Abstract
Purpose
The purpose of this study was to compare ligament balance and laxity profiles achieved throughout flexion in restricted kinematic alignment (rKA) and gap balancing (GB). rKA and GB both aim to improve soft tissue balance and reduce ligament releases in total knee arthroplasty (TKA).
Methods
One surgeon performed 68 rKA, another performed 73 GB TKAs using the same CR implant and robotic system. rKA limited femoral valgus and tibial varus to 6°, with tibial recuts performed to achieve balance. GB limited tibial varus and femoral valgus to 2°, with femoral resections adjusted to achieve mediolateral balance throughout flexion using predictive-gap planning software. Final joint laxity was measured using a robotic ligament tensioner. Statistical analyses were performed to compare differences in mediolateral balance and joint laxity throughout flexion. Further analyses compared alignment, joint line elevation and orientation (JLO), and frequency of ligament releases and bone recuts.
Results
Both techniques reported greater lateral laxity throughout flexion, with GB reporting improved mediolateral balance from 10° to 45° flexion. GB resected 1.7 mm more distal femur (p ≤ 0.001) and had greater overall laxity than rKA throughout flexion (p ≤ 0.01). rKA increased JLO by 2.5° and 3° on the femur and tibia (p ≤ 0.001). Pre-operative and post-operative coronal alignment were similar across both techniques. rKA had a higher tibial recut rate: 26.5% vs 1.4%, p < 0.001.
Conclusions
rKA and GB both report lateral laxity but with different JLO and elevation. Use of a predictive-gap GB workflow resulted in greater mediolateral gap symmetry with fewer recuts.
Level of evidence
III, retrospective cohort study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restricted kinematic alignment (rKA) and gap balancing (GB) are alternative alignment strategies for total knee arthroplasty (TKA), which aim to improve soft tissue balance and reduce ligament releases compared to mechanically aligned (MA) TKA [2, 6, 7]. These benefits are believed to improve pain and functional outcome by minimizing soft tissue trauma and improving knee stability and kinematics [10, 16, 30].
rKA aims to correct the arthritic deformity by restoring the native distal and posterior femur joint lines while compensating for articular cartilage wear and restricting distal femoral and proximal tibial coronal angles to limit outlier alignments [10, 19]. GB uses the soft tissue envelope to drive alignment, using a neutral tibial resection and adjusting femoral component position to optimize rectangular mediolateral (ML) joint stability [6, 21]. The difference in resultant joint balance and component position between these techniques remains unclear. While some studies have reported on joint laxity in flexion and extension [19, 33], no studies have characterized laxity profiles throughout flexion under standardized loads. Robotic technologies now allow for digitally controlled soft tissue assessment throughout the entire flexion range [32, 34] and recent studies have shown that small differences in laxity (1–2 mm) can affect patient outcomes [35].
This study explores the differences in joint laxity profiles between rKA and GB under a standardized load. A better understanding of how component alignment and joint line obliquity affect joint laxity profiles and joint balance throughout the range of motion may help surgeons with intraoperative clinical decision making. Consequently, the primary purpose of this study was to characterize rKA and GB laxity profiles measured using a digitally controlled ligament tensioner. A secondary purpose was to compare bone resection obliquity and depth, and soft tissue release and bone recut rates. The hypotheses were that (1) rKA would result in greater flexion laxity laterally than medially and a looser flexion gap than extension gap laterally; (2) GB would exhibit less imbalance throughout flexion and a more neutral joint line while requiring fewer recuts; and (3) that final overall alignment would be similar in both groups due to the imposed alignment boundaries [28].
