Abstract
Purpose
Performing kinematically aligned total knee arthroplasty (TKA) with generic instruments is less costly than patient-specific instrumentation; however, the alignment and function with this new technique are unknown.
Methods
One hundred and one consecutive patients (101 knees) treated with kinematically aligned TKA, implanted with use of generic instruments, were prospectively followed. The medial collateral ligament was not released. The lateral collateral ligament was released in the 17 % of patients with a fixed valgus deformity. Six measures of alignment were categorized from a scanogram of the extremity, an axial scan of the knee, and an intraoperative measurement. Both the Oxford Knee and WOMAC™ scores were assessed as function. High function was a mean Oxford Knee score >41.
Results
The frequency that patients were categorized as in-range was 93 % for the mechanical alignment of the limb (0° ± 3°), 94 % for the joint line (−3° ± 3°), 57 % for the anatomic axis of the knee (−2.5° ± −7.4° valgus), 4 % for the varus–valgus rotation of the tibial component (≤0° valgus), 98 % for the rotation of the tibial component with respect to the femoral component (0° ± 10°), and 94 % for the intraoperative change in the anterior–posterior distance of the tibia with respect to the femur at 90° of flexion (0 ± 2 mm). The mean OKS score was 42, and WOMAC™ score was 89. For each alignment, the function was the same for patients categorized as an outlier or in-range.
Conclusions
The authors prefer the use of generic instruments to perform kinematically aligned TKA in place of mechanically aligned TKA because five of six alignments were accurate and because high function was restored regardless of whether patients had an alignment categorized as an outlier or in-range.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mechanically aligned TKA strives to achieve a neutral mechanical alignment of the limb (0° hip–knee–ankle angle), an anatomic axis of the knee (femoral–tibial angle) within −2.5° ± −7.4° valgus, and a varus–valgus angle of the tibial component perpendicular to the tibial mechanical axis in all subjects [4, 30–32]. Although mechanically aligned TKA improves function, 20–25 % of patients remain dissatisfied [1, 5].
The conventional assumption that mechanically aligned TKA leads to the best implant survival following TKA has been proved false [4, 17, 30, 34]. The relationship between in-range and varus and valgus outlier categories of the limb and implant survival of a primary TKA is weak at 15 years [4, 30]. Leaving a limb, knee, or tibial component within a natural range of varus does not reduce implant survival at 3, 5, 7, and 10 years [17, 25, 26, 34]. Because most of the normal population has a natural alignment of the limb that is not neutral, and because in these patients a neutral mechanical alignment may create dissatisfaction, there is a need for another technique for aligning a TKA performed with the goal of improving patient function and restoring more normal contact kinematics [3, 9, 16].
In contrast to mechanically aligned TKA performed with patient-specific instrumentation, kinematically aligned TKA performed with patient-specific instrumentation has gained interest because both function and contact kinematics are better than mechanically aligned TKA performed with manual instruments [8, 16, 17]. The primary goal of kinematically aligned TKA is to position the femoral and tibial components so that the angles and levels of the distal and posterior femoral joint lines and the tibial joint line are each restored to the patient’s natural alignment, and not to a neutral limb alignment that is unnatural for most patients [3, 34]. Resurfacing the knee theoretically aligns the components with the three kinematic axes of the knee, lowers the frequency of ligament release, and restores contact kinematics closer to normal [8, 16] (Fig. 1).
