Abstract
Purpose
Achieving a balanced knee is accepted as an important goal in total knee arthroplasty; however, the definition of ideal balance remains controversial. This study therefore endeavoured to determine: (1) whether medio-lateral gap balance in extension, midflexion, and flexion are associated with improved outcome scores at one-year post-operatively and (2) whether these relationships can be used to identify windows of optimal gap balance throughout flexion.
Methods
135 patients were enrolled in a multicenter, multi-surgeon, prospective investigation using a robot-assisted surgical platform and posterior cruciate ligament sacrificing gap balancing technique. Joint gaps were measured under a controlled tension of 70–90 N from 10°–90° flexion. Linear correlations between joint gaps and one-year KOOS outcomes were investigated. KOOS Pain and Activities of Daily Living sub-scores were used to define clinically relevant joint gap target thresholds in extension, midflexion, and flexion. Gap thresholds were then combined to investigate the synergistic effects of satisfying multiple targets.
Results
Significant linear correlations were found throughout extension, midflexion, and flexion. Joint gap thresholds of an equally balanced or tighter medial compartment in extension, medial laxity ± 1 mm compared to the final insert thickness in midflexion, and a medio-lateral imbalance of less than 1.5 mm in flexion generated subgroups that reported significantly improved KOOS pain scores at one year (median ∆ = 8.3, 5.6 and 2.8 points, respectively). Combining any two targets resulted in further improved outcomes, with the greatest improvement observed when all three targets were satisfied (median ∆ = 11.2, p = 0.002).
Conclusion
Gap thresholds identified in this study provide clinically relevant and achievable targets for optimising soft tissue balance in posterior cruciate ligament sacrificing gap balancing total knee arthroplasty. When all three balance windows were achieved, clinically meaningful pain improvement was observed.
Level of Evidence
Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A poorly balanced, unstable or stiff joint is a leading cause of residual pain [36], dissatisfaction [12], and revision after Total Knee Arthroplasty (TKA) [1,2,3, 19, 23]. The quantitative definition of a well-balanced joint, however, remains a source of controversy [17]. Traditional balance (mechanical alignment (MA)) aims to create a neutrally aligned joint (± 3° from mechanical axis) and achieves equal flexion and extension gaps through soft tissue releases [13]. Whereas a gap balancing (GB) approach executes a neutral tibial resection then modifies the femoral component placement to generate equal flexion and extension gaps. Both techniques have suffered from an historic difficulty in accurate characterisation and control of midflexion laxity [24]. As a result, a target joint balance for optimising patient outcomes has not been well-defined.
Golladay et al. measured medial and lateral joint forces through an instrumented tibial trial in extension, and at 45° and 90° flexion using measured resection MA and GB techniques [12]. Knees which were more balanced across an average of all three flexion angles reported significantly improved Knee Society Score (KSS) and Forgotten Joint Score. The study, however, did not investigate the effect of balance at distinct flexion angles on patient outcome.
The relationship between joint balance measurements and patient outcome at flexion angles other than extension (0°–10°) and flexion (90°) has not yet been investigated. Identifying a relationship between TKA balance and outcome throughout flexion may allow the development of intra-operative balancing targets for improved outcomes. This study therefore endeavoured to determine: (1) whether medio-lateral gap balance in extension, midflexion, and flexion are associated with improved KOOS scores at one-year post-operatively and (2) whether these relationships can be used to identify windows of optimal gap balance throughout flexion. The hypotheses were that joint balance under a controlled force is associated with one-year patient outcomes throughout flexion, and that clinically relevant balance windows of improved outcomes can be identified.
