Abstract
Purpose
Femoral rotation in total knee arthroplasty (TKA) is hypothesized to vary in the same knee depending on the method used to establish it.
Methods
Thirty-eight patients who underwent TKA surgery using a measured resection technique (RT) were compared with 40 patients who underwent a flexion-gap balancing technique with computer-assisted (for navigation) surgery (FB-CAS) to assess clinical and radiographic alignment differences at two years postoperatively. In 36 of the 40 patients in the FB-CAS group, both methods were used. Intraoperatively, the transepicondylar femoral rotation (TEFR) in reference to the transepicondylar axis was established as the rotation that balanced the flexion gap. Once the TEFR was obtained, an analogous rotation as measured by a posterior reference femoral rotation (PRFR) cutting guide was determined.
Results
Femoral component rotation determined by the TEFR and PRFR methods differed in each of the knees. The median TEFR was 0.08°±0.6° (range − 1.5°, 1.5°), and the median PRFR was 0.06°±2.8° (range − 6°, 5°). The mean difference in the rotational alignment between the TEFR and PRFR techniques was 0.01° ± 3.1°. The 95% limits of agreement between the mean differences in measurements were between 6.2° external rotation and − 6.1° internal rotation. At 2 years postoperatively, we found no differences in the radiographic or clinical American Knee Society score between the two groups.
Conclusion
Rotation of the femoral component in TKA can vary in the same knee depending on the surgical method used to establish it. This variation in femoral rotation is sufficiently small enough to have no apparent effect on the 2-year clinical outcome score.
Level of evidence
II.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Malalignment of total knee arthroplasty (TKA) components in the coronal, sagittal, and axial planes alters knee biomechanics and peak contact forces [3] and increases the risk of poor functional outcome. The rotational alignment of the femoral component has a direct impact on patellar tracking and flexion gap balance, and it can influence patellar stability and wear, knee flexion stability, range of motion [17], and polyethylene wear [3]. However, it is unclear whether the best practise is to insert a femoral component to reproduce the patient’s anatomic femoral rotation or to insert the component in a new way to accommodate the joint kinetics and kinematics created by the bone resections, implant geometry, implant placement, and ligament releases [13]. It is also unknown how best to create the proper alignment once a goal is established.
Computer-assisted surgery (CAS) can improve TKA alignment in the frontal and sagittal planes [4, 10, 14, 28], although it is unclear whether CAS increases implant survivorship [14]. Patient-specific guides have shown conflicting results that question whether they improve the accuracy of component alignment [25] or femoral rotation [7] compared with the traditional mechanical guides or results that suggest patient-specific guides may reduce outliers in all planes, but lead to weakness in sagittal orientation [15].
The literature reflects a growing interest in establishing whether navigation improves rotational alignment relative to the traditional mechanical guides and whether it more accurately reproduces the true anatomical femoral rotation axis [10, 19, 23, 26, 28]. Some studies favour navigation, including those comparing pre- and post-operative femoral rotation on computer tomography (CT) scans in CAS surgery [23] or those comparing CAS versus standard techniques [10]. Other studies question the usefulness of navigation, including those analysing the transepicondylar femoral rotation (TEFR) angle with post-operative CT [28], reviewing the effectiveness on CT femoral rotational alignment between imageless CAS and traditional TKA [19], and characterising the variability associated with femoral rotation obtained by CAS with respect to traditional techniques used on cadaveric specimens [26].
A systematic review of 17 studies [19] comparing the femoral rotation obtained by CAS with the traditional techniques found that the authors did so in different knees without taking into account the influence of knee anatomy [20], deformity due to degenerative changes [5, 16], and/or small [5, 9] or large [9, 16, 24] ligament release. To avoid these factors, a comparison of femoral rotation obtained by different techniques should be made in the same knee during the same surgical procedure [7, 9, 15]. No study has evaluated whether navigation will establish a different femoral rotation alignment compared with the traditional mechanical guides in the same knee during the same surgical procedure.
This study investigated whether the femoral rotation established by CAS and a classic posterior referencing cutting guide would differ in the same knee during the same surgical procedure. A second objective was to ascertain whether the short-term functional clinical scores would differ between the two techniques.
Materials and methods
A prospective, non-randomised, study was performed in 78 patients with painful primary osteoarthritis, who were non-responding to non-operative treatment and undergoing TKA with a maximum of 10° fixed varus or valgus alignment. Patients who met the requirements and accepted to participate were consecutively recruited to the first group and then to the other, but excluding all patients who had previous fractures of the femur or tibia or who had previous tibial or femoral osteotomy to avoid any degree of rotational alteration.
