Abstract
Subarachnoid hemorrhage (SAH) is a worldwide devastating type of stroke with high mortality and morbidity. Accumulating evidence show early brain injury (EBI) as the leading cause of mortality after SAH. The pathological processes involved in EBI include decreased cerebral blood flow, increased intracranial pressure, vasospasm, and disruption of the blood–brain barrier. In addition, neuroinflammation, oxidative stress, apoptosis, and autophagy have also been proposed to contribute to EBI. Among the various processes involved in EBI, neuronal apoptosis has been proven to be a key factor contributing to the poor prognosis of SAH patients. Meanwhile, as another important catabolic process maintaining the cellular and tissue homeostasis, autophagy has been shown to be neuroprotective after SAH. Studies have shown that enhancing autophagy reduced apoptosis, whereas inhibiting autophagy aggravate neuronal apoptosis after SAH. The physiological substrates and mechanisms of neuronal autophagy and apoptosis by which defects in neuronal function are largely unknown. In this review, we summarize and discuss the role of autophagy and apoptosis after SAH and contribute to further study for investigation of the means to control the balance between them.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subarachnoid hemorrhage (SAH), a disease that primarily occurs secondary to aneurysm rupture, affects 1 in 10,000 people annually, and is one of the most severe types of brain hemorrhage [1, 2]. Early brain injury (EBI) and delayed cerebral vasospasm are the main contributors impacting the poor outcomes of SAH patients [3]. However, treatments toward ameliorating cerebral vasospasm outcomes after SAH have been underwhelming. Recent studies have shifted focus from cerebral vasospasm to EBI which was first coined in 2004 to explain the acute pathophysiological event that occurs within the first 72 h after SAH. EBI accounts for brain injury, and is characterized by elevated intracranial pressure, autoregulation dysfunction, and brain edema within the first 72 h after SAH.
Autophagy is a cellular defense and survival mechanism under physiological conditions. The autophagy pathway is activated and lasts up to 3 days after SAH [4]. Meanwhile, the activation of the autophagy process has been shown to be neuroprotective [5]. Apoptosis is the most well-characterized type of programmed cell death. Apoptosis after SAH is one kind of important intracellular pathways, which leads to cell death in EBI [6]. Compelling evidence indicated that autophagy and apoptosis play important roles in EBI after SAH [7, 8]. Autophagy can precede apoptosis, and exerts a protective role in the early stages of programmed cell death [9, 10]. However, it can promote apoptosis under some circumstances [11].
In this review, we attempt to emphasize autophagy and apoptosis interplay after SAH, and we discuss several molecular and cellular mechanisms that are potential candidates for novel treatment options.
The autophagic process
Autophagy is a programmed cell death pathway in mammalian cells that is essential for elimination of obsolete cellular proteins and damaged organelles to maintain homeostasis [12, 13]. There are three primary types of autophagy process: macroautophagy chaperone-mediated autophagy, and microautophagy [14, 15].
Macroautophagy is the most demonstrated pathway in SAH and intracerebral hemorrhage [16, 17]. There are five stages in the macroautophagy process, including initiation, elongation, closure, maturation, fusion, and degradation (Fig. 1). To begin, an isolation membrane called the phagophore engulfs a portion of the cytoplasm, resulting in the formation of a double-membrane known as the autophagosome. After autophagosome formation, the autophagosome will deliver its cargo to the lysosome and the outer autophagosomal and lysosomal membranes will fuse [18]. Macroautophagy is regulated by evolutionarily conserved autophagy related genes (ATG) in yeast. There are more than 40 ATG genes identified in yeast. Of which, 15 are known for their core ATG genes. They are involved in both selective and nonselective autophagy [19]. ATG1-ATG13-ATG17-ATG31-ATG29 assemble into a kinase complex to induce the formation of the autophagosome. In mammalian cells, the UNC-51-like kinase family comprise a complex, which includes ULK1, ATG13, ATG101, and FIP200. It plays a critical role in the induction of autophagy [20, 21]. Under nutrient-rich conditions, the serine/threonine kinase mammalian Target of rapamycin (mTOR) associates with the complex and phosphorylates, as well as inactivates ULK1/2 and ATG13. Meanwhile, when cells are starved for nutrients, the mTOR complex 1 dissociates, leading to the dephosphorylation of ULK1/2 and ATG13 and initiation of macroautophagy [22, 23].
The apoptotic process
Apoptosis is a programmed cell death process by which a cell ceases to grow and enters a controlled cell death stage without any spillage of its contents into the surrounding environment. There are two main apoptotic pathways: the intrinsic or mitochondrial pathway and the extrinsic or death receptor pathway [17, 24] (Fig. 2). The intrinsic pathway, which is mediated by the mitochondrial release of cytochrome c, activates different caspases as downstream signals [25, 26]. The extrinsic pathway originates from the activation of cell death receptors [27, 28]. Both pathways share the final caspase activation step after the activation of different intermediate molecules by the signaling cascade, leading to the cleavage of different proteins.
