Abstract
Introduction
Combining patient-specific instrumentation (PSI) with a balancer device in total knee arthroplasty (TKA) to achieve functional femoral rotational alignment is a novel technique. The primary goal of this study was to introduce a new method to combine PSI with a gap-balancing technique and to determine the impact of the technique on rotation of the femoral component.
Materials and methods
Twenty-five primary TKAs (15 women, 10 men) were prospectively studied. All TKAs involved PSI with an associated gap-balancing device. Front plane alignment was performed intraoperatively with the PSI, followed by rectangular, symmetrical extension and creation of a flexion gap using the balancer device to set the femoral rotation.
Results
Femoral component rotation was between 3° internal and 6° external rotation versus the transepicondylar axis. There were no postoperative signs of patellofemoral dysfunction. In no cases was the resulting joint line displacement >3 mm. The mean elevation was 1.2 ± 0.9 mm (range 0–3). The leg axis was straight in all cases (±3°), at a mean of 1.6° ± 1.0° varus (range 0°–3° varus).
Conclusions
PSI was with the gap-balancing technique was successfully used without affecting anatomical alignment. With the balancer device, PSI can be used more widely than techniques based solely on landmarks, as the soft-tissue tension can be taken into account, thus virtually eliminating flexion instabilities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rotation of the femoral components in total knee arthroplasty (TKA) affects flexion stability and tibiofemoral and patellofemoral kinematics [1–3]. The potential consequences include: an asymmetrical flexion gap [4, 5]; contractures [6]; persistent instability, particularly in flexion with lift-off [7–9]; unilateral wear of the polyethylene inlay [10]; postoperative pain [11]; and early implant failure [5, 12–14].
The optimum femoral rotation has not been consistently described in the literature. The rotational alignment of the femoral component [4, 15] is either anatomical (measured-resection technique) or references the soft tissue (gap-balancing technique). The gold standard for the measured-resection technique, which has hitherto been used with patient-specific instrumentation (PSI), is the femoral component alignment parallel to the transepicondylar axis, or 0°–3° from the posterior condylar line [16–19]. Rotational adjustment deviations of up to 6° are, however, not an uncommon feature when using the gap-balancing technique [20], and a symmetrical flexion gap is crucial to its success [18, 19]. Comparable clinical results are reported with both techniques [21–23].
A key criticism of the gap-balancing technique is that component alignment is based on the proximal tibial cut and there is thus a risk that initial alignment errors will be carried through to all subsequent cuts [24, 25]. With the development of PSI, anatomically referenced cutting blocks can be produced preoperatively based on MRI or CT data, which improve alignment [17, 26–29]. All currently used PSI systems are, however, bone-referenced, and it is therefore not possible to take functional parameters into account. In some cases, planned workups have had to be stopped [30–33]. Studies have shown that PSI deviated from the surgical plan in up to 50 % of cases, partially because femoral rotation could not be controlled and it was not possible to achieve a rectangular flexion gap with symmetrical tissue tension [30–32].
PSI with the gap-balancing technique is currently being explored, although the impact on rotational alignment of the femoral component is unclear. For the current study, it was hypothesized that, when used correctly, kinematic femoral alignment in combination with PSI leads to deviation from anatomical alignment, while it adequately restores stability, range of motion, joint line, as well as alignment of the leg axis.
Materials and methods
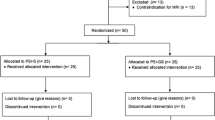
In a prospective study, 25 primary TKAs (15 women, 10 men) were performed with PSI (Visionaire, Smith & Nephew Inc., Memphis, TN) and an associated gap-balancing device (Visionaire; Fig. 1). The study was approved by the local ethics committee (S1(a)/2013). Patients scheduled to undergo resurfacing for primary or secondary gonarthrosis and who had provided their written consent were enrolled. Patients aged under 18 years at the time of surgery, those with rheumatoid arthritis or post-traumatic arthrosis, and those who did not give their consent were excluded. The average age of the study population was 67.6 ± 6.7 years. The preoperative leg axis was between 18° varus and 15° valgus.