The clinical scores and radiographic alignment of a group of 38 patients who underwent TKA surgery by a measured resection technique (RT) that used a posterior referencing cutting guide were compared to a second group of 40 patients who were operated on using a flexion-gap-balancing technique with computer-assisted surgery (FB-CAS). Five patients in the RT group and one patient in the FB-CAS group were lost to follow-up at 2 years post-operatively due to medical issues; in one patient in each group, the radiographic alignment could not be evaluated due to loss of post-operative radiographs. The average age was 69.9 ± 7.4 and 70.2 ± 6.7 years in the RT and FB-CAS groups, respectively. Twenty-nine women were in the RT group and thirty-one were in the FB-CAS group. Nineteen patients in the RT group and twenty-three in the FB-CAS group underwent surgery on the right knee.
To establish the differences in rotational alignment achieved between the two methods, rotational alignment in 36 of the 40 patients in the FB-CAS group was determined using both methods, but the implants were inserted using the FB-CAS method. It was presumed that the mean and variations in the differences between the two methods would apply to any differences in both the RT group (38 patients) and FB-CAS group (40 patients).
A single surgeon (JAHH) performed all surgical procedures with a cemented PS ScorpioR (Stryker, Mahwah, NJ, USA) prosthesis. Antibiotic and thromboembolic prophylaxis was used in all patients. All were operated under tourniquet with a parapatellar approach, and all underwent the same post-operative protocol. Patellar resurfacing was performed in all procedures by subluxing the patella. The drain was removed after 24 h, and passive and active knee motion was initiated immediately, allowing sitting and ambulation to be tolerated.
In the RT group, bone cuts were first performed, followed by ligament balancing in extension. The proximal tibia cut was made perpendicular to the mechanical axis in the antero-posterior (AP) and sagittal planes with the aid of an extramedullary guide. The distal femoral cut, perpendicular to the mechanical axis in the AP and sagittal planes, was performed with the aid of an intramedullary guide. Three degrees of external femoral rotation were applied in all patients with a posterior referencing cutting guide that allowed a range of external to internal rotation (IR) from 0° to 9°. The external rotation (ER) of the guide was always 3° of ER and was not adjusted regardless of varus or valgus alignment. Staged ligamentous releases to balance flexion–extension gaps were performed as needed. In varus knees, the deep medial collateral ligament was released after medial arthrotomy by removing approximately 1 cm of periosteum from the tibia. All medial osteophytes were removed. A minor release of the posterior medial capsule was performed if the knee was tight. Rarely, a major release of the superficial medial collateral ligament or semimembranosus was needed. The valgus knees were balanced, removing all lateral osteophytes, and a minor release of the lateral posterior capsule was performed if the knee was tight. No major releases of the popliteus tendon, fibular ligament, or lateral intermuscular septum on the femur were needed. No lateral releases or additional femoral recuts were performed.
In the FB-CAS group, we used a wireless image-free CAS system (Stryker NAV3i platform) with OrthoMap-PrecisiónR (Botzinger STR, 41.7911; Freiburg, Germany) knee navigation software. We then placed the active wireless trackers bicortically, one in the femur and another in the tibia, and palpated the medial and lateral epicondyles with an optically tracked stylus that allowed us to establish the transepicondylar axis and subsequently map the distal surface of the epicondyles to digitally simulate the patient’s anatomy and bone cuts. The proximal tibia cut was perpendicular to the mechanical axis in the AP and sagittal planes. The distal femoral cut was perpendicular to the mechanical axis in the AP plane and flexed to 3° of flexion in the sagittal plane. Staged ligament releases were performed to balance the extension gap as described above, with the help of a manual tensor device until a rectangular gap was obtained with tensed medial and lateral ligaments and a neutral mechanical axis (Fig. 1a). The flexion gap was balanced at 90° of knee flexion using a manual tensor ligament device by simulating computer changes in the size and rotation of the femoral component (Fig. 1b). No major releases of the popliteus tendon, fibular ligament, or lateral intermuscular septum on the femur were needed. No lateral releases or additional femoral recuts were performed.