The intrinsic pathway involves a series of molecular events occurring entirely within cells. Many stimuli, such as toxins, DNA damage, trophic factor deprivation, ionizing radiation, and other cellular stress, could trigger the intrinsic pathway. As the core of the intrinsic pathway, mitochondria release a number of pro-apoptotic factors into the cytoplasm to induce or regulate the intrinsic apoptosis pathway [25, 29]. Among the pro-apoptotic factors, the most important is cytochrome c. In normal cells, the mature form of cytochrome c is remained in an enclosed space between the inner and outer mitochondrial membranes (IMM and OMM) where it functions to remove electrons from respiratory complex III (BCL complex) to complex IV (cytochrome oxidase) in the electron-transport chain. The release of cytochrome c is positively regulated by pro-apoptotic BCL-2 family members, including BAX (BCL-2 associated X protein), BAK (BCL-2 antagonist killer 1), BID, BIM, and PUMA, and is negatively regulated by anti-apoptotic BCL-2 family members, including BCL-XL, BCL-2, BCL-W, and MCL1. Once they receive the apoptotic signals, the pro-apoptotic BCL-2 family oligomerizes and inserts into the outer mitochondrial membrane, leading to permeabilization of the outer mitochondrial membrane and allowing the redistribution of cytochrome c into the cytoplasm [30, 31]. Cytochrome c binds to APAF-1 in the cytoplasm and induces oligomerization of APAF1 molecules. This binding induces the conformational change in APAF1, exposing its caspase recruitment domain (CARD domain) and its oligomerization domains, thereby assembling APAF1s and caspase-9 into a complex known as the apoptosome [32]. Caspase-9 cleaves and activates the downstream effector caspases, such as caspases-3 and -7, which will cleave many protein substrates and cause cell death [33]. The activation of caspase-3 is negatively regulated by the inhibitory apoptosis (IAP) protein family, such as XIAP, c-IAP1, and c-IAP2. Other proteins released from mitochondria, such as apoptosis-inducing factor (AIF) and SAC, also have pro-apoptotic functions [34].
The extrinsic pathway is also called the death receptor pathway. The pro-apoptotic death receptors include TNFR1, TNFR2, Fas, and TRAIL receptors, DR4 and DR5 [35]. When pro-apoptotic ligands bind to cell surface death receptors, the extrinsic pathway is activated. There is one conserved protein–protein interaction domain, known as the death domain, in the intracellular domains of the proapoptotic death receptors. Upon binding to the ligands, the adaptor protein, FADD (Fas-associated protein with death domain), forms a complex with the initiator 8 or 10, called the DISC (death-inducing signaling complex) [36]. The formation of this complex activates caspase-8, which in turn, cleaves and activates downstream effector caspases-3, -6, and -7, as well as BID cleavage [37].
The relationship between autophagy and apoptosis
The relationship between autophagy and apoptosis is relatively complex, including the physical and functional interactions between the several proteins (Fig. 3). Autophagy and apoptosis are regulated by various transcription factors [38]. They share some same triggering by different protein kinase cascades. While apoptosis is invariably involved in cell death, autophagy plays dual roles in cell death and survival, depending on the cellular context [39].
As important regulatory factors in cell apoptosis, an increasing number of studies have revealed the importance of BCL-2 family members in autophagy. As pro-apoptotic proteins, BCL-xl and BCL-2 can bind to the BCL-2 homology (BH) 3 domain of Beclin 1 through their BH3 receptor domain [40, 41]. The regulation of the BCL-2-Beclin 1 has been demonstrated by the competitive substitution of the Beclin 1 BH3 domain by other BCL-2 family proteins, such as BNIP and BAD, but not by BAK and BAX [42, 43]. When the BH3 domain of Beclin 1 or the BH3 receptor domain of BCL-xl is mutated, BCL-xl is unable to inhibit Beclin 1-induced autophagy [44]. The phosphorylation of BCL-2 blocks its binding to Beclin-1, meaning that phosphorylated BCL-2 loses its ability to inhibit autophagy [45]. AMPK can dissociate the BCL-2-Beclin 1 complex and promote the formation of the Beclin 1- PI3K complex to enhance autophagy [46]. Phosphorylation of BCL-2 at multiple sites by c Jun N terminal protein kinase 1 (JNK1) and extracellular signal related kinase (Erk) has been shown to reduce binding of BCL-2 to Beclin, causing the activation of autophagy [46,47,48]. There are two cellular resources of BCL-2, the endoplasmic reticulum and the mitochondria, and both can regulate apoptosis and autophagy. Endoplasmic reticulum proteins and nutrient deprivation autophagy factor 1 facilitate the binding of BCL-2 to Beclin at the endoplasmic reticulum to inhibit autophagy, while endoplasmic reticulum localized BH3-only protein and B cell interacting killer (BIK) [49].