Methods
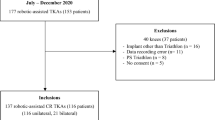
One hundred fifty-two consecutive robotic-assisted TKA’s performed by two surgeons at two centres were reviewed retrospectively. The exclusion criterion for this study was that final laxity data had to be captured by the digital robotic ligament tensioner. Eleven cases were excluded for missing data. 68 patients from the rKA surgeon and 73 patients from the GB surgeon were included. The indication for TKA for all patients was end-stage osteoarthritis with a K-L grade ≥ 3. Three patients in the rKA group had previous ACL surgery. Both techniques used the same cruciate retaining (CR) implant (Apex) and robotic-assisted system in combination with the BalanceBot™, a digital robotic ligament tensioning device (Corin Ltd, Raynham, MA). Cases were performed between March 2020 and June 2021. The rKA TKA’s were performed by an experienced knee arthroplasty surgeon having performed over 300 KA knees using modified standard instruments and further robotic experience with OMNIBotics performing rKA in over 100 cases. The GB surgeon had performed over 300 robotic GB knees with various robotic platforms and over 150 using the same workflow described in this study.
The digital joint tensioner consists of two active spacing units for the lateral and medial knee compartments (Fig. 1a, b) [32]. The device applies a user specified force to the joint and collects intra-operative laxity data. The device operates in conjunction with a bone mounted robotic cutting guide. In a tibia-first workflow, predictive-gap planning software can virtually place the femoral component and render a post-operative gap prediction throughout flexion. The predictive algorithm uses data from an initial balance assessment performed prior to femoral resections (Fig. 1a). The accuracy and repeatability of the gap measurements has been validated to be within 0.5 mm, with an average variation of 0.25 mm laterally and 0.17 mm medially throughout flexion across multiple trained surgeons [14].
Digital joint tensioning device. The digital joint tensioning device utilizes independent medial and lateral active spacing units which are controlled via the navigation system to measure joint gaps throughout the flexion range. Joint tension is selected by the surgeon. a) In a tibia-first workflow, gap data collected after tibial resection is used for predictive balance. b) In both tibia-first and femur-first workflows, final gap data are collected with the femoral trial in place. c) The system provides a visual representation of the joint gaps throughout the flexion range
rKA was performed with a femur-first workflow, similar to Howell’s philosophy for component alignment [16, 24] but with restricted femoral and tibial coronal resections [19, 28]. Femoral resections were limited to 6° valgus. Tibial resections limited to between 0° and 6° varus. Tibial recuts were performed to achieve balance as required using balance and laxity information provided by the digital joint tensioner.
GB was performed with a tibia-first workflow targeting a neutral proximal tibial resection. Up to 2° of varus was allowed during tibial resection planning using the OMNIBotics system based on the surgeon’s clinical experience, particularly for patients with non-correctable varus deformity. The digital joint tensioner was then inserted into the joint space and the knee was taken through a range of motion to capture the joint gaps. Femoral resections were then adjusted to achieve rectangular ML gaps, and stability throughout the flexion range using the predictive-gap planning software [32]. No limit was placed on femoral rotation. Distal femoral valgus was limited to 2° to the mechanical axis.
For both rKA and GB, post-op laxity was recorded as the knee moved from 90° to 10° flexion with the digital joint tensioner in place of a tibial trial insert (Fig. 1b, c). The force profile started at 70 N in flexion and was ramped linearly to 90 N in extension in all patients. Laxity was defined as the implanted tibial insert thickness subtracted from the gap measured by the digital joint tensioner. A positive laxity value represents a joint compartment which, under the applied force, has a gap larger than the thickness of the combined tibial and femoral prostheses.
ML coronal balance, lateral laxity, and medial laxity were compared at 10°, 25°, 45° and 90°. Overall medial and lateral laxity were compared throughout flexion. In a sub-analysis, medial and lateral laxity was independently normalized to 0 mm at 10° for rKA and GB to account for surgeon extension laxity preferences and allow for comparison of the laxity changes throughout flexion. Pre- and post-operative leg alignment was measured intraoperatively using the robotic system with the knee in full extension and the leg suspended by the heel. Pre-operative alignment was captured prior to making any resections; post-operative alignment was captured after implantation. Resection depth, joint line obliquity (JLO) and alignment were also captured using the robotic system. JLO was defined using the method described by MacDessi et al. as the sum of the lateral distal femoral angle (LDFA) and medial proximal tibial angle (MPTA) [20]. Recuts, soft tissue releases, and final insert thickness usage were also collected and compared. A soft tissue release was recorded if the release was performed above the normal exposure procedure.
