Abstract
Background
Left ventricular mechanical dyssynchrony (LVMD) by phase analysis of gated single-photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) is a useful tool for predicting response to cardiac resynchronization therapy and has prognostic value. While most of the studies were done on patients with ischemic cardiomyopathy or those with LV ejection fraction (EF) < 35%, there are little data on the prognostic value of LVMD in patients with non-ischemic cardiomyopathy (NICM), particularly those with mildly decreased systolic function and narrow or intermediate QRS duration.
Methods and Results
From the stress SPECT-MPI database at Cleveland Clinic, we identified 324 consecutive patients (mean age 62 ± 13 years, 62% male, 36% diabetics) with NICM, LVEF 35-50% (median [Q1,Q3] 45 [41,49]), and QRS < 150 ms (13% with QRS 120-149 ms). LVMD was determined from gated stress images and expressed as phase standard deviation (SD) and histogram BW (% R-R cycle). For easier graphical illustration, patients were divided into tertiles of LVMD. All-cause death was the primary endpoint and determined using the Social Security Death Index. Cox proportional hazard model was performed to determine the independent predictive value of LVMD, and next Cox models for incremental value. After a mean follow-up time of 1,689 days, 86 (26.5%) of patients died. These patients were older, had more diabetes, more use of diuretics, with wider QRS duration, and with a trend for higher phase SD and BW. After adjusting for age, hypertension, diabetes, aspirin, beta-blockers, diuretics, QRS, and EF, phase SD was an independent predictor of all-cause mortality with hazard ratio [95% CI] 1.97 [1.06,3.66] for the highest tertile, and added incremental prognostic value (P = .025). Similar findings were obtained using histogram BW.
Conclusion
In patients with NICM, EF 35-50%, and QRS < 150 ms, increased LVMD on peak stress SPECT was an independent predictor of all-cause mortality. The utility and applicability of such findings in clinical practice need further evaluation in larger and prospective studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Phase analysis of single-photon emission computer tomography (SPECT) gated myocardial perfusion imaging (MPI) has proven as a useful tool in evaluation of patients. As an automated, reproducible technique to accurately assess left ventricular mechanical dyssynchrony (LVMD),1-3 phase analysis has proven to be a quick tool in the assessment and prognostication of patients presenting for nuclear stress testing. The clinical applications and prognostic value of LVMD by phase analysis has been established in patients with ischemic cardiomyopathy and LV ejection fraction (EF) < 35%,4-6 and those with left bundle branch block undergoing cardiac resynchronization therapy (CRT).7
While patients with mild-to-intermediate cardiomyopathy have been shown to have significant LVMD,8 the prognostic value of LVMD in this cohort is not well defined. There has been increasing interest in identifying patients who do not meet the currently identified criteria for implantable cardiac defibrillator (ICD) or CRT by QRS duration and morphology or LV systolic function, but may have significant LVMD, and potential survival benefit from these interventions. Therefore, we sought to assess whether increased LVMD by phase standard deviation (SD) or histogram BW on SPECT-MPI would have prognostic value in patients with normal perfusion on SPECT-MPI, mild-to-moderate LV systolic dysfunction (LVEF 35-50%), and narrow-to-intermediate duration QRS (less than 150 ms).
Methods
Patient Selection
From the stress SPECT-MPI database maintained at Cleveland Clinic, we identified 928 consecutive patients with non-ischemic cardiomyopathy (NICM) and QRS duration < 150 ms who underwent stress/rest Technetium-99m gated SPECT-MPI between October 2004 and December 2010. Patients with NICM were defined as those with normal stress/rest MPI, no history of coronary artery disease or revascularization, and EF < 50%. Patients with moderately depressed LVEF < 35%, hypertrophic cardiomyopathy, infiltrative disease, significant valvular heart disease, atrial fibrillation at the time of the stress test, or ventricular pacing were excluded, leaving 324 patients for final analysis.
Patient demographics, comorbidities, medications, and electrocardiographic data were all collected prospectively at the time of SPECT imaging, and subsequently retrieved for analysis. CAD was defined on coronary angiography as >50% stenosis of a major epicardial coronary artery, or Q waves on an electrocardiogram with clinical diagnosis of myocardial infarction. Hypertension was defined as systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg at the time of the stress test or clinic visits, self-reported history, or the use of anti-hypertensive medications. Hyperlipidemia was defined as an abnormal fasting lipid panel according to the ATP III guidelines, self-reported history, or the use of statins. Diabetes mellitus was defined as fasting glucose ≥ 126 mg/dL, self-reported history, or the use of hypoglycemic medications.
