Abstract
Objective
To report a kindred with an association between hereditary primary lateral sclerosis (PLS) and progressive nonfluent aphasia.
Patients and methods
Six members from a kindred with 15 affected individuals spanning three generations, suffered from spasticity without muscle atrophy or fasciculation, starting in the lower limbs and spreading to the upper limbs and bulbar musculature, followed by effortful speech, nonfluent language and dementia, in 5 deceased members. Disease onset was during the sixth decade of life, or later. Cerebellar ataxia was the inaugural manifestation in two patients, and parkinsonism, in another.
Results
Neuropathological examination in two patients demonstrated degeneration of lateral corticospinal tracts in the spinal cord, without loss of spinal, brainstem, or cerebral motor neurons. Greater loss of corticospinal fibers at sacral and lumbar, rather than at cervical or medullary levels was demonstrated, supporting a central axonal dying-back pathogenic mechanism. Marked reduction of myelin and nerve fibers in the frontal lobes was also present. Argyrophilic grain disease and primary age-related tauopathy were found in one case each, and considered incidental findings. Genetic testing, including exome sequencing aimed at PLS, ataxia, hereditary spastic paraplegia, and frontotemporal lobe dementia, triplet-repeated primed polymerase chain reaction aimed at dominant spinocerebellar ataxias, and massive sequencing of the human genome, yielded negative results.
Conclusion
A central distal axonopathy affecting the corticospinal tract, exerted a pathogenic role in the dominantly inherited PLS-progressive nonfluent aphasia association, described herein. Further molecular studies are needed to identify the causative mutation in this disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary lateral sclerosis (PLS) is a rare spastic spinobulbar neurodegenerative disease, differentiated from amyotrophic lateral sclerosis (ALS) by preservation of lower motor neurons. Primary progressive aphasia (PPA) is a variant of frontotemporal dementia (FTLD); to our knowledge, the association between hereditary PLS and progressive nonfluent aphasia, a subtype of PPA, has been rarely reported in the medical literature. Here, we describe a kindred with such an association, which spanned three generations.
Patients and methods
The pedigree of the family under study appears in Fig. 1, comprising 15 affected individuals over three generations. There was no familial consanguinity. Six affected individuals were examined by clinical neurologists, three of them (cases III-7, III-12, and III-21) by one of us (JG). We, therefore, describe in detail the clinical data of these patients, making a tabular summary of the remaining three patients.
Informed consents from surviving patient III-21 and relatives of deceased patients were obtained for all tests performed, and for publication. The study was in accordance with the Declaration of Helsinki and the local ethics committee.
Clinical studies
Case III-21 [proband] A 65-year-old woman experienced progressively unsteady gait as of age 56, accompanied by dysarthria and episodes of choking; socially inappropriate remarks, emotional lability and irritability were noted later by family members.
On examination, she was alert and oriented. Spontaneous language consisted of short sentences with syntactic errors. Confrontation naming revealed phonemic paraphasia, single-word comprehension and sentence repetition being preserved. Speech was explosive, slow and effortful, with disrupted prosody. Spasticity was found in the hips and knees, Ashworth scale grade 2 [50], together with hyperactive limb and jaw muscle stretch reflexes, and ankle clonus; plantar responses were indifferent. Limb muscle and tongue bulk and strength were normal, without fasciculation. Stance was wide-based, Romberg test was negative, gait was ataxo-spastic requiring occasional support, and tandem gait was impossible. There was final tremor and slight dysmetria in the finger-to-nose and heel-to-shin manoeuvres (see videotapes). Sensation was intact to pinprick, joint position and vibration. Eye movements were full, with no nystagmus, and ocular pursuit was smooth.
Neuropsychological testing performed 7 and 9 years after disease onset, using the Wisconsin Card Sorting Test, Boston Naming Test, Trail Making Tests A and B, Tower of London Test, Semantic Fluency Test (animals), Phonemic Verbal Fluency test, and the Barcelona Test, revealed a progressive decrease of speed in information processing, phonemic verbal fluency, and executive function, with perseveration and rigidity. Phonemic paraphasia was increasingly detected. A slight impairment in episodic memory did not worsen between tests, while attention, orientation to time and place, calculation, insight, and bidimensional constructive praxis were preserved. Globally, these results outlined a frontosubcortical deterioration profile.
Case III-7 A previously healthy woman developed wide-based gait at the age of 70 years, accompanied by hand dysmetria. Muscle stiffness appeared in the legs and later in the arms, together with extremely painful spasms in the limbs and trunk, which abated spontaneously after 5 years. Joint contractures developed, and she became bedridden. Pseudobulbar affect, dysarthria, dysphagia, urinary and fecal incontinence subsequently ensued.
Twelve years after disease onset, progressively hesitant, halting, and scarce spontaneous language appeared, followed by apathy, diminished social interest and memory impairment. The patient died aged 85.
On examination 5 months before death, spontaneous language was limited to very short sentences with syntactic errors; she repeated single words and followed two-step commands. There was a spastic quadriparesis with flexion contractures at the elbows, wrists, hips, and knees; gait and limb coordination could not be tested. Tongue and limb muscle volume was normal, without fasciculation. Limb and jaw tendon reflexes were hyperactive, with ankle clonus, and plantar responses were extensor. Pain and vibration sense was preserved. Eye movements were full on vertical and lateral gaze, no nystagmus was observed, and ocular pursuit was saccadic. Speech was effortful and hypophonic, and snout and grasp reflexes were present.