A right femur (left) and kinematically aligned TKA (right) show the relationships of the three kinematic axes of the knee with respect to the joint lines of the distal and posterior femur and the position of the components. The transverse axis in the femur about which the tibia flexes and extends is the green line. The transverse axis in the femur about which the patella flexes and extends is the magenta line. The longitudinal axis about which the tibia internally and externally rotates on the femur is the orange line. All three axes are either parallel or perpendicular to the joint lines. Resecting bone, after correcting for wear, from the distal and posterior femur equal in thickness to the condyles of the femoral component kinematically aligns the femoral component. Resecting bone, after correcting for wear, from the tibia equal in thickness to the tibial component kinematically aligns the tibial component
To eliminate the expenses of patient-specific instrumentation, a new technique was developed that uses generic instruments to kinematically align the TKA. As with any new technique, the frequency of patients with an alignment categorized as an ‘outlier’ should be determined because some surgeons remain concerned that ‘outliers’ have a high risk of implant failure and worse function [4, 7, 21, 24, 31]. Studies suggest that six alignments should be evaluated: (1) mechanical alignment of the limb, (2) joint line alignment, (3) anatomic axis of the knee, (4) varus–valgus alignment of the tibial component, (5) axial rotation of the tibial component with respect to the femoral component, and (6) intraoperative change in the anterior–posterior (A–P) distance of the tibia with respect to the femur at 90° of flexion [4, 6, 24, 31]. Function should also be determined with the Oxford Knee score at 6 months because patients with lower scores at 6 months have a higher revision rate at 2 years and lower scores at 5 years [33]. Accordingly, the present study determined (1) the accuracy for six measures of alignment by determining the frequency that patients are categorized in-range, (2) whether high function is restored, and (3) for each alignment whether the function is the same in patients categorized as an outlier and in-range.
Materials and methods
One hundred and one patients (101 knees) treated with a kinematically aligned TKA performed with generic instruments were prospectively followed from June to September 2012. The indications for performing TKA were (1) disabling knee pain and functional loss unresolved with customary nonoperative treatment modalities; (2) radiographic evidence of advanced arthritic change; and (3) all severities of varus, valgus, and flexion contracture deformities. There were 56 women and 45 men with an average age of 67 ± 8.9 years and an average BMI of 30 ± 4.9 kg/m2 at the time of surgery (Table 1). The preoperative diagnoses for patients in this study were degenerative osteoarthritis (91 knees), traumatic osteoarthritis (9 knees), and patellofemoral arthrosis (1 knee). The minimum follow-up was 6 months (range 6–9 months). An institutional review board approved the analysis.
All kinematically aligned TKAs were performed with generic instruments and a cruciate-retaining, fixed-bearing implant (Triathlon; Stryker, Inc, Mahwah, NJ, USA) with a previously described technique [12]. The following steps are highlighted because of their importance. Measure the anterior–posterior distance from the tibia to the distal medial femoral condyle with a calliper with the knee in 90° of flexion (Fig. 2). Remove cartilage to bone with a curette on the distal femoral condyle(s) with wear. Place a 2-mm shim on the extramedullary femoral guide to compensate for the cartilage wear which averages 2 mm, and then set the level of resection so the combined thickness of the distal femoral resection, wear, and kerf equals the thickness of the condyle of the femoral component (Fig. 3) [12]. Set the posterior referencing guide to neutral, and make the chamfer cuts on the femur. Visualize the boundary of the lateral tibial condyle and mark the A–P axis (Fig. 4). Set the extramedullary tibial guide to cut the tibia parallel to the articular surface after correcting for wear. Align the A–P axis of the tibial trial component parallel to the A–P axis of the lateral tibial condyle [27]. With the trial components in place, adjust the posterior slope and thickness of the tibial liner until the anterior–posterior distance from the tibia to the distal medial femoral condyle is restored. When the limb is in excessive valgus, release the lateral collateral ligament and the popliteus tendon, recut the tibia in 2° more varus, and insert a thicker liner, which straightens the limb.
