastle-Ottawa Scale (NOS) for cohort studies and case-control studies [16], adapted NOS for cross-sectional studies [17], and AMSTAR-2 [18] and the Oxford Centre Evidence-based Medicine: Levels of Evidence 2009 [19].
In this systematic review, we did not perform a meta-analysis due to differences in study design, outcome, and BMD evaluation. However, as the primary aims in some studies did not meet the scope of this review, the comparisons relevant to our aims were not always made. In these five cases [20••, 21,22,23,24], we have used the data from the manuscripts to perform simple variance tests and t-tests by assumption of normality by use of Stata (R) software. By use of means and standard deviations, it was in some cases relevant to compute the 95% confidence interval (CI) by use of Excel(c) [24, 25]. These calculations can be found in the supplemental material. Below, means are represented as mean with standard deviation (SD) or 95% CI.
Results
The search yielded a total of 2182 hits, 691 results from PubMed and 1491 results from the Embase search. After manual removal of 606 duplicates, 1576 eligible hits remained for evaluation. One study was added from the updated search of September 2023 [26]. The selection process is presented in Fig. 1. We included 28 studies with information (either primary or secondary) on BMD/T-score of the lumbar spine (LS), femoral neck (FN), or total hip, and fractures in subjects with diabetes. However, four studies did not meet the criteria of a control group for comparison [27,28,29,30]; four studies did not allow for evaluation of BMD or T-score in the fracture risk estimates [31,32,33,34]; and five studies were excluded as they only included fracture cases (case-only studies) [26, 35,36,37,38]. An Australian cohort study [22] was excluded because the study population was contained within another study but restricted to subjects with an available calcaneal quantitative ultrasound [39]. These 14 studies and the reason for their exclusion can be found in the supplementary table. Consequently, 14 reports were included in the systematic review, in one of which two studies were reported [40•].
In the following, a summary of the results will be provided separated by study design.
Systematic Reviews with Meta-analyses
One systematic review was included. Koromani and colleagues included studies from 1986 to 2019 in their primary analysis and a sub-analysis of seven studies with individual BMD data available (n = 31,530) in the same period [41••]. The sub-analysis included data from large cohort studies: SOF [42], CaMos [43], MRCHIP [44], Osteolaus [45], and the Rotterdam study cohorts RSI, RSII, and RSIII [46]. The femoral neck (FN-BMD)-adjusted hazard ratio (HR) of incident non-vertebral fractures for subjects with T2D with no prevalent vertebral fracture (VF) was 1.24 (95% CI 1.09–1.40) compared with subjects without diabetes. Moreover, the FN-BMD-adjusted HR of incident non-vertebral fractures was 1.73 (95% CI 1.32–2.27) for subjects with T2D with prevalent VF compared to subjects without diabetes with prevalent VF. These results indicate that T2D is a risk factor for non-vertebral fracture independent of BMD, which implies that non-vertebral fracture risk is higher in DM at a given FN-BMD. Furthermore, the risk of incident non-vertebral fractures was elevated in subjects with T2D and normal BMD (HR 1.22 (95% CI 0.98–1.52)), higher in those with osteopenia (HR 1.28 (95% CI 1.08–1.52)) and not significantly different in those with osteoporosis (HR 1.04 (95% CI 0.71–1.51).
All considered, Koromani et al. present higher fracture risk in T2D after adjustment for BMI and the FN-BMD, but not spine BMD. Data was not presented in a way that allows for evaluation of the arbitrarily modified T-score threshold of − 2.0 for T2D.
Cohort Studies
Five cohort studies were included in the present review (Table 1).
Two studies (Agarwal et al. and Schousboe et al.) both reported data from the same Manitoba cohort. Though these studies included data from different time spans, there was an overlap [20••, 40•]. The objective in the study by Schousboe et al. was to evaluate incident vertebral, hip, and other non-vertebral fractures as well as prevalent VF and prior non-VFs in subjects with T2D who had a DXA yielding hip and lumbar spine BMD. The study by Agarwal and colleagues aimed to evaluate the performance of the Garvan fracture risk calculator in subjects with and without diabetes [20••]. Both studies found higher fracture risk among subjects with T2D. In the BMD adjusted analyses, Schousboe et al. found a HR for major osteoporotic fracture (MOF) of 1.27 (95% CI 1.18–1.36), a HR for clinical vertebral fracture of 1.16 (95% CI 1.01–1.33), a HR for proximal humerus fracture of 1.59 (95% CI 1.39–1.83) and a HR for hip fracture of 1.63 (95% CI 1.44–1.85) in subjects with T2D compared with subjects without diabetes. Agarwal et al. reported a HR for major osteoporotic fracture adjusted for Garvan fracture risk with BMD of 1.23 (95% CI 1.01–1.49) in subjects with T2D [20••]. Whereas Schousboe et al. reported a higher BMD in the T2D group compared to the control group [40•], a similar tendency in the study by Agarwal et al. was observed only in those without incident fractures and only statistically significant in women (see supplemental material) [20••]. It should be noted that patients with a vertebral fracture assessment (VFA) were excluded from the sub-cohort studied by Schousboe et al., to be studied as in a cross-sectional analysis (see later) [40•].
Mesinovic et al. studied a broad cohort of 1705 elderly Australian men and reported insignificantly higher total hip BMD in T2D subjects (p = 0.08) [47]. The hazards of both hip and any fractures were significantly decreased by higher hip BMD in both the T2D and the control group. The decrease was most pronounced in the control group though the CIs widely overlapped [47]. Sheu et al. reported (like Mesinovic et al.) higher FN-BMD among persons with T2D compared to persons without diabetes (p < 0.05) in a cohort study including 3618 community-dwelling persons aged 60 or more from the Dubbo Osteoporosis Epidemiology Study (DOES) in Australia. The two Australian studies both reported that the fracture risk depended on BMD in both participants with and without T2D, whereas the overall incident fracture risk did not differ between groups [39, 47], although Mesinovic et al. observed more falls in the T2D group [47] and Sheu et al. observed a higher amount of prior fractures within the T2D group [39].