There is another regulation between apoptosis and autophagy in spatial separation of proteins to cellular compartments. MCL1, the anti-apoptotic protein, has been proven to regulate autophagy. The degradation is an early event in nutrient deprivation condition and apoptosis induction. Under nutrient deprivation conditions, MCL1 levels regulate activation of autophagy [50, 51]. The mammalian target of rapamycin (mTOR) kinase plays an important role in the interplay between apoptosis and autophagy as well. The deletion of Raptor, a positive regulator of mTOR, promotes both apoptosis and autophagy by activating caspase-3, leading to abnormal mitochondria [52, 53]. Under hypoxic conditions, the mTOR pathway is inhibited by BNIP3, which directly binds to and inactivates Rheb. Therefore, mTOR induces a positive relationship of apoptosis and autophagy in a caspase-dependent manner [54, 55]. The death-associated protein kinase (DAPK) is a calcium/calmodulin-regulated Ser/Thr kinase that mediates cell death induced by diverse death signals. DAPK has also been proven to be related to cellular autophagy and apoptosis [56]. DAPK is activated in ER stress conditions to trigger a mixed reaction of cellular autophagy and apoptosis [57]. In times of ER stress, DAPK integrates signals from apoptotic and autophagic pathways to induce cell death [58]. As a classic ligand that participates in activation of the extrinsic apoptotic pathway, TRAIL promotes an autophagic program while activating caspase-mediated apoptosis during the process of lumen formation in human mammary epithelial cells [59]. Moreover, TRAIL induces FADD, which in turn activates cellular apoptosis and autophagy. TRAIL supports the positive relationship between apoptosis and autophagy [60].
Reactive oxygen species (ROS) are classified as a heterogeneous group of molecules naturally generated in cellular metabolism of diatomic oxygen [61]. The relationship between ROS and autophagy represents an adjusted negative feedback mechanism by which autophagy eliminates the source of oxidative stress and protects the cells from oxidative damage [62]. ROS induces cellular autophagy, whereas autophagy reduces the levels of ROS as it consumes the major source of ROS, damaged mitochondria. Many factors, including hypoxia, TNF-α, starvation, and nerve growth factor deprivation, simultaneously trigger both autophagic flux and an increase in intracellular ROS [63, 64]. Several environmental endocrine-disruptors can increase oxidative stress and ROS production, which can ultimately lead to the activation of cell death processes, such as apoptosis. Several apoptotic effectors, including caspases, BCL-2, and cytochrome c, are significantly regulated by cellular ROS [65, 66]. Licarin A induces autophagy and apoptosis in non-small cell lung cancer cells by ROS. Furthermore, upregulation of autophagy by mTOR-dependent pathways appears to be cytoprotective in preventing CYT997-induced excessively high levels of ROS [67].
To sum, autophagy and apoptosis are connected by several molecules in order to keep the coordinate regulation in survival and death.
The roles of autophagy and apoptosis interplay in SAH
The pathophysiological mechanism of SAH is complicated and remains incompletely understood. SAH causes a sudden increase in intracranial pressure, which causes a decrease in blood perfusion pressure. The following events, such as acute hydrocephalus, platelet aggregation, microvascular alterations, reperfusion injury, and acute vasospasm, may contribute to EBI after SAH [68,69,70]. Cellular apoptosis may be seen in endothelium, cortical, subcortical, or hippocampal neurons after SAH [71,72,73]. The mechanisms, that initiate apoptosis after SAH, include global ischemia, decreased cerebral perfusion pressure, microcirculatory disturbance, transient global ischemia, and blood toxicity [68,69,70]. There are several apoptotic pathways that are believed to be important in relation to SAH. First, the death receptor pathway: SAH can activate many death receptors including Fas, P2X7R, TNF receptor, and death receptor 4/5, leading to the activation of caspase-3, and thus activating apoptosis [74, 75]. Second, the mitochondrial pathway: after SAH, mitochondrial matrix releases cytochrome c, which binds with APAF-1 and pro-caspase-9 to form the apoptosome [76]. The Cytochrome c-procaspase-9-APAF-1 complex further activates downstream effector molecules to trigger apoptosis. Third, the p53 pathway in response to SAH: p53 regulates the apoptotic cascade [77,78,79]. Last, the caspase-independent pathway: after SAH, p53 regulates the release of apoptosis-inducing factor in the absence of APAF-1, and then activates the caspase-independent pathway [30]. Inhibition of apoptosis has been proven to have a neuroprotective effect after SAH, and has become a key target in preventing and treating EBI after SAH.
After SAH, the levels of the autophagy marker proteins, such as Beclin-1 and LC3, were significantly increased in the ipsilateral region and persisted for 3 days. It was shown that autophagy activity peaks at 24 h after SAH. However, the role of autophagy remains controversial. After SAH, autophagic activation is accompanied by inhibition of apoptosis and improvement of EBI [80, 81]. Study has reported gradually increased levels of autophagy-related proteins, such as Beclin-1 and LC3- II, over 24 h after SAH. The expression of Beclin-1 and LC3- II in the basilar artery wall is upregulated during the first 48 h after SAH [82, 83]. Lee et al. found out that Beclin-1, LC3- II, and cathepsin-d gradually increased within 24 h after SAH induction, but decreased at 72 h. Beclin-1 and cathepsin-d are expressed in neurons, but not in astrocytes [84].
