Abstract
In this new feature of The Journal of Nuclear Cardiology we will summarize key articles that were published in the Journal in the previous year. In the first article of this 2-part series we concentrated on publications dealing with cardiac positron emission tomography, computed tomography, and neuronal imaging. This review will focus on myocardial perfusion imaging summarizing advances in the field including in diagnosis, prognosis, appropriateness, and safety of testing.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Prognostic Value of Myocardial Perfusion Imaging (MPI)
There are extensive prognostic data on the value of MPI including its important role in risk stratification.1 However, the data in very elderly patients are limited. Katsikis et al2 from Onassis Cardiac Surgery Center, Athens, Greece evaluated the prognostic value of treadmill exercise MPI in 247 patients older than 80 years who underwent testing at their institution. The patients exercised for 5 ± 2 minutes achieving a peak heart rate of 124 ± 19 beats/min. The exercise duration was less than 3 minutes in 9 patients. The test was terminated due to fatigue or dyspnea in 64%, angina in 15%, hemodynamic abnormalities in 3%, and achievement of maximum predicted heart rate in 17%. A low summed stress score (SSS, ≤3) was present in 41%, intermediate SSS4-12 in 30%, and high SSS (>12) in 28% of patients. After a median follow-up of 7 years there were 48 deaths (17 cardiac deaths), 8 non-fatal myocardial infarctions (MIs), and 21 late coronary revascularizations (>3 months after MPI). There were significant differences in the Kaplan–Meier survival curves for all outcomes according to SSS categories. For example, patients in the low SSS category had an annual cardiac mortality rate of 0.9% compared to 5% for those with high SSS. This study extends the prognostic data available for MPI to octogenarians. Risk stratification with MPI can be useful in this patient population when it is deemed meaningful due to the limited life expectancy in this cohort.
An important aspect of risk stratification with MPI is the low cardiac risk associated with normal MPI. Rozanski et al3 evaluated how coronary artery disease (CAD) risk factors influenced long-term risk in more than 12000 patients with normal exercise MPI. During a follow-up time of 11.2 ± 4.5 years, 8.6% of the patients died (annualized mortality rate of 0.8%/year). Smoking, hypertension, diabetes, and decreasing exercise duration were associated with worse outcomes. Further, these risk factors were synergistically associated with outcomes such that patients without any of these factors who exercised >9 minutes had a annualized mortality of 0.2% per year and this increased stepwise to 1.6%/year in those with 2–3 risk factors who exercised <6 minutes. Thus, while a normal exercise MPI conferred a low long-term mortality risk, this population can be further risk stratified based on the presence of clinical risk factors and exercise capacity. Acampa et al4 also evaluated the effect of diabetes status on cardiac risk in patients with normal stress MPI. They studied 260 patients with diabetes who were propensity-matched to 260 without diabetes all with normal perfusion on imaging. During a median follow-up of 53 months, 18 events (11 cardiac deaths and 7 non-fatal MIs) occurred in the diabetes group compared to 6 events (2 cardiac deaths and 4 MIs) in the non-diabetes group. Both diabetes status and post-stress left ventricular ejection fraction (LVEF) ≤45% were independent predictors of events. While non-diabetic patients with normal LVEF remained at low risk for the length of follow-up, patients with diabetes and LVEF ≤45% achieved a risk level >3% in 12 months (Figure 1). Thus, the ‘warranty period’ of a normal stress MPI varies according to diabetes status and post-stress LVEF. The same group performed a meta-analysis of 14 studies recruiting more than 13000 patients with diabetes and showed that the negative predictive value for cardiac death and non-fatal MI for a normal MPI is 95% with a corresponding annualized event rate after a negative test of 1.6%5.
Estimated time (mean with 95% confidence intervals, CI) from stress MPI to reach a defined level of risk for cardiac death or nonfatal MI in a propensity score-matched cohort of diabetic and non-diabetic patients stratified by post-stress LVEF. Reproduced with permission from Acampa et al4
In another large study of almost 15000 patients (3654 with diabetes), Padala et al6 evaluated the impact of the level of exercise achieved during exercise MPI on cardiovascular outcomes in diabetic patients. In patients with significant perfusion defect (SSS > 8), inability to achieve ≥5 METs predicted cardiac events better than diabetes status. Further, diabetic patients who achieved more than 10 METs had a very low event rate. After risk factor adjustment, 1-MET increment in exercise capacity was associated with 12% decrease in cardiac events in the diabetes group.