Finally, Anna et al. performed a small cohort study of 62 Swedish subjects with either T1D or T2D with peripheral neuropathy treated for foot ulcers and followed for a median of 11 ± 8 years and 10 ± 7, respectively [25]. Among these, they reported a higher incidence of fractures than that in the general Swedish population [25]. The study did not include a control group without diabetes, but as the BMD results were reported as Z-scores with SD, we estimated the 95% CI of Z-scores (supplemental material). The Z-score of the spine BMD in the T2D group was 1.22 (95% CI 0.38–2.05). Moreover, the FN-BMD Z-score was statistically significantly higher in the T2D than in the T1D group. They did not report any association between fracture risk and BMD Z-scores.
Collectively, data from the large Canadian Manitoba cohort study support the thesis of an association between higher fracture risk and higher BMD in subjects with T2D. Although, no difference in BMD in subjects with previous fractures was observed between T2D and subjects without diabetes in the study by Agarwal et al. confined to data from 2012 to 2018 [20••]. However, the exact BMD at the time of fracture was not reported, and the same applies to all the included cohort studies having mean follow-up times of 2.6 to 15.5 years. Consequently, age, BMD, and other risk factors change as the diabetes disease progresses and anti-osteoporotic treatment may have been initiated during the follow-up. This may indeed result in substantial and immense changes in bone indices within the follow-up period. Among the remaining cohort studies, BMD is also reported higher in the T2D groups and coherence is seen in fracture risk depending on the BMD in both subjects with and without diabetes.
Cross-Sectional Studies
In the systematic review described above, Koromani et al. concludes that the risk of an incident VF is most likely higher among subjects with T2D. Paul et al. performed DXA with VFA on 202 women with T2D and 200 control subjects. They reported a higher hip and FN-BMD in T2D women compared to the control group [48]. Moreover, the mean spine BMD was insignificantly higher (p = 0.09). An elevated prevalence of VFs was identified by the VFA in subjects with T2D, though statistically insignificant (p = 0.15) [48].
Ramírez-Stieben et al. assessed prevalent VF by DXA scans in adult women and grouped the study subjects in a VF and a no VF group [49]. There were more women with T2D in the VF group than in the group without VF (61% vs. 31.5%, p < 0.00001), denoting a higher prevalence of VF among subjects with T2D. The LS BMD in women with T2D did not differ between those with and without VF, whereas in women without diabetes the BMD was significantly lower in those with VF. Consequently, these findings indicate that women with T2D and with a VF have higher LS BMD compared to women without diabetes and with VF [49].
Schousboe et al. presented cross-sectional data from a subgroup of the original cohort (MANITOBA) with no overlapping subjects [40•]. This subgroup was characterised by available VFA. It comprised 1185 T2D subjects and 8409 controls. The groups were compatible in age (mean age in T2D group 76.3 (6.8) vs. 76.0 (6.8) in subjects without diabetes), whereas there were more men in the T2D group, the mean BMI was higher (28.3 (6.0) vs. 25.7 (4.6)), and due to substantial differences in subject characteristics, a multivariate analysis was performed. The FN T-score was − 2.0 (0.7) in both groups and the multivariate analysis did not disclose any difference in the prevalence of VFs based on VFA nor prior clinical VFs in the T2D group compared to the control group.
Van Hulten et al. investigated LS-, hip-, and FN-BMD and the prevalence of vertebral fractures by VFA on DXA images available from the study cohort of The Maastricht Study [23]. In this cohort, the reported mean BMDs among both women and men with T2D were significantly higher than participants with normal glucose metabolism in all BMD sites (see supplemental material) [23]. In a fully adjusted model including BMD, women with T2D had a lower probability of at least one prevalent VF compared with persons with normal glucose metabolism (OR 0.25 (95% CI 0.09–0.65), while this tendency was not observed in men (OR 1.01 (95% CI 0.59–1.72)) [23].
Both de Tejada-Romero et al. and Adami et al. performed studies evaluating the effect of both obesity and T2D on BMD and vertebral as well as non-vertebral fractures. De Tejada-Romero et al. investigated a subgroup of postmenopausal obese women with (n = 32) and without (n = 154) T2D and observed no difference in BMD between obese participants with and without T2D [50]. However, the prevalence of prior fragility fractures and non-vertebral fractures were highest among subjects with diabetes, while there was no difference in the prevalence of prior VFs or hip fractures. A multivariate logistic regression showed that both high BMI and T2D were associated with higher odds of any fragility fracture. As the prevalence of hip fractures and VFs in the group with diabetes was not elevated, the findings may suggest an uneven distribution of fragility fractures in obese persons with and without T2D. Adami et al. conducted a cross-sectional study exploring the effect of both diabetes and obesity on bone using data from the Italian DeFRAcalc79 database [51]. They presented two categories of fracture outcomes: prevalent vertebral or hip fractures and prevalent non-vertebral and non-hip fractures. The study population consisted of 59,950 women and was analyzed as a full cohort and several sub-analyses were performed: a subpopulation of T2D patients and 1:1 age-matched controls (n = 6224); an overlapping smaller cohort that in addition to age also was matched on FN T-score (n = 1684); and finally, a subpopulation of non-obese T2D subjects and age- and T-score-matched controls (n = 1282). Mean T-scores in the groups including T2D subjects were significantly higher than in the groups without diabetes, whereas the rates of all types of prevalent fractures were higher (p < 0.0001). This difference was attenuated when matching on both age and T-scores for both prevalent vertebral and hip fractures and prevalent non-vertebral and non-hip fractures. However, in the subpopulation from which obese patients were excluded, the prevalence of non-vertebral, non-hip fractures remained higher in the T2D group when matching on age and T-score (p < 0.001). Non-vertebral and non-hip fractures seem more overrepresented in the T2D group than the VFs and hip fractures, which concurs with findings by de Tejada-Romero et al. [50]. Adami et al. also reported an elevated fracture rate among obese patients without diabetes [51]. Taking this into consideration, removing obese control persons at risk of fracture from the subpopulation may explain that the difference in fracture risk reached significance in this sub analysis.