Preoperatively, all patients underwent MRI (Optima MR 360 1.5 T, GE Health Care, Little Chalfont, UK) and long-standing (lower extremity) radiographs. The production of the PSI, as well as the patient-customized cutting blocks for the femur and tibia, were then planned. The objective was to achieve a neutral mechanical axis for the femur and tibia, 4° flexion in the sagittal plane for the femoral component, a 3° posterior slope for the tibial component and a femoral rotation ±2° parallel to the surgical transepicondylar axis. Planning was reviewed and confirmed by the surgeon in each case. Age, gender, weight, body mass index, American Society of Anesthesiologists classification (physical status classification) and the planned femoral rotation based on the transepicondylar axis were all recorded preoperatively.
All patients underwent a medial parapetallar approach and were implanted with a cemented Journey BCS Posterior Stabilized TKA (Smith & Nephew Inc., Memphis, TN) by the first author. The proximal tibial and the distal femoral cuts were first carried out using the PSI. Soft-tissue balancing was performed by first setting the extension gap with the balancer device and, where appropriate, gradually releasing the ligament to achieve a symmetrical extension gap [34–36]. The balancer device was used to distract the femur from the proximal tibia. Following each release step with the balancer device, the extension gap was measured until a symmetrical extension gap was achieved. The values established for the extension gap tension were subsequently applied to the flexion gap. The rotation of the femur was adjusted based on the soft-tissue tension to achieve a rectangular flexion gap (Fig. 2). The pinholes for the 5-in-1 block were drilled over the balancer device. Next, the final bone cuts were made and implant placement was performed as instructed by the manufacturer. The patella was not replaced in any of the cases, nor was lateral release required to correct patellar tracking.
Clinical examinations were carried out 3 months postoperatively to assess stability (extension and mid-flexion), patellofemoral pain and joint range of motion. Mid-flexion instability was defined as 30°–45° of flexion [37]. Radiological follow-up examinations were performed using a CT (Philips Brilliance CT 6 No. 44639207). Femoral rotation and joint line displacement were assessed. Femorotibial joint line height restoration was determined radiographically using the ratio of the adductor tubercle to joint line distance and the femoral width [38].
The mechanical leg axis (hip–knee angle (HKA) [39]) was measured on a long-standing (lower extremity) radiograph. Radiographs were taken in neutral rotation of the leg. The X-ray beam was centered between the two knees. Mechanical axis of the lower limb was measured using digital radiographs and special software (PACS, Carestream Health, Rochester, US). All postoperative measurements were performed by an independent physician.
Patient data were analysed descriptively. The mean and standard deviation were used to analyze continuous variables, while numbers and percentages were used for group variables. Outliers in the displacement of the joint line (>5 mm) [40] and the alignment of the leg axis (>3°) [41] were defined. Data were analyzed using Stata 12.1 (Stata Corporation, College Station, TX).
Results
Demographic data are provided in Table 1. In all cases, the TKA was implanted with PSI, and the balancer device was used for gap balancing, as planned. Additionally, all knees received the pre-planned insert and femoral size. In two cases, a tibial component one size smaller than planned was used. There were no intraoperative complications. In four TKAs, a first-degree soft-tissue release was carried out in extension. The time required to balance the flexion and extension gap averaged 2 min.
On follow-up examination, ligament stability was achieved in extension and in mid-flexion (gapping <2 mm) in all knee joints. Patellofemoral pain was not reported. Mean flexion improved from 99.2° ± 8.4° preoperatively to 108.4° ± 9.4° at 12 weeks.
Six (24 %) femoral components were aligned into internal rotation (1°–3°) with gap-balancing. Femoral rotation was as planned in three (12 %) cases, while, in the remaining 16 (64 %) cases external rotation resulted (1°–5°; Fig. 3). The rotation of the femoral components was between 3° internal rotation and 6° external rotation (Fig. 3).
The average joint line displacement was 1.2 ± 0.9 mm (range 0–3) proximal. No outliers >5 mm were recorded. The mean leg axis was 1.6° ± 1.0° varus (range 0°–3° varus) versus the neutral mechanical axis. No outliers with >3° deviation were recorded (Table 2).