Left Ventricular Dyssynchrony
Phase analysis of gated MPI has been used to assess for LV mechanical dyssynchrony.7,8 Several studies evaluated the additive prognostic value of LV dyssynchrony by MPI on top of traditional parameters. Zafrir et al9 studied 787 patients who underwent gated MPI with phase analysis at their institution. During a median follow-up of 19 months, 55 patients died and 45 had cardiac events (26 cardiac death, 16 heart failure hospitalization, 2 patients with sustained ventricular tachycardia and one with ventricular fibrillation). In multivariate analysis, low LVEF (<50%), NYHA class and diabetes were the independent predictors of cardiac events while NYHA class and phase standard deviation (SD) were the independent predictors of cardiac deaths. Cardiac death occurred in 7.8% of patients with abnormal phase SD (>40°) and in 1.9% of patients with normal SD (P < 0.001). Thus, phase analysis by MPI can be used for the prediction of cardiac death on top of other more traditional prognostic indicators.
Hage et al10 studied the association of LV mechanical dyssynchrony by phase analysis and cardiac sympathetic denervation (MIBG) with potential sudden cardiac death events as a substudy of ADMIRE-HF (AdreView Myocardial Imaging for Risk Evaluation in Heart Failure). ADMIRE-HF studied 964 patients with symptomatic heart failure and reduced LVEF (≤35%). During a median follow-up of 17 months, 92 patients experienced adjudicated potential sudden cardiac death events (23 with sudden cardiac death, 5 fatal MI, 7 resuscitated cardiac arrest, 46 with appropriate cardiac defibrillator therapy, and 11 with sustained ventricular tachycardia). Propensity score matching was used to assemble a cohort of 85 patients without potential sudden cardiac death events who were well-balanced in 21 measured baseline characteristics to those with events. Patients who experienced potential events had significantly wider phase SD than matched control patients (62.3 ± 2.4° vs 55.5 ± 2.3°, P = 0.03) and were more likely to have a phase SD ≥ 60° (53% vs 35%, P = 0.03). Thus, in ADMIRE-HF LV mechanical dyssynchrony by phase analysis of gated SPECT MPI was independently associated with potential sudden cardiac death events.
Goldberg et al11 evaluated the prognostic value of LV mechanical dyssynchrony in 324 patients with non-ischemic cardiomyopathy with mildly decreased systolic function (LVEF 35%-50%) and narrow or intermediate QRS duration (WRS <150 ms). During a mean follow-up time of 4.6 years, 86 (26%) patients died. On multi-variate analysis, age, diabetes status, and phase SD were independent predictors of all-cause mortality. Importantly, phase SD remained an independent predictor of death in the patients with narrow QRS (<120 ms). Therefore, phase SD may be a useful prognostic marker in this population that is generally considered at lower risk of events compared to patients with ischemic cardiomyopathy and severe LV systolic dysfunction. In a separate study Aggarwal et al12 evaluated the prognostic value of LV dyssynchrony in 828 patients with end-stage renal disease being evaluated for renal transplantation. During a mean follow-up of 5 years, 35% of the patients died. Parameters on phase analysis indicative of dyssynchrony (phase SD and bandwidth) were larger in patient who died than those who survived. In a multivariate model adjusting for demographics, co-morbidities, abnormal perfusion, and LVEF, a phase bandwidth above the median (>56°) was independently associated with mortality (HR 1.34, P = 0.01). A wide phase bandwidth was associated with mortality in the subset of patients with abnormal perfusion but not in those with normal perfusion. This study showed that phase analysis provides prognostic data beyond traditional MPI parameters in patients with end stage renal disease being evaluated for renal transplantation, especially in those with abnormal perfusion pattern on imaging.
Huang et al13 studied the relationship between stress-induced LV dyssynchrony and the extent of CAD on coronary angiography. Patients with multi-vessel CAD had more global dyssynchrony than those without CAD on angiography. Further, in patients with multi-vessel disease there was significantly more dyssynchrony on the stress images than rest images indicating the possibility of myocardial stunning. Specifically, patients with significant LAD disease had more global dyssynchrony as well as territorial dyssynchrony in the LAD region at stress than at rest (Figure 2) indicating that LAD stenosis has an important impact on dyssynchrony. This study suggested that the territorial assessment of LV synchrony may assist in the diagnosis of multi-vessel CAD as an indicator of myocardial stunning.