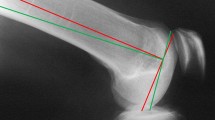
a CAS extension gap balancing. A computer screen image shows virtual extension gap balancing to obtain a rectangular extension gap and a knee mechanical axis with 0° of varus or valgus. b CAS flexion gap balancing. A computer screen image shows virtual flexion gap balancing to obtain a rectangular flexion gap equal to the extension gap; a 1° of internal TEFR was needed in this case. c Posterior referencing cutting guide and the CAS tracker. The free active wireless tracker was inserted into a posterior referencing cutting guide to determine the PRFR value in this device that was equivalent to the previous TEFR value in the same knee during the same surgical procedure. We subtracted 3° of external rotation from the posterior referencing cutting guide femoral rotation to obtain the rotation of this device (in degrees) that balances the flexion gap in relation to the optimal value of 0° of the established CAS transepicondylar axis. This rotation was called the posterior reference femoral rotation (PRFR)
Among the 36 patients in the FB-CAS group, the TEFR was obtained as the rotation in degrees that balanced the flexion gap in relation to the optimal value of 0° of the established CAS transepicondylar axis (Fig. 1b). Once the TEFR was determined, the free active wireless tracker was inserted in a posterior referencing cutting guide to determine the rotation value of the cutting guide that was equivalent to the previous TEFR value in the same knee during the same surgical procedure (Fig. 1c). Assuming that there was a consistent relationship of 3° of ER between the transepicondylar axis and the posterior condylar axis, in an ideal situation 3° of ER of the posterior referencing cutting guide corresponds with 0º of rotation about the transepicondylar axis. We subtracted 3° of ER from the posterior referencing cutting guide rotation to obtain the rotation in degrees that balanced the flexion gap in relation to the optimal value of 0° of the established CAS transepicondylar axis. This rotation was called the posterior reference femoral rotation (PRFR).
In each of the 36 knees assessed with both approaches during the same surgical procedure, we compared the degrees of femoral component rotation to balance the flexion gap achieved by the TEFR and PRFR methods against the optimal value of 0° of the established CAS transepicondylar axis. After verifying the normal distribution of the difference between the two methods (using the Shapiro–Wilk test), the agreement between the measurements obtained from the TEFR and PRFR techniques was assessed with the Bland–Altman method [2]. The 95% limits of agreement were estimated by the mean difference ± 1.96 standard deviations (SDs) of the differences.
One blinded observer (DRM) not involved in the surgical procedures examined all patients using the American Knee Society (AKS) clinical [11] and radiographic [6] protocols at the 2-year post-operative follow-up, during which post-operative AP weight-bearing radiographs and lateral and 30º axial knee radiographs were acquired for all patients. On the radiographs, the AP femoral and tibia component angle, AP total knee angle, lateral femoral component angle, lateral tibia component angle, axial 30° patellar angle, and patellar height were determined. Radiographic measures were taken with a semiautomatic software system (RAIM Viewer® version 2.5.0.511). All patients completed an informed consent form; the authors of Hospital Ethics Committee approved this work (institutional review board approval number AC-14-033) that was performed according to the ethical standards of the 1964 Declaration of Helsinki and its later amendments.
Statistical analysis
The normal distribution of the data was confirmed using the Shapiro–Wilk test. With an α-level of 0.05, a β-level of 0.20 (80% power), and with an estimated difference set at mean + 1.96 SD and a maximum allowed difference between methods set at 13°, a desired sample size of 36 was calculated using MedCalc statistical software version 19.0.3 (MedCalc Software bvba, Ostend, Belgium) to assess agreement between the two methods of measurement using the Bland–Altman test. Qualitative clinical variables and radiographic quantitative variables are presented descriptively as the arithmetic means, standard deviations, 95% confidence intervals of the means, and minimum and maximum of the evaluated values (Tables 1 and 2). The differences in clinical and radiographic variables between the two groups were analysed using ANOVA for equality of variances. The analyses were performed using statistical software IBM® SPSS® version 24.0 (IBM Corp.; Armonk, NY, USA). The statistical significance was set at P < 0.05.
Results
Femoral component rotation by the TEFR and PRFR methods differed in the knee of each patient (Fig. 2). The median TEFR was 0.08° ± 0.6° (range − 1.5°, 1.5°), and the median PRFR was 0.06° ± 2.9° (range − 6°, 5°).
The mean difference of the rotational alignment between the TEFR and PRFR techniques was 0.01° ± 3.1°, with 95% limits of agreement of the mean differences in measurements expected to fall between 6.2° ER and − 6.1º IR.
We found no difference (n.s.) in the short-term AKS total score between the RT and FB-CAS groups (Table 1). AKS pain and AKS functional scores were also similar in both groups. There were no differences (n.s.) in the range of motion between the RT and FB-CAS groups, 102° ± 16° and 106° ± 12°, respectively.