The study was approved by the Institutional Review Board with waiver of consent, and complied with the Declaration of Helsinki.
MPI SPECT Acquisition
The full protocol was previously described in detail.3,9 In brief, gated SPECT-MPI was obtained at rest (low dose, ~9-15 mCi) and stress (exercise [Bruce, modified Bruce, or Cornell], or pharmacological [dipyridamole, adenosine, or regadenoson]) (high dose, ~30-45 mCi) using Tc-99m tetrofosmin according to the American Society of Nuclear Cardiology.10 Imaging was started at 30-60 minutes after resting or pharmacological testing, and 10-20 minutes after exercise testing, using a dual-headed detector gamma camera with high-resolution, low-energy collimators. Images were acquired using a 64 × 64 matrix with a step-and-shoot protocol, 180° elliptical orbit, 64 total projections, and 16 frames per RR cycle. They were then reconstructed by filtered back projection using Ramp and Butterworth filters or iterative reconstruction (starting September 2008), without attenuation correction. All images were reviewed for quality assurance by a senior nuclear technologist and a board-certified nuclear cardiologist. The LV volumes and EF were calculated from the gated stress images (higher counts). The summed stress score, summed rest score, and summed difference score were all zero (all patients had normal rest/stress MPI as part of the inclusion criteria).
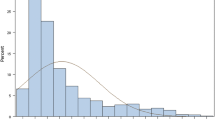
LV Mechanical Dyssynchrony
LVMD indices were obtained by phase analysis on the gated stress SPECT images (higher count)9 and as previously described.3,11 In brief, three-dimensional (3D) count distributions were extracted from each LV short-axis dataset. The time intensity curves were then fitted to a first-order harmonic using Fourier analysis (Corridor 4DM, Michigan). The generated 3D phase distribution spanning the R-R interval was then represented on a polar map and histogram. The peak phase is the most frequent phase of the cardiac cycle, the phase SD represents the SD of the phase distribution on the histogram plot, and histogram BW represents 95% of the phase distribution. Phase SD and histogram BW were expressed as % of the R-R interval (conversion from % R-R to degrees: 1% = 3.6°) (Figure 1).
Primary Outcome
All-cause mortality, determined by the Social Security Death Index and the Cleveland Clinic electronic medical record, was the primary outcome of interest because of its high specificity.12 The censoring date was December 31, 2012. Annualized mortalities rates were obtained by dividing by the mean follow-up times.
Statistical Analysis
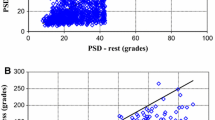
A descriptive analysis was performed examining selected variables for each group. Continuous variables were expressed as mean (SD) or median [Q1,Q3] and were compared using one way Anova or Kruskal-Wallis test as appropriate. Categorical variables were expressed as number (%) and compared using Pearson Chi-square test or Fisher exact test as appropriate. Scatter plots were used to illustrate the distribution of LVMD indices vs LVEF and QRS duration. Survival analysis treated the time of stress MPI as ‘time 0.” Cox proportional hazard model was performed to assess the independent predictive value of phase SD on all-cause mortality in this cohort. Covariates that were significant on univariate analysis (P < .1) were entered in the model. Those that were borderline significant or deemed clinically relevant were forced in. The final model was adjusted for age, hypertension, diabetes, aspirin, beta-blockers, diuretics, QRS, EF, and phase SD. Phase SD was used as categorical variable (tertiles) to allow easier graphical illustration of the adjusted Kaplan-Meier survival curve that was generated from the multivariable Cox model. We repeated the analysis using phase SD as continuous variable, EDV or ESV instead of EF (confounding variable), and also histogram BW instead of phase SD. QRS was used as dichotomous variable (> or <120 ms) and as continuous variable. We also did sensitivity analysis and excluded patients with QRS > 120 ms. Lastly, the incremental prognostic value of LVMD was tested using nested Cox models and the corresponding increase in the Chi-square of the model up to 1 degree of freedom. A P value < .05 was set a priori and considered statistically significant. All statistical analyses were performed using the Statistical Package for Social Sciences, version 19, for Windows (SPSS, Chicago, Illinois).