Methods
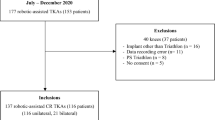
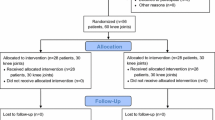
A prospective, investigation involving five surgeons at five sites was performed between November 2017 and December 2018. All patients provided informed consent to participate and IRB approval was obtained from the New England Institutional Review Board (No: 120170260). Patients were eligible if they presented with a diagnosis of end-stage degenerative joint disease and were scheduled to undergo a primary TKA. Exclusion criteria included BMI > 45 kg/m2, neurological disease, diagnosis of cancer, a mental condition that may affect the subject’s ability to respond to questionnaires, joint sepsis, and metal sensitivity. If metal sensitivity was suspected or confirmed by the surgeon, the patient was not offered inclusion in the study.
All surgeries were performed using the OMNIBotics robot-assisted TKA platform and BalanceBot device (Corin Ltd, Rayham, MA, Fig. 1). The posterior cruciate ligament (PCL) was routinely resected and APEX implants (Corin Ltd, Rayham, MA) were used in all cases implanting a CR femoral component with an Ultra-congruent (UC) tibial insert. The patella was resurfaced in all cases. A mixture of tibia-first GB and femur-first (targeting MA) approaches were performed. The alignment philosophies were performed as follows: surgeons using the GB technique targeted a neutral tibial resection followed by a femoral component placement to balance the knee; in the femur first MA technique a neutral tibial and femoral coronal resections, three external femoral rotation and a hip-knee-ankle angle ± 3° was targeted, followed by soft tissue releases to achieve balance; both techniques aim for equal medial and lateral gaps in extension and flexion; however, surgeons were not provided with a prescribed balance target and were free to target any joint balance or gap profile.
After performing the tibial and femoral resections and any final soft tissue balancing, the BalanceBot was inserted into the knee and the final gaps were measured under a digitally controlled load throughout flexion. Medial and lateral joint gaps were recorded by the BalanceBot with the patella reduced and under an applied load of 70–90 N as described by Shalhoub et al. [34]. Accuracy and repeatability of the gap measurements has been reported to be within 0.5 mm, with an average variation of 0.25 mm laterally and 0.17 mm medially throughout flexion across multiple trained surgeons [37]. All surgeons received training on the correct use of the BalanceBot to avoid external forces impacting the data capture. The force applied by the BalanceBot was chosen by the surgeon on a patient-specific basis based on intra-operative feel of the soft tissue properties. While capturing joint gap data, the surgeon supported the femur posteriorly with the tibia in flexion preventing the weight of the femur from affecting the measurement. Adequate support of the superior posterior aspect of the knee was performed by ensuring the heel was not in contact with the operating table during data capture. The knee was then extended with care not to apply a varus/valgus or internal/external rotation force to the joint. In extension, the heel was supported, and the knee was allowed reach full extension, defined as: the position achieved with the heel supported, the posterior surface of the knee raised off the operating table, and without applying additional pressure at the knee. Medial, lateral, and average gaps and the medio-lateral (ML) gap difference were calculated (Fig. 2). The thickness of the final tibial insert implanted was subtracted from the joint gap measurements to give final gap values.
Knee Injury and Osteoarthritis Outcome Score (KOOS) was collected at one-year post-op and were investigated for correlations with the measured joint gaps.
Statistical analysis
Due to the reported ceiling effect observed using the KOOS questionnaire [33], Kruskal–Wallis non-parametric tests were used to determine significant differences between groups, and the median difference reported. Patients were also subdivided into groups which achieved the Patient Acceptable Symptom State (PASS) for further analysis of the pain subscore (> 84.5) [8]. The PASS criteria is a threshold value validated for use in TKA [7, 22]. Patients with individual scores above the relevant PASS threshold value are likely to consider themselves satisfied. In contrast to the minimal clinically important difference (MCID) of 8–10 KOOS points [32], PASS allows the evaluation of the rate of individual satisfaction rather than group differences in scores, although PASS and MCID both identify clinically relevant patient reported outcome measures (PROMs) differences from the patient perspective. Revision operations for study participants were recorded in an online database. Revisions were assessed in October 2020, giving a revision follow-up timeframe of 22–35 months.