Case III-12 A 62-year-old man developed hypomimia, bradikynesia and slow gait. On examination, left-sided cogwheel rigidity, slow left hand and foot tapping, and decreased arm sway during gait were noted. Parkinson’s disease was diagnosed and treated with rotigotin and pramipexole, without improvement. Two years later, progressive stiffness in the legs appeared, which spread to the arms, causing frequent and extremely painful spasms in the limbs and trunk (Ashworth scale grade 4, Tardieu scale grade 4, Penn Spasm Frequency Scale grade 3) [25, 52], temporarily relieved by intrathecal baclofen. Dysarthria, dysphagia, and sphincter incontinence ensued, and he became wheelchair-bound 9 years after disease onset. At age 66, a progressively scarce, stuttering, and effortful speech started, followed by apathy, emotional lability, ideas of prejudice, bouts of verbal and physical aggressiveness, and memory loss. Generalized spasticity without muscle atrophy was found on examination at age 69, and muscle strength was grade 4/5 [44]. Mini-Mental State Examination [19] score was 26/30, which fell to 20/30 over 1 year, and he was diagnosed with PLS and FTLD. Death came at age 72.
On neurological examination at age 70, he was bedridden, alert with no spontaneous language, verbal answers limited to short sentences. Extreme spasticity was present in upper and lower limbs. Limb muscle and tongue bulk were normal, without fasciculation. Tendon reflexes were brisk, spontaneous ankle clonus was present, and plantar responses were extensor. Muscle strength was grade 4/5 [44].Stance and gait were impossible. Pain sensation was preserved. Facial hypomimia and fixed stare were observed. Extraocular movements were full and ocular pursuit was saccadic, without nystagmus. Speech was effortful and hypophonic.
Tabular summary of clinical studies
Clinical data of all 6 examined individuals are summarized in Table 1. Age of onset varied from 52 to 70 years (median 60). There were 5 deceased patients at ages ranging between 70 and 85 years (median 75); median disease duration was 15 years (range 10–25). Pyramidal semeiology initiated with spastic gait was the inaugural manifestation, which extended to the upper limbs and lower cranial nerve musculature, gradually causing quadriparesis with painful muscle spasms and pseudobulbar palsy. In no case was fasciculation or muscle atrophy observed. In addition, cases III-7 and III-21 showed clear static and kinetic cerebellar ataxia, and case III-21 exhibited parkinsonism.
In a variable period of the clinical course, all six patients developed an alteration of language, initially consisting of effortful, halting, and dysprosodic speech, with phonemic paraphasia and reduced verbal fluency appearing later. With disease progression, apathy, followed by memory and orientation difficulties, mutism and dementia, appeared in five cases. Cognitive deterioration following a frontosubcortical pattern was detected in case III-21.
Electrophysiological studies
In case III-16, an electromyographic study performed 7 years after disease onset, revealed normal motor unit action potentials and absence of spontaneous activity in the deltoid, triceps brachii, first dorsal interosseous, quadriceps, medial gastrocnemius, and tibialis anterior muscles.
In case III-21, nerve conduction and electromyographic studies performed 6 years after disease onset revealed normal findings; no spontaneous muscle activity was recorded. Sensory evoked potentials were normal.
Imaging studies
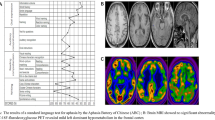
MRI findings in case III-12 showed thinning of the trunk of the corpus callosum, dilation of supratentorial ventricles, and widening of central and frontoparietal sulci. Subcortical hyperintensities were detected in both central regions. Temporal and occipital lobes were normal in appearance (Fig. 2).
MRI study in case III-12. a Cranial MRI axial T2-weighted image showing frontoparietal atrophy and sulcal enlargement, especially of the central sulci (SC). b Coronal T2-FLAIR image shows subtle subcortical hyperintensity underlying the dilated intraparietal sulci (IS), and atrophy of the gyrus parietalis superior (GPS). c Midsagittal T2-weighted image showing atrophy of the trunk of the corpus callosum (CC), and enlargement of the marginal branch of the cingulated (MBCS) and precentral sulci (PS)
In case III-21, MRIs performed 6 and 7 years after disease onset revealed thinning of the corpus callosum, ventricular dilation and progressive dilation of frontoparietal and central sulci; the remaining intracranial structures displayed a normal appearance.
An amyloid positron emission tomography-computerized tomography (PET-CT) with florbetapir did not show abnormal tracer binding.
Neuropathological studies
Autopsy studies were performed on cases III.7 and III.12.
Case III.7 Macroscopically, the brain showed marked atrophy of the frontal lobes due to severely reduced white matter, with atrophy of the corpus callosum and ventricular dilation; the temporal lobes were normal (Fig. 3a).
Autopsy features in Case III-7. a Macroscopic coronal section showing atrophy of the frontal lobes, reduction in the white matter of the centrum semiovale and corpus callosum, enlargement of lateral ventricles and normal temporal lobes. b Microscopic section of the motor cortex (MC) showing preservation of Betz neurons (Klüver-Barrera; bar = 45 µm). c In this transverse section of the lateral pyramidal tract, note marked reduction of axons in the lateral pyramidal tract (anti-neurofilament 200 kDa antibody, clone RT97; bar = 25 µm). d Section of the hippocampus (CA1 region) showing neurons with deposits of hyperphosphorylated tau and grains (Phospho-Tau [Ser202, Thr205] Monoclonal Antibody AT8; bar = 225 µm). Sections processed for immunohistochemistry are slightly counterstained with hematoxylin
Microscopic examination revealed marked reduction of myelin and nerve fibers, as revealed by myelin, myelin basic protein and neurofilament antibody stains. The primary motor cortex showed preservation of Betz neurons and mild astrogliosis (Fig. 3b).
A marked reduction of myelin and nerve fibers was found in the pyramidal tracts of the lumbar spinal cord, the only level available for study (Fig. 3c). Spinal motor neurons were preserved, with a few axonal balloonings in the anterior horn. In addition, abundant 4Rtau pre-tangles and grains, and a few tangles were observed in the hippocampus and entorhinal cortex, accompanied by thorn-shaped astrocytes and abundant oligodendrocytes with tau deposits conforming coiled bodies, in the temporal white matter (Fig. 3d). Abnormal TDP-43, α-synuclein or β-amyloid deposits were not detected.
