Abstract
Background
Myocardial perfusion scintigraphy (MPS) represents a key prognostic tool, but its predictive yield is far from perfect. We developed a novel clinically relevant segmentation method and a corresponding maximal ischemia score (MIS) in order to risk-stratify patients undergoing MPS.
Methods
Patients referred for MPS were identified, excluding those with evidence of myocardial necrosis or prior revascularization. A seven-region segmentation approach was adopted for left ventricular myocardium, with a corresponding MIS distinguishing five groups (no, minimal, mild, moderate, or severe ischemia). The association between MIS and clinical events was assessed at 1 year and at long-term follow-up.
Results
A total of 8,714 patients were included, with a clinical follow-up of 31 ± 20 months. Unadjusted analyses showed that subjects with a higher MIS were significantly different for several baseline and test data, being older, having lower ejection fraction, and achieving lower workloads (P < .05 for all). Adverse outcomes were also more frequent in patients with higher levels of ischemia, including cardiac death, myocardial infarction (MI), and their composites (P < .05 for all). Differences in adverse events remained significant even after extensive multivariable adjustment (hazard ratio for each MIS increment = 1.57 [1.29-1.90], P < .001 for cardiac death; 1.19 [1.04-1.36], P = .013 for MI; 1.23 [1.09-1.39], P = .001 for cardiac death/MI).
Conclusions
Our novel segmentation method and corresponding MIS efficiently yield satisfactory prognostic information.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Myocardial perfusion scintigraphy (MPS) has an established prognostic role in the management of patients with or at risk for coronary artery disease (CAD),1 yet several fields of research remain open.2 Consensus has been reached on the use of specific segmentation methods to identify imaging areas of the left ventricle which can best be exploited for multi-imaging modalities.3 Specifically, current recommended approaches to left ventricular imaging rely on 17- or 20-unit segmentation models,3-6 that, however, still remain debated and far from perfect.7-9
In fact, excessive segmentation of left ventricular myocardium in multiple sub-segments may actually conflict with the coronary circulation, which is based on two coronary vessels and three main branches.9 Accordingly, a more parsimonious and clinically relevant segmentation method, combined with the grade of ischemia, may increase the homogeneity between patients belonging to the same score group. Thus, it holds the promise of more accurate and robust prognostic results.
Given these premises and prior experience with the drawbacks of the 17-segment approach in other institutions,7-9 we have applied since 2004 a novel seven-region segmentation approach, and a corresponding maximal ischemia score (MIS), distinguishing five main groups of patients: from those with no ischemia up to those with severe ischemia in at least one of the seven regions. In order to formally appraise the prognostic accuracy of this novel approach, we retrospectively reviewed our institutional database focusing on mid- and long-term clinical outcomes.
Methods
Design
This is a retrospective observational study exploiting prospectively collected data entered into a dedicated administrative database. All patients provided written informed consent for the imaging test and data collection.
Patients
Patients undergoing MPS for the diagnostic or prognostic work-up of CAD since April 2004 at our center were identified by querying our institutional database (OPCCardioPro). Patients were excluded from data retrieval if aged <18 years, ineligible for 1-year clinical follow-up, having a history of prior coronary revascularization, having a prior or recent clinical diagnosis of myocardial infarction, or having scintigraphic evidence of myocardial necrosis (i.e., irreversible stress/rest defect). Subjects with necrosis were excluded to maximize the internal validity of our work, and to maintain our specific focus on the prognostic role of ischemia, rather than on a complex mix of ischemia and necrosis.
Protocol
Patients were exercised in a fasting state having discontinued long-acting nitrates and beta-blockers for at least 24 hours. Symptom-limited dynamic stress testing was performed on a bicycle ergometer according to standard protocol. At peak exercise, a weight-adjusted dose (3.0-4.0 mCi) of 201Tl was injected, and patients exercised at the same level for two additional minutes.
Subjects unable to exercise were instructed to abstain from caffeine-containing foods, beverages, and medications containing methylxantines for at least 24 hours, and underwent pharmacologic stress testing. Dipyridamole was administered intravenously at a rate of 0.14 mg·kg−1·minute−1 for 6 minutes. Three minutes after the end of the dipyridamole infusion, a weight-adjusted dose (3.0-4.0 mCi) of 201Tl was injected. Blood pressure and heart rate were recorded every minute.