Ethics approval was obtained from an independent Institutional Review Board (Bellberry Ltd Approval No. 2020-08-764-A-1).
Statistical analysis
All data were considered normally distributed (Kolmogorov–Smirnov test of ML balance and resection thickness rejected alternate hypothesis, p > 0.05 in all cases). Welch's unequal variances t-tests, variance tests (F-tests), and Chi-squared tests were used where appropriate in comparing demographics, achieved balance, laxity, resection thickness and angles between GB and rKA groups using R4.1.0 [31]. Statistically significant differences are indicated in figures by ‘***’/‘†††’ = p ≤ 0.001; ‘**’/‘††’ = p ≤ 0.01; ‘*’/‘†’ = p ≤ 0.05; with ‘*’ and ‘†’ denoting t and F tests, respectively. A prospective two-sample means power analysis was performed. Using an alpha of 0.05, beta of 0.8, a joint gap balance standard deviation of 1.5 mm with equal sampling ratio and a threshold joint balance difference of 0.75 mm: a minimum of 63 participants were required for each group.
Demographic analyses showed no differences in age, gender, and pre-op deformities between rKA and GB groups. However, mean BMI was 3.5 kg/m2 greater in rKA (p = 0.007), Table 1. Using landmarks collected from the navigation system, a phenotype analysis similar to Jenny et al. indicated 28 unique phenotypes (rKA: 21, GB: 22) were included in this study [12]. The most common being 3° varus medial distal native femur (MDNFA) with 3° varus native tibia (NTA). The proportion of patients within ± 3° MDNFA and ± 3° NTA was similar to a TKA population reported by Jenny et al. (68–70% vs 74%, p > 0.05) [12].
Results
Balance and laxity
Lateral laxity imbalance throughout flexion was observed in both techniques, Fig. 2. Mean ML gap imbalance at 10°, 25°, 45°, and 90° ranged from 0.6 to 1.2 mm for GB and 1.3–2.2 mm for rKA while rKA had greater ML imbalance at 10°, 25°, and 45°, Fig. 2 and Table 2a. rKA had a higher proportion of knees with > 2 mm of ML gap imbalance than GB at 10° (39% vs 14%, p = 0.001), 25° (54% vs 27%, p = 0.003), and 45° (57% vs 29%, p = 0.001), but not at 90° (31% vs 21%, p = N.S.).
GB had greater medial and lateral laxity throughout flexion, Fig. 3 and Table 2b. The average overall increase throughout flexion was 1.9 mm medially and 1.1 mm laterally (p < 0.001), with the largest difference occurring medially at 25° (2.4 vs -0.1 mm, p < 0.001). Medial, lateral and ML flexion-to-extension balance were not significantly different between the two techniques (p ≥ 0.091). GB reported greater medial laxity variance at 25°, while rKA reported greater lateral laxity variance at 90°, Fig. 3 and Table 2b. Lateral flexion laxity was greater than medial flexion laxity and lateral extension laxity in both rKA and GB (p ≤ 0.030). After normalizing laxity curves at 10°, GB laxity remained greater than rKA only at 25° medially (2.0 vs 1.2 mm, p = 0.010) and laterally (2.4 vs 1.8 mm, p = 0.041), Fig. 4.
Bone resections and insert thicknesses
GB resected more medial and lateral distal femur, resulting in 1.7 mm greater mean distal femur resection and 1.5 mm greater total bone resection in extension, Fig. 5 and Table 3. There were no significant differences in tibial resections. GB used minimum thickness tibial inserts (10 mm total tibial construct thickness) more frequently than rKA (59/73 (80.8%) vs. 43/68 (63.2%), p = 0.032).