Case III.12 The primary motor cortex displayed normal neuronal populations (Fig. 4a–c), and so did other regions of the frontal and parietal cortices.
Histological features in Case III-12. a–c Sections of primary motor cortex (MC) stained with hematoxylin and eosin (HE), myelin basic protein (MBP), and glial fibrillary acidic protein (GFAP), showing neuronal preservation and absence of reactive astrocytosis (bar = 45 µm). Transverse sections of the spinal cord at the cervical level showing preservation of the dorsal columns (d) and loss of myelinated fibers in the lateral pyramidal tract (e) (Klüver-Barrera; bar = 45 µm). f, g Note absence of alterations in anterior (ant root) or dorsal roots of the spinal cord (Klüver-Barrera; bar = 100 µm). h–j Neurofibrillary degeneration visualized with AT8 antibody in the entorhinal cortex (EC) and CA1 region of the hippocampus (CA1, bar = 100 µm); section of the cerebellar cortex (bar = 25 µm) showing axonal ballooning, as revealed with anti-phosphorylated neurofilament antibodies (RT97). Sections processed for immunohistochemistry are slightly counterstained with hematoxylin
Degeneration of the lateral and, to a lesser extent, anterior corticospinal fascicles with axon and myelin loss, moderate astrogliosis, and absence of microglial response, macrophages or inflammatory cells, was the main alteration in the spinal cord. Degeneration was much more marked at sacral and lumbar, than at cervical spinal cord and medullary levels (Fig. 5a–d). No neuronal loss or cell body alteration was noted in the anterior horns of the spinal cord, except for a few ballooned axons in the anterior horn in the distal spinal cord and in Clarke’s column (a normal finding with aging in this region, Fig. 5g, h)). Other spinal cord fascicles were not affected; myelin and nerve fibers were preserved in the spinal roots and dorsal tracts (Figs. 4d–g, 5e, f).
Case III-12. Sections of medulla oblongata (a) and spinal cord (b cervical; c lumbar; d sacral) processed for immunohistochemistry with anti-phosphorylated neurofilament antibodies (RT97), showing axonal loss in the crossed pyramidal tract, more intense at sacral than at lumbar, cervical and medullary levels, and very discrete axonal loss in the anterior pyramidal tract (e); conversely, axons in the dorsal column (f) are preserved (bar = 25 µm). g, h Axonal ballooning is seen in the lumbar and sacral anterior horn of the spinal cord and in Clarke’s column (i) (RT97, bar = 45 µm). Sections slightly counterstained with hematoxylin
The cerebellum showed moderate loss of Purkinje cells with occasional torpedoes and empty baskets (Fig. 4j). Moderate neuronal loss was observed in the bulbar olive (greater than corresponding to age), accompanied by moderate astrocytosis but no reactive microglia. No alteration was found in the nucleus of the hypoglossal nerve, motor nucleus of the vagus nerve, oculomotor and pontine nuclei, red nuclei, colliculi or substantia nigra.
Only one section each of the anterior caudate, putamen, and pulvinar nucleus was available for study; no neuronal alterations were seen.
Neurofibrillary tangles (NFT) composed of 4Rtau and 3Rtau were observed in the hippocampus and entorhinal cortex (Fig. 4h, i). Abnormal TDP-43, α-synuclein or β-amyloid deposits were not observed in any region.
To summarize, the neuropathological studies showed: (1) degeneration of the lateral corticospinal tracts, with an axonal dying-back pattern in case III.12; (2) preservation of spinal, brainstem and cortical motor neurons; (3) severe atrophy of the frontal white matter and corpus callosum in case III-7; (4) cerebello-olivary degeneration, mainly affecting Purkinje cells in case III.12; (5) argyrophilic grain disease (AGD) stage III in case III-7; and (6) primary age-related tauopathy (PART) in case III-12.
Genetic testing
In case III-7, an exome panel aimed at PLS (24 genes) did not detect pathogenic variants, or variants of unknown significance (VUS). In addition, microarray-based Comparative Genomic Hybridization (aCGH) 400K was performed to detect deletions in genes involved in PLS, especially TBK1, with negative results.
Finally, massive sequencing of the human genome was carried out to identify genomic variants: (1) single nucleotide (SNV) and insertion–deletion (INDEL) variants included in exonic regions, 3´UTR and 5′UTR regions, and all intron variants described as probably pathogenic or pathogenic in the ClinVar database (v20150330); and (2) copy number variations in exonic, intronic or intergenic regions. No pathogenic variants associated with the object of consultation were identified. However, a low-frequency population VUS was identified in a gene that has compatible signs with the phenotype under study, with which it was not possible to establish an association: p.(Pro656Thr), exon 17, MED25 [NM_030973.3:c.1966C > A], missense variant, carrier in heterozygosis.
In case III-12, MLPA (Multiplex Ligation-dependent Probe Amplification) aimed at the hereditary spastic paraparesis (HSP) genes SPAST, NIPA1 (SPG6), SPG7, REEP1 (SPG31), and ALT1 (SPG3A) was negative. A Next Generation Sequencing (NGS) panel study of 27 genes associated with HSP was also negative.
In Case III-16, MLPA of SPAST, NIPA, SPG7, REEP, and ALT genes was negative.
In Case III-21, an initial molecular study performed with Triplet-repeated Primed Polymerase Chain Reaction (TP-PCR) of autosomal dominant spinocerebellar ataxias (SCA) 1, 2, 3, 6, 7, 8, 10, 12, and 17 and dentatorubral–pallidoluysian atrophy, yielded negative results. Dynamic expansions of the GGGGCC hexamer in intron 1 of C9orf72 were ruled out, as was the presence of large deletions/duplications (MLPA) in the analyzed regions of MAPT and GRN.