Discussion
In the current study, rotational values of the femoral components using the gap-balancing technique were within the range considered typical for this technique (3° internal rotation to 6° external rotation versus the transepicondylar axis) [18], but deviated from anatomical alignment. Using the balancer device meant that it was possible to take the individual tissue conditions into account while using PSI. Proper leg axis alignment was achieved in all cases. The joint line was only marginally raised in the study population.
The use of PSI allowed alignment of the tibial component in this study, with no deviations >1.5° compared to planning. Similar accuracy of primary bone cuts has been described for PSI by other authors [17, 26–28, 42]. Reliable use of the gap-balancing technique with a sufficiently accurate tibial cut is therefore ensured. Femoral rotation is more accurate if it has already been balanced in extension, and avoids secondary rotational malalignment of the femoral component due to a varus or valgus malalignment of the tibial component [43, 44]. Raising the joint line by up to 5 mm is then possible without having a detrimental effect [40, 45–47]. In our study, there was no relevant displacement of the joint line >3 mm, at 3 mm in two cases, 2 mm in five cases, and <2 mm in the remaining 18 knees. Restoration or preservation of the natural joint line, considered to be a key factor in successful TKA, was thus achieved [40, 46, 48].
Elevation of the joint line affects the patellofemoral joint specifically by increasing contact forces and thereby contributing to pain, instability, wear and impaired function [40, 47]. The literature reports femoropatellar complication rates of 2–7 % following primary TKA [4, 49, 50]. Functional impairment and an increased risk of revision are also reported [46]. Postoperative clinical effects or complications, such as mid-flexion instability, patellofemoral pain syndrome, or contractures, due to raising the joint line were not observed in the study cohort.
It was possible to carry out the surgical technique in all cases without complications. In the event of rotations >6°, the literature advises that lateral ligament instability should be assessed. Any further rotation of the femoral component may lead to suboptimal patellar tracking with anterior knee pain, kinematic restrictions, crepitation, overexertion and excessive wear of the polyethylene surfaces [19, 34, 51]. With the exception of two tibial components that were downsized following the removal of exophytes, the planned implants were used in all cases. There were no other deviations from the surgical plan described in the literature, nor were there any requirements to abandon the planned workups because a balanced gap was not achieved, as has been reported elsewhere in the literature [30–32].
A right-angled flexion gap with symmetrical ligament tension was achieved in all cases. The postoperative leg axis was 1.6° varus on average (range 0°–3° varus). A neutral [13] or slightly varus [52] leg axis of 0° to 1°–2° varus are considered to be ideal, whereas deviations of >3° are considered a risk factor for implant failure [13, 53].
Limitations of the current study include the lack of a control group, the relatively short follow-up period, and the small, heterogeneous, study population. Moreover, an a priori power analysis was not conducted. Consequently, our findings should be interpreted with caution.
In conclusion, the gap-balancing technique was successfully applied in combination with PSI in 25 knees. The balancer device takes into account individual soft-tissue tension, and can be used in PSI by surgeons who prefer the gap-balancing technique. However, only prospective comparative long-term studies can determine whether this technique is well-suited for TKA.