Comparison of the medial and lateral tibial and femoral resection depths. Total resection (right) is calculated by taking the sum of the average of the medial and lateral tibial resections plus the average of the medial and lateral femoral resections. Medial distal femoral, lateral distal femoral, and total resections are greater in the GB group
Femoral rotation, joint line obliquity, and coronal alignment
External femoral rotation (ER) was greater and more variable with GB versus rKA, Fig. 6 and Table 3. rKA had greater LDFA and MPTA versus GB, Fig. 6b and Table 3. Pre-operative and post-operative coronal alignment were not significantly different between techniques, Fig. 6c and Table 3.
Resection angles and alignments. a) Compare the narrow distribution and neutral femoral rotation in rKA vs. the variable and more externally rotated GB. b) Oblique joint line in rKA compared to the neutral joint line in GB. c) No difference in the means for pre-op alignments between the groups indicating a similar population deformity. Both rKA and GB corrected a varus cohort into slight varus post-op
Bone recuts and soft tissue releases
The frequency of tibial recuts was greater in rKA compared to GB, Table 4. Two releases occurred in rKA in two separate cases, one MCL and one PCL release, for an overall release rate of 3% (2/68). No releases occurred in GB.
Discussion
The most important findings of this study were that (1) both rKA and GB exhibited medial stability with relative lateral laxity throughout the range despite targeting different component alignment; (2) GB improved ML gap symmetry in extension and midflexion but had greater laxity throughout flexion compared to rKA; (3) when normalizing for surgeon preferences in extension, laxity profiles were similar across techniques apart from a minor increase in midflexion laxity with GB; and (4) the tibial recut rate was significantly greater in rKA compared to the predictive GB workflow.
rKA aims to improve ML balance compared to MA by restoring physiologic laxity, targeting a tight extension space, and allowing for lateral flexion laxity. Using a load sensor to compare intercompartmental pressures, rKA has been shown to achieve ML balance within 15 lbs more frequently than MA [19]. ML compartmental forces in unbound KA knees have also been shown to be highest in extension, with the medial compartment tighter than lateral throughout the range [33]. A similar study used a manual maximum stress technique to assess ML laxity and reported rKA patients were tight in extension with mean medial and lateral laxities under 1 mm, and looser in flexion with mean laxities of 2.2 and 4.5 mm, respectively [23]. rKA laxity in the present study showed similar results to both Shelton et al. and McEwen et al. with a tight medial compartment in extension, and lateral laxity throughout the range. Furthermore, 76% of rKA patients in the present study exhibited lateral flexion laxity imbalance similar to McEwen et al., who reported rKA patients with lateral flexion laxity imbalance had significantly better EQ-5D VAS and mean KOOS quality of life at 3.5 years mean follow-up [23].
Golladay et al. reported that patients with an ML load differential of less than 15 lbs at 10°, 45°, and 90° had greater HSS and FJS scores at 6 weeks and 6 months compared to an unbalanced group [7]. GB in the present study showed similar trends to Golladay with mean ML gap imbalance under 1.2 mm at 10°, 45°, and 90° [7]. Keggi et al. [13] recently evaluating the impact of ML balance on patient outcomes in GB and showed improved KOOS scores for patients with ML imbalance < 1.5 mm throughout the range. However, these balance thresholds were in posterior cruciate sacrificing knees with ultra-congruent inserts, and it is not yet known how these balance targets translate to CR GB knees which may favour larger lateral laxity in flexion to facilitate posterior rollback of the lateral femoral condyle [25, 29]. Although GB showed improved ML balance compared to rKA in the present study, it is not yet understood how balance and laxity targets are impacted by the interplay of JLO, implant congruity, and cruciate retention or sacrifice in TKA.