Imaging
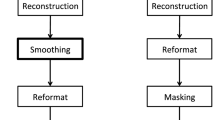
Post-stress and rest gated single photon emission computed tomography (SPECT) was performed 3 minutes and 6-24 h after 201Tl injection with the patient in the supine position to maximize redistribution. A dual-head gamma camera (Millennium MG, GE Healthcare, Milan, Italy), equipped with a low-energy, general-purpose collimator, was used according to a standard protocol for data acquisition and elaboration.10 The gated data were processed with completely automated software (QGS 3.0; Cedars-Sinai Medical Center, Los Angeles, CA, USA).
From the established 20-unit segmentation method,6 seven regions were graphically obtained to quantify the degree of myocardial perfusion. This segmentation approach was in keeping with the anatomic distribution of the main coronary vessels: 1—apical, 2—antero-medio-distal, 3—antero-proximal, 4—septal, 5—postero-lateral, 6—lateral (which corresponds to the anatomic variability in coronary dominance), and 7—inferior (Figures 1, 2). Specifically, this approach was based on the fact that the left anterior descending (LAD) almost invariably provides blood to the antero-proximal, antero-medial, antero-distal, apical, or septal regions, with multi-segment involvement typical of proximal or diffuse disease. The postero-lateral region and the inferior region are typically fed by, respectively, the left circumflex (LCX) and the right coronary artery (RCA). Conversely, the lateral region is the extension of the postero-lateral or inferior regions as a consequence of coronary dominance.
The seven regions take into account the role of the three main coronary vessels and the amount of myocardium fed by them. In addition, when the LAD is diseased, the apical region is always ischemic, whereas the antero-proximal region and the septal region are ischemic only when the LAD stenosis involves the proximal tract. The only exception is an isolated stenosis of the first diagonal branch, in the absence of LAD disease, which leads to ischemia in the antero-proximal region only.
Semiquantitative interpretation of stress/rest images was performed based on the seven-region model by consensus of two experienced observers using both visual assessment of the color-coded tomographic images for the three axes and the standard deviation (SD) polar map of detectable tracer uptake (with a 2.5 SD cut-off to distinguish those with normal perfusion from those with variable degrees of ischemia), finally obtaining a five-point scoring system (0, normal uptake; 1, minimally reduced uptake; 2, mildly reduced uptake; 3, moderately reduced uptake; and 4, severely reduced or absent uptake).4,11 This score directly yielded the five classes of MIS (0, no ischemia; 1, minimal ischemia; 2, mild ischemia; 3, moderate ischemia; 4, severe ischemia), as the final MIS is strictly depending on the worst region of perfusion. Left ventricular ejection fraction was also computed with SPECT.
Follow-Up and Endpoints
Clinical follow-up was systematically collected on a yearly basis up to 5 years after the index MPS, by direct patient visit or phone contact. In case an adverse event was elicited, hard copies of the source documents (e.g., hospitalization records) were retrieved to enable event adjudication. Endpoints of the study were the 1-year and long-term rates of: death; cardiac death; non-fatal myocardial infarction; percutaneous coronary intervention; coronary artery bypass grafting; the composite of death or myocardial infarction; the composite of cardiac death or myocardial infarction; the composite of death, myocardial infarction, or revascularization; and the composite of cardiac death, myocardial infarction, or revascularization. Cardiac death was defined as any death with a specific cardiac cause or without any established non-cardiac cause but occurring suddenly.
Statistical Analysis
Continuous variables are reported as mean ± standard deviation. Categorical variables are reported as n (%). Bivariate analyses were performed distinguishing patients according to MIS, using ANOVA for continuous variables and χ 2 test for categorical variables. Survival curves were computed according to Kaplan and Meier, and compared with the log-rank test. Multivariable analyses were then performed with logistic regression and Cox proportional hazard analysis, to appraise the independent prognostic impact of MIS simultaneously adjusting for all covariates significantly (P < .05) associated with this parameter. Statistical significance was set at the two-tailed 0.05 level. Computations were performed with SPSS 20 (IBM, Armonk, NY, USA).