Results
Patients’ Characteristics
There were 324 patients, mean age 62 ± 13 years, and 62% male. The overall cohort was characterized by significant proportions of patients with diabetes (36%), hypertension (86%), history of smoking (57%), and obesity (mean body mass index 32 kg/m2). All patients had normal MPI and were with relatively mildly decreased systolic function (median [Q1,Q3] LVEF 45% [41,49]). Mean QRS duration was 100 ms, with 13% of the total cohorts having QRS duration between 120 and 150 ms. When stratified by tertiles of phase SD (Table 1), there was no significant difference in demographics, comorbidities, or QRS duration, but there was a difference with LVEF among groups.
Mechanical Dyssynchrony
The cohort included patients with relatively narrow phase SD (mean 4.7% ± 1.6% that corresponds to 16.9° ± 5.8°), and histogram BW (25% ± 10%). Patients were divided into tertiles of phase SD (tertile 1, phase SD < 3.6%; tertile 2, phase SD 3.6-5.2%; and tertile 3, phase SD > 5.2%), and similarly histogram BW (<20%, 20-27%, and >27%). There was significant scatter between phase SD and LVEF with a weak correlation (r = 0.22, P < .001) (Figure 2), and no correlation with QRS duration (r = 0.09, P = .9) (Figure 3). Similar findings were obtained with histogram BW.
Outcome
After a mean follow-up time (SD) of 1,689 (843) days, 86 (25.6%) patients died (Table 2). They were significantly older (69 [13] vs 60 [12] years, P < .0001), had more diabetes mellitus (45% vs 33%, P = .03), and were taking more diuretics (41% vs 24%, P = .01) (Table 2). There were also a higher proportion of patients with intermediate QRS duration (120 < QRS < 150 ms) that died (21% vs 11% respectively, P = .025). There was no significant difference in LVEF or other comorbidities between those who met the primary endpoint and those who did not.
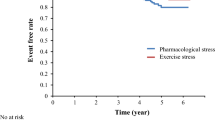
Patients who died had a trend toward a higher mean phase SD (P = .1) and BW (P = .08). Conversely, there was a trend toward higher annual mortality among different tertiles of phase SD (4.7%/year vs 5.6%/year vs 7.0%/year, for the first, second and third tertiles respectively, P = .2), and histogram BW (P = .028). On multivariate Cox proportional hazard analysis, and after adjusting for baseline demographics, comorbidities and gated SPECT-MPI, increasing age (HR = 1.06, 95% CI [1.04,1.08] per year), diabetes mellitus (HR = 1.90 [1.20,3.02]), and phase SD (third tertile HR 1.97 [1.06,3.66]; continuous variable HR 1.01 [1.0,1.36]) were independent predictors of all-cause mortality (Table 3). Similarly, histogram BW was an independent predictor of death (third tertile HR 1.82 [1.01,3.37]; and continuous variable HR 1.02 [1.002,1.048]). Phase SD was also an independent predictor of death when patients with QRS > 120 ms were excluded (third tertile HR 1.82 [1.01,3.61]). Increasing QRS duration (whether used as continuous variable or dichotomous [i.e., greater or less than 120 ms]) was not an independent predictor of all-cause death. Similarly, LVEF or LV volumes (entered separately in the model due to confounding effect) were not independent predictors of outcomes in this cohort (Table 3). There was no interaction between phase SD and EF, QRS, age, or diabetes. Adjusted Kaplan Meier survival curves illustrate the freedom from the primary outcome of the different tertiles of phase SD (Figure 4).
Finally, when using nested Cox models, adding phase SD to a clinical model of age and diabetes mellitus with other comorbidities resulted in increase in chi-square model from 50 to 55 (P = .025) (Figure 5) and similarly for histogram BW.
Discussion
The assessment of mechanical dyssynchrony in patients with LV systolic dysfunction has proven useful in prognostication of mortality as well as in potential response to CRT. Phase analysis of SPECT-MPI has the advantage of being automated, reproducible with high inter- and intraobserver correlation, analyses hundreds of R-R cycles over several minutes (advantage in patients with arrhythmia as compared with echocardiography) from 3D dataset which can be obtained from previously acquired gated images and without additional radiation burden or cost.1,3
Phase analysis to quantify LVMD has been shown to have prognostic value when identifying patients who may benefit from CRT.7 as well as identify those with higher risk of mortality or fatal arrhythmia treated with ICD shock.4-6 However, to date, most work with phase analysis has been in patient populations largely defined by significant LV dysfunction with EF < 35%, or in those with already identified electrical dyssynchrony defined as a QRS duration > 150 ms on ECG. Further, most studies thus far have identified patient populations that are strictly ischemic cardiomyopathy (ICM) or have a predominance of ischemic patients over those with normal perfusion.4,6,7,11,13,14 Still, and despite the evidence in such cohort of patients, the most recent ACC/AHA appropriateness criteria did not include any discussion on the role of LV dyssynchrony before ICD or resynchronization therapy.15
Atchley et al8 evaluated patients with mild-to-moderate LV systolic dysfunction, defined as a LVEF between 35% and 50%, and compared them to patients with severe LV dysfunction (EF < 35%) and normal controls (EF > 55%). They found that patients with mild-to-moderate LV systolic dysfunction had more mechanical dyssynchrony than normal controls, but less than those with severe dysfunction. Further, they found little correlation between QRS duration and mechanical dyssynchrony on SPECT, suggesting that in patients with mild-to-moderate LV dysfunction, ECG analysis for assessment of LVMD may not be sufficient in identifying those patients that would benefit from resynchronization therapy or are at higher risk of death.