In the radiographic analysis (Table 2), there were no differences between the RT and FB-CAS groups in AP total angle (n.s.), AP femoral component angle (n.s.), AP tibial component angle (n.s.), lateral tibia angle (n.s.), axial 30º patellar angle (n.s.), or patellar height (n.s.). We found a difference of 1.39° (P = 0.00) in the lateral femoral component angle between the RT and FB-CAS groups due to the surgical technique.
Discussion
The most important finding of the present study is that there was a discrepancy in the femoral component rotation in TKA depending on the technique chosen in the same knee during the same surgical procedure, although the difference in the rotational alignment between the two techniques was small and unlikely of any clinical importance. There are several methods to establish total knee femoral component rotation using different anatomical knee reference axes or planes [12], but apparently none of the methods produce femoral component rotation in a precise and reproducible way [26, 28, 29]. There is no consensus regarding the usefulness of navigation to reproduce [10, 23] or to not reproduce [19, 26, 28] femoral rotational malalignment. Rarely, the femoral rotation obtained by different techniques has been studied in the same surgical procedure [7, 9, 15] or knee [26], but no study has determined whether navigation will establish a different femoral rotation alignment compared with the traditional mechanical guides in the same knee during the same surgical procedure.
In a systematic review of randomised and non-randomised control trials comparing CAS TKA with conventional TKA, Meijer et al. [19] found a mean difference in femoral rotation from − 0.64° to 1.9° and a 95% confidence interval between − 1.09° IR and 2.44° ER. We cannot directly compare these findings with ours, because they analysed the difference in femoral rotation with respect to the anatomical transepicondylar axis on the post-operative CT images in different groups and knees, while we analysed the difference in femoral rotation with respect to the CAS transepicondylar axis in the same knee and surgical procedure. Nonetheless, both studies found differences between the two techniques. Comparing the femoral rotational alignment obtained with the flexion gap versus the posterior condylar reference technique, Laskin [16] found a relatively consistent rotation of 3.2° ± 0.3° of ER for neutral and varus knees and a higher and less consistent rotation of 10.1° ± 4.2° in knees with more than 10° of valgus. Heesterbeek et al. [9] reported substantial interpatient variability in femoral component rotation, ranging from 4° IR to 13° ER, in patients who underwent a balanced gap implantation technique referenced from the posterior condyles.
The femoral rotation discrepancy likely occurs for several reasons. First, the inter-individual variability in the angle between the posterior condylar axis and the transepicondylar axis may contribute to rotational discrepancy [20]. This variability ensures differences in rotation between methods based on a predetermined value. The second is the imprecision in CAS determination of the transepicondylar axis [26, 28]. Third, the increase in IR or ER of the distal part of the femur in relation to the tibia produced by lateral and medial ligament releases to balance the gap in extension in varus [5, 9, 24] or valgus [9, 16] coronal deformities, respectively, may also influence rotational discrepancy. This fact will increase the external and internal femoral component rotations which are needed to balance the gap in flexion. Finally, the size of the selected femoral component can alter the femoral rotation; selection of a small component requires increased external femoral rotation to compensate for the flexion gap relative to a larger femoral component [5].
It remains unclear whether the rotational discrepancies between these two techniques can cause clinical problems, although any clinical effect of femoral rotation may be influenced by the rotational alignment of the tibial component [1]. Mild IR (1°–4°) may cause lateral patellar tracking and tilting [1, 18], moderate IR (5°–8°) may cause patellar subluxation [1, 18], and severe IR (7°–17°) may cause patellar dislocation or component failure [1, 18]. Excessive external femoral rotation is related to increased medial laxity in flexion, increased shear forces on the patella [21], and mechanical overload of the medial side of the joint due to varus alignment in flexion [8].
In addition, there is controversy regarding the correct femoral rotational alignment. There is no consensus on whether the femoral rotation should be anatomical (“normal”) or if a new, “adapted” femoral rotation should be used to compensate for alterations created by the bone cuts, implant geometry, implant placement, and ligament releases [13]. An adapted rotation may create a discrepancy in the femoral component rotation alignment when a method using the flexion balancing CAS technique is compared with another method using a fixed 3° ER posterior condylar axis in the same knee.