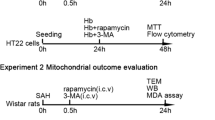
Shao et al. reported that 3-MA inhibition of class III PI3K activity and autophagy activation resulted in increased cell apoptosis after SAH [85, 86]. In contrast, treatment with RAP, inducing autophagy by inhibiting mTOR, significantly reduced apoptosis in the EBI phase [87, 88]. To investigate the interaction or balance between autophagy and apoptosis after SAH at the histological level, dual immunofluorescence staining was performed with apoptotic marker, cleaved caspase-3, and autophagy marker, p62 to show that resveratrol could upregulate autophagy while inhibiting apoptosis after SAH in rats [87]. Sun et al. found that after SAH, caspase-3 expression was concentrated closely around the injured core, whereas Beclin 1 expression could only be observed at a small distance from the blood clot area, but not at the injured core [89]. They also found that cells were either stained with caspase-3 or with Beclin 1, but not both. This led to the observation of a “confrontation line” between caspase-3-positive cells and Beclin 1-positive cells, suggesting that when a cell expressed a large amount of autophagy-initiating protein, Beclin 1, it would not enter late phase apoptosis [90]. In conclusion, autophagy and apoptosis might be two opposing processes for individual cells after SAH. In addition, administration of osteopontin improved neurobehavioral dysfunction, enhanced autophagy while inhibiting apoptosis, and regulated autophagy-apoptosis interaction [91, 92].
Conclusion
Autophagy exerts critical roles in maintaining intracellular homeostasis within the brain in the setting of SAH. Proper functioning of autophagic mechanisms has a pro-survival effect and reduces apoptotic cell death after SAH. However, if SAH exceeds a certain stress threshold, autophagic mechanisms lead to increased apoptotic cell death. Therefore, regulation of the autophagic and apoptotic interplay processes in the setting of SAH will likely lead to a beneficial effect that will allow us to develop effective therapeutic strategies for SAH patients.
References
Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, Fung GL, Goldstein JN, Macdonald RL, Mitchell PH, Scott PA, Selim MH, Woo D (2015) Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 46:2032–2060
Suzuki H (2022) Letter to irreversible neuronal damage begins just after aneurysm rupture in poor-grade subarachnoid hemorrhage patients. Transl Stroke Res 13:355–356
Neulen A, Meyer S, Kramer A, Pantel T, Kosterhon M, Kunzelmann S, Goetz H, Thal SC (2018) Large vessel vasospasm is not associated with cerebral cortical hypoperfusion in a murine model of subarachnoid hemorrhage. Transl Stroke Res 10:319–326
Chen S, Wu H, Tang J, Zhang J, Zhang JH (2015) Neurovascular events after subarachnoid hemorrhage: focusing on subcellular organelles. Acta Neurochir Suppl 120:39–46
Zheng Y, Zhou Z, Han F, Chen Z (2021) Special issue: neuroinflammatory pathways as treatment targets in brain disorders autophagic regulation of neuroinflammation in ischemic stroke. Neurochem Int 148:105114
Ruan W, Hu J, Zhou H, Li Y, Xu C, Luo Y, Chen T, Xu B, Yan F, Chen G (2020) Intranasal wnt-3a alleviates neuronal apoptosis in early brain injury post subarachnoid hemorrhage via the regulation of wnt target PPAN mediated by the moonlighting role of aldolase C. Neurochem Int 134:104656
Shi L, Liang F, Zheng J, Zhou K, Chen S, Yu J, Zhang J (2018) Melatonin regulates apoptosis and autophagy Via ROS-MST1 pathway in subarachnoid hemorrhage. Front Mol Neurosci 11:93
Guo D, Xie J, Zhao J, Huang T, Guo X, Song J (2018) Resveratrol protects early brain injury after subarachnoid hemorrhage by activating autophagy and inhibiting apoptosis mediated by the Akt/mTOR pathway. NeuroReport 29:368–379
Jellinger KA, Stadelmann CH (2000) The enigma of cell death in neurodegenerative disorders. J Neural Transm Suppl. https://doi.org/10.1007/978-3-7091-6301-6_2
Boya P, González-Polo RA, Casares N, Perfettini JL, Dessen P, Larochette N, Métivier D, Meley D, Souquere S, Yoshimori T, Pierron G, Codogno P, Kroemer G (2005) Inhibition of macroautophagy triggers apoptosis. Mol Cell Biol 25:1025–1040