Correlations between joint gaps in extension (10–20°), midflexion (30°–40°), and full flexion (> 70°) and KOOS outcome were performed using Spearman’s correlation. A critical p value of 0.05 was used to determine significance. All statistical analysis was performed using R 3.5.3 (R Project, Vienna, Austria).
Results
A total of 135 patients (29 femur first and 106 tibia first technique) received TKA surgery using the BalanceBot device and completed one-year KOOS outcome scores. The patient demographics are typical of a TKA population (Table 1) [1]. Diagnosis for TKA surgery was evaluated during analysis: one hundred thirty-two (132) patients were diagnosed with osteoarthritis, two (2) patients with inflammatory arthritis and one (1) with post-traumatic osteoarthritis.
Soft tissue balance correlated significantly with the KOOS Pain score in extension, midflexion, and flexion. Balance targets were identified at each flexion angle that reported significantly improved pain scores (Fig. 3). These targets are: in extension, equal balance (up to 0.5 mm imbalance on either side) or tighter medially than laterally (p = 0.002); in midflexion, medial laxity within ± 1 mm of the final insert thickness (p = 0.003); and in flexion, absolute balance within 1.5 mm mediolaterally (p = 0.029).
Comparison of KOOS pain subscore at 1 Year between knees which satisfy balance thresholds (Green) and those which do not (Red) throughout flexion. a Extension, threshold is defined as a knee that is equally balanced or tighter medially compared to those tighter laterally, b midflexion, joint gap window is a medial laxity that is equal to the tibial insert thickness ± 1 mm compared to those with a greater gap difference, c flexion, joint gap window is absolute medio-lateral imbalance < 1.5 mm compared to those with a greater medio-lateral imbalance. Thresholds were informed by the results of linear correlations. Median change in score and significance indicated on the figure
Further improved KOOS pain outcomes were found when any two balance targets were combined, see Fig. 4a–c. The distribution of soft tissue balance for each combination of two targets is overlaid by a classification of achieving the KOOS pain PASS threshold of 84.5 [8] in Fig. 4d–f. The proportion of knees that satisfy the PASS criteria is greater in all target combinations than knees which only satisfy one or neither criteria (Flexion/Extension: p = 0.032, Midflexion/Extension: p = 0.040 and Midflexion/Flexion: p = 0.041). The greatest improvement in KOOS pain, however, was found when all three soft tissue balance criteria were achieved (p = 0.002), Fig. 5. Patients which achieved all three balance criteria were more likely to achieve the PASS threshold compared to those who did not satisfy all balance targets (p = 0.040). However, there was no significant difference compared to those who satisfied any two criteria (p = 0.194). No significant differences in patient demographics were found between the study population and patients which satisfied any combination of balance targets, see Table 2.
Comparison of KOOS pain and KOOS PASS percentage resulting from combining two gap windows (Green = satisfied 2 gap windows, Red = does not satisfy 2 gap windows). a–c Box plots showing the change in KOOS pain score when two joint gap windows are combined. Median change in score and significance indicated on the figure. a flexion and extension; b: midflexion and extension; c midflexion and flexion. d–f: Dot plots showing combinations of joint gaps and thresholds identified in Fig. 3. Dot colour denotes patients which have achieved the Patient Acceptable Symptom State (PASS) for 1 year KOOS pain (84.5 points). Green regions denote areas in which both gap criteria defined in a–c are satisfied. Fraction of patients which satisfy the PASS criteria in the green zone vs outside the green zone is indicated on the figure
Soft tissue balance also correlated significantly with the KOOS ADL score in midflexion, and flexion. In flexion, a similar window for improved pain outcome was identified; knees that were balanced within 1.5 mm mediolaterally (p = 0.035, Fig. 6a). In addition, knees that reported less than 1.5 mm residual lateral laxity compared to the implant thickness also reported improved ADL outcomes (p = 0.025, Fig. 6b). No window was identified for coronal imbalance in midflexion.