Results
A total of 8,714 (18.5%) subjects undergoing MPS were identified in keeping with our selection criteria. Overall, myocardial ischemia was present in 4,553 (52.3%). Specifically, 4,161 (47.8%) patients had no ischemia, 1,399 (16.1%) minimal ischemia, 1,566 (18.0%) mild ischemia, 1,020 (11.7%) moderate ischemia, and 568 (6.5%) patients had severe ischemia. Several baseline and procedural features were different in subjects with different MIS (Tables 1, 2).
Unadjusted bivariate analyses for clinical outcomes at 1 year of follow-up (Tables 3, 4), showed that MIS was associated with a significantly increased risk in 1-year death, cardiac death, and non-fatal myocardial infarction, as well as the composite of death or myocardial infarction, cardiac death or myocardial infarction (all P < .05). As expected, patients with higher MIS were also more likely to undergo coronary revascularization within 1 year, as well as the composite of death (or cardiac death), myocardial infarction, or revascularization (all P < .05).
Unadjusted bivariate analysis for clinical outcomes at long-term follow-up (mean 31 ± 20 months) (Table 3; Online only Table 1), confirmed the significant association between MIS and adverse events, as patients with higher MIS also had a higher risk of death, cardiac death, myocardial infarction, or their composites (all P < .05). Similar findings were evident when inspecting and formally testing survival curves (Figures 3, 4, 5, 6).
Bivariate analyses for 1-year and long-term clinical outcomes obtained after stratifying for total % of ischemic myocardium computed according to a standard 20-segment method in order to enable visual comparison with results based on MIS were also performed (Online only Table 2).
Multivariable adjusted analyses, exploring the association between MIS and clinical outcomes while adjusting for several potential confounders and also enabling the comparison of MIS vs total % of ischemic myocardium, confirmed that MIS was an independent risk factor for death, cardiac death, myocardial infarction, or their composites at both 1-year and long-term follow-up (all P < .05) (Table 4). Specifically, the hazard ratio for each increment in MIS was 1.22 (1.06-1.40, P = .007) for death, 1.57 (1.29-1.90, P < .001) for cardiac death, 1.19 (1.04-1.36, P = .013) for myocardial infarction, 1.16 (1.05-1.29, P = .005) for death or myocardial infarction, and 1.23 (1.09-1.39], P = .001) for cardiac death or myocardial infarction.
Discussion
The present study, exploiting an extensive and prospectively collected real-world dataset on MPS, provides important insights on the prognostic yield of this functional imaging test. Specifically, exploiting a novel parsimonious seven-region segmentation method for the left ventricular myocardium, and a simple five-tier MIS, the analytical approach hereby proposed proved remarkably effective in risk-stratifying patients with established or subclinical CAD at both 1-year and long-term follow-up. Hence, this straightforward, user-friendly, and clinically relevant method to appraise MPS results can be proposed for clinical decision making.