Dyssynchrony assessment for the entire LV (phase standard deviation [SD] and histogram bandwidth) and coronary territories (phase SD in the territories). This patient had a 100% stenosis in the mid LAD according to the coronary angiography. The global dyssynchrony parameters (phase SD and histogram bandwidth) and LAD phase SD deteriorated from rest to early post-stress. Such deterioration was due to the delayed contraction in the ischemic region. Figure reproduced from Huang et al13 with permission
Zhang et al14 used phase analysis to assess the effect of right ventricular apical vs septal pacing on LV synchrony. Phase analysis by MPI was performed at 1 week and 6 months after pacemaker placement in 39 patients with complete atrioventricular block who were randomized to receive right ventricular apical vs. septal pacing. There were no significant differences in LV dyssynchrony parameters between the 2 groups at 1 week after pacemaker placement. At 6 months, phase SD was significantly lower in the patients that received septal vs apical pacing (18.65 ± 9.14° vs 28.67 ± 15.33°, P = 0.004). While LV synchrony improved from the 1-week to the 6-month scans in the septal pacing group, it was unchanged in the apical pacing group (−4.37 ± 7.59° vs 6.17 ± 15.17°, P = 0.01). The findings from this small randomized study suggest that right ventricular septal pacing may result in better LV mechanical synchrony compared to right ventricular apical pacing.
Innovations
Several reports were published in the Journal in 2014 involving advances and innovations in MPI.15-21 Patil et al15 studied 54 patients with high-resolution Anger SPECT (128 × 128 matrix with 3.2 mm pixel size) with attenuation correction, noise reduction and resolution recovery algorithms. The sensitivity of this innovative software for detection of obstructive CAD by angiography was 89%, which was equally high in men and women, obese and non-obese, and in those stressed with exercise and pharmacologic stress. Image quality was high and interpretative certainty was an impressive 96%. Mut et al16 used early (15 ± 5 minutes) post-exercise conventional gated SPECT MPI to improve the detection of post-ischemic stunning. Nudi et al17 developed a novel 7-region segmentation approach in keeping with the anatomic distribution of the main coronary vessels and a corresponding ischemia score (Figure 3). They validated the prognostic value of this approach in 8714 patients with mean follow-up of 31 months. This novel ischemia score was significantly associated with 1-year and long-term outcomes even after adjusting for multiple confounding variables. Fransson et al18 developed an open access software for automated quantitation of ischemia and infarction by MPI that used voxel-based image registration of rest and stress images in combination with regional myocardial function at rest. Mouden et al20 showed that availability of coronary artery calcium score to the interpreting physician altered the diagnostic interpretation in 37% of cases and, notably, reduced the number of equivocal findings from 21% to 13%. Ather et al21 studied 120 patients using 3 commercially available automated quantitative softwares. They showed significant differences between the softwares in measuring perfusion defect size and LV function. For example, there was discordance among the three softwares in 62% of cases for classification of perfusion defect size as mild, moderate, or severe (Figure 4). These findings could have major implications for patient care.
Comparison between the standard 20-unit segmentation method (left panel) and the approach of Nudi et al17 which segments the left ventricular myocardium into 7 regions (right panel 1, apical; 2, antero-medial and antero-distal; 3, antero-proximal; 4, septal; 5, postero-lateral; 6, lateral; and 7, inferior). Figure reproduced from Nudi et al17 with permission
A patient with discordant assessment of perfusion defect with the three softwares. Whereas 4 dimension-myocardial SPECT (4DM) assessed the reversible perfusion defect as severe (45%), Emory cardiac toolbox measured it as moderate (10%), and quantitative perfusion SPECT (QPS) as mild (7%). Reproduced with permission Ather et al21
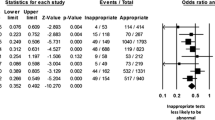
Appropriateness and Safety
Appropriate Use Criteria for detection and risk assessment of stable CAD using MPI and other imaging modalities were recently published.22 Winchester et al23 evaluated the role of training, specialty, and practice location of the ordering clinician on the appropriate use of MPI. Out of 582 patients studied ~10% were considered inappropriate. There was no effect of training (housestaff vs clinicians), specialty (cardiology vs others) or practice location (emergency room vs inpatient vs outpatient) on the rate of inappropriate testing. The majority of inappropriate MPIs were performed in asymptomatic patients. The most common inappropriate indications ordered by each group were different suggesting that interventions to reduce inappropriate use of MPI may be more successful if tailored to each group separately.