Despite the discrepancy in femoral rotation produced depending on surgical technique, we believe that discrepancies of less than 6° in IR or ER of the femur are consistent with a reasonable clinical outcome or simply do not affect the outcome. Nedopil et al. [22] suggested that mismatches less than 10º have no clinical effects. However, it is conceivable that small imbalances in the flexion gap may cause alterations in the distribution of loads in the patella femoral joint [27] and in the femoral tibia joint [3], which can accelerate polyethylene wear and compromise implant survival over time. As in other studies [4, 10], we found no differences in the radiographic alignment of the implants in the frontal and sagittal planes, although there was less dispersion of values in the FB-CAS group. The difference in the lateral alignment of the femoral component was due to surgical technique, given that, in the FB-CAS group, the femoral component was implanted with 3° of flexion.
The design of the study comparing two techniques to establish the femoral component rotational alignment in the same knee during the same surgical procedure is the strength of this study; the anatomic variability and ligament releases were the same for both techniques. This is a single-surgeon study that while eliminating any variables introduced by multiple surgeons nonetheless assures that the anatomic landmarks in CAS were established using the same criteria and with the same skill in all patients. We note several limitations to our study. First, this is not a randomised-controlled trial comparing the techniques based on pre- or post-operative computer tomography of the knee. Therefore, while we were unable to ascertain which technique was the most accurate to reproduce the anatomic femoral rotation, the absence of randomization did not alter the findings regarding the agreement or variability between both techniques. Second, the posterior referencing cutting guide used to measure femoral rotation allowed a range of ER to IR from 0° to 9° in 1.5° increments; when the rotation value was between two settings, it was considered 0.5°. The same rotational increment was applied to the femoral rotational alignment determined by CAS when the value varied between +0.5° and − 0.5°. In both techniques, these variations can be a source of inaccuracy that is attenuated by the large sample size. Third, it was impossible to blind the observer for the clinical examination due to the scars of the CAS tracker in the tibia used in the FB-CAS group, but he was blinded for the radiographic measurements. Finally, we assumed that any differences found using both methods in the same knees would apply to the differences found in different knees. We are confident that this happens due to the uniformity of a single-surgeon surgical technique.
It is clinically relevant to know that different femoral rotation depending on the measured resection or flexion balance technique does not produce differences in frontal or sagittal TKA alignment or clinical outcomes. Discordance of less than 6º internal or external femoral TKA rotations may not justify revision surgery in a painful TKA.
Conclusion
In conclusion, FB-CAS versus posterior condylar axis referencing at a fixed ER of 3° resulted in differing rotational placements of the femoral component. A discrepancy in femoral component rotation of less than 6° of IR or ER appears to have no effect on the coronal and sagittal alignments of the prosthesis or the short-term clinical follow-up.
Abbreviations
- TKA:
-
Total knee arthroplasty
- RT:
-
Measured resection technique
- FB-CAS:
-
Flexion gap-balancing technique with computer-assisted surgery
- TEFR:
-
Transepicondylar femoral rotation
- PRFR:
-
Posterior reference femoral rotation
- AKS:
-
American Knee Society score
- IR:
-
Internal rotation
- ER:
-
External rotation
References
Berger RA, Rubasch HE, Seel MJ, Warren HT, Crosset LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop 286:40–47
Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat Methods Med Res 8:135–160
Chen Z, Wang L, Liu Y, He J, Lian Q, Li D, Jin Z (2015) Effect of component mal-rotation on the knee loading in total knee arthroplasty using multi-body dynamics modeling under a simulated walking gait. J Orthop Res 33(9):1287–1296
Cheng T, Zhao S, Peng X, Zhang X (2012) Does computer assisted surgery improve postoperative leg alignment and implant positioning following total knee arthroplasty? A meta-analysis of randomized control trials. Knee Surg Sports Traumatol Arthrosc 20:1307–1322
Chon JG, Sun DH, Jung JY, Kim TI, Jnag SW (2011) Rotational alignment of the femoral component for minimal medial collateral ligament release in total knee arthroplasty. Knee Surg Relat Res 23(3):153–158
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop 248:9–12