Since the pioneering efforts of the prior decades to the last developments, the diagnostic and prognostic yield of MPS has seen momentous improvements. Taking into account the differences between anatomic and functional definitions of CAD, MPS and similar functional tests for myocardial ischemia are a mainstay in the management of subjects with suspected as well as established CAD. Despite its apparent maturity, MPS remains, however, an active field of research, going from improvements in technological equipments, to testing protocols, and image reconstruction. Even the steps involving the segmentation of the left ventricular myocardium and the distinction between minimal, mild, moderate, or severe ischemia remain debated.9
There is widespread consensus nowadays that a 17- or 20-unit segmentation for the left ventricular myocardium is particularly useful to compare MPS results with those stemming from other cardiac imaging modalities.3,4 Conversely, this approach has limitations when inferring on CAD. Patients have only a limited set of main coronary vessels, and even an apparently secondary vessel always brings flow to a region which is by far larger than a 1/17 or 1/20 of the left ventricular myocardium. In addition, despite the huge variability in coronary anatomy (for instance length, size, collaterals, and dominance), preserving a logical relationship between the diseased coronary vessel and the underperfused region is a an important goal for any diagnostic test. For instance, it is unclear whether any coronary artery stenosis can lead to an isolated defect of the mid septal segment, as this could be just spurious precision. Instead, larger myocardial regions do correspond with reasonable accuracy to the main and prognostically relevant coronary branches.12
Another commonly adopted approach is the use of a simple estimate to quantify myocardial ischemia, by means of summed scores.13 This approach, combined with the typical 17- or 20-segment reconstructions, and using a simple cut-off for severely abnormal findings (e.g., summed score >10) has the intuitively appeal of a comprehensive and quantitatively precise estimation of myocardial ischemia. However, the summed score approach appears clearly counterintuitive after thoughtful perusal and particularly limited in recognizing groups of patients with homogeneous MPS results as well as similar prognosis. For instance, it assumes in fact that a patient with a set of three contiguous segments in the LAD territory each with complete absence tracer uptake (summed score of 12) would be equivalent to a patient with set of 12 segments, randomly dispersed in the three coronary territories, each with only equivocal reduction in radioisotope uptake (summed score of 12 also in this case).
In light of these drawbacks and based on prior evidence with planar and SPECT MPS that degree of ischemia is the most powerful driver of prognosis, since 2004, we chose a segmentation approach for the left ventricular myocardium and adopted MIS, i.e., a score which identifies a test as showing severe ischemia only (or at least) if one or more of the seven left ventricular regions has signs of severe ischemia. This means that in no case an exam will be considered indicative of severe ischemia if only minimal, mild, or moderate ischemia is present in the left ventricular segments. Accordingly, an abnormal MIS score applies on average to at least 1/7 of the left ventricular myocardium, as, for instance, a severe MIS means that at least 14% of the left ventricular myocardium is already ischemic. This method may increase the user-friendliness and clinical relevance of MPS, by reducing the risk of spurious precision in appraising the geographical extent and severity of perfusion defects.
Our results, which build upon those from groups which have similarly challenged 17- or 20-segment and summed score approaches,7-9 show that a MIS stemming from a seven-region segmentation approach is capable to risk-stratify in an efficient and precise fashion patients with established or subclinical CAD in terms of their 1-year as well as long-term risk of major clinical events. In particular, MIS appeared as a consistent adverse event predictor, with a significant increase in risk for every MIS class change. Such findings, as well as the bivariate analyses for total % of ischemic myocardium computed according to the conventional 20-segment method as well as the multivariable analyses, suggest that our model, compared to those based on other approaches typically exploiting a 20- or 17-segment model and giving the same prognostic weight to ischemia severity and extent,1 seems to have at least a similar prognostic accuracy while featuring a much more simple and straightforward computation and derivation approach.
Notably, the fact that the MIS proved an independent risk predictor even among patients undergoing revascularization as first event and when such treatment modality was forced as covariate into the multivariable model suggests that the prognostic role of MPS, as appraised according to the present methodology, is substantially independent from the subsequent type of treatment received by patients. In addition, the complex prognostic synergy between severity and extent of ischemia is shown by the fact that using extent of ischemia within a given MIS class was useful to improve risk prediction within the same class, but was not capable of identifying patients at higher risk in comparison to those belonging to the subsequent class. Of course, in routine clinical practice our reporting characterizes patients on maximal ischemia score as well as ischemia extent and LAD involvement, as both these additional features represent also very important factors for clinical decision making.
It is noteworthy that several patients underwent revascularization despite the evidence of only mild or minimal ischemia, and occasionally even in the absence of myocardial ischemia. Despite randomized trials suggesting that this approach might not be clinically appropriate when performed routinely,14 this scenario is typical of real-world observational datasets. Several explanations may be proposed, including the fact that interventional cardiologists and cardiac surgeons do not necessarily rely for decision-making solely on the results of MPS, but also, and often correctly, take into account coronary anatomy, patient symptoms, and response to medical therapy.
This work has several limitations, including the retrospective design, single-center setting, and lack of focus on the relationship between degree of stenosis and MIS, and the impact of ischemia extension in each MIS class. Similarly, an adequate model to validate our segmentation approach will be the association between such approach and the potential areas of necrosis.