A right knee in 90° of flexion shows the use of a calliper on the medial compartment to measure the anterior–posterior distance from the tibia to the distal medial femoral condyle at exposure (a) and after implantation of the TKA (b). Because there is 2 mm of cartilage wear on the medial femoral condyle in this varus knee, the distance after the TKA was 2 mm less than at exposure. An increase in the thickness of the polyethylene insert of 2 mm tightens the posterior cruciate ligament and moves the distance of the medial femoral condyle 2.5 mm posterior on the tibia [6]
A right knee in 90° of flexion shows the use of the extramedullary femoral guide on the distal femur. A 2-mm shim is inserted under the distal medial and lateral pads to compensate for 2 mm of cartilage wear on both distal condyles in this knee with tricompartmental osteoarthritis from chronic ACL deficiency (a). The extramedullary rod is visually aligned parallel to the anterior thigh and femoral shaft. A calliper measures the thickness of the distal medial condyle, which equals the thickness of the distal medial condyle of the femoral component after correcting for cartilage wear (2 mm) and the kerf (1.5 mm) (b)
A top view of a right tibia shows the steps for aligning the rotation of the tibial component. On the articular surface of the tibial plateau, the boundary of the oval-shaped lateral tibial condyle is outlined by a series of partially opaque black dots (a). A vertical blue line is drawn on the A/P axis that bisects the oval shape. Two parallel pins were drilled parallel to the A/P line through the articular surface of the medial tibial condyle with a guide (b). On the cut surface of the tibial plateau, two A/P lines were drawn parallel to the two drill holes into which pins have been placed to clarify their location (c). The A/P axis of the trial tibial component was aligned parallel to these two A/P lines (d)
On the day of discharge, each patient had an anterior–posterior rotationally controlled long-leg, nonweightbearing, CT scanogram [15, 17] and 1.25-mm axial images of the femoral and tibial components [2]. Patient demographics, preoperative, intraoperative, and postoperative data were recorded [13] (Table 1).
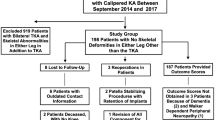
Alignment was studied in 100 of 101 patients (Table 2) (Fig. 5). One author (KTK), blinded to the function scores, categorized five alignments with use of measurements reported to have high interobserver reliability: (1) mechanical alignment of the limb as the angle between a line connecting the mechanical axes of the femur and tibia [4, 17, 30], (2) joint line alignment as the angle between the joint line and a line connecting the centres of the hip and ankle [20], (3) anatomic axis of the knee as the angle between the anatomic axes of the femur and tibia [17], (4) varus–valgus alignment of the tibial component as the angle between the tibial component and the mechanical axis of the tibia [17], and (5) rotation of the tibial component as the angle between a line connecting the centre of the lugs of the femoral component and a line tangent to the posterior border of the tibial component or liner [24]. In the 83 of 101 knees with an intact ACL, one author (SMH) measured with a calliper the A–P distance of the anterior tibia with respect to the distal medial femoral condyle at 90° of flexion at exposure and after implantation of the TKA, and computed the change. The in-range category was 0° ± 3° for the mechanical alignment of the limb [30], −3° ± 3° for the joint line alignment [20], −2.5° to −7.4° valgus for the anatomic axis of the knee [31], ≤0° for the varus–valgus alignment of the tibial component [31], 0° ± 10° for rotation of the tibial component [24], and ±2 mm for the change in the A–P distance of the anterior tibia with respect to the medial femoral condyle [6]. Patients with values outside each in-range category were categorized as either a varus or a valgus outlier, or an outlier in the case of the varus–valgus alignment of the tibial component.
Scanograms and axial CT images from one patient show the lines used to measure limb alignment, joint line alignment, knee alignment, tibial component alignment, and rotation of the tibial component on the femoral component. Because the angles measured on the extremity with the TKA and the contralateral normal knee are nearly identical, the femoral and tibial components are closely restored to the joint line of the contralateral knee. Although the limb and joint line alignments are in-range, paradoxically, the alignments of the knee and tibial component are categorized as varus outliers even though they match the normal contralateral knee
Function was studied with both the Oxford Knee Score (48 best, 0 worst) and WOMAC™ questionnaires (100 best, 0 worst) in 101 of 101 patients at a minimum follow-up of 6 months(range 6–8).
Statistical analysis
The arithmetic mean, frequency, standard deviation (SD), 95 % confidence interval (CI) of the mean, and frequency distribution were computed for each measured quantity when appropriate (JMP, 10.02, http://www.jmp.com). For each alignment, a nonparametric Kruskal–Wallis test determined whether the Oxford Knee and WOMAC™ scores were different between categories. Significance was p < 0.05.