An NGS study of the human exome was performed to identify genomic variants in 145 genes associated with ataxia, HSP, and FTLD/exome directed, without finding pathogenic variants or VUS. An extension was made to the clinical exome study by NGS (5713 genes), and the following low-frequency allelic variants (< 1%) and VUS were detected in heterozygosis: (1) c.134C > A (p.Pro45Gln), missense, SPAST (in silico pred 3/8); (2) c.666C > A (p.Tyr222*), nonsense, MMACHC; (3) c.5118C > A (p.Asn1706Lys) exon 40, missense, (4) ITPR1 (in silico pred 2/8); and (5) c.1486C > T (p.Pro496Ser) exon 13, missense, TTBK2 (in silico pred 1/8). Sanger sequencing of these variants was negative in case III-16, variant number 4 being positive only in case III-12.
Discussion
The core clinical features of the kindred under study were spastic spinobulbar paresis without muscle atrophy, and dementia characterized by inaugural speech disturbance. Disease onset was in the sixth decade of life or later, and inheritance was autosomal dominant with complete penetrance.
The motor manifestations exhibited by this family fulfilled the clinical diagnostic criteria of PLS [56]: (1) insidious onset of spastic paresis, beginning in the lower extremities; (2) onset in the fifth decade or later; (3) gradually progressive course (duration ≥ 3 years; (4) clinical findings limited to corticospinal dysfunction; and (5) symmetrical distribution, ultimately developing spastic spinobulbar paresis. Criterion number 3 (absence of family history) was not met.
Juvenile PLS may be sporadic but also inherited in a recessive mode, the causative mutant gene being ALS2 on chromosome 2q33.1, which is also responsible for infantile-onset ascending spastic paralysis and a juvenile form of ALS [25, 46, 51]. Erb claimed that PLS could be hereditary [18], albeit recent examples of adult onset autosomal dominant PLS are limited to a kinship with compound heterozygote mutations in SPG7, and a French–Canadian family, in which a locus was identified on chromosome 4 [15, 69, 73]. Adult onset PLS is not caused by mutations in ALS2 [5], but apparently sporadic cases have been related to mutations in SPG7, SPG11, DCTN1, PARK2, and expansions in C9orf72 [47, 72]. Isolated instances of PLS may occur within FTLD [21] and ALS pedigrees [4, 55, 58], such as those associated with mutations in TBK1 and UBQLN2, respectively [72]. None of the mentioned variants was found in this study.
PLS is rare, comprising about 5% of motor neuron disease [MND] patients presenting at specialized neuromuscular clinics [49]. The controversy about whether PLS is a subtype of ALS or a discrete entity continues to this day [22, 26]: revised El Escorial criteria consider PLS a restricted ALS phenotype [40], while other authors maintain PLS is a distinct syndrome [13].
Our patients had no lower motor neuron signs; in consequence, electrophysiological testing was performed only in cases III-16 and III-21, in which electromyographic studies were, respectively, normal, 7 and 6 years after disease onset.
The manifestations displayed by this kindred fell into the category of PLS-plus (complicated PLS): “predominant upper motor neuron signs plus clinical, laboratory, or pathological evidence of dementia, parkinsonism, or sensory abnormalities”, because “spastic spinobulbar paralysis without muscle atrophy, visible fasciculations or evidence of denervation on electromyography at ≥ 4 years from disease onset” [22, 39, 62], together with dementia or cognitive decline, was present in every case.
Case III-12 associated dopamine agonist therapy-resistant parkinsonism with PLS, as reported in PLS-plus [20, 22, 41, 62]. Although the substantia nigra was normal on pathological examination, assessment of the basal ganglia could not be performed in depth, precluding any potential clinicopathological correlation.
Cerebellar ataxia has not been considered a component of PLS-plus, its presence making it necessary to differentiate PLS-plus from multiple system atrophy [20, 40]. However, cerebellar intention tremor and unsteady gait were reported in a family with MND and dementia [two members expressing PLS], in correlation with loss of Purkinje cells [54]. Patients III-7 and III-21 exhibited inaugural unsteady gait and dysmetria, although no histological abnormalities were present in the cerebellum in the first case. Contrariwise, cerebello-olivary degeneration was found in case III-12, in spite of an absence of ataxic signs. The presence of cerebellar ataxia in this context could be related to factors that modify the expression of the causative gene and induce differing clinical and pathological manifestations, as demonstrated in hereditary ataxia [61].
In spite of preserved bladder function being considered part of PLS [56], urinary incontinence was present in five of our cases and urinary urgency in the other, as reported in PLS [39, 47], the cause being detrusor hyperreflexia and a spastic internal vesical sphincter [59].
PLS is considered to spare intellect, although impairment in executive function, verbal memory, psychomotor speed and verbal fluency (similar to ALS and progressive muscular atrophy) has been identified in up to 49% of patients [8, 12, 53]. In one study, total score on the Addenbrooke’s Cognitive Examination was abnormal in 21 patients with PLS (mean 82.5/100, cutoff value 88), the most prominent deficits being reduced verbal fluency, and deficiencies in memory, language and visuospatial function [1].
PLS is not believed to form part of the FTLD–MND complex; however, this association has been reported before [14, 29]. In one series, 3.3% of PLS cases developed FTLD of the behavioural or semantic variants [12]. Rapid and severe cognitive decline appeared years after progressive UMN signs, with memory impairment never being an early symptom, as observed in this kindred, in which similar time courses of evolution and progression of symptoms, suggest a common pathogenic origin for motor and cognitive symptoms. Amyloid was absent in pathological material [1], as in our neuropathological and florbetapir PET-CT studies, ruling out Alzheimer’s disease as the present illness’ cause.