References
Merican AM, Ghosh KM, Iranpour F, Deehan DJ, Amis AA (2011) The effect of femoral component rotation on the kinematics of the tibiofemoral and patellofemoral joints after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19(9):1479–1487
Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, Nakamura T (1999) Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 366:155–163
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Hube R, Mayr HO, Kalteis T, Matziolis G (2011) Extension first technique for TKA implantation. Oper Orthop Traumatol 23(3):241–248
Walde TA, Bussert J, Sehmisch S, Balcarek P, Sturmer KM, Walde HJ, Frosch KH (2010) Optimized functional femoral rotation in navigated total knee arthroplasty considering ligament tension. Knee 17(6):381–386
Lustig S, Scholes CJ, Stegeman TJ, Oussedik S, Coolican MR, Parker DA (2012) Sagittal placement of the femoral component in total knee arthroplasty predicts knee flexion contracture at one-year follow-up. Int Orthop 36(9):1835–1839
Scuderi GR, Komistek RD, Dennis DA, Insall JN (2003) The impact of femoral component rotational alignment on condylar lift-off. Clin Orthop Relat Res 410:148–154
Daines BK, Dennis DA (2014) Gap balancing vs. measured resection technique in total knee arthroplasty. Clin Orthop Surg 6(1):1–8
Dennis DA, Komistek RD, Kim RH, Sharma A (2010) Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res 468(1):102–107
Fehring TK (2000) Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res 380:72–79
Czurda T, Fennema P, Baumgartner M, Ritschl P (2010) The association between component malalignment and post-operative pain following navigation-assisted total knee arthroplasty: results of a cohort/nested case-control study. Knee Surg Sports Traumatol Arthrosc 18(7):863–869
Hoffart HE, Langenstein E, Vasak N (2012) A prospective study comparing the functional outcome of computer-assisted and conventional total knee replacement. J Bone Joint Surg Br 94(2):194–199
Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA (2011) The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am 93(17):1588–1596
Matziolis G, Pfiel S, Wassilew G, Boenicke H, Perka C (2011) Kinematic analysis of the flexion axis for correct femoral component placement. Knee Surg Sports Traumatol Arthrosc 19(9):1504–1509
Heesterbeek PJ, Jacobs WC, Wymenga AB (2009) Effects of the balanced gap technique on femoral component rotation in TKA. Clin Orthop Relat Res 467(4):1015–1022
Parratte S, Blanc G, Boussemart T, Ollivier M, Le Corroller T, Argenson JN (2013) Rotation in total knee arthroplasty: no difference between patient-specific and conventional instrumentation. Knee Surg Sports Traumatol Arthrosc 21(10):2213–2219
Heyse TJ, Tibesku CO (2014) Improved femoral component rotation in TKA using patient-specific instrumentation. Knee 21(1):268–271
Matziolis G, Boenicke H, Pfiel S, Wassilew G, Perka C (2011) The gap technique does not rotate the femur parallel to the epicondylar axis. Arch Orthop Trauma Surg 131(2):163–166
Rienmuller A, Guggi T, Gruber G, Preiss S, Drobny T (2012) The effect of femoral component rotation on the five-year outcome of cemented mobile bearing total knee arthroplasty. Int Orthop 36(10):2067–2072
Schnurr C, Nessler J, Konig DP (2009) Is referencing the posterior condyles sufficient to achieve a rectangular flexion gap in total knee arthroplasty? Int Orthop 33(6):1561–1565
Becker R, Malzdorf M, Starke C, Randolf P, Lohmann C (2012) No difference between tibia-first and femur-first techniques in TKA using computer-assisted surgery. Knee Surg Sports Traumatol Arthrosc 20(10):2011–2016
Matsumoto T, Muratsu H, Kawakami Y, Takayama K, Ishida K, Matsushita T, Akisue T, Nishida K, Kuroda R, Kurosaka M (2014) Soft-tissue balancing in total knee arthroplasty: cruciate-retaining versus posterior-stabilised, and measured-resection versus gap technique. Int Orthop 38(3):531–537
Singh VK, Varkey R, Trehan R, Kamat Y, Raghavan R, Adhikari A (2012) Functional outcome after computer-assisted total knee arthroplasty using measured resection versus gap balancing techniques: a randomised controlled study. J Orthop Surg (Hong Kong) 20(3):344–347