Codogno P, Meijer AJ (2005) Autophagy and signaling: their role in cell survival and cell death. Cell Death Differ 12(Suppl 2):1509–1518
White E (2012) Deconvoluting the context-dependent role for autophagy in cancer. Nature Rev Cancer 12:401–410
Klionsky DJ, Petroni G, Amaravadi RK, Baehrecke EH, Ballabio A, Boya P, Bravo-San Pedro JM, Cadwell K, Cecconi F, Choi AMK, Choi ME, Chu CT, Codogno P, Colombo MI, Cuervo AM, Deretic V, Dikic I, Elazar Z, Eskelinen EL, Fimia GM, Gewirtz DA, Green DR, Hansen M, Jaattela M, Johansen T, Juhasz G, Karantza V, Kraft C, Kroemer G, Ktistakis NT, Kumar S, Lopez-Otin C, Macleod KF, Madeo F, Martinez J, Melendez A, Mizushima N, Munz C, Penninger JM, Perera RM, Piacentini M, Reggiori F, Rubinsztein DC, Ryan KM, Sadoshima J, Santambrogio L, Scorrano L, Simon HU, Simon AK, Simonsen A, Stolz A, Tavernarakis N, Tooze SA, Yoshimori T, Yuan J, Yue Z, Zhong Q, Galluzzi L, Pietrocola F (2021) Autophagy in major human diseases. EMBO J 40:e108863
Sonsky I, Vodicka P, Vodickova Kepkova K, Hansikova H (2021) Mitophagy in Huntington’s disease. Neurochem Int 149:105147
Durocher M, Knepp B, Yee A, Jickling G, Rodriguez F, Ng K, Zhan X, Hamade F, Ferino E, Amini H, Carmona-Mora P, Hull H, Ander BP, Sharp FR, Stamova B (2021) Molecular correlates of hemorrhage and edema volumes following human intracerebral hemorrhage implicate inflammation, autophagy, mRNA splicing, and T cell receptor signaling. Transl Stroke Res 12:754–777
Liang Y, Deng Y, Zhao J, Liu L, Wang J, Chen P, Zhang Q, Sun C, Wang Y, Xiang Y, He Z (2022) Ferritinophagy is involved in experimental subarachnoid hemorrhage-induced neuronal ferroptosis. Neurochem Res 47:692–700
Schipper HM, Song W, Tavitian A, Cressatti M (2019) The sinister face of heme oxygenase-1 in brain aging and disease. Prog Neurobiol 172:40–70
Tukaj C (2013) The significance of macroautophagy in health and disease. Folia Morphol 72:87–93
Nakatogawa H, Suzuki K, Kamada Y, Ohsumi Y (2009) Dynamics and diversity in autophagy mechanisms: lessons from yeast. Nat Rev Mol cell Biol 10:458–467
Levine B, Mizushima N, Virgin HW (2011) Autophagy in immunity and inflammation. Nature 469:323–335
Mizushima N, Komatsu M (2011) Autophagy: renovation of cells and tissues. Cell 147:728–741
Kim J, Kundu M, Viollet B, Guan KL (2011) AMPK and mTOR regulate autophagy through direct phosphorylation of Ulk1. Nat cell Biol 13:132–141
Zheng J, Wang Y, Liu Y, Han S, Zhang Y, Luo Y, Yan Y, Li J, Zhao L (2022) cPKCgamma deficiency exacerbates autophagy impairment and hyperphosphorylated tau buildup through the AMPK/mTOR pathway in mice with Type 1 Diabetes Mellitus. Neurosci Bull. https://doi.org/10.1007/s12264-022-00863-4
Igney FH, Krammer PH (2002) Death and anti-death: tumour resistance to apoptosis. Nat Rev Cancer 2:277–288
Saelens X, Festjens N, Vande Walle L, van Gurp M, van Loo G, Vandenabeele P (2004) Toxic proteins released from mitochondria in cell death. Oncogene 23:2861–2874
Hegazy AM, Chen N, Lin H, Babu VS, Li F, Yang Y, Qin Z, Shi F, Li J, Lin L (2021) Induction of apoptosis in SSN-1cells by snakehead fish Vesiculovirus (SHVV) via Matrix protein dependent intrinsic pathway. Fish Shellfish Immunol 113:24–34
Wajant H (2002) The Fas signaling pathway: more than a paradigm. Science (New York, NY) 296:1635–1636
Goelz N, Eekels JJM, Pantic M, Kamber CT, Speer O, Franzoso FD, Schmugge M (2021) Platelets express adaptor proteins of the extrinsic apoptosis pathway and can activate caspase-8. PLoS ONE 16:e0244848
Yoon JH, Her S, Kim M, Jang IS, Park J (2012) The expression of damage-regulated autophagy modulator 2 (DRAM2) contributes to autophagy induction. Mol Biol Rep 39:1087–1093
Elmore S (2007) Apoptosis: a review of programmed cell death. Toxicol Pathol 35:495–516
Cory S, Adams JM (2002) The Bcl2 family: regulators of the cellular life-or-death switch. Nat Rev Cancer 2:647–656
Acehan D, Jiang X, Morgan DG, Heuser JE, Wang X, Akey CW (2002) Three-dimensional structure of the apoptosome: implications for assembly, procaspase-9 binding, and activation. Mol Cell 9:423–432