All considered, the six included cross-sectional studies on T2D report ambiguous findings concerning differences in BMD and T-score in persons with T2D. Two studies reported higher BMD in those with T2D [23, 51], whereas two others observed no difference in BMD among individuals with and without diabetes [40•, 50]. Finally, Paul et al. observed higher BMD in the T2D group, but no difference in BMD when examining only participants with VFs with and without T2D, and Ramirez-Stieben et al. conflictingly only reported a BMD difference between persons with and without T2D in those with a VF, as the BMD of the persons with T2D and VF was not lower than those with T2D and no VF. Also, the evidence on fracture risk is conflicting, though only a single study reported a reduced risk of VFs in T2D [23]. The studies by de Tejada-Romero et al. and Adami et al. suggest a trend of a distribution of fractures among those with T2D with an elevated prevalence of fragility fractures other than hip and vertebral [50, 51]. When considering correlations between current BMD and prevalent fractures and VFs diagnosed by VFA, there is an unknown time variable as the BMD at the exact time of VF or fracture is unreported.
Case-Control Studies
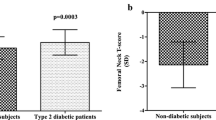
Two case-control studies were included. Valentini et al. investigated 107 cases with low-energy trauma hip fracture compared with 65 subjects without fracture recruited from a medical outpatient clinic in a secondary analysis [21]. The mean BMD was higher in the T2D fracture cases compared with those without diabetes. Similar findings were reported in the group without fractures (supplemental material) [21]. These results correspond to the findings from Giner et al., although the difference did not reach statistical significance [52]. When comparing T-scores, Valentini et al. also reported higher values in subjects with T2D compared to subjects without diabetes.
Taken together, the two studies suggest that subjects with T2D in general have a higher BMD and T-score compared with subjects without diabetes, regardless of fracture history.
Type 1 Diabetes
Only two small studies on T1D were identified among the included studies in the systematic search.
The cohort study by Anna et al. reported a higher fracture incidence among subjects with diabetes and concurrent neuropathy and foot ulcers compared to the general population and also found decreased FN-BMD in the subjects with T1D [25], as the 95% CI of the FN-BMD Z-score in the T1D group was below zero (Z-score − 0.98, 95% CI − 1.40–− 0.56), indicating that the FN-BMD in these T1D subjects with peripheral neuropathy and foot ulcers is 95% likely to be lower than the FN-BMD in the reference population. However, they did not identify any association between BMD and fracture risk.
Coll et al. presented data from a cross-sectional study including 127 subjects with T1D and 65 subjects without diabetes with a median age of approximately 42 years [53]. The participants were DXA scanned and a modified VFA method was used to examine VFs. The observed T-scores of the total hip and the femoral neck were lower in participants with T1D compared to the subjects without diabetes. However, the fracture outcome of interest was rare in both groups, as prevalent VFs were only identified in 5 subjects: 3 subjects with T1D and 2 subjects without diabetes. For this reason, no association analysis was performed, but characteristics were described. To note, the VFs among subjects with diabetes occurred at younger ages than in the controls.
As the primary search only evolved two studies on T1D, we decided to narrow the PubMed search from the systematic review to include only studies on T1D and broaden the timespan to 18 years (search string in supplemental material). Studies before this were expected to be included in a thorough and well-cited review from 2007 [1]), in which we found only 1 study reporting on both BMD and prevalent vertebral deformities, however, did not explore the association between BMD and fracture risk [54]. After filtering results to only include human adults the search added a single study by Zhukouskaya et al. reporting BMD T- and Z-scores specifically for subjects with T1D with morphometric VFs compared to subjects without diabetes with the same type of fractures (Table 1) [24]. The researchers reported significantly more VFs among subjects with T1D compared to subjects without diabetes (p = 0.002) and the T-scores of both the spine and femoral neck were lower in T1D subjects both with and without fractures (supplemental material). In subjects with a VF both with and without diabetes the median T-score was above − 1.0 and well above − 2.5. Based on 95% CIs of given Z-scores (see supplemental material, for calculation), the BMD in T1D subjects with and without VF was lower than in the reference population [24].
Discussion
This systematic literature review has presented data from the recent years of clinical research investigating the association between fractures and bone mineral density related to osteoporosis in subjects with diabetes compared to subjects without diabetes. The aim was to investigate if and how the BMD level varies within the diabetes population, at which BMD T-score persons with diabetes suffer an osteoporotic fracture, and if it differs from the background population.
Currently, the benchmark for diagnosing and initiating pharmacological treatment for osteoporosis stands at a T-score equal to or below − 2.5 SD, only modified in those with glucocorticoid-induced osteoporosis (T-score threshold − 1.0). However, the updated American Diabetes Guidelines now recommend assessing fracture risk, monitor BMD, and to consider anti-osteoporotic medication at a T-score of − 2.0 in the standards of care in diabetes. The query at hand pertains to whether recent studies endorse the implementation of a T-score threshold of − 2.0 for diagnosis and treatment of osteoporosis in subjects with diabetes.