New Knowledge Gained
The present work originally exploits a novel seven-region approach for left ventricular myocardial perfusion assessment, combined with a maximal ischemia scoring system, to enable straightforward and anatomically relevant risk-prognostication in patients undergoing stress MPS. Formal appraisal of its accuracy in a large patient sample with follow-up spanning several years suggests that this method provides prognostic results which are at least as accurate and clinically relevant as those provided by the standard more fragmented and complex scoring system.
References
Beller GA. First annual Mario S. Verani, MD, Memorial lecture: Clinical value of myocardial perfusion imaging in coronary artery disease. J Nucl Cardiol 2003;10:529-42.
Clark AN, Beller GA. The present role of nuclear cardiology in clinical practice. Q J Nucl Med Mol Imaging 2005;49:43-58.
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. J Nucl Cardiol 2002;9:240-5.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Stress myocardial perfusion single-photon emission computed tomography is clinically effective and cost effective in risk stratification of patients with a high likelihood of coronary artery disease (CAD) but no known CAD. J Am Coll Cardiol 2004;43:200-8.
Kang SJ, Cho YR, Park GM, Ahn JM, Han SB, Lee JY, et al. Predictors for functionally significant in-stent restenosis: An integrated analysis using coronary angiography, IVUS, and myocardial perfusion imaging. JACC Cardiovasc Imaging 2013;6:1183-90.
Hansen CL, Goldstein RA, Akinboboye OO, Berman DS, Botvinick EH, Churchwell KB, et al. Myocardial perfusion and function: Single photon emission computed tomography. J Nucl Cardiol 2007;14:e39-60.
Vaduganathan P, He ZX, Vick GW 3rd, Mahmarian JJ, Verani MS. Evaluation of left ventricular wall motion, volumes, and ejection fraction by gated myocardial tomography with technetium 99m-labeled tetrofosmin: A comparison with cine magnetic resonance imaging. J Nucl Cardiol 1999;6:3-10.
Cerci RJ, Arbab-Zadeh A, George RT, Miller JM, Vavere AL, Mehra V, et al. Aligning coronary anatomy and myocardial perfusion territories: An algorithm for the CORE320 multicenter study. Circ Cardiovasc Imaging 2012;5:587-95.
Candell-Riera J, Ferreira-González I, Marsal JR, Aguadé-Bruix S, Cuberas-Borrós G, Pujol P, et al. Usefulness of exercise test and myocardial perfusion-gated single photon emission computed tomography to improve the prediction of major events. Circ Cardiovasc Imaging 2013;6:531-41.
DePasquale EE, Nody AC, DePuey EG, Garcia EV, Pilcher G, Bredlau C, et al. Quantitative rotational thallium-201 tomography for identifying and localizing coronary artery disease. Circulation 1988;77:316-27.
Berman DS, Kiat H, Friedman JD, Wang FP, van Train K, Matzer L, et al. Separate acquisition rest thallium-201/stress technetium-99m sestamibi dual-isotope myocardial perfusion single-photon emission computed tomography: A clinical validation study. J Am Coll Cardiol 1993;22:1455-64.
Pereztol-Valdés O, Candell-Riera J, Santana-Boado C, Angel J, Aguadé-Bruix S, Castell-Conesa J, Garcia EV, Soler-Soler J. Correspondence between left ventricular 17 myocardial segments and coronary arteries. Eur Heart J 2005;26:2637-43.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003;107:2900-7.
Shaw LJ, Berman DS, Maron DJ, Mancini GB, Hayes SW, Hartigan PM, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: Results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 2008;117:1283-91.
Disclosures
All authors have no funding or conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi:10.1007/s12350-014-9929-x.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nudi, F., Pinto, A., Procaccini, E. et al. A novel clinically relevant segmentation method and corresponding maximal ischemia score to risk-stratify patients undergoing myocardial perfusion scintigraphy. J. Nucl. Cardiol. 21, 807–818 (2014). https://doi.org/10.1007/s12350-014-9877-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-014-9877-5