Every investigated member in this kin suffered from dementia starting up to 12 years after motor symptom onset, except for patient III-21 (who only exhibited frontosubcortical deterioration after 8 years of disease). Early speech (halting, stuttering and effortful speech) and language disturbances (agrammatism, decreased verbal fluency and phonemic paraphasia) preceded apathy, emotional lability, and memory impairment. These manifestations were evaluated against clinical criteria for PPA, and a nonfluent/agrammatic variant was diagnosed [23]. Aggressiveness and delusional ideas occurred in case III-12, and social disinhibition and emotional lability in case III-21; however, clinical diagnostic criteria for behavioural variant FTLD were not met [9, 23].
Nonfluent PPA has been related to potential development of ALS and other motor syndromes [16, 30, 64], as found in this family. It was mentioned in association with PLS in one case, but no clinical description was provided [34]. Deposition of tau protein predominating in the left posterior frontoinsular cortex is the most likely pathological basis [30, 33], although in this study, tau deposition was found in the form of AGD in case III-7, and of PART in case III-12.
AGD is an age-related 4R tauopathy. It may overlap with other neurodegenerative disorders and is second only to Alzheimer’s disease in frequency, although no association with the APOE ε4 genotype has been reported. It is characterized by three main pathological features: argyrophilic grains, oligodendrocytic coiled bodies, and neuronal cytoplasmatic pre-tangles in the medial temporal lobes, as found in case III-7. AGD lacks distinctive clinical features and may manifest as a slowly progressive amnestic syndrome; however, up to 59% of cases with pathologically demonstrated AGD were cognitively normal [31, 57].
PART refers to the presence of age-related 3R and 4R tau-positive NFT in neurons, without extension beyond the temporal neocortex. Whether PART represents early Alzheimer’s disease remains controversial, as the frequency of association with APOE ε4 is low [33, 57]. A diagnosis of PART requires a Braak NFT stage ≤ IV (usually III or lower), and a Thal beta-amyloid phase ≤ 2. PART is classified pathologically as definite or possible, depending on whether beta-amyloid is absent or present, respectively [10, 32]. Clinically, it may be divided into asymptomatic (no cognitive decline or dementia), or symptomatic (cognitive decline or dementia present); [10]; case III-12 can be classified as definite, symptomatic PART.
Definite PART may go either with normal intellect, mild cognitive impairment or dementia, as no precise clinical features have been outlined for it. Depression, increasing Braak stage, and presence of other tau pathologies or neurodegenerative diseases have been associated with definite, symptomatic PART [3].
AGD and PART do not affect the left frontoinsular cortex involved in nonfluent PPA, and have not been previously associated with PLS in the medical literature; therefore, they must be considered incidental findings in the present kindred.
Neuropathological examination of cases with PLS and dementia have revealed corticospinal tract degeneration, preservation of spinal motor neurons and loss of cerebral cortex neurons, which displayed either ubiquitin-positive tau [66], ubiquitin-positive [36, 48], TDP-43 [29, 34, 37], neurofilament-immunoreactive neuronal inclusions [42], dendritic ballooning [65], or diffuse beta-amyloid plaques [17]. Every one of these cases was sporadic, and the data provided were insufficient to define a dementing syndrome characteristic of PLS. None of the aforementioned cortical changes was found in our autopsied cases.
A diagnosis of autopsy-proven PLS in this study was corroborated by degeneration of corticospinal tracts in the spinal cord and bulbar pyramids without neuron loss, gliosis, Bunina bodies, ubiquitin or TDP-43 inclusions, in spinal motor neurons [22]. The more pronounced corticospinal fiber loss at sacral and lumbar, rather than at cervical and medullary levels found in case III-12, supports by pathological means a dying-back pathogenic mechanism, in which central axons degenerate following a distal-to-proximal gradient, as previously proposed for PLS [11, 74]. Moreover, preservation of upper motor neuron cell bodies indicated that a cerebral cortical neuronopathy could not be claimed as causal in cases III-7 and III-12.
Marked loss of myelin and nerve fibers in the frontal and parietal lobes without deposition of abnormal material, was found in case III-7. Taken together, these data suggest that white matter degeneration centered on axonal motor and language networks could be a primary pathologic alteration in this kindred [27, 34, 67].
Central distal axonopathies have been implied as causal mechanisms in HSP, lathyrism, Friedreich’s ataxia, ALS and clioquinol intoxication [38, 68, 74]. A primary central axonopathy that affects language structures has been proposed for progressive nonfluent aphasia on the basis of white matter damage on MRI [60], as found in case III.12.
MRI demonstrated dilation of central sulci in this series [as reported in PLS], enlarged frontoparietal sulci and lateral ventricles, bilateral white matter abnormalities in the corona radiata and atrophy of the corpus callosum; the last two have been associated with PLS and PPA [2, 35, 56, 63]. In addition, impairment in memory, executive and language test scores in PLS, has been found to correlate with white matter tract damage on diffusion-tensor MRI [7, 45].
The main differential diagnosis in this kindred would be FTLD–MND, excluded by absence of lower motor neuron clinical, electromyographic and pathological signs, and a mean survival time of 196.8 months, approximately equivalent to 217 ± 22.4 months in one series [53]. This is in contrast with FTLD–MND, whose mean duration was estimated as 2–3 years [29], and 38.5 ± 4.5 months [28]. SPG4, SPG7, and SPG11 were also considered in the differential diagnosis [6, 69, 71], as well as SCA1 and SCA17 in cases III-7 and III-21, because these exhibited cerebellar ataxia in addition to spasticity and cognitive decline [43, 70]. All these diseases were ruled out by genetic analysis. Furthermore, no potentially pathogenic gene mutations were identified on NGS whole exome sequencing, covering 5.713 genes, and whole genome sequencing.