Results
The average surgical time was 42 ± 5 min. No medial collateral or posterior cruciate ligaments were released. One lateral retinacular release was performed in the patient with patellofemoral arthritis. In the 17 of 101 patients with a fixed valgus deformity, the lateral collateral ligament and popliteus tendon were released. The posterior capsule was released in the 33 of 101 patients with a fixed flexion contracture. One patient required a blood transfusion. All patients were discharged to home, with 56 staying 1 night and 39 staying 2 nights in the hospital. No patient reported having further surgery on the knee or seeking consultation with another orthopaedic surgeon because of dissatisfaction.
The frequency of patients categorized as in-range was 93 % for mechanical alignment of the limb, 94 % for the joint line alignment, 57 % for the anatomic axis of the knee, 4 % for the varus–valgus alignment of the tibial component, 98 % for the rotation of the tibial component with respect to the femoral component, and 94 % for the intraoperative change in the A–P distance of the tibia with respect to the medial femoral condyle (Table 2).
For all subjects, the mean Oxford Knee score was 42 ± 5.2 (95 % CI 41–43), and the mean WOMAC™ score was 89 ± 11.2 (95 % CI 87–91). For each alignment, there was no difference in function scores between patients categorized as an outlier and in-range (Table 3)
.
Discussion
The most important findings of the present study were that the use of generic instruments to kinematically align a TKA accurately aligned five of the six alignments, restored high function, and high function was restored regardless of whether patients had an alignment categorized as an outlier or in-range.
The frequency the mechanical alignment of the limb of patients treated with kinematically aligned TKA using generic instruments was in-range was comparable if not more accurate than reports of patients with mechanically aligned TKA performed with conventional instruments, patient-specific instrumentation, or computer-assisted instruments [4, 8, 17, 19, 30] (Table 4). This accuracy is due to treatment of the 17 % of patients with a fixed valgus deformity by releasing the lateral collateral ligament and the popliteus tendon, recutting the tibia in 2° more varus, and inserting a thicker liner.
In the present study, the frequency the alignment of the joint line was aligned in-range parallel to the floor in single-leg stance of patients in the present study was more accurate than reports of patients treated with mechanically aligned TKA with conventional instruments [8]. Mechanically aligned TKA changes the joint line an average of 2.5° more valgus than normal, which places the joint line oblique to the floor in single-leg stance, and imbalances compartmental forces and increases medial and lateral shear forces across the knee [8, 20].
The frequency the anatomic axis of the knee of patients treated with kinematically aligned TKA using generic instruments was in-range was at least comparable if not more accurate than reports of patients treated with mechanically aligned TKA performed with conventional instruments and with patient-specific instrumentation [28, 31] (Table 4). The 11° range (3° to −8°) of the anatomic axis of the knee in the present study is comparable to normal extremities and is 66 % narrower than the 32° range (12° to −20°) reported for mechanically aligned TKA performed with conventional instruments [10, 31].
Because the varus–valgus alignment of the tibial component was aligned to the natural joint line and not perpendicular to the mechanical axis of the tibia in the present study, the frequency of patients categorized in-range was lower than patients treated with mechanically aligned TKA performed either with conventional instruments or with patient-specific instrumentation (Table 4) [8, 28, 31]. Several studies have shown that positioning the tibial component within a natural range of varus does not reduce implant survival at 3, 5, 7, and 10 years [17, 25, 26, 34]. One study has shown that function is better when a varus limb is left in mild varus than when overcorrected to ‘in-range’ [34]. Restoring the natural varus–valgus alignment of the tibial joint line is the only way to maintain the normal orthogonal relationships between the longitudinal kinematic axis in the tibia, the two transverse kinematic axes in the femur, and the joint lines of the knee (Fig. 1) [8, 9, 11, 14, 16, 18].
In the present study, the frequency the rotation of the fixed-bearing tibial component with respect to the femoral component of patients was in-range was comparable if not more accurate than reported for patients treated with mechanically aligned TKA performed with a mobile-bearing component (Table 4) [23, 24]. The new kinematically aligned technique maintained the rotation in nearly all patients within 0° ± 10°, which is associated with better function and more normal contact kinematics after mechanically aligned TKA [24, 27].