Comparison of KOOS ADL subscore at 1 Year between knees which satisfy balance thresholds (Green) and those which do not (Red) in flexion. a medio-lateral imbalance in flexion, b Lateral laxity in flexion. Thresholds were defined and informed by linear correlations. Statisitical significance and median difference indicated on the figure
A single revision surgery was recorded during this investigation. The revision was a tibial liner exchange, following instability resulting from a fall, injuring the MCL after one-year KOOS scores were recorded. Prior to the fall, the patient satisfied the midflexion and flexion balance criteria and reported a one-year KOOS pain score of 91.7.
All correlations investigated between intra-operative gap measurements and KOOS scores are reported in the Appendix.
Discussion
The most important finding of this study was that knees which satisfied intra-operative gap thresholds in extension, midflexion, and flexion, reported an improvement in the median KOOS Pain outcome beyond the MCID [32] compared to knees that did not achieve these gap windows.
Although ligament balance and laxity are known to affect TKA success, few studies have associated optimal ranges for gap balance throughout flexion with clinical outcomes. In this study, post-operative medial and lateral joint gaps as well as coronal joint imbalance were investigated for correlations with KOOS outcomes. KOOS Pain scores correlated with gap and imbalance measurements across all flexion angles investigated and allowed clinically achievable windows of improved outcomes to be defined. KOOS ADL scores correlated with gap and imbalance in midflexion and flexion, and clinically relevant windows of improved outcomes were defined in flexion.
A balanced or medially favoured extension space has previously been correlated with improved PROMs and function outcomes by Kamenaga and Tsukiyama [20, 37] in agreement with pain results presented here. In these studies and other work by Azukizawa et al. [5], flexion joint balance was also investigated with post-operative outcomes favouring a balanced joint in which medial stability was preserved throughout flexion. Azukizawa reported reduced KSS scores in knees with ≥ 4 mm medial laxity in flexion. This result, however, is not repeated here and may be due to different data ranges. Azukizawa reported 61% (28/46) of knees with ≥ 4 mm medial laxity in flexion; however, the data presented here only report 4% (6/135) of knees with this amount of laxity. Furthermore, the low rate of high coronal imbalance measured in extension has prevented identification of an association between excessively medially favoured imbalance and worse pain outcomes. As such, the results from this study are unable to define an outer boundary to the extension threshold target.
The results support findings of improved pain outcomes when medial stability is preserved, albeit in midflexion, and improved pain and ADL outcomes when a balanced knee in flexion is achieved. Aunan et al. [19] examined joint gaps statically at full extension and at 90° flexion and showed a negative correlation of increasing medial laxity with KOOS Pain scores. Gustke et al. [4, 14] have investigated the impact of joint pressures and found a more balanced knee, with coronal imbalance < 15 lbs, correlated with improved early KSS and KOOS outcomes but did not investigate the effect of imbalance at individual flexion angles. Within this cohort, achieving multiple balance targets throughout flexion produced an additive improvement in outcome as well as support findings of improved outcomes when a knee is balanced dynamically throughout the range of motion with a consistent, internally applied force. One of the drivers behind this additive effect may be that when all balance targets are satisfied, medial stability is maintained throughout flexion. This medial ligament isometry and other combinations of coronal balance between flexion angles may represent a further joint gap target for improved outcomes.