In summary, a kindred with a hitherto undescribed, dominantly inherited variant of PLS and progressive nonfluent aphasia, in which the corticospinal tracts were affected by a central distal axonopathy, and cortical motor neurons were preserved, is presented. Further molecular studies are needed to identify the causative mutation in this disease, to offer accurate genetic counseling to the family under study.
References
Agarwal S, Highton-Williamson E, Caga J, Matamala JM, Dharmadasa T, Howells J et al (2018) Primary lateral sclerosis and the amyotrophic lateral sclerosis-frontotemporal dementia spectrum. J Neurol 265:1819–1828
Agosta F, Galantucci S, Magnani G, Marcone A, Martinelli D, Antonietta Volontè M et al (2015) MRI signatures of the frontotemporal lobar degeneration continuum. Hum Brain Mapp 36:2602–2614
Besser LM, Crary JF, Mock C, Kukull WA (2017) Comparison of symptomatic and asymptomatic persons with primary age-related tauopathy. Neurology 89:1707–1715
Brugman F, Wokke JH, Vianney de Jong JM, Franssen H, Faber CG, Van den Berg LH (2005) Primary lateral sclerosis as a phenotypic manifestation of familial ALS. Neurology 64:1778–1779
Brugman F, Eymard-Pierre E, van den Berg LH, Wokke JH, Gauthier-Barichard F, Boespflug-Tanguy O (2007) Adult-onset primary lateral sclerosis is not associated with mutations in the ALS2 gene. Neurology 69:702–704
Brugman F, Veldink JH, Franssen H, de Visser M, de Jong JM, Faber CG et al (2009) Differentiation of hereditary spastic paraparesis from primary lateral sclerosis in sporadic adult-onset upper motor neuron syndromes. Arch Neurol 66:509–514
Canu E, Agosta F, Galantucci S, Chiò A, Riva N, Silani V et al (2013) Extramotor damage is associated with cognition in primary lateral sclerosis patients. PLoS One 8:e82017
Caselli RJ, Smith BE, Osborne D (1995) Primary lateral sclerosis: a neuropsychological study. Neurology 45:2005–2009
Chare L, Hodges JR, Leyton CE, McGinley C, Tan RH, Kril JJ et al (2014) New criteria for frontotemporal dementia syndromes: clinical and pathological diagnostic implications. J Neurol Neurosurg Psychiatry 85:865–870
Crary JF, Trojanowski JQ, Schneider JA, Abisambra JF, Abner EL, Alafuzoff I et al (2014) Primary age-related tauopathy (PART): a common pathology associated with human aging. Acta Neuropathol 128:755–766
Deng HX, Zhai H, Fu R, Shi Y, Gorrie GH, Yang Y et al (2007) Distal axonopathy in an alsin-deficient mouse model. Hum Mol Genet 16:2911–2920
de Vries BS, Rustemeijer LMM, van der Kooi AJ, Raaphorst J, Schröder CD, Nijboer TCW et al (2017) A case series of PLS patients with frontotemporal dementia and overview of the literature. Amyotroph Lateral Scler Frontotemporal Degener 18:534–548
de Vries BS, Rustemeijer LMM, Bakker LA, Schröder CD, Veldink JH, van den Berg LH et al (2019) Cognitive and behavioural changes in PLS and PMA: challenging the concept of restricted phenotypes. J Neurol Neurosurg Psychiatry 90:141–147
Doran M, Enevoldson TP, Ghadiali EJ, Larner AJ (2005) Mills syndrome with dementia: broadening the phenotype of FTD/MND. J Neurol 252:846–847
Dupré N, Valdmanis PN, Bouchard JP, Rouleau GA. Autosomal dominant primary lateral sclerosis. Neurology 68:1156–7
Elahi FM, Miller BL (2017) A clinicopathologic approach to the diagnosis of dementia. Nat Rev Neurol 13:457–476
Engel PA, Grunnet M (2000) Atypical dementia and spastic paraplegia in a patient with primary lateral sclerosis and numerous neocortical beta amyloid plaques: new disorder or Alzheimer’s disease variant? J Geriatr Psychiatry Neurol 13:60–64
Erb W (1902) Spastic and syphilitic spinal paralysis. Lancet 2:969–974
Folstein M, Folstein SE, McHugh PR (1975) “Mini-Mental State” a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Gilbert RM, Fahn S, Mitsumoto H, Rowland LP (2010) Parkinsonism and motor neuron diseases: twenty-seven patients with diverse overlap syndromes. Mov Disord 25:1868–1875
Gómez-Tortosa E, Van der Zee J, Ruggiero M, Gijselinck I, Esteban-Pérez J, García-Redondo A et al (2017) Familial primary lateral sclerosis or dementia associated with Arg573Gly TBK1 mutation. J Neurol Neurosurg Psychiatry 88:996–997
Gordon PH, Cheng B, Katz IB, Pinto M, Hays AP, Mitsumoto H, Rowland LP (2006) The natural history of primary lateral sclerosis. Neurology 66:647–653
Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF et al (2011) Classification of primary progressive aphasia and its variants. Neurology 76:1006–1014
Haugh AB, Pandyan AD, Johnson GR (2006) A systematic review of the Tardieu Scale for the measurement of spasticity. Disabil Rehabil 28:899–907
Helal M, Mazaheri N, Shalbafan B, Malamiri RA, Dilaver N, Buchert R et al (2018) Clinical presentation and natural history of infantile-onset ascending spastic paralysis from three families with an ALS2 founder variant. Neurol Sci 39:1917–1925
Hudson AJ, Kiernan JA, Muñoz DG, Pringle CE, Brown WF, Ebers GC (1993) Clinicopathological features of primary lateral sclerosis are different from amyotrophic lateral sclerosis. Brain Res Bull 30:359–364