GB having greater laxity than rKA is likely attributed to surgeon preference as soft tissue balancing is inherently subjective [15, 22, 29]. During early use of the robotic system, the GB surgeon observed the final laxity was often tighter than desired in extension and began targeting a looser knee. This is supported from the results as GB resected 1.5 mm more bone in extension and used a thinner insert more frequently. Medial and lateral normalized GB and rKA laxity profiles were similar throughout the range except in midflexion where GB laxity remained greater than rKA both medially and laterally. This small difference in midflexion laxity (Fig. 4) is likely due to GB resecting more distal femur [5, 11, 17]. Resecting more distal femur will translate the implant and its centre of rotation proximally, decreasing the collateral ligament insertion distances and causing relative slack and joint laxity. Maximum laxity has been reported between 10° and 30° flexion, corroborating our findings of maximum laxity occurring at 25° [4]. However, the mean distal femoral resection in GB was only 0.7 mm greater than the 9 mm distal implant thickness. This may be a result of the digital joint tensioner providing accurate joint gap data in combination with a validated predictive algorithm [32]. Preemptive adjustments to implant positioning can be made to avoid excessive midflexion laxity caused by over-resecting the distal femur.
Both techniques corrected their varus population into mild residual varus and both achieved similar ML balance in flexion, albeit through distinct pathways. GB used a neutral joint line in extension and variable ER; rKA used an oblique joint line in extension and neutral ER. The variable ER seen with GB has been shown in multiple studies to not adversely impact outcomes [3, 8, 9, 26]. However, studies to date have only compared GB and rKA (or KA) to MA and no study has directly compared rKA to GB. Thus, it is not yet known if the alteration of femoral anatomy that occurs with GB to achieve balance negatively impacts outcomes in comparison to rKA where balance is achieved through more anatomic implant positioning leading to more natural kinematics with a reduction in the peak knee abduction moment [27].
Limited data exist on the recut frequency of rKA; however, An et al. [1] reported tibial recuts in 4.4% of rKA knees, which is lower than the present study. However, MacDessi et al. reported poor correlation in balance assessment between surgeon estimates and sensor data suggesting surgeons may not always know when recuts could improve balance. Thus, the higher recut rate in the present study may come from the surgeon electing to recut based on the quantitative intraoperative digital joint tensioner data [18].
This study has several limitations. The retrospective nature can potentially introduce various biases. To limit biases, a consecutive group was selected from each surgeon and a demographic analysis showed the only significant difference was a mean difference in BMI of 3.5 kg/m2. Another limitation of this study was that each technique was performed by an individual surgeon which may have confounded the results due to surgeon specific technique preferences. However, both surgeons used a standardized technique with the same robotic system and the same CR implant. Furthermore, a sub-analysis was undertaken with laxity normalized in extension to adjust for variation in surgeon preference for knee tightness or looseness. A limitation, but also a strength, was that a single multi-radius implant design was used. Consequently, the results may not be replicated using a single-radius implant design. Predictive balancing with the digital joint tensioner was not used for both techniques as this technology does not yet exist for femur-first workflows. If predictive balancing were available for rKA, a significant reduction in the tibial recut rate would be expected. Patellofemoral joint instability was not evaluated in either technique. This remains a controversial topic as rKA and GB routinely place the femoral component in a non-neutral coronal alignment and internally rotated. Another limitation of this study was that post-operative JLO was calculated based on resection angles and did not include soft tissue laxity. Lastly, clinical outcomes were not included in this study.
This study successfully characterized balance and laxity differences between two contemporary alignment strategies. Recent literature has shown that the differences found here are large enough to impact patient outcomes [35]. Future work is required to determine how these technique specific differences affect patient outcomes.
Conclusions
Both techniques exhibited relative lateral laxity throughout flexion, while GB had improved ML balance in extension and midflexion. GB exhibited greater laxity with a more neutral joint line and reduced tibial recuts compared to rKA. Despite differences in component alignment, postop coronal alignment was similar between the techniques.