In contrast, studies which targeted Kinematic Alignment (KA) have found that greater lateral laxity in flexion [26] correlates with improved OKS and KOOS scores. KA is predominately a cruciate retaining approach while all knees in this study had the PCL resected. The presence of the PCL restraint on the medial compartment, particularly in flexion, combined with non-neutral alignment in KA may be responsible for a different target balance in flexion for improved outcomes. Furthermore, all tibiae in the present study were targeted with a neutral coronal resection. Tibia native coronal angles are varied and patient-specific [6] such that a neutral tibial coronal resection represents a significant deviation from the native articulating surface and modification to the resultant knee kinematics. This represents a different kinematic environment than KA which balances the joint by modifying the tibial component placement after resurfacing the femur [18]. Soft tissue balance targets, therefore, may not be the same across all techniques and may explain why a more balanced knee in flexion is found here to be optimal rather than a trapezoidal lateral flexion gap favoured by KA [31]. Ideal target balance, therefore, remains a controversial topic that may be technique dependent. The present study provides further insight into target ligament balance using a cruciate sacrificing, tibial first gap balancing technique.
There are several limitations to this study. It is unknown if the ideal distraction force for TKA is between 70 and 90 N. It is possible that the ideal force is patient-specific and based on the individual’s ligament properties. The force used here was chosen as it has previously been demonstrated to be safe clinically [16, 28], and assessed by experienced orthopaedic surgeons to result in suitable post-operative stability. Applying a greater distraction force, however, may result in an overly tight joint and an externally rotated femoral component when using a gap balancing technique [29]. The relationship between applied force, ligament response and patient outcomes, therefore, is the subject of ongoing investigation. PCL sacrificing TKA using a UC tibial insert only was investigated in this study. Femoral rollback and flexion balance when using a PS insert or a PCL retaining technique are expected to differ significantly. Further investigation is required to determine if these targets are applicable to other implant types. A mixture of GB and femur first MA approaches were used in this study. Although both techniques target a neutral tibial resection, the method of achieving joint balance is different. In GB, balance is achieved by modifying the femoral component placement; however, in an MA technique, final balance is achieved through soft tissue release. The impact of soft tissue releases on outcome in this cohort was not investigated. KOOS scores in this study were collected at one-year post-surgery. Additional time points should be considered to build a more complete picture of the impact of joint balance on patient outcomes during short-term recovery and long-term survival. The effect of joint balance on outcome may be present at both earlier (e.g. 3 and 6 months) as well as later (e.g. 2 years) time points. For example, Connelly, et al. showed improving KOOS scores between 1 and 3 years post-operatively [8]. Conversely, Nilsdotter et al. reported KOOS scores that peaked at one year and were lower at the 5 year interval [30]. Additionally, Giesinger and colleagues evaluated the responsiveness of PROMs, including WOMAC but not KOOS specifically [11]. After one-year WOMAC and most other measures were much less responsive to changes in outcome compared to earlier intervals. Consideration of additional noise in early outcome data that may be associated with joint swelling and healing regardless of the soft tissue balance will be needed to understand the independent effect of balance on the knee. Later time points will need to consider the effect of soft tissue remodelling as part of the post-TKA kinematic environment. Revision data, however, were recorded for all participants. A low rate of revision was reported, in which only 1 tibial insert was revised due to a patient fall, indicating the balancing technique employed here did not result in an increase in early implant failure. Murer et al. [27], have identified threshold joint gaps in extension (medial: 5.2 mm, lateral: 4.6 mm) and midflexion (medial: 6.1 mm, lateral: 5.7 mm) associated with an increased risk of revision under a valgus and varus stress of 15 N. Although these thresholds were obtained using a different method, the result indicates that a high level of imbalance is required to predispose a knee to revision TKA. The imbalance observed in this study does not exceed these thresholds, consistent with the low revision rate observed. The gap data investigated here are not normalised for patient-specific anatomic, demographic or pre-operative outcome data. Previous literature has reported several pre-operative factors that are predictive of patient outcome [9, 15, 25, 38, 39]. Major demographic factors such as age, sex, and BMI were not found to be significantly different between groups that satisfied different combinations of target windows indicating an absence of selection bias. The gap windows identified here, therefore, can be interpreted as population-wide targets within the cohort under investigation for minimising post-operative pain. Future investigations of pre-operative patient factors and post-operative outcomes such as activity, mental health, disease progression, native laxity, range of motion (ROM) or pain catastrophising scores may allow further subdivisions of patients and gap targets for optimising a variety of patient outcome measures (e.g. post-operative ROM, activity level, satisfaction) [9, 35].