Iwata NK, Kwan JY, Danielian LE, Butman JA, Tovar-Moll F, Bayat E et al (2011) White matter alterations differ in primary lateral sclerosis and amyotrophic lateral sclerosis. Brain 134:2642–2655
Josephs KA, Knopman DS, Whitwell JL, Boeve BF, Parisi JE, Petersen RC et al (2005) Survival in two variants of tau-negative frontotemporal degeneration: FTLD-U vs. FTLD-MND. Neurology 65:645–647
Josephs KA, Dickson DW (2007) Frontotemporal lobar degeneration with upper motor neuron disease/primary lateral sclerosis. Neurology 69:1800–1801
Josephs KA, Duffy JR (2008) Apraxia of speech and nonfluent aphasia: a new clinical marker for corticobasal degeneration and progressive supranuclear palsy. Curr Opin Neurol 21:688–692
Josephs KA (2017) Current understanding of neurodegenerative diseases associated with the protein tau. Mayo Clin Proc 92:1291–1303
Josephs KA, Murray ME, Tosakulwong N, Whitwell JL, Knopman DS, Machulda MM et al (2017) Tau aggregation influences cognition and hippocampal atrophy in the absence of beta-amyloid: a clinico-imaging-pathological study of primary age-related tauopathy (PART). Acta Neuropathol 133:705–715
Knopman DS, Nestor PJ (2017) Beyond clinical syndromes in primary progressive aphasia. Seeking etiologic diagnoses. Neurology 88:2244–2245
Kobayashi Z, Tsuchiya K, Arai T, Yokota O, Yoshida M, Shimomura Y et al (2010) Clinicopathological characteristics of FTLD-TDP showing corticospinal tract degeneration but lacking lower motor neuron loss. J Neurol Sci 298:70–77
Kolind S, Sharma R, Knight S, Johansen-Berg H, Talbot K, Turner MR (2013) Myelin imaging in amyotrophic and primary lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener 14:562–573
Konagaya M, Sakai M, Matsuoka Y, Konagaya Y, Hashizume Y (1998) Upper motor neuron predominant degeneration with frontal and temporal lobe atrophy. Acta Neuropathol 96:532–536
Kosaka T, Fu YJ, Shiga A, Ishidaira H, Tan CF, Tani T et al (2012) Primary lateral sclerosis: upper-motor-predominant amyotrophic lateral sclerosis with frontotemporal lobar degeneration–immunohistochemical and biochemical analyses of TDP-43. Neuropathology 32:373–384
Lamarche JB, Lemieux B, Lieu HB. The neuropathology of “typical” Friedreich’s ataxia in Quebec (1984). Can J Neurol Sci 11(4 Suppl): 592–600
Le Forestier N, Maisonobe T, Piquard A, Rivaud S, Crevier-Buchman L, Salachas F et al (2001) Does primary lateral sclerosis exist? A study of 20 patients and a review of the literature. Brain 124:1989–1999
Ludolph A, Drory V, Hardiman O, Nakano I, Ravits J, Robberecht W et al (2015) A revision of El escorial criteria. Amyotroph Lateral Scler Frontotemporal Degener 16:291–292
Mabuchi N, Watanabe H, Atsuta N, Hirayama M, Ito H, Fukatsu H et al (2004) Primary lateral sclerosis presenting parkinsonian symptoms without nigrostriatal involvement. J Neurol Neurosurg Psychiatry 75:1768–1771
Mackenzie IR, Feldman H (2004) Neurofilament inclusion body disease with early onset frontotemporal dementia and primary lateral sclerosis. Clin Neuropathol 23:183–193
Matilla-Dueñas A, Goold R, Giunti P (2008) Clinical, molecular, and pathophysiological insights into spinocerebellar ataxia type 1. Cerebellum 7:106–114
Medical Research Council (1976) Aids to the examination of the peripheral nervous system. Her Majesty’s Stationery Office, London
Meoded A, Kwan JY, Peters TL, Huey ED, Danielian LE, Wiggs E et al (2013) Imaging findings associated with cognitive performance in primary lateral sclerosis and amyotrophic lateral sclerosis. Dement Geriatr Cogn Dis Extra 3:233–250
Mintchev N, Zamba-Papanicolaou E, Kleopa KA, Christodoulou K (2009) A novel ALS2 splice-site mutation in a Cypriot juvenile-onset primary lateral sclerosis family. Neurology 72:28–32
Mitsumoto H, Nagy PL, Gennings C, Murphy J, Andrews H, Goetz R et al (2015) Phenotypic and molecular analyses of primary lateral sclerosis. Neurol Genet 1:e3
Mochizuki A, Komatsuzaki Y, Iwamoto H, Shoji S (2004) Frontotemporal dementia with ubiquitinated neuronal inclusions presenting with primary lateral sclerosis and parkinsonism: clinicopathological report of an autopsy case. Acta Neuropathol 107:377–380
Murphy MJ, Grace GM, Tartaglia MC, Orange JB, Chen X, Rowe A et al (2008) Cerebral haemodynamic changes accompanying cognitive impairment in primary lateral sclerosis. Amyotroph Lateral Scler 9:359–368
Pandyan AD, Johnson GR, Price CI, Curless RH, Barnes MP, Rodgers H (1999) A review of the properties and limitations of the Ashworth and modified Ashworth Scales as measures of spasticity. Clin Rehabil 13:373–383
Panzeri C, De Palma C, Martinuzzi A, Daga A, De Polo G, Bresolin N et al (2006) The first ALS2 missense mutation associated with JPLS reveals new aspects of alsin biological function. Brain 129:1710–1719
Penn RD, Savoy SM, Corcos D, Latash M, Gottlieb G, Parke B et al (1989) Intrathecal baclofen for severe spinal spasticity. N Engl J Med 320:1517–1521