In the patients with an intact ACL in the present study, the intraoperative change in the A–P distance of the tibia with respect to the medial femoral condyle was accurately minimized. Several studies have shown the importance but also the difficulty of adjusting the A–P distance, which is the key step in adjusting the flexion gap to balance the PCL in a PCL-retaining TKR [6, 35]. A loose PCL may result in instability and pain, and excessive tension in the PCL may restrict flexion [29]. The technique of kinematically aligning the femoral component and adjusting both the slope of the tibia and the thickness of the tibial liner while maintaining an intact PCL without release accurately minimized the intraoperative change in the A–P distance of the tibia with respect to the medial femoral condyle.
Finally, for each alignment measured, the function was comparable if not higher than reports of kinematically aligned TKA performed with patient-specific instrumentation, and mechanically aligned TKA performed with conventional instruments, patient-specific instrumentation, or computer-assisted instruments (Table 4). Because high function was restored regardless of whether patients had an alignment categorized as an outlier or in-range, the exercise of categorizing alignment to determine function was shown to serve no purpose. Resurfacing the knee by positioning the components to restore the normal joint lines would be perceived as natural to the patient, and may be desirable because the release of collateral, posterior cruciate, and retinacular ligaments is rarely needed except in the knee with a fixed valgus deformity [3].
Two limitations that require further study should be discussed. First, the results in the present study require independent confirmation even though they were obtained independent of the treating surgeon because alignment and function published by designing surgeons are typically better than those reported by registries [22]. Second, although the New Zealand Joint Registry has shown that the high Oxford Knee score reported in the present study prognosticates a low revision rate at 2 years and high function at 5 years, the present study did not determine long-term survival of the implant and long-term patient function [17, 33].
Conclusion
The authors prefer the use of generic instruments to perform kinematically aligned TKA in place of mechanically aligned TKA because five of six alignments were accurate and because high function was restored regardless of whether patients had an alignment categorized as an outlier or in-range.
References
Baker PN, van der Meulen JH, Lewsey J, Gregg PJ (2007) The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J Bone Joint Surg Br 89(7):893–900
Bedard M, Vince KG, Redfern J, Collen SR (2011) Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res 469(8):2346–2355
Bellemans J, Colyn W, Vandenneucker H, Victor J (2011) The Chitranjan Ranawat Award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470(1):45–53
Bonner TJ, Eardley WGP, Patterson P, Gregg PJ (2011) The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Joint Surg Br 93-B(9):1217–1222
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468(1):57–63
Christen B, Heesterbeek P, Wymenga A, Wehrli U (2007) Posterior cruciate ligament balancing in total knee replacement: the quantitative relationship between tightness of the flexion gap and tibial translation. J Bone Joint Surg Br 89(8):1046–1050
de Jong RJ, Heesterbeek PJ, Wymenga AB (2010) A new measurement technique for the tibiofemoral contact point in normal knees and knees with TKR. Knee Surg Sports Traumatol Arthrosc 18(3):388–393
Dossett H, Swartz G, Estrada N, Lefevre G, Kwasman B (2012) Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics 35(2):160–169
Eckhoff DG, Bach JM, Spitzer VM, Reinig KD, Bagur MM, Baldini TH, Flannery NM (2005) Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg Am 87(Suppl 2):71–80
Gu Y, Roth J, Howell SM, Hull ML (in press) How frequently do four methods for mechanically-aligning a total knee arthroplasty cause collateral ligament imbalance and change alignment from normal in Caucasians? J Bone Joint Surg Am
Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG (1993) The axes of rotation of the knee. Clin Orthop Relat Res 290:259–268
Howell SM, Hull ML (2012) Kinematic alignment in TKA: definition, surgical technique, and challenging cases orthopedic knowledge online 10(7).www.orthoportal.aaos.org/oko/article.aspx?article=OKO_ADU050#abstract