This investigation was able to successfully characterise three joint gap windows for identifying improved pain outcomes. Combining these windows identified subgroups of patients who reported further improved outcomes with the greatest improvement identified in patients which satisfied all target windows. The digital ligament tensioning tool used in this study has previously been shown to predict and achieve post-operative joint gaps based on femoral component planning reliably with sufficient accuracy to execute the windows described in this study [34]. However, a substantial proportion of knees in this study did not achieve the balance windows. In this study, surgeons were not advised on an optimal joint balance, however, robotic arthroplasty surgeons can now use these targets with digital tensioning tools to achieve a joint balance for improved pain outcomes.
While incremental costs may represent a significant barrier against broader adoption of robotic technology at present, some early reports suggest that use of such technologies may lead to reduced readmissions, revisions and 90-day episode of care costs along with functional improvements which may help to offset costs and increase future adoption [10, 21]. Further research is required to better understand how these potential benefits, along with improved intra-operative balance targets, will impact the value equation.
Conclusions
Using a digitally controlled distraction device, intra-operative joint gaps were found to correlate with one-year post-operative outcomes throughout flexion. By combining joint gap target windows in extension, midflexion and flexion, subpopulations were identified with clinically significant improved pain outcomes.
References
Australian Orthopaedic Association National Joint Registry Annual Report. 2019; 221. Available at: https://aoanjrr.sahmri.com/annual-reports-2019.
National Joint Registry (UK) (2018) 137. Available at: https://reports.njrcentre.org.uk/.
Swedish Knee Arthroplasty Registry, Annual Report. 2018; 39. Available at: http://myknee.se/en/publications/annual-reports.
Aunan E, Kibsgård TJ, Diep LM, Röhrl SM (2015) Intraoperative ligament laxity influences functional outcome 1 year after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23(6):1684–1692
Azukizawa M, Kuriyama S, Nakamura S, Nishitani K, Lyman S, Morita Y et al (2018) Intraoperative medial joint laxity in flexion decreases patient satisfaction after total knee arthroplasty. Arch Orthop Trauma Surg 138(8):1143–1150
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) Is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop 470(1):45–53
Bonnefoy-Mazure A, Lübbeke A, Miozzari HH, Armand S, Junior YS, Turcot K, et al. (2020) Walking speed and maximal knee flexion during gait after total knee arthroplasty: minimal clinically important improvement are not determinable; patient acceptable symptom state are potentially useful. J Arthroplasty:2865–2871
Connelly JW, Galea VP, Rojanasopondist P, Matuszak SJ, Ingelsrud LH, Nielsen CS et al (2019) Patient acceptable symptom state at 1 and 3 years after total knee arthroplasty: thresholds for the Knee Injury and Osteoarthritis Outcome Score (KOOS). J Bone Joint Surg Am 101(11):995–1003
Connelly JW, Galea VP, Rojanasopondist P, Nielsen CS, Bragdon CR, Kappel A et al (2020) Which preoperative factors are associated with not attaining acceptable levels of pain and function after TKA? Findings from an international multicenter study. Clin Orthop 478(5):1019–1028
Cool CL, Jacofsky DJ, Seeger KA, Sodhi N, Mont MA (2019) A 90-day episode-of-care cost analysis of robotic-arm assisted total knee arthroplasty. J Comp Eff Res 8(5):327–336