MPI may show normal perfusion in patients with CAD. An important concern is whether patients with significant CAD may be missed with MPI and specifically whether patients with left main disease or 3-vessel CAD may have normal perfusion due to balanced ischemia. Yokota et al24 studied the prevalence, location, and extent of significant CAD in 256 patients with normal MPI who had invasive coronary angiography due to worsening of symptoms. Of these, 93(36%) patients had significant CAD (≥70% stenosis in major coronary artery or >50% stenosis in left main) on angiography. The majority of these patients had single (61%) or 2-vessel (22%) disease while 10% had 3-vessel CAD and 7% had left main disease. Overall, ‘unprotected’ left main and/or 3-vessel CAD was present in 11% of patients. During a mean follow-up period of 5 years, 6.6% of patients died with no significant difference between those that had CAD on angiography vs. those that did not. These data indicate that balanced ischemia as a cause of false-negative MPI is not common.
Currently, regadenoson is the most commonly used pharmacologic stress agent for MPI. Recent reports25,26 of MI occurring after regadenoson injection raised concerns regarding the safety of stress testing with regadenoson. Rosenblatt et al27 reported 2 cases of asystole that led to hemodynamic collapse following regadenoson administration in stable outpatients in the absence of baseline conduction abnormalities or interfering medications. Further, cases of seizures associated with regadenoson have been described.28 However, it is important to note that the absolute risk associated with regadenoson appears to be small and may not be different than that associated with other stress agents.29,30 Whether patients who are at high risk of complications with regadenoson administration can be reliably identified by screening prior to stress testing is an important topic that should be comprehensibly addressed.
References
Shaw LJ, Hage FG, Berman DS, Hachamovitch R, Iskandrian A. Prognosis in the era of comparative effectiveness research: where is nuclear cardiology now and where should it be? J Nucl Cardiol. 2012;19:1026-43.
Katsikis A, Theodorakos A, Papaioannou S, Tsapaki V, Kolovou G, Drosatos A, et al. Long-term prognostic value of myocardial perfusion imaging in octogenarians able to undergo treadmill exercise stress testing. J Nucl Cardiol. 2014;21:1213-22.
Rozanski A, Gransar H, Min JK, Hayes SW, Friedman JD, Thomson LE, et al. Long-term mortality following normal exercise myocardial perfusion SPECT according to coronary disease risk factors. J Nucl Cardiol. 2014;21:341-50.
Acampa W, Petretta M, Cuocolo R, Daniele S, Cantoni V, Cuocolo A. Warranty period of normal stress myocardial perfusion imaging in diabetic patients: a propensity score analysis. J Nucl Cardiol. 2014;21:50-6.
Acampa W, Cantoni V, Green R, Maio F, Daniele S, Nappi C, et al. Prognostic value of normal stress myocardial perfusion imaging in diabetic patients: a meta-analysis. J Nucl Cardiol. 2014;21:893-902, quiz 890-2, 903-5.
Padala SK, Ghatak A, Padala S, Katten DM, Polk DM, Heller GV. Cardiovascular risk stratification in diabetic patients following stress single-photon emission-computed tomography myocardial perfusion imaging: the impact of achieved exercise level. J Nucl Cardiol. 2014;21:1132-43.
Chen J, Garcia EV, Bax JJ, Iskandrian AE, Borges-Neto S, Soman P. SPECT myocardial perfusion imaging for the assessment of left ventricular mechanical dyssynchrony. J Nucl Cardiol. 2011;18:685-94.
Salimian S, Thibault B, Finnerty V, Gregoire J, Harel F. The effects of dobutamine stress on cardiac mechanical synchrony determined by phase analysis of gated SPECT myocardial perfusion imaging in a canine model. J Nucl Cardiol. 2014;21:375-83.
Zafrir N, Nevzorov R, Bental T, Strasberg B, Gutstein A, Mats I, et al. Prognostic value of left ventricular dyssynchrony by myocardial perfusion-gated SPECT in patients with normal and abnormal left ventricular functions. J Nucl Cardiol. 2014;21:532-40.
Hage FG, Aggarwal H, Patel K, Chen J, Jacobson AF, Heo J, et al. The relationship of left ventricular mechanical dyssynchrony and cardiac sympathetic denervation to potential sudden cardiac death events in systolic heart failure. J Nucl Cardiol. 2014;21:78-85.
Goldberg AS, Alraies MC, Cerqueira MD, Jaber WA, Aljaroudi WA. Prognostic value of left ventricular mechanical dyssynchrony by phase analysis in patients with non-ischemic cardiomyopathy with ejection fraction 35-50% and QRS < 150 ms. J Nucl Cardiol. 2014;21:57-66.
Aggarwal H, AlJaroudi WA, Mehta S, Mannon R, Heo J, Iskandrian AE, et al. The prognostic value of left ventricular mechanical dyssynchrony using gated myocardial perfusion imaging in patients with end-stage renal disease. J Nucl Cardiol. 2014;21:739-46.