References
An VVG, Twiggs J, Leie M, Fritsch BA (2019) Kinematic alignment is bone and soft tissue preserving compared to mechanical alignment in total knee arthroplasty. Knee 26:466–476
Babazadeh S, Dowsey MM, Vasimalla MG, Stoney JD, Choong PFM (2018) Gap balancing sacrifices joint-line maintenance to improve gap symmetry: 5-year follow-up of a randomized controlled trial. J Arthroplasty 33:75–78
Becker R, Baker K, Hommel H, Bernard M, Kopf S (2019) No correlation between rotation of femoral components in the transverse plane and clinical outcome after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 27:1456–1462
Chalmers BP, Elmasry SS, Kahlenberg CA, Mayman DJ, Wright TM, Westrich GH et al (2021) Additional distal femoral resection increases mid-flexion coronal laxity in posterior-stabilized total knee arthroplasty with flexion contracture : a computational study. Bone Joint J 103:87–93
Cross MB, Nam D, Plaskos C, Sherman SL, Lyman S, Pearle AD et al (2012) Recutting the distal femur to increase maximal knee extension during TKA causes coronal plane laxity in mid-flexion. Knee 19:875–879
Dennis DA, Komistek RD, Kim RH, Sharma A (2010) Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res 468:102–107
Golladay GJ, Bradbury TL, Gordon AC, Fernandez-Madrid IJ, Krebs VE, Patel PD et al (2019) Are patients more satisfied with a balanced total knee arthroplasty? J Arthroplasty 34:S195–S200
Heesterbeek PJ, Jacobs WC, Wymenga AB (2009) Effects of the balanced gap technique on femoral component rotation in TKA. Clin Orthop Relat Res 467:1015–1022
Hernandez-Hermoso JA, Nescolarde-Selva L, Rodriguez-Montserrat D, Martinez-Pastor JC, Garcia-Oltra E, Lopez-Marne S (2020) Different femoral rotation with navigated flexion-gap balanced or measured resection in total knee arthroplasty does not lead to different clinical outcomes. Knee Surg Sports Traumatol Arthrosc 28:1805–1813
Howell SM, Papadopoulos S, Kuznik KT, Hull ML (2013) Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc 21:2271–2280
Huang T, Long Y, George D, Wang W (2017) Meta-analysis of gap balancing versus measured resection techniques in total knee arthroplasty. Bone Joint J 99:151–158
Jenny JY, Baldairon F, Hirschmann MT (2021) Functional knee phenotypes of OA patients undergoing total knee arthroplasty are significantly more varus or valgus than in a non-OA control group. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06687-5
Keggi JM, Wakelin EA, Koenig JA, Lawrence JM, Randall AL, Ponder CE et al (2021) Impact of intra-operative predictive ligament balance on post-operative balance and patient outcome in TKA: a prospective multicenter study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04043-3
Koulalis D, O’Loughlin PF, Plaskos C, Kendoff D, Cross MB, Pearle AD (2011) Sequential versus automated cutting guides in computer-assisted total knee arthroplasty. Knee 18:436–442
Kuster MS, Bitschnau B, Votruba T (2004) Influence of collateral ligament laxity on patient satisfaction after total knee arthroplasty: a comparative bilateral study. Arch Orthop Trauma Surg 124:415–417
Lee YS, Howell SM, Won YY, Lee OS, Lee SH, Vahedi H et al (2017) Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:3467–3479
Luyckx T, Vandenneucker H, Ing LS, Vereecke E, Ing AV, Victor J (2018) Raising the joint line in TKA is associated with mid-flexion laxity: a study in cadaver knees. Clin Orthop Relat Res 476:601–611
MacDessi SJ, Gharaibeh MA, Harris IA (2019) How accurately can soft tissue balance be determined in total knee arthroplasty? J Arthroplasty 34:290-294e291
MacDessi SJ, Griffiths-Jones W, Chen DB, Griffiths-Jones S, Wood JA, Diwan AD et al (2020) Restoring the constitutional alignment with a restrictive kinematic protocol improves quantitative soft-tissue balance in total knee arthroplasty: a randomized controlled trial. Bone Joint J 102-B:117–124
MacDessi SJ, Griffiths-Jones W, Harris IA, Bellemans J, Chen DB (2021) Coronal Plane Alignment of the Knee (CPAK) classification. Bone Joint J 103:329–337
Matsumoto T, Muratsu H, Kubo S, Matsushita T, Ishida K, Sasaki H et al (2012) Soft tissue balance using the tibia first gap technique with navigation system in cruciate-retaining total knee arthroplasty. Int Orthop 36:975–980