Giesinger K, Hamilton D, Jost B, Holzner B, Giesinger J (2014) Comparative responsiveness of outcome measures for total knee arthroplasty. Osteoarthr Cart 22(2):184–189
Golladay GJ, Bradbury TL, Gordon AC, Fernandez-Madrid IJ, Krebs VE, Patel PD et al (2019) Are patients more satisfied with a balanced TKA? J Arthroplasty 34(7):S195–S200
Griffin FM, Insall JN, Scuderi GR (2000) Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty 15(8):970–973
Gustke KA, Golladay GJ, Roche MW, Elson LC (2014) Anderson CR (2014) Primary TKA patients with quantifiably balanced soft-tissue achieve significant clinical gains sooner than unbalanced patients. Adv Orthop 1:1–6
Halawi MJ, Jongbloed W, Baron S, Savoy L, Williams VJ, Cote MP (2019) Patient dissatisfaction after primary total joint arthroplasty: the patient perspective. J Arthroplasty 34(6):1093–1096
Higuchi H, Hatayama K, Shimizu M, Kobayashi A, Kobayashi T, Takagishi K (2009) Relationship between joint gap difference and range of motion in total knee arthroplasty: a prospective randomised study between different platforms. Int Orthop 33(4):997–1000
Hirschmann MT, Becker R, Tandogan R, Vendittoli P-A, Howell S (2019) Alignment in TKA: what has been clear is not anymore! Knee Surg Sports Traumatol Arthrosc:2037–2039
Howell SM, Hull ML, Mahfouz M (2014) Kinematic alignment in total knee arthroplasty. Arthropaedia 1(1):44–53
Hughes RE, Zheng H, Hallstrom BR (2018) Michigan arthroplasty registry collaborative quality initiative (MARCQI) report: 2012–2017. University of Michigan. Ann Arbor:39
Kamenaga T, Muratsu H, Kanda Y, Miya H, Kuroda R, Matsumoto T (2018) The influence of postoperative knee stability on patient satisfaction in cruciate-retaining total knee arthroplasty. J Arthroplasty 33(8):2475–2479
Kayani B, Konan S, Tahmassebi J, Pietrzak J, Haddad F (2018) Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J 100(7):930–937
Kvien TK, Heiberg T, Hagen KB (2007) Minimal clinically important improvement/difference (MCII/MCID) and patient acceptable symptom state (PASS): what do these concepts mean? Ann Rheum Dis 66(suppl 3):40–41
Le DH, Goodman SB, Maloney WJ, Huddleston JI (2014) Current modes of failure in TKA: infection, instability, and stiffness predominate. Clin Orthop 472(7):2197–2200
Longo UG, Candela V, Pirato F, Hirschmann MT, Becker R, Denaro V (2020) Midflexion instability in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc:1–11
Lungu E, Desmeules F, Dionne CE, Belzile ÉL, Vendittoli P-A (2014) Prediction of poor outcomes six months following total knee arthroplasty in patients awaiting surgery. BMC Musculoskelet Disord 15(1):299–310
McEwen P, Balendra G, Doma K (2019) Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty. Bone Joint J 101(3):331–339
Murer M, Falkowski A, Hirschmann A, Amsler F, Hirschmann MT (2020) Threshold values for stress radiographs in unstable knees after total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy: Official Journal of the ESSKA
Nagai K, Muratsu H, Matsumoto T, Miya H, Kuroda R, Kurosaka M (2014) Soft tissue balance changes depending on joint distraction force in total knee arthroplasty. J Arthroplasty 29(3):520–524
Nagai K, Muratsu H, Takeoka Y, Tsubosaka M, Kuroda R, Matsumoto T (2017) The influence of joint distraction force on the soft-tissue balance using modified gap-balancing technique in posterior-stabilized total knee arthroplasty. J Arthroplasty 32(10):2995–2999
Nilsdotter A-K, Toksvig-Larsen S, Roos E (2009) A 5 year prospective study of patient-relevant outcomes after total knee replacement. Osteoarthr Cart 17(5):601–606
Rivière C, Lazic S, Boughton O, Wiart Y, Vïllet L, Cobb J (2018) Current concepts for aligning knee implants: patient-specific or systematic? EFORT Open Rev 3(1):1–6
Roos E. KOOS FAQs. 2019; http://www.koos.nu/index.html. Accessed Dec 13, 2019.