Huang WS, Huang CH, Lee CL, Chen CP, Hung GU, Chen J. Relation of early post-stress left ventricular dyssynchrony and the extent of angiographic coronary artery disease. J Nucl Cardiol. 2014;21:1048-56.
Zhang H, Hou X, Wang Y, Xue S, Cao K, Chen J, et al. The acute and chronic effects of different right ventricular site pacing on left ventricular mechanical synchrony as assessed by phase analysis of SPECT myocardial perfusion imaging. J Nucl Cardiol. 2014;21:958-66.
Patil HR, Bateman TM, McGhie AI, Burgett EV, Courter SA, Case JA, et al. Diagnostic accuracy of high-resolution attenuation-corrected Anger-camera SPECT in the detection of coronary artery disease. J Nucl Cardiol. 2014;21:127-34.
Mut F, Giubbini R, Vitola J, Lusa L, Sobic-Saranovic D, Peix A, et al. Detection of post-exercise stunning by early gated SPECT myocardial perfusion imaging: results from the IAEA multi-center study. J Nucl Cardiol. 2014;21:1168-76.
Nudi F, Pinto A, Procaccini E, Neri G, Vetere M, Tomai F, et al. A novel clinically relevant segmentation method and corresponding maximal ischemia score to risk-stratify patients undergoing myocardial perfusion scintigraphy. J Nucl Cardiol. 2014;21:807-18.
Fransson H, Ljungberg M, Carlsson M, Engblom H, Arheden H, Heiberg E. Validation of an automated method to quantify stress-induced ischemia and infarction in rest-stress myocardial perfusion SPECT. J Nucl Cardiol. 2014;21:503-18.
Takamine S, Fujiwara S, Shigeru M, Ito T, Kawai H, Shiotani H, et al. Relationship of decreased accumulation of (99m)Tc-tetrofosmin on myocardial single-photon emission computed tomography images between QRS duration in dilated cardiomyopathy patient with left bundle branch block. J Nucl Cardiol. 2014;21:1023-8.
Mouden M, Ottervanger JP, Timmer JR, Reiffers S, Oostdijk AH, Knollema S, et al. The influence of coronary calcium score on the interpretation of myocardial perfusion imaging. J Nucl Cardiol. 2014;21:368-74.
Ather S, Iqbal F, Gulotta J, Aljaroudi W, Heo J, Iskandrian AE, et al. Comparison of three commercially available softwares for measuring left ventricular perfusion and function by gated SPECT myocardial perfusion imaging. J Nucl Cardiol. 2014;21:673-81.
Ronan G, Wolk MJ, Bailey SR, Doherty JU, Douglas PS, Hendel RC, et al. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Nucl Cardiol. 2014;21:192-220.
Winchester DE, Hymas J, Meral R, Nguyen D, Dusaj R, Shaw LJ, et al. Clinician-dependent variations in inappropriate use of myocardial perfusion imaging: training, specialty, and location. J Nucl Cardiol. 2014;21:598-604.
Yokota S, Ottervanger JP, Mouden M, Timmer JR, Knollema S, Jager PL. Prevalence, location, and extent of significant coronary artery disease in patients with normal myocardial perfusion imaging. J Nucl Cardiol. 2014;21:284-90.
Hsi DH, Marreddy R, Moshiyakhov M, Luft U. Regadenoson induced acute ST-segment elevation myocardial infarction and multivessel coronary thrombosis. J Nucl Cardiol. 2013;20:481-4.
Shah S, Parra D, Rosenstein RS. Acute myocardial infarction during regadenoson myocardial perfusion imaging. Pharmacotherapy. 2013;33:e90-5.
Rosenblatt J, Mooney D, Dunn T, Cohen M. Asystole following regadenoson infusion in stable outpatients. J Nucl Cardiol. 2014;21:862-8.
Agarwal V, DePuey EG. Regadenoson and seizures: a real clinical concern. J Nucl Cardiol. 2014;21:869-70.
Hage FG. Regadenoson for myocardial perfusion imaging: is it safe? J Nucl Cardiol. 2014;21:871-6.
Hage FG, Iskandrian AE. Serious complications associated with regadenoson administration for myocardial perfusion imaging: a commentary. J Nucl Cardiol. 2014;21:877-9.
Disclosure
Dr. Hage has received grant support from Astellas Pharma US.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hage, F.G., AlJaroudi, W.A. Review of cardiovascular imaging in The Journal of Nuclear Cardiology in 2014: Part 2 of 2: Myocardial perfusion imaging. J. Nucl. Cardiol. 22, 714–719 (2015). https://doi.org/10.1007/s12350-015-0144-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-015-0144-1