In our present study, we were able to identify a large cohort of patients (N = 324) with normal perfusion imaging and mild-to-moderate LV systolic dysfunction, as well as narrow-to-intermediate QRS duration (less than 150 ms). The phase SD, histogram BW, and degree of LVMD were relatively narrow or mild, but still significantly greater than normal control3; this is not surprising given the pre-selected cohort.
There was significant scatter between phase SD indices and LVEF as well as with QRS, reflecting poor correlation between these parameters (Figures 2, 3) (similarly with histogram BW, figures not shown). Indeed, the correlation between electrical and mechanical dyssynchrony is poor as previously shown.6
Despite the narrow range of phase SD in our population, when grouped into tertiles of phase SD, we found that there was a trend toward higher unadjusted annualized all-cause mortality with increasing phase SD. After adjusting for potential confounders, phase SD and similarly, histogram BW were independent predictors of mortality, and added incremental value to traditional clinical variables such as age and diabetes.
These findings suggest that in patients thought to be relatively at low risk, increasing LVMD by phase analysis of gated SPECT-MPI identifies those at higher risk of death. The clinical and therapeutic implications of this finding warrant further investigation in large prospective studies.
Strength and Limitations
This is the largest study to our knowledge to evaluate the prognostic value of LVMD among patients with NICM, mild-to-moderate LV systolic dysfunction and normal-to-intermediate QRS durations. In this selected cohort, phase SD and BW were independent predictors of all-cause death after adjusting for traditional risk factors. However, we acknowledge several limitations. This is a retrospective study from a single tertiary center, with selection and referral biases. We excluded patients with EF < 35%, QRS > 150 ms, and those with ischemic cardiomyopathy since these groups were evaluated prior with significant data. Important variables such as heart failure symptoms and severity were not available in the database; however, we did account for the use of diueretics which can reflect the presence of heart failure symptoms but not the severity. We used all-cause mortality rather than cardiac death since the former does not need adjudication and is more accurate. The number of events was relatively small; however, we adjusted for up to nine covariates to avoid overpowering the Cox proportional hazard model. Finally, LVMD was obtained at one time only; whether it is dynamic and might have changed over time due to unknown factors or cofounders is unknown.
New Knowledge Gained
In the current study, LVMD has proven to be a useful non-invasive prognostic marker with incremental value in patients with NICM, mild LV systolic dysfunction and minimal to intermediate electrical dyssynchrony. In such cohort that has been thought to be at lower risk of events, as compared to those with ischemic cardiomyopathy and severe LV dysfunction, the presence of significant LVMD is associated with doubling of mortality.
Conclusion
Increased LV mechanical dyssynchrony in patients with mild-to-moderate, NICM, and narrow-to-intermediate QRS duration is an independent predictor of increased all-cause mortality, and adds incremental prognostic value beyond traditional risk factors. Future studies are needed to validate these findings, and evaluate the utility and applicability of such findings in clinical practice.
References
Chen J, Garcia EV, Folks RD, Cooke CD, Faber TL, Tauxe EL, et al. Onset of left ventricular mechanical contraction as determined by phase analysis of ECG-gated myocardial perfusion SPECT imaging: Development of a diagnostic tool for assessment of cardiac mechanical dyssynchrony. J Nucl Cardiol 2005;12:687-95.
Lin X, Xu H, Zhao X, Folks RD, Garcia EV, Soman P, et al. Repeatability of left ventricular dyssynchrony and function parameters in serial gated myocardial perfusion SPECT studies. J Nucl Cardiol 2010;17:811-6.