Cain K, Bratton SB, Cohen GM (2002) The Apaf-1 apoptosome: a large caspase-activating complex. Biochimie 84:203–214
Ekert PG, Vaux DL (2005) The mitochondrial death squad: hardened killers or innocent bystanders? Curr Opin Cell Biol 17:626–630
Locksley RM, Killeen N, Lenardo MJ (2001) The TNF and TNF receptor superfamilies: integrating mammalian biology. Cell 104:487–501
Kischkel FC, Hellbardt S, Behrmann I, Germer M, Pawlita M, Krammer PH, Peter ME (1995) Cytotoxicity-dependent APO-1 (Fas/CD95)-associated proteins form a death-inducing signaling complex (DISC) with the receptor. EMBO J 14:5579–5588
Teringova E, Tousek P (2017) Apoptosis in ischemic heart disease. J Transl Med 15:87
Sorice M (2022) Crosstalk of autophagy and apoptosis. Cells. https://doi.org/10.3390/cells11091479
Thorburn A (2020) Crosstalk between autophagy and apoptosis: mechanisms and therapeutic implications. Prog Mol Biol Transl Sci 172:55–65
Oberstein A, Jeffrey PD, Shi Y (2007) Crystal structure of the Bcl-XL-Beclin 1 peptide complex: Beclin 1 is a novel BH3-only protein. J Biol Chem 282:13123–13132
He Y, Wang W, Xu X, Yang B, Yu X, Wu Y, Wang J (2022) Mettl3 inhibits the apoptosis and autophagy of chondrocytes in inflammation through mediating Bcl2 stability via Ythdf1-mediated m(6)A modification. Bone 154:116182
Maiuri MC, Criollo A, Kroemer G (2010) Crosstalk between apoptosis and autophagy within the Beclin 1 interactome. EMBO J 29:515–516
Lindqvist LM, Heinlein M, Huang DC, Vaux DL (2014) Prosurvival Bcl-2 family members affect autophagy only indirectly, by inhibiting Bax and Bak. Proc Natl Acad Sci USA 111:8512–8517
Galonek HL, Hardwick JM (2006) Upgrading the BCL-2 network. Nat Cell Biol 8:1317–1319
Pattingre S, Tassa A, Qu X, Garuti R, Liang XH, Mizushima N, Packer M, Schneider MD, Levine B (2005) Bcl-2 antiapoptotic proteins inhibit Beclin 1-dependent autophagy. Cell 122:927–939
He C, Zhu H, Li H, Zou MH, Xie Z (2013) Dissociation of Bcl-2-Beclin1 complex by activated AMPK enhances cardiac autophagy and protects against cardiomyocyte apoptosis in diabetes. Diabetes 62:1270–1281
Wei Y, Pattingre S, Sinha S, Bassik M, Levine B (2008) JNK1-mediated phosphorylation of Bcl-2 regulates starvation-induced autophagy. Mol Cell 30:678–688
Jiang H, Wen X, Zhang X, Zhong X, Li Z, Zhang B (2022) Lens culinaris agglutinin inhibits human hepatoma cell migration via mannose and fucose-mediated ERK1/2 and JNK1/2/3 signalling pathway. Mol Biol Rep. https://doi.org/10.1007/s11033-022-07582-z
Chang NC, Nguyen M, Germain M, Shore GC (2010) Antagonism of Beclin 1-dependent autophagy by BCL-2 at the endoplasmic reticulum requires NAF-1. EMBO J 29:606–618
Thomas RL, Gustafsson AB (2013) MCL1 is critical for mitochondrial function and autophagy in the heart. Autophagy 9:1902–1903
Germain M, Nguyen AP, Le Grand JN, Arbour N, Vanderluit JL, Park DS, Opferman JT, Slack RS (2011) MCL-1 is a stress sensor that regulates autophagy in a developmentally regulated manner. EMBO J 30:395–407
Shende P, Plaisance I, Morandi C, Pellieux C, Berthonneche C, Zorzato F, Krishnan J, Lerch R, Hall MN, Rüegg MA, Pedrazzini T, Brink M (2011) Cardiac raptor ablation impairs adaptive hypertrophy, alters metabolic gene expression, and causes heart failure in mice. Circulation 123:1073–1082
Sharma A, Mehan S (2021) Targeting PI3K-AKT/mTOR signaling in the prevention of autism. Neurochem Int 147:105067
Li Y, Wang Y, Kim E, Beemiller P, Wang CY, Swanson J, You M, Guan KL (2007) Bnip3 mediates the hypoxia-induced inhibition on mammalian target of rapamycin by interacting with Rheb. J Biol Chem 282:35803–35813
Movahhed P, Saberiyan M, Safi A, Arshadi Z, Kazerouni F, Teimori H (2022) The impact of DAPK1 and mTORC1 signaling association on autophagy in cancer. Mol Biol Rep. https://doi.org/10.1007/s11033-022-07154-1
Bialik S, Kimchi A (2006) The death-associated protein kinases: structure, function, and beyond. Ann Rev Biochem 75:189–210