Roos EM, Toksvig-Larsen S (2003) Knee injury and Osteoarthritis Outcome Score (KOOS)–validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 1(1):1–10
Shalhoub S, Lawrence JM, Keggi JM, Randall AL, DeClaire JH, Plaskos C (2019) Imageless, robotic-assisted total knee arthroplasty combined with a robotic tensioning system can help predict and achieve accurate postoperative ligament balance. Arthroplasty Today 5(3):334–340
Sheth NP (2020) Which preoperative factors are associated with not attaining acceptable levels of pain and function After TKA? Findings from an International Multicenter Study. Clin Orthop 478(5):1029–1030
Siddiqi A, Smith T, McPhilemy JJ, Ranawat AS, Sculco PK, Chen AF (2020) Soft-tissue balancing technology for total knee arthroplasty. J Bone Joint Surg Am 8(1):1–15
Tsukiyama H, Kuriyama S, Kobayashi M, Nakamura S, Furu M, Ito H et al (2017) Medial rather than lateral knee instability correlates with inferior patient satisfaction and knee function after total knee arthroplasty. Knee 24(6):1478–1484
Twiggs JG, Wakelin EA, Fritsch BA, Liu DW, Solomon M, Parker D et al (2019) Clinical and statistical validation of a probabilistic prediction tool of total knee arthroplasty outcome. J Arthroplasty 34(11):2624–2631
Van Onsem S, Van Der Straeten C, Arnout N, Deprez P, Van Damme G, Victor J (2016) A new prediction model for patient satisfaction after total knee arthroplasty. J Arthroplasty 31(12):2660–2667
Acknowledgements
The authors would like to acknowledge the critical data collection and study administration performed by: Jayne Crofut, Katie Mabee, Sharon Stewart, Cindy Murphy, Kathryn Darley and Alex Friedl, and the data processing and analysis performed by Anna Geraghty. We dedicate this work to the memory of Dr. Leonid Dabuzhsky, 1952 –2019. Dr Dabuzhsky was extremely passionate and actively involved in this project from the start. His contribution was immense, and his unwavering dedication to his patients’ care will continue to inspire us.
Funding
No external funding was provided for this study.
Author information
Authors and Affiliations
Contributions
EW designed study, performed statistical analysis, interpretation of results and drafted manuscript. SS designed study, assisted in interpretation of results and edited manuscript, JL, JK, JD, AR, CEP, JAK assisted in study design, performed clinical data capture and clinical interpretation of results, and reviewed manuscript, SL developed and reviewed statistical analysis methodology and assisted in drafting and editing the manuscript, CP conceived and designed study, assisted in interpretation of results and drafting and editing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
EW, SS: paid employees of Corin. CP: paid employee, stock options in Corin. JL: paid consultant and speaker to Corin and Stryker. JK: paid consultant, speaker and research support from Corin. JD: paid consultant, speaker and research support Corin, Smith and Nephew and Zimmer Biomet. Royalties from Zimmer Biomet AR: paid consultant, speaker and research support to Corin. CEP: paid consultant, speaker, research support and Royalties from Corin. Paid consultant to Styker and Med 7. Share holder of Joint Development LLC JAK: paid consultant, research support, paid speaker and royalties from Corin SL: paid consultant from Corin and Cell Source (Tokyo).
Ethical approval
Ethical approval was obtained for this study through New England Independent Review Board (No: 120170260).
Informed consent
Informed consent was obtained for all patients within this study before participating in study protocol.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wakelin, E.A., Shalhoub, S., Lawrence, J.M. et al. Improved total knee arthroplasty pain outcome when joint gap targets are achieved throughout flexion. Knee Surg Sports Traumatol Arthrosc 30, 939–947 (2022). https://doi.org/10.1007/s00167-021-06482-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06482-2