The DXA evaluation including BMD and T-score calculations is to date the only diagnostic tool for assessing low bone quality. As both the evaluation and fracture predictions are insufficient in subjects with diabetes, another threshold and/or other methods are necessary to evaluate bone health and fracture risk in subjects with diabetes. T1D is, unlike T2D, incorporated in the FRAX tool and is indirectly considered as a secondary cause of osteoporosis, i.e., assumed to increase the fracture probability via low BMD. If BMD is unknown, the fracture risk in T1D is assumed similar to a person with rheumatoid arthritis. As a result, the calculated fracture risk is only increased in T1D when BMD is unknown or simply not included in the calculation [55]. For that reason, the fracture probability is underestimated by the FRAX tool in subjects with both T1D and T2D [56], and hip fractures in particular [57].
The strongest evidence burden included in the review suggests an elevated or similar BMD in people with and without T2D. However, a few studies reported an unequal BMD between T2D subjects with and without an osteoporotic fracture. Paul et al. reported higher BMD in T2D subjects in the full study population, but not in the subgroup with VFs [48] and Agarwal et al. only observed increased BMD in T2D subjects without incident fractures, while Ramirez-Stieben et al. on the other hand reported an elevated BMD in T2D only among those with VF (as the BMD was not equally decreased in persons with and without diabetes who had experienced a VF) [20••, 49]. Few studies have reported BMD at the time of fracture but were not included due to the case-only design [26, 35,36,37,38]. As these studies were lacking a control group without fractures, they were highly susceptible to considerable concealed selection bias and, consequently, were not sufficiently informative on fracture risk by BMD level. However, in accordance with the BMD being generally higher among persons with T2D, the BMD was reported higher in subjects with T2D at the time of fracture as well [26, 36]. These results may contradict the findings by Paul et al. and Agarwal et al. [20••, 26, 36, 48].
Overall, the results from the studies in this review agree on the consensus of an elevated fracture risk in persons with T1D and T2D. However, an elevated risk of VFs was not distinctly evident in T2D, as indicated by results from the cross-sectional studies included in this review. And so, VFs are not reported to occur at a higher BMD in subjects with diabetes compared to subjects without diabetes. Non-vertebral fragility fractures seem to be more frequent among those with diabetes and some evidence points towards a distribution of fractures not carried by hip and vertebral fractures [50, 51].
The meta-analysis by Koromani et al. included both the US studies from the aforementioned meta-analysis by Schwartz et al. and several European studies from a wider time range as well. They concluded, in concordance with Schwartz et al. [4], that subjects with T2D have a higher BMD, while the risk of non-vertebral fractures was particularly elevated in those with osteopenia (T-score between − 1.0 and − 2.4) [41••]. These findings support the need for an improved fracture risk stratification in T2D subjects with osteopenia. As reported above, Agarwal et al. included a large dataset from the Canadian Manitoba Cohort and observed an increased risk of osteoporotic fractures among subjects with T2D compared to subjects without diabetes but did not find any difference in BMD between T2D subjects with fractures than in subjects without diabetes with fractures [20••]. This diverges from the general findings in the large cohort studies included in the meta-analyses. As Agarwal et al. included only data from the Manitoba cohort from a recent time range (2012 to 2018), it may impede considerations of significant changes in antidiabetic treatment during the last 2–3 decades. In the 1990s and 2000s, glucose-lowering drugs were restricted to insulin, biguanides, sulfonylurea, and thiazolidinedione (TZD). In 2010s, the use of newer glucose-lowering drugs accelerated, e.g., glucagon-like peptide 1 receptor agonists and sodium-glucose cotransporter-2 inhibitors of which the former may have the potential to preserve bone mass during weight loss [58, 59]. Moreover, age of diabetes diagnosis, screening, and treatment of osteoporosis in T2D may have changed during the last decades and it remains unknown if the BMD of subjects with fractures in this Canadian study were similar in subjects with and without diabetes before 2012. Hence, similar studies from a wider time range of the Manitoba cohort may illuminate this. Moreover, other studies including recent observations [25, 47, 52] did not find differences in T-score or BMD comparable to those reported by Schwartz et al. [4]. This might lead to considerations of whether a decision of a revised treatment threshold should rely upon data dating 20 or 30 years back, considering that the clinical features of the target population (persons with T2D) may have changed considerably during the past two decades. One example is the general decrease in fracture rates among people with diabetes found in a Danish population study between 1997 and 2017 [60]. As another example, TZDs have been shown to cause bone loss and increased fracture risk [61]. Hence, the use of these drugs in the treatment of diabetes before 2011 [62] may have influenced both BMD and fracture risk in studies including real-life data from this time span. Generally, information on the use of TZD in the studies included in this review was not available. However, as described above, recent data is included in the meta-analysis by Koromani et al. [41••] and other studies also reported higher BMD in subjects with non-vertebral fractures and concomitant T2D compared to subjects with non-vertebral fractures without diabetes [21]. Furthermore, the T-score difference reported by Valentini [21] et al. was comparable to that suggested by Schwartz et al. [4] supporting a 0.5 SD modified T-score threshold in T2D. In some studies, the BMD difference was reported instead of a T-score difference [48, 49, 52].
There are several limitations in the current review, of which heterogeneity of the included studies is central. Due to diversity in aims, primary outcomes, and design, it was not possible to set a meta-analysis. Moreover, a comparison of T-scores between studies should be interpreted with caution as the characteristics of the measures should be taken into consideration. However, exact information of BMD calculation and reference were not reported in most of the included studies. Lastly, comparisons of BMD and T-score results between studies were not possible due to the divergence in demographics. The Z-score is the deviation in SD from the mean BMD in the reference population of subjects with the same age and sex. If the same references are used in the calculation, this can in some cases be a more suitable comparison to be used between studies, though the clinical relevance is less important. Only a few studies in this review reported Z-scores [25, 53]. In general, information on how BMD contributes to the fracture risk was limited. Most studies made a multivariate analysis adjusting for several confounders including BMD but without information concerning the isolated impact of BMD on the estimates. We consider the risk of publication bias in this systematic review to be low. Small studies with negative findings are represented. Many of the included studies had primary aims different from the scope of this review, and so, some results in this review represent secondary outcomes. The studies using data from the Manitoba and DeFraCalc cohorts [20••, 51] are at risk of selection bias as only subjects referred for DXA-scan are included. As appreciation of osteoporosis as a complication of diabetes is growing, an increasing proportion of these patients may be referred to DXA scans. There may be a selection in the level of self-care, though this would be expected not to differ between persons with diabetes and persons without diabetes. The case-control studies encountered difficulties in identifying suitable control subjects. We included several cross-sectional studies. As for the studies using prevalent or prior fractures as outcome, it remains unknown what the BMD or T-score was at the time of fracture. Therefore, studies that assess BMD in subjects with recent fractures (compared to subjects without fractures at the same fracture risk) are pertinent for addressing the primary inquiry of this review.