Nasiri-Ansari N, Nikolopoulou C, Papoutsi K, Kyrou I, Mantzoros CS, Kyriakopoulos G, Chatzigeorgiou A, Kalotychou V, Randeva MS, Chatha K, Kontzoglou K, Kaltsas G, Papavassiliou AG, Randeva HS, Kassi E (2021) Empagliflozin attenuates non-alcoholic fatty liver disease (NAFLD) in high fat diet fed ApoE((-/-)) mice by activating autophagy and reducing ER stress and apoptosis. Int J Mol Sci 22:818
Gozuacik D, Bialik S, Raveh T, Mitou G, Shohat G, Sabanay H, Mizushima N, Yoshimori T, Kimchi A (2008) DAP-kinase is a mediator of endoplasmic reticulum stress-induced caspase activation and autophagic cell death. Cell Death Differ 15:1875–1886
Mills KR, Reginato M, Debnath J, Queenan B, Brugge JS (2004) Tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) is required for induction of autophagy during lumen formation in vitro. Proc Natl Acad Sci USA 101:3438–3443
Thorburn J, Moore F, Rao A, Barclay WW, Thomas LR, Grant KW, Cramer SD, Thorburn A (2005) Selective inactivation of a Fas-associated death domain protein (FADD)-dependent apoptosis and autophagy pathway in immortal epithelial cells. Mol Biol Cell 16:1189–1199
Kim SA, Jang JH, Kim W, Lee PR, Kim YH, Vang H, Lee K, Oh SB (2022) Mitochondrial reactive oxygen species elicit acute and chronic itch via transient receptor potential canonical 3 activation in mice. Neurosci Bull 38:373–385
Gao L, Loveless J, Shay C, Teng Y (2020) Targeting ROS-mediated crosstalk between autophagy and apoptosis in cancer. Adv Exp Med Biol 1260:1–12
Kirkland RA, Adibhatla RM, Hatcher JF, Franklin JL (2002) Loss of cardiolipin and mitochondria during programmed neuronal death: evidence of a role for lipid peroxidation and autophagy. Neuroscience 115:587–602
Kirkland RA, Saavedra GM, Franklin JL (2007) Rapid activation of antioxidant defenses by nerve growth factor suppresses reactive oxygen species during neuronal apoptosis: evidence for a role in cytochrome c redistribution. J Neurosci Off J Soc Neurosci 27:11315–11326
Luo Z, Xu X, Sho T, Zhang J, Xu W, Yao J, Xu J (2019) ROS-induced autophagy regulates porcine trophectoderm cell apoptosis, proliferation, and differentiation. Am J Physiol Cell Physiol 316:C198–C209
Li B, Zhou P, Xu K, Chen T, Jiao J, Wei H, Yang X, Xu W, Wan W, Xiao J (2020) Metformin induces cell cycle arrest, apoptosis and autophagy through ROS/JNK signaling pathway in human osteosarcoma. Int J Biol Sci 16:74–84
Maheswari U, Ghosh K, Sadras SR (2018) Licarin A induces cell death by activation of autophagy and apoptosis in non-small cell lung cancer cells. Apoptosis Int J Progr Cell Death 23:210–225
Park S, Yamaguchi M, Zhou C, Calvert JW, Tang J, Zhang JH (2004) Neurovascular protection reduces early brain injury after subarachnoid hemorrhage. Stroke 35:2412–2417
Bederson JB, Levy AL, Ding WH, Kahn R, DiPerna CA, Jenkins AL 3rd, Vallabhajosyula P (1998) Acute vasoconstriction after subarachnoid hemorrhage. Neurosurgery 42:352–360 (discussion 360-352)
Matz PG, Copin JC, Chan PH (2000) Cell death after exposure to subarachnoid hemolysate correlates inversely with expression of CuZn-superoxide dismutase. Stroke 31:2450–2459
Prunell GF, Mathiesen T, Diemer NH, Svendgaard NA (2003) Experimental subarachnoid hemorrhage: subarachnoid blood volume, mortality rate, neuronal death, cerebral blood flow, and perfusion pressure in three different rat models. Neurosurgery 52:165–175
Endo H, Nito C, Kamada H, Yu F, Chan PH (2006) Akt/GSK3beta survival signaling is involved in acute brain injury after subarachnoid hemorrhage in rats. Stroke 37:2140–2146
Chung CL, Wu CH, Huang YH, Wu SC, Chai CY, Tsai HP, Kwan AL (2022) Blocking hepatoma-derived growth factor attenuates vasospasm and neuron cell apoptosis in rats subjected to subarachnoid hemorrhage. Transl Stroke Res 13:300–310
Shioda N, Ishigami T, Han F, Moriguchi S, Shibuya M, Iwabuchi Y, Fukunaga K (2007) Activation of phosphatidylinositol 3-kinase/protein kinase B pathway by a vanadyl compound mediates its neuroprotective effect in mouse brain ischemia. Neuroscience 148:221–229