Howell SM, Rogers SL (2009) Method for quantifying patient expectations and early recovery after total knee arthroplasty. Orthopedics 32(12):884–890
Howell SM, Howell SJ, Hull ML (2010) Assessment of the radii of the medial and lateral femoral condyles in varus and valgus knees with osteoarthritis. J Bone Joint Surg Am 92(1):98–104
Howell SM, Kuznik K, Hull ML, Siston RA (2010) Longitudinal shapes of the tibia and femur are unrelated and variable. Clin Orthop Relat Res 468(4):1142–1148
Howell SM, Hodapp EE, Vernace JV, Hull ML, Meade TD (2012) Are undesirable contact kinematics minimized after kinematically aligned total knee arthroplasty? An intersurgeon analysis of consecutive patients. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-012-2220-2
Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML (2013) Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res 471(3):1000–1007
Iranpour F, Merican AM, Dandachli W, Amis AA, Cobb JP (2010) The geometry of the trochlear groove. Clin Orthop Relat Res 468(3):782–788
Kamat YD, Aurakzai KM, Adhikari AR, Matthews D, Kalairajah Y, Field RE (2009) Does computer navigation in total knee arthroplasty improve patient outcome at midterm follow-up? Int Orthop 33(6):1567–1570
Kapandji IA (1987) The physiology of the joints, vol 2. Churchill Livingston, Edinburgh, pp 66–74
Klatt BA, Goyal N, Austin MS, Hozack WJ (2008) Custom-fit total knee arthroplasty (OtisKnee) results in malalignment. J Arthroplasty 23(1):26–29
Labek G, Neumann D, Agreiter M, Schuh R, Böhler N (2011) Impact of implant developers on published outcome and reproducibility of cohort-based clinical studies in arthroplasty. J Bone Joint Surg Am 93(Supplement 3):55–61
Lutzner J, Krummenauer F, Gunther KP, Kirschner S (2010) Rotational alignment of the tibial component in total knee arthroplasty is better at the medial third of tibial tuberosity than at the medial border. BMC Musculoskelet Disord 11:1–7. doi:10.1186/1471-2474-11-57
Lützner J, Kirschner S, Günther K-P, Harman M (2012) Patients with no functional improvement after total knee arthroplasty show different kinematics. Int Orthop 1–7. doi:10.1007/s00264-012-1584-8
Malkani AL, Rand JA, Bryan RS, Wallrichs SL (1995) Total knee arthroplasty with the kinematic condylar prosthesis. A 10-year follow-up study. J Bone Joint Surg Am 77(3):423–431
Matziolis G, Adam J, Perka C (2010) Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg 130(12):1487–1491
Nedopil AJ, Howell SM, Rudert M, Roth J, Hull ML (In Press) How frequent is rotational mismatch within 0° ± 10° in kinematically-aligned TKA? orthopedics
Nunley R, Ellison B, Zhu J, Ruh E, Howell S, Barrack R (2012) Do patient-specific guides improve coronal alignment in total knee arthroplasty? Clin Orthop Relat Res 470(3):895–902
Pagnano MW, Hanssen AD, Lewallen DG, Stuart MJ (1998) Flexion instability after primary posterior cruciate retaining total knee arthroplasty. Clin Orthop Relat Res 356:39–46
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the 15-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92(12):2143–2149
Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA (2011) The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am 93-A(17):1588–1596
Ritter MA, Davis KE, Davis P, Farris A, Malinzak RA, Berend ME, Meding JB (2013) Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Joint Surg Am 95(2):126–131
The New Zealand Joint Registry 10 Year Report: January 1999 to December 2008 (2009), http://www.nzoa.org.nz/nz-joint-registry
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2481-4
Victor J, Banks S, Bellemans J (2005) Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: a prospective randomised outcome study. J Bone Joint Surg Br 87(5):646–655
Acknowledgments
We thank the imaging department and technicians at Methodist Hospital, Sacramento, CA for performing the scanograms and axial CT scans.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was performed at Methodist Hospital in Sacramento, CA, USA, and at the Department of Mechanical Engineering at the University of California at Davis, Davis, CA, USA.
Rights and permissions
About this article
Cite this article
Howell, S.M., Papadopoulos, S., Kuznik, K.T. et al. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc 21, 2271–2280 (2013). https://doi.org/10.1007/s00167-013-2621-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2621-x