There is a notable scarcity of findings including BMD and fracture risk in subjects with T1D. The presented studies do not contribute to the existing body of evidence concerning the association between T-score and fractures in subjects with T1D. Further research in this domain, as well as exploration of alternative risk assessment modalities, is imperative. As far as our knowledge and the constrained search extends, there appears to be minimal existing research on T-scores in subjects with T1D at the time of fracture occurrence.
Some studies have suggested higher rates of bone loss in subjects with T2D. A study [63] reported a more rapid bone loss in older women with T2D compared with those without diabetes. Another large registry-based study [57] found that women with diabetes had a greater BMD loss located to the femoral neck but not at other skeletal sites compared to a population without diabetes. These findings might imply the necessity of periodic BMD assessments for diabetes subjects, such as performing a DXA scan of all diabetes subjects aged over 65 every 2–3 years, even in cases where the BMD appears normal, as was also recently suggested by the American Diabetes Association [15]. Nevertheless, there is a dearth of data concerning the optimal timing for acting based on a specific BMD change to prevent fractures.
The fact that individuals with diabetes have an affected bone quality is well-recognized among scientists across the world. Yet, the patients are less likely to have insight into fractures as a diabetes-related complication [64, 65] and they are less likely to be diagnosed with and treated for osteoporosis to prevent fractures [66]. In the clinical setting, the guidelines in Europe and America clearly state that all patients with diabetes should be informed about, screened, and preventively treated for micro- and macrovascular complications, e.g., retinopathy, nephropathy, neuropathy, and cardiovascular disease. And only recently, bone health was included in the evaluation of comorbidities by the American Diabetes Association. Consequently, clinicians may not be able to diagnose and treat osteoporosis in these patients before the first hip or vertebral fracture is present, and people with diabetes do not receive adequate guidance and management to optimize bone health. Naturally, these facts emphasize the need to enhance the diagnostics of low bone quality in individuals with diabetes. However, as presented in this review, current research covering the differences in T-scores between subjects with and without diabetes and including fractures related to osteoporosis is sparse and almost completely absent in T1D.
Besides reducing the FN T-score input to FRAX by 0.5 SD, other methods have been proposed to improve FRAX performance in subjects with T2D, including the rheumatoid arthritis input to FRAX, the trabecular bone score (TBS)-adjustment to FRAX, and increasing the age input to FRAX by 10 years [67].
Conclusion
The prevalence of T2D and osteoporosis is increasing, and the treatment strategies have improved. Still, the diagnostic criteria for osteoporosis have remained unchanged for more than 30 years. Low bone quality and fractures have been acknowledged as a diabetes-related complication in the research setting. However, the dearth of acceptance of diabetes as an independent risk factor for osteoporosis-related fractures in the clinical setting could impede fracture prevention in this population.
While the findings regarding the risk of vertebral fractures in T2D are conflicting, a notable congruence has emerged in the elevated risk of non-vertebral fractures. Moreover, there is consistency of a higher BMD and T-score in subjects with T2D. The proposed modified T-score threshold limit of − 2.0 derives from extensive but decade-old investigations which may not be generalizable to the current T2D population. Newer clinical trials are warranted and so, two substantial questions remain: 1) do subjects with T2D actually fracture at a higher BMD compared with subjects without diabetes, and if so 2) does this endorse a T-score treatment threshold of − 2.0 in subjects with T2D?
All considered, there is a pressing necessity for contemporary research. We propose future studies to focus on the evaluation of T-scores among diabetes subjects who sustain a fracture related to osteoporosis compared to subjects without diabetes. There is a need for both large-scale cross-sectional data and long-term follow-up cohort studies to evaluate the T-score differences as well as changes in T-scores over time and the risk of fractures between subjects with and without diabetes.
Data Availability
The evidence in this systematic literature study is based on already published data and is summarized in Table 1.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Vestergaard P. Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes - a meta-analysis. Osteoporos Int. 2007;18:427–44. https://doi.org/10.1007/s00198-006-0253-4.
Hough FS, Pierroz DD, Cooper C, Ferrari SL. Mechanisms and evaluation of bone fragility in type 1 diabetes mellitus. Eur J Endocrinol. 2016;174:R127–38. https://doi.org/10.1530/EJE-15-0820.
Shah VN, Harrall KK, Shah CS, et al. Bone mineral density at femoral neck and lumbar spine in adults with type 1 diabetes: a meta-analysis and review of the literature. Osteoporos Int. 2017;28:2601–10. https://doi.org/10.1007/s00198-017-4097-x.
Schwartz AV, Vittinghoff E, Bauer DC, et al. Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. Jama. 2011;305:2184–92. https://doi.org/10.1001/jama.2011.715.
Eastell R, Vittinghoff E, Lui L-Y, et al (2022) Diabetes mellitus and the benefit of antiresorptive therapy on fracture risk. Bone Rep 16. https://doi.org/10.1016/j.bonr.2022.101190
Anagnostis P, Paschou SA, Gkekas NN, et al. Efficacy of anti-osteoporotic medications in patients with type 1 and 2 diabetes mellitus: a systematic review. Endocrine. 2018;60:373–83. https://doi.org/10.1007/s12020-018-1548-x.