Xu MX, Zhao GL, Hu X, Zhou H, Li SY, Li F, Miao Y, Lei B, Wang Z (2022) P2X7/P2X4 receptors mediate proliferation and migration of retinal microglia in experimental glaucoma in mice. Neurosci Bull. https://doi.org/10.1007/s12264-022-00833-w
Satturu V, Vattikuti JLJDS, Kumar A, Singh RKMSP, Zaw H, Jubay ML, Satish L, Rathore A, Mulinti S, Lakshmi H, Chakraborty A, Thirunavukkarasu N (2020) Multiple genome wide association mapping models identify quantitative trait nucleotides for BROWN Planthopper (Nilaparvata lugens) resistance in MAGIC indica population of rice. Vaccines (Basel) 8:608
Cahill J, Calvert JW, Solaroglu I, Zhang JH (2006) Vasospasm and p53-induced apoptosis in an experimental model of subarachnoid hemorrhage. Stroke 37:1868–1874
Cahill J, Calvert JW, Zhang JH (2006) Mechanisms of early brain injury after subarachnoid hemorrhage. J Cereb Blood Flow Metab 26:1341–1353
Cahill J, Zhang JH (2009) Subarachnoid hemorrhage: is it time for a new direction? Stroke 40:S86-87
Li T, Sun KJ, Wang HD, Zhou ML, Ding K, Lu XY, Wei WT, Wang CX, Zhou XM (2015) Tert-butylhydroquinone ameliorates early brain injury after experimental subarachnoid hemorrhage in mice by enhancing Nrf2-independent autophagy. Neurochem Res 40:1829–1838
Galluzzi L, Bravo-San Pedro JM, Blomgren K, Kroemer G (2016) Autophagy in acute brain injury. Nat Rev Neurosci 17:467–484
Wang Z, Shi XY, Yin J, Zuo G, Zhang J, Chen G (2012) Role of autophagy in early brain injury after experimental subarachnoid hemorrhage. J Mol Neurosci 46:192–202
Zheng B, Zhou X, Pang L, Che Y, Qi X (2021) Baicalin suppresses autophagy-dependent ferroptosis in early brain injury after subarachnoid hemorrhage. Bioengineered 12:7794–7804
Lee JY, He Y, Sagher O, Keep R, Hua Y, Xi G (2009) Activated autophagy pathway in experimental subarachnoid hemorrhage. Brain Res 1287:126–135
Shao A, Wang Z, Wu H, Dong X, Li Y, Tu S, Tang J, Zhao M, Zhang J, Hong Y (2016) Enhancement of autophagy by histone deacetylase inhibitor Trichostatin A ameliorates neuronal apoptosis after subarachnoid hemorrhage in rats. Mol Neurobiol 53:18–27
Wang J, Wang Y, Zuo Y, Duan J, Pan A, Li JM, Yan XX, Liu F (2021) MFGE8 mitigates brain injury in a rat model of SAH by maintaining vascular endothelial integrity via TIGbeta5/PI3K/CXCL12 signaling. Exp Brain Res 239:2193–2205
Jing CH, Wang L, Liu PP, Wu C, Ruan D, Chen G (2012) Autophagy activation is associated with neuroprotection against apoptosis via a mitochondrial pathway in a rat model of subarachnoid hemorrhage. Neuroscience 213:144–153
Huang W, Li N, Zhang Y, Wang X, Yin M, Lei QY (2022) AHCYL1 senses SAH to inhibit autophagy through interaction with PIK3C3 in an MTORC1-independent manner. Autophagy 18:309–319
Sun L, Ma Y, Zhang Z, Li X, Chen Y, Liu G, Fu A (2018) ROCK2 regulates autophagy in the hippocampus of rats after subarachnoid hemorrhage. NeuroReport 29:1571–1577
Cai Z, Zhang H, Song H, Piao Y, Zhang X (2020) Edaravone combined with cinepazide maleate on neurocyte autophagy and neurological function in rats with subarachnoid hemorrhage. Exp Ther Med 19:646–650
Sun CM, Enkhjargal B, Reis C, Zhou KR, Xie ZY, Wu LY, Zhang TY, Zhu QQ, Tang JP, Jiang XD, Zhang JH (2019) Osteopontin attenuates early brain injury through regulating autophagy-apoptosis interaction after subarachnoid hemorrhage in rats. CNS Neurosci Ther 25:1162–1172
Asada R, Suzuki H (2022) Osteopontin in post-subarachnoid hemorrhage pathologies. J Integr Neurosci 21:62
Acknowledgements
SC and QW were the principal investigators. YZ and YL wrote the paper. YL made the original figures. YZ and YL revised the figures. CL handled the language and made some comments.
Funding
This research was supported by the National Natural Science Foundation of China (81971107).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest, financial or otherwise.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhao, Y., Luo, Y., Liu, Y. et al. The role of autophagy and apoptosis in early brain injury after subarachnoid hemorrhage: an updated review. Mol Biol Rep 49, 10775–10782 (2022). https://doi.org/10.1007/s11033-022-07756-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07756-9