McAuliffe MJ, O’Connor PB, Major LJ, Garg G, Whitehouse SL, Crawford RW (2020) Highly satisfied total knee arthroplasty patients display a wide range of soft tissue balance. J Knee Surg 33:247–254
McEwen P, Balendra G, Doma K (2019) Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty. Bone Joint J 101-B:331–339
McEwen PJ, Dlaska CE, Jovanovic IA, Doma K, Brandon BJ (2020) Computer-assisted kinematic and mechanical axis total knee arthroplasty: a prospective randomized controlled trial of bilateral simultaneous surgery. J Arthroplasty 35:443–450
Most E, Zayontz S, Li G, Otterberg E, Sabbag K, Rubash HE (2003) Femoral rollback after cruciate-retaining and stabilizing total knee arthroplasty. Clin Orthop Relat Res. https://doi.org/10.1097/01.blo.0000062380.79828.2e101-113
Murgier J, Clatworthy M (2020) Variable rotation of the femur does not affect outcome with patient specific alignment navigated balanced TKA. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06226-8
Niki Y, Nagura T, Nagai K, Kobayashi S, Harato K (2018) Kinematically aligned total knee arthroplasty reduces knee adduction moment more than mechanically aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26:1629–1635
Nisar S, Palan J, Riviere C, Emerton M, Pandit H (2020) Kinematic alignment in total knee arthroplasty. EFORT Open Rev 5:380–390
Nozaki H, Banks SA, Suguro T, Hodge WA (2002) Observations of femoral rollback in cruciate-retaining knee arthroplasty. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-200211000-00046308-314
Pang HN, Yeo SJ, Chong HC, Chin PL, Ong J, Lo NN (2011) Computer-assisted gap balancing technique improves outcome in total knee arthroplasty, compared with conventional measured resection technique. Knee Surg Sports Traumatol Arthrosc 19:1496–1503
R: A language and environment for statistical computing (2021) R Foundation for statistical computing [computer program]. Version 4.1.0: R Foundation for Statistical Computing
Shalhoub S, Lawrence JM, Keggi JM, Randall AL, DeClaire JH, Plaskos C (2019) Imageless, robotic-assisted total knee arthroplasty combined with a robotic tensioning system can help predict and achieve accurate postoperative ligament balance. Arthroplast Today 5:334–340
Shelton TJ, Howell SM, Hull ML (2019) Is there a force target that predicts early patient-reported outcomes after kinematically aligned TKA? Clin Orthop Relat Res 477:1200–1207
Siddiqi A, Smith T, McPhilemy JJ, Ranawat AS, Sculco PK, Chen AF (2020) Soft-tissue balancing technology for total knee arthroplasty. JBJS Rev 8:e0050
Wakelin EA, Shalhoub S, Lawrence JM, Keggi JM, DeClaire JH, Randall AL et al (2021) Improved total knee arthroplasty pain outcome when joint gap targets are achieved throughout flexion. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06482-2
Funding
This study was funded by Corin Ltd.
Author information
Authors and Affiliations
Contributions
AO was involved with conception and design of the study, was the lead for data analysis and interpretation, as well as the lead manuscript drafter and reviser. EW was involved with conception and design of the study, data interpretation, as well manuscript revisions. CP was involved with conception and design of the study, data interpretation, as well manuscript revisions. JP was involved with conception and design of the study, data collection, data interpretation, as well manuscript revisions. SC was involved with conception and design of the study, data collection, data interpretation, as well manuscript revisions.
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no conflict of interest.
Ethical approval
Ethics approval was obtained from an independent Institutional Review Board (CorinRegistry, Bellberry Ltd Approval No. 2020-08-764-A-1).
Informed consent
Informed consent was not obtained as this project was a retrospective analysis using deidentified data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Orsi, A.D., Wakelin, E.A., Plaskos, C. et al. Restricted kinematic alignment achieves similar relative lateral laxity and greater joint line obliquity compared to gap balancing TKA. Knee Surg Sports Traumatol Arthrosc 30, 2922–2930 (2022). https://doi.org/10.1007/s00167-022-06863-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06863-1