Bliuc D, Tran T, Chen W, et al. The association between multimorbidity and osteoporosis investigation and treatment in high-risk fracture patients in Australia: a prospective cohort study. PLoS Med. 2023;20:e1004142. https://doi.org/10.1371/journal.pmed.1004142.
Fraser LA, Papaioannou A, Adachi JD, et al. Fractures are increased and bisphosphonate use decreased in individuals with insulin-dependent diabetes: a 10 year cohort study. BMC Musculoskelet Disord. 2014;15:1–9. https://doi.org/10.1186/1471-2474-15-201.
Vilaca T, Schini M, Harnan S, et al. The risk of hip and non-vertebral fractures in type 1 and type 2 diabetes: a systematic review and meta-analysis update. Bone. 2020;137:115457. https://doi.org/10.1016/j.bone.2020.115457.
Sheffield TU of FRAX(R). https://frax.shef.ac.uk/FRAX/tool.aspx?country=29.
Society DE Danish national treatment guideline. https://endocrinology.dk/nbv/calcium-og-knoglemetabolisme/postmenopausal-osteoporose/.
Champakanath A, Keshawarz A, Pyle L, et al. Fracture risk assessment (FRAX) without BMD and risk of major osteoporotic fractures in adults with type 1 diabetes. Bone. 2021;143:115614. https://doi.org/10.1016/j.bone.2020.115614.
Morin SN, Feldman S, Funnell L, et al. Clinical practice guideline for management of osteoporosis and fracture prevention in Canada : 2023 update. CMAJ. 2023;195:1333–48. https://doi.org/10.1503/cmaj.221647.
Ferrari SL, Abrahamsen B, Napoli N, et al. Diagnosis and management of bone fragility in diabetes: an emerging challenge. Osteoporos Int. 2018;29:2585–96. https://doi.org/10.1007/s00198-018-4650-2.
Elsayed NA, Aleppo G, Aroda VR, et al. 4. Comprehensive medical evaluation and assessment of comorbidities: standards of care in diabetes—2023. Diabetes Care. 2023;46:S49–67. https://doi.org/10.2337/dc23-S004.
Wells G, Shea B, O’connell D, Peterson J, Welch V, Losos M (2000) Newcastle-Ottawa Scale.
Herzog R, Álvarez-Pasquin MJ, Díaz C, et al (2013) Are healthcare workers intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health 13:. https://doi.org/10.1186/1471-2458-13-154.
Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:1–9. https://doi.org/10.1136/bmj.j4008.
Levels of evidence - centre for evidence-based medicine (University of Oxford). 2009; https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009. Accessed 12 Oct 2023.
•• Agarwal A, Leslie WD, Nguyen TV, et al. Performance of the Garvan fracture risk calculator in individuals with diabetes: a registry-based cohort study. Calcif Tissue Int. 2022;110:658–65. https://doi.org/10.1007/s00223-021-00941-1. This study is interesting as it includes from the MANITOBA data only from 2012 to 2018 and does not report of higher BMD in type 2 diabetes subjects with fractures compared to subjects without diabetes.
Valentini A, Cianfarani MA, Federici M, et al. Osteoprotegerin in diabetic osteopathy. Nutr Metab Cardiovasc Dis. 2020;30:49–55. https://doi.org/10.1016/j.numecd.2019.08.018.
Lasschuit JWJ, Center JR, Greenfield JR, Tonks KTT. Comparison of calcaneal quantitative ultrasound and bone densitometry parameters as fracture risk predictors in type 2 diabetes mellitus. Diabet Med. 2020;37:1902–9. https://doi.org/10.1111/dme.14183.
van Hulten V, Sarodnik C, Driessen JHM, et al. Prevalent morphometrically assessed vertebral fractures in individuals with type 2 diabetes, prediabetes and normal glucose metabolism: the Maastricht study. Front Endocrinol (Lausanne). 2022;13:832977. https://doi.org/10.3389/fendo.2022.832977.
Zhukouskaya VV, Eller-Vainicher C, Vadzianava VV, et al. Prevalence of morphometric vertebral fractures in patients with type 1 diabetes. Diabetes Care. 2013;36:1635–40. https://doi.org/10.2337/dc12-1355.
Anna U-M, Maria S, Kerstin B. Comparison of quantitative ultrasound of calcaneus and dual energy X-ray absorptiometry in measuring bone density and predicting fractures in patients with diabetic polyneuropathy: a prospective cohort study. Diabetes Res Clin Pract. 2021;180:109064. https://doi.org/10.1016/j.diabres.2021.109064.
Di Monaco M, Castiglioni C, Bardesono F, et al. Femoral bone mineral density at the time of hip fracture is higher in women with versus without type 2 diabetes mellitus: a cross-sectional study. J Endocrinol Invest. 2023. https://doi.org/10.1007/s40618-023-02122-3.
Cairoli E, Grassi G, Gaudio A, et al. Validation of the clinical consensus recommendations on the management of fracture risk in postmenopausal women with type 2 diabetes. Nutr Metab Cardiovasc Dis. 2023;33:158–67. https://doi.org/10.1016/j.numecd.2022.10.004.
Meng C, Zhao D, Ye X-H. Association of body composition with bone mineral density and fractures in Chinese male type 2 diabetes mellitus. Medicine (Baltimore). 2023;102:e33400. https://doi.org/10.1097/MD.0000000000033400.
Lin Y-C, Wu J, Kuo S-F, et al. Vertebral fractures in type 2 diabetes patients: utility of trabecular bone score and relationship with serum bone turnover biomarkers. J Clin Densitom. 2020;23:37–43. https://doi.org/10.1016/j.jocd.2019.01.003.