Piquard A, Le Forestier N, Baudoin-Madec V, Delgadillo D, Salachas F, Pradat PF et al (2006) Neuropsychological changes in patients with primary lateral sclerosis. Amyotroph Lat Scler 7:150–160
Polvikoski TM, Murray A, Harper PS, Neal JW (2003) Familial motor neuron disease with dementia: phenotypic variation and cerebellar pathology. J Neurol Neurosurg Psichiatry 74:1516–1520
Praline J, Guennoc AM, Vourc’h P, De Toffol B, Corcia P (2010) Primary lateral sclerosis may occur within familial amyotrophic lateral sclerosis pedigrees. Amyotroph Lat Scler 11:154–156
Pringle CE, Hudson AJ, Muñoz DG, Kiernan JA, Brown WF, Ebers GC (1992) Primary lateral sclerosis. Clinical features, neuropathology and diagnostic criteria. Brain 115:495–520
Rodriguez RD, Suemoto CK, Molina M, Nascimento CF, Leite RE, de Lucena Ferretti-Rebustini RE, et al (2016) Argyrophilic grain disease: demographics, clinical, and neuropathological features from a large autopsy study. J Neuropathol Exp Neurol 75:628–635
Rosen DR, Siddique T, Patterson D, Figlewicz DA, Sapp P, Hentati A et al (1993) Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature 362:59–62
Russo LS (1982) Clinical and electrophysiological studies in primary lateral sclerosis. Arch Neurol 39:662–664
Schwindt GC, Graham NL, Rochon E, Tang-Wai DF, Lobaugh NJ, Chow TW et al (2013) Whole-brain white matter disruption in semantic and nonfluent variants of primary progressive aphasia. Hum Brain Mapp 34:973–984
Schut JW, Haymaker W (1951) Hereditary ataxia. A pathologic study of five cases of common ancestry. J Neuropathol Clin Neurol 1:183–213
Singer MA, Statland JM, Wolfe GI, Barohn RJ (2007) Primary lateral sclerosis. Muscle Nerve 35:291–302
Smith CD (2002) Serial findings in a case of primary lateral sclerosis. Neurology 57:647–649
Strong MJ, Abrahams S, Goldstein LH, Woolley S, Mclaughlin P, Snowden J et al (2017) Amyotrophic lateral sclerosis—frontotemporal spectrum disorder (ALS-FTSD): revised diagnostic criteria. Amyotroph Lateral Scler Frontotemporal Degener 18:153–174
Sugihara H, Horiuchi M, Kamo T, Fujisawa K, Abe M, Sakiyama T et al (1999) A case of primary lateral sclerosis taking a prolonged clinical course with dementia and having an unusual dendritic ballooning. Neuropathology 19:77–84
Tan CF, Kakita A, Piao YS, Kikugawa K, Endo K, Tanaka M et al (2003) Primary lateral sclerosis: a rare upper-motor-predominant form of amyotrophic lateral sclerosis often accompanied by frontotemporal lobar degeneration with ubiquitinated neuronal inclusions? Report of an autopsy case and a review of the literature. Acta Neuropathol 105:615–620
Tartaglia MC, Laluz V, Rowe A, Findlater K, Lee DH, Kennedy K et al (2009) Brain atrophy in primary lateral sclerosis. Neurology 72:1236–1241
Thomas PK, Schaumburg HH, Spencer PS, Kaeser HE, Pallis CA, Rose FC et al (1984) Central distal axonopathy syndromes: newly recognized models of naturally occurring human degenerative disease. Ann Neurol 15:313–315
Valdmanis PN, Dupré N, Rouleau GA (2008) A locus for primary lateral sclerosis on chromosome 4ptel-4p16.1. Arch Neurol 65:383–386
Van Gaalen J, Giunti P, van de Warrenburg BP (2011) Movement disorders in spinocerebellar ataxias. Mov Disord 26:792–800
Vázquez-Costa JF, Bataller L, Vílchez JJ (2016) Primary lateral sclerosis and hereditary spastic paraplegia in sporadic patients. An important distinction in descriptive studies. Ann Neurol 80:169–170
Yamashita S, Ando Y (2015) Genotype-phenotype relationship in hereditary amyotrophic lateral sclerosis. Transl Neurodegener 3:13
Yang Y, Zhang L, Lynch DR, Lukas T, Ahmeti K, Sleiman PM et al (2016) Compound heterozygote mutations in SPG7 in a family with adult-onset primary lateral sclerosis. Neurol Genet 2:e60
Zhai P, Pagan F, Statland J, Butman JA, Floeter MK (2003) Primary lateral sclerosis. A heterogeneous disorder composed of different subtypes? Neurology 60:1258–1265
Acknowledgements
Our thanks to Dr. Antonio Oliveros-Juste for remission of patients; Drs. Ana Vela and Jordi Aldomá for MR images; Mr. Juan Ramón Solans, Drs. Ariadna Fernández-Sanz and Jesús Aladrén-Sangrós for help with the videtapes; Mrs. María Jesús Chopo for obtention of DNA samples; Mrs. Teresa Sopeña Biarge and Mrs. Mar González-Cantalejo from the Medical Library of Hospital Universitario Miguel Servet, for bibliographical research; and Dr. Jorge Alfaro for assistance in the pathological studies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical standards
All human studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MP4 15897 KB)
Supplementary material 2 (MP4 34972 KB)
Rights and permissions
About this article
Cite this article
Gazulla, J., Ferrer, I., Izquierdo-Alvarez, S. et al. Hereditary primary lateral sclerosis and progressive nonfluent aphasia. J Neurol 266, 1079–1090 (2019). https://doi.org/10.1007/s00415-019-09235-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09235-x