Fitz W, Jäger S, Rieger JS, Seebach E, Bitsch RG (2017) Femoral rotation in total knee arthroplasty: a comparison of patient individualized jigs with gap balancing in relation to anatomic landmarks. Knee Surg Sports Traumatol Arthrosc 25:1712–1719
Hanada H, Whiteside LA, Steiger J, Dyer P, Masatoshi N (2007) Bone landmarks are more reliable than tensioned gaps in TKA component alignment. Clin Orthop 462:137–142
Heesterbeek PJ, Jacobs WCH, Wymenga AB (2009) Effects of the balanced gap technique on femoral component rotation in TKA. Clin Orthop 467:1015–1022
Hernández-Vaquero D, Noriega-Fernandez A, Fernandez-Carreira JM, Fernandez-Simon JM, Llorens de los Rios J (2014) Computer-assisted surgery improves rotational positioning of the femoral component but not the tibial component in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(12):3127–3134
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee society clinical rating system. Clin Orthop 248:13–14
Ishii Y, Noguchi Sato J, Todoroki K, Toyabe S (2014) Retention of the posterior cruciate ligament does not affect femoral rotational alignment in TKA using a gap-balance technique. Knee Surg Sports Traumatol Arthrosc 22:3121–3126
Ishikawa M, Kuriyama S, Ito H, Furu M, Nakamura S, Matsuda S (2015) Kinematic alignment produces near-normal knee motion but increases contact stress after total knee arthroplasty: a case study on single implant design. Knee 22(3):206–212
Jones CW, Jerabek SA (2018) Current role of computer navigation in total knee arthroplasty. J Arthroplasty 33(7):1989–1993
Kwangkyoun K, Jungsung K, Dokyoung L, Sohui L, Jiyoon E (2019) The accuracy of alignment determined by patient-specific instrumentation system in total knee arthroplasty. Knee Surg Relat Res 31(1):19–24
Laskin RS (1995) Flexion space configuration in total knee arthroplasty. J Arthroplasty 10:657–660
Matsuda S, Ishii Y, Noguchi H, Ishii R (2005) Varus-valgus balance and range of movement after total knee arthroplasty. J Bone Joint Surg Br 87:804–808
Matsuda S, Miura H, Nagamine R, Urabe K, Irate G, Iwamoto Y (2001) Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-years followup of Miller-Galante I knees. Am J Knee Surg 14:152–156
Meijer MF, Reininga IH, Boerboom AL, Bulstra SK, Stevens M (2014) Does imageless computer-assisted TKA lead to improved rotational alignment or few outliers? A systematic review. Clin Orthop 472(10):3124–3133
Meric G, Gracitelli GC, Aram LJ, Swank ML, Bugbee WD (2015) Variability in distal femoral anatomy in patients undergoing total knee arthroplasty: measurements on 13456 computed tomography scans. J Arthroplasty 30:1835–1838
Miller MC, Berger RA, Petrella AJ, Karmeas A, Rubash HE (2001) Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop 392:38–45
Nedopil AJ, Howell SM, Rudert M, Roth J, Hull ML (2013) How frequent is rotational mismatch within 0º + -10º in kinematically aligned total knee arthroplasty? Orthopedics 36(12):e1515–e1520
Pirou P, Peronne E, Ouanezar H (2013) Rotational alignment of the femoral component using trochlear navigation during total knee arthroplasty: a dual-center study of 145 cases. J Arthroplasty 28(7):1107–1111
Seung-Yup L, Hong-Chul L, Ki-Mo J, Ji-Hoon B (2017) What factors are associated with femoral component rotation in TKA using the gap balancing technique? Clin Orthop 475:1999–2010
Shen C, Tang ZH, Hu JZ, Zou GY, Xiao RC, Yan DX (2015) Patient-specific instrumentation does not improve accuracy in total knee arthroplasty. Orthopedics 38(3):178–188
Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ (2005) The variability of femoral rotational alignment in total knee arthroplasty. J Bone Jt Surg Am 87:2276–2280
Terashima T, Onodera T, Sawagucho N, Kasahara Y, Majima T (2014) External rotation of the femoral component decreases patellofemoral contact stress in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-014-3103-5
der Linden-Van Van, der Zwaag HLM, Valstar ER, Van der Molen AJ, Nelissen RGH (2008) Transepicondylar axis accuracy in computer assisted knee surgery. A comparison of the CT-based measured axis versus the CAS-determined axis. Comput Aided Surg 13(4):200–206
Victor J (2009) Rotational alignment of the distal femur: a literature review. Orthop Traumatol Sur 95:365–372
Funding
No financial support was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest relevant to this article.
Ethical approval
The authors of Hospital Ethics Committee approved this work (institutional review board approval number AC-14-033) that was performed according to the ethical standards of the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hernández-Hermoso, J.A., Nescolarde-Selva, L., Rodríguez-Montserrat, D. et al. Different femoral rotation with navigated flexion-gap balanced or measured resection in total knee arthroplasty does not lead to different clinical outcomes. Knee Surg Sports Traumatol Arthrosc 28, 1805–1813 (2020). https://doi.org/10.1007/s00167-019-05591-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05591-3