Schwartz AV, Backlund J-YC, de Boer IH, et al. Risk factors for lower bone mineral density in older adults with type 1 diabetes: a cross-sectional study. Lancet Diabetes Endocrinol. 2022;10:509–18. https://doi.org/10.1016/S2213-8587(22)00103-6.
Dhaliwal R, Ewing SK, Vashishth D, et al. Greater carboxy-methyl-lysine is associated with increased fracture risk in type 2 diabetes. J Bone Miner Res. 2022;37:265–72. https://doi.org/10.1002/jbmr.4466.
Alfadhli EM, Alsharif AS, Alharbi RA, et al. Comparison of bone mineral density and Fracture Risk Assessment Tool in Saudi women with and without type 2 diabetes mellitus. Saudi Med J. 2022;43:700–7. https://doi.org/10.15537/SMJ.2022.43.7.20220144.
Pechmann LM, Petterle RR, Moreira CA, Borba VZC. Osteosarcopenia and trabecular bone score in patients with type 2 diabetes mellitus. Arch Endocrinol Metab. 2021;65:801–10. https://doi.org/10.20945/2359-3997000000418.
Koç Z. The effect of type 2 diabetes mellitus on osteopenia and vertebral fractures in elderly women. Turk Osteoporoz Derg. 2022;28:125–30. https://doi.org/10.4274/tod.galenos.2021.35403.
Abdelmaksoud NM, Abulsoud AI, Abulsoud MI, Elshaer SS. Genetic impact of vitamin D receptor TaqI polymorphism on the risk of osteoporotic fractures in diabetic patients. Gene Rep. 2022;27:101591. https://doi.org/10.1016/j.genrep.2022.101591.
Gani LU, Saripalli KR, Fernandes K, et al. Bone mineral density and trabecular bone score in elderly type 2 diabetes Southeast Asian patients with severe osteoporotic hip fractures. PLoS One. 2020;15:e0241616. https://doi.org/10.1371/journal.pone.0241616.
Sihota P, Yadav RN, Dhaliwal R, et al. Investigation of mechanical, material, and compositional determinants of human trabecular bone quality in type 2 diabetes. J Clin Endocrinol Metab. 2021;106:E2271–89. https://doi.org/10.1210/clinem/dgab027.
Sihota P, Pal R, Naresh Yadav R, et al. Can fingernail quality predict bone damage in type 2 diabetes mellitus? a pilot study. PLoS One. 2021;16:e0257955. https://doi.org/10.1371/journal.pone.0257955.
Sheu A, Bliuc D, Tran T, et al. Fractures in type 2 diabetes confer excess mortality: The Dubbo osteoporosis epidemiology study. Bone. 2022;159:116373. https://doi.org/10.1016/j.bone.2022.116373.
• Schousboe JT, Morin SN, Kline GA, et al. Differential risk of fracture attributable to type 2 diabetes mellitus according to skeletal site. Bone. 2022;154:116220. https://doi.org/10.1016/j.bone.2021.116220. This study analyses data from the Manitoba cohort and finds elevated fracture risk among subjects with type 2 diabetes, namely hip and humerus fractures.
•• Koromani F, Oei L, Shevroja E, et al. Vertebral fractures in individuals with type 2 diabetes: more than skeletal complications alone. Diabetes Care. 2020;43:137–44. https://doi.org/10.2337/dc19-0925. This systematic review and metanalysis includes a high number of total participants from major cohort studies and find that the risk of fractures is increased in individuals with type 2 diabetes, especially in those with osteopenia.
Cummings SR, Black DM, Michael C, Nevitt P, et al. Appendicular bone density and age predict hip fracture in women. JAMA - J Am Med Assoc. 1990;263:665–8. https://doi.org/10.1001/jama.1990.03440050059033.
Tenenhouse A, Joseph L, Kreiger N, et al. Estimation of the prevalence of low bone density in Canadian women and men using a population-specific DXA reference standard: The Canadian Multicentre Osteoporosis Study (CaMos). Osteoporos Int. 2000;11:897–904. https://doi.org/10.1007/s001980070050.
McCloskey EV, Beneton M, Charlesworth D, et al. Clodronate reduces the incidence of fractures in community-dwelling elderly women unselected for osteoporosis: results of a double-blind, placebo-controlled randomized study. J Bone Miner Res. 2007;22:135–41. https://doi.org/10.1359/jbmr.061008.
Shevroja E, Marques-Vidal P, Aubry-Rozier B, et al. Cohort profile: the OsteoLaus study. Int J Epidemiol. 2019;48:1046-1047G. https://doi.org/10.1093/ije/dyy276.
Ikram MA, Brusselle GGO, Murad SD, et al. The Rotterdam study: 2018 update on objectives, design and main results. Eur J Epidemiol. 2017;32:807–50. https://doi.org/10.1007/s10654-017-0321-4.
Mesinovic J, Scott D, Seibel MJ, et al. Risk factors for incident falls and fractures in older men with and without type 2 diabetes mellitus: the Concord Health and Ageing in Men Project. J Gerontol A Biol Sci Med Sci. 2021;76:1090–100. https://doi.org/10.1093/gerona/glab062.
Paul J, Devarapalli V, Johnson JT, et al. Do proximal hip geometry, trabecular microarchitecture, and prevalent vertebral fractures differ in postmenopausal women with type 2 diabetes mellitus? A cross-sectional study from a teaching hospital in southern India. Osteoporos Int. 2021;32:1585–93. https://doi.org/10.1007/s00198-021-05855-0.
Ramírez Stieben LA, Dobry R, González A, et al. Vertebral fractures in adult women with type 2 diabetes mellitus. Actual osteol. 2020;16:1–9.
de Tejada-Romero MJG, Saavedra-Santana P, de la Rosa-Fernández F, et al. Effect of obesity on fragility fractures, BMD and vitamin D levels in postmenopausal women. Influence of type 2 diabetes mellitus. Acta Diabetol. 2022;59:1201–8. https://doi.org/10.1007/s00592-022-01923-x.