AlJaroudi W, Jaber WA, Grimm RA, Marwick T, Cerqueira MD. Alternative methods for the assessment of mechanical dyssynchrony using phase analysis of gated single photon emission computed tomography myocardial perfusion imaging. Int J Cardiovasc Imaging 2012;28:1385-94.
AlJaroudi W, Alraies MC, Hachamovitch R, Jaber WA, Brunken R, Cerqueira MD, et al. Association of left ventricular mechanical dyssynchrony with survival benefit from revascularization: A study of gated positron emission tomography in patients with ischemic LV dysfunction and narrow QRS. Eur J Nucl Med Mol Imaging 2012;39:1581-91.
AlJaroudi W, Alraies MC, Menon V, Brunken RC, Cerqueira MD, Jaber WA. Predictors and incremental prognostic value of left ventricular mechanical dyssynchrony response during stress-gated positron emission tomography in patients with ischemic cardiomyopathy. J Nucl Cardiol 2012;19:958-69.
Aljaroudi WA, Hage FG, Hermann D, Doppalapudi H, Venkataraman R, Heo J, et al. Relation of left-ventricular dyssynchrony by phase analysis of gated SPECT images and cardiovascular events in patients with implantable cardiac defibrillators. J Nucl Cardiol 2010;17:398-404.
Boogers MM, Van Kriekinge SD, Henneman MM, Ypenburg C, Van Bommel RJ, Boersma E, et al. Quantitative gated SPECT-derived phase analysis on gated myocardial perfusion SPECT detects left ventricular dyssynchrony and predicts response to cardiac resynchronization therapy. J Nucl Med 2009;50:718-25.
Atchley AE, Trimble MA, Samad Z, Shaw LK, Pagnanelli R, Chen J, et al. Use of phase analysis of gated SPECT perfusion imaging to quantify dyssynchrony in patients with mild-to-moderate left ventricular dysfunction. J Nucl Cardiol 2009;16:888-94.
AlJaroudi W, Jaber WA, Cerqueira MD. Effect of tracer dose on left ventricular mechanical dyssynchrony indices by phase analysis of gated single photon emission computed tomography myocardial perfusion imaging. J Nucl Cardiol 2012;19:63-72.
Hansen CL, Goldstein RA, Akinboboye OO, Berman DS, Botvinick EH, Churchwell KB, et al. Myocardial perfusion and function: Single photon emission computed tomography. J Nucl Cardiol 2007;14:e39-60.
Aljaroudi W, Alraies MC, Brunken R, Cerquiera M, Jaber WA. Paradoxical septal motion from prior coronary artery bypass graft surgery does not impact left ventricular mechanical dyssynchrony by gated myocardial perfusion imaging. J Nucl Cardiol 2012;19:1190-7.
Lauer MS, Blackstone EH, Young JB, Topol EJ. Cause of death in clinical research: Time for a reassessment? J Am Coll Cardiol 1999;34:618-20.
Aljaroudi W, Koneru J, Heo J, Iskandrian AE. Impact of ischemia on left ventricular dyssynchrony by phase analysis of gated single photon emission computed tomography myocardial perfusion imaging. J Nucl Cardiol 2011;18:36-42.
Samad Z, Atchley AE, Trimble MA, Sun JL, Shaw LK, Pagnanelli R, et al. Prevalence and predictors of mechanical dyssynchrony as defined by phase analysis in patients with left ventricular dysfunction undergoing gated SPECT myocardial perfusion imaging. J Nucl Cardiol 2011;18:24-30.
Russo AM, Stainback RF, Bailey SR, Epstein AE, Heidenreich PA, Jessup M, et al. ACCF/HRS/AHA/ASE/HFSA/SCAI/SCCT/SCMR 2013 appropriate use criteria for implantable cardioverter-defibrillators and cardiac resynchronization therapy: A report of the American College of Cardiology Foundation appropriate use criteria task force, Heart Rhythm Society, American Heart Association, American Society of Echocardiography, Heart Failure Society of America, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol 2013;61:1318-68.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding: None.
Rights and permissions
About this article
Cite this article
Goldberg, A.S., Alraies, M.C., Cerqueira, M.D. et al. Prognostic value of left ventricular mechanical dyssynchrony by phase analysis in patients with non-ischemic cardiomyopathy with ejection fraction 35-50% and QRS < 150 ms. J. Nucl. Cardiol. 21, 57–66 (2014). https://doi.org/10.1007/s12350-013-9787-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-013-9787-y