Adami G, Gatti D, Rossini M, et al. Risk of fragility fractures in obesity and diabetes: a retrospective analysis on a nation-wide cohort. Osteoporos Int. 2020;31:2113–22. https://doi.org/10.1007/s00198-020-05519-5.
Giner M, Miranda C, Vázquez-Gámez MA, et al. Microstructural and strength changes in trabecular bone in elderly patients with type 2 diabetes mellitus. Diagnostics. 2021;11:577. https://doi.org/10.3390/diagnostics11030577.
Coll J-C, Garceau É, Leslie WD, et al. Prevalence of vertebral fractures in adults with type 1 diabetes: DenSiFy study (diabetes spine fractures). J Clin Endocrinol Metab. 2022;107:E1860–70. https://doi.org/10.1210/clinem/dgac031.
Hanley DA, Brown JP, Tenenhouse A, et al. Associations among disease conditions, bone mineral density, and prevalent vertebral deformities in men and women 50 years of age and older: cross-sectional results from the Canadian Multicentre Osteoporosis Study. J Bone Miner Res. 2003;18:784–90. https://doi.org/10.1359/jbmr.2003.18.4.784.
Vandenput L, Johansson H, McCloskey EV, et al. Update of the fracture risk prediction tool FRAX: a systematic review of potential cohorts and analysis plan. Osteoporos Int. 2022;33:2103–36. https://doi.org/10.1007/s00198-022-06435-6.
Giangregorio LM, Leslie WD, Lix LM, et al. FRAX underestimates fracture risk in patients with diabetes. J Bone Miner Res. 2012;27:301–8. https://doi.org/10.1002/jbmr.556.
Leslie WD, Morin SN, Majumdar SR, Lix LM. Effects of obesity and diabetes on rate of bone density loss. Osteoporos Int. 2018;29:61–7. https://doi.org/10.1007/s00198-017-4223-9.
Hygum K, Harsløf T, Jørgensen NR, et al. Bone resorption is unchanged by liraglutide in type 2 diabetes patients: a randomised controlled trial. Bone. 2020;132:115197. https://doi.org/10.1016/j.bone.2019.115197.
Iepsen EW, Lundgren JR, Hartmann B, et al. GLP-1 receptor agonist treatment increases bone formation and prevents bone loss in weight-reduced obese women. J Clin Endocrinol Metab. 2015;100:2909–17. https://doi.org/10.1210/jc.2015-1176.
Kvist AV, Nasser MI, Vestergaard P, et al. Site-specific fracture incidence rates among patients with type 1 diabetes, type 2 diabetes, or without diabetes in Denmark (1997–2017). Diabetes Care. 2023;46:633–42. https://doi.org/10.2337/dc22-1004.
McDonough AK, Rosenthal RS, Cao X, Saag KG. The effect of thiazolidinediones on BMD and osteoporosis. Nat Clin Pract Endocrinol Metab. 2008;4:507–13. https://doi.org/10.1038/ncpendmet0920.
Sundhedsdatastyrelsen (2023) MEDSTAT.DK. https://medstat.dk/da. Accessed 9 Oct 2023.
Schwartz AV, Ewing SK, Porzig AM, et al. Diabetes and change in bone mineral density at the hip, calcaneus, spine, and radius in older women. Front Endocrinol (Lausanne). 2013;4:1–9. https://doi.org/10.3389/fendo.2013.00062.
Sanz-Nogués C, Mustafa M, Burke H, et al. Knowledge, perceptions and concerns of diabetes-associated complications among individuals living with type 1 and type 2 diabetes mellitus. Healthc. 2020;8:1–12. https://doi.org/10.3390/healthcare8010025.
Drummond K, Bennett R, Gibbs J, et al. Perceptions of fracture and fall risk and of the benefits and barriers to exercise in adults with diabetes. Osteoporos Int. 2022;33:2563–73. https://doi.org/10.1007/s00198-022-06524-6.
Viggers R, Starup-Linde J, Vestergaard P. Discrepancies in type of first major osteoporotic fracture and anti-osteoporotic therapy in elderly people with type 2 diabetes mellitus: A retrospective Danish cohort study. Bone. 2023;171:116745. https://doi.org/10.1016/j.bone.2023.116745.
Leslie WD, Johansson H, McCloskey EV, et al. Comparison of methods for improving fracture risk assessment in diabetes: the Manitoba BMD Registry. J Bone Miner Res. 2018;33:1923–30. https://doi.org/10.1002/jbmr.3538.
Funding
During the conduct of the study, Dr. Viggers and Dr. Brandt received grants from Novo Nordisk Foundation, Denmark (grants no. NNF18OC0052064 and no. NNF20OC0065960, respectively).
Author information
Authors and Affiliations
Contributions
I.B. and R.V. performed the initial search and (independently) evaluated results for eligibility J.S-L. was consulted in cases of doubt. The manuscript was written in collaboration between I.B., R.V and J.S-L. and critically revised by S.A. Supplemental material was set up by I.B. and calculations were performed by I.B.
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Viggers holds shares in Novo Nordisk. During the conduct of the study, Dr. Starup-Linde presented for UCB Nordic A/S. Apart from this, the authors have no conflict of interest to declare.
Human and Animal Rights and Informed Consent
No clinical trials or animal studies were set up in relation to the conduct of this review. The included studies were conducted in accordance with the Helsinki Declaration and national or local ethics committee’s standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brandt, I.A.G., Starup-Linde, J., Andersen, S.S. et al. Diagnosing Osteoporosis in Diabetes—A Systematic Review on BMD and Fractures. Curr Osteoporos Rep 22, 223–244 (2024). https://doi.org/10.1007/s11914-024-00867-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-024-00867-1