Insall JN, Binazzi R, Soudry M, Mestriner LA (1985) Total knee arthroplasty. Clin Orthop Relat Res 192:13–22
Insall J, Ranawat CS, Scott WN, Walker P (1976) Total condylar knee replacement: preliminary report. Clin Orthop Relat Res 120:149–154
Daniilidis K, Tibesku CO (2013) Frontal plane alignment after total knee arthroplasty using patient-specific instruments. Int Orthop 37(1):45–50
Daniilidis K, Tibesku CO (2014) A comparison of conventional and patient-specific instruments in total knee arthroplasty. Int Orthop 38(3):503–508
Boonen B, Schotanus MG, Kort NP (2012) Preliminary experience with the patient-specific templating total knee arthroplasty. Acta Orthop 83(4):387–393
Heyse TJ, Tibesku CO (2015) Improved tibial component rotation in TKA using patient-specific instrumentation. Arch Orthop Trauma Surg 135(5):697–701
Victor J, Dujardin J, Vandenneucker H, Arnout N, Bellemans J (2014) Patient-specific guides do not improve accuracy in total knee arthroplasty: a prospective randomized controlled trial. Clin Orthop Relat Res 472(1):263–271
Scholes C, Sahni V, Lustig S, Parker DA, Coolican MR (2014) Patient-specific instrumentation for total knee arthroplasty does not match the pre-operative plan as assessed by intra-operative computer-assisted navigation. Knee Surg Sports Traumatol Arthrosc 22(3):660–665
Roh YW, Kim TW, Lee S, Seong SC, Lee MC (2013) Is TKA using patient-specific instruments comparable to conventional TKA? A randomized controlled study of one system. Clin Orthop Relat Res 471(12):3988–3995
Woolson ST, Harris AH, Wagner DW, Giori NJ (2014) Component alignment during total knee arthroplasty with use of standard or custom instrumentation: a randomized clinical trial using computed tomography for postoperative alignment measurement. J Bone Joint Surg Am 96(5):366–372
Whiteside LA (2004) Ligament balancing. Weichteilmanagement in der Knieendoprothetik. Springer, Berlin
Mihalko WM, Saleh KJ, Krackow KA, Whiteside LA (2009) Soft-tissue balancing during total knee arthroplasty in the varus knee. J Am Acad Orthop Surg 17(12):766–774
Whiteside LA (2002) Soft tissue balancing: the knee. J Arthroplasty 17(4 Suppl 1):23–27
Del Gaizo DJ, Della Valle CJ (2011) Instability in primary total knee arthroplasty. Orthopedics 34(9):e519–e521
Iacono F, Raspugli GF, Bruni D, Filardo G, Zaffagnini S, Luetzow WF, Lo Presti M, Akkawi I, Marcheggiani Muccioli GM, Marcacci M (2014) The adductor tubercle as an important landmark to determine the joint line level in total knee arthroplasty: from radiographs to surgical theatre. Knee Surg Sports Traumatol Arthrosc 22(12):3034–3038
Cooke TD, Li J, Scudamore RA (1994) Radiographic assessment of bony contributions to knee deformity. Orthop Clin North Am 25(3):387–393
Konig C, Sharenkov A, Matziolis G, Taylor WR, Perka C, Duda GN, Heller MO (2010) Joint line elevation in revision TKA leads to increased patellofemoral contact forces. J Orthop Res 28(1):1–5
Ritter MA, Faris PM, Keating EM, Meding JB (1994) Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res 299:153–156
Ng VY, DeClaire JH, Berend KR, Gulick BC, Lombardi AV Jr (2012) Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res 470(1):99–107
Pfitzner T, Rohner E, Preininger B, Perka C, Matziolis G (2012) Femur positioning in navigated total knee arthroplasty. Orthopedics 35(10 Suppl):45–49
Pang HN, Yeo SJ, Chong HC, Chin PL, Ong J, Lo NN (2011) Computer-assisted gap balancing technique improves outcome in total knee arthroplasty, compared with conventional measured resection technique. Knee Surg Sports Traumatol Arthrosc 19(9):1496–1503
Bellemans J (2004) Restoring the joint line in revision TKA: does it matter? Knee 11(1):3–5
Figgie HE 3rd, Goldberg VM, Heiple KG, Moller HS 3rd, Gordon NH (1986) The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Joint Surg Am 68(7):1035–1040
Babazadeh S, Dowsey MM, Stoney JD, Choong PF (2014) Gap balancing sacrifices joint-line maintenance to improve gap symmetry: a randomized controlled trial comparing gap balancing and measured resection. J Arthroplasty 29(5):950–954
Wyss TF, Schuster AJ, Munger P, Pfluger D, Wehrli U (2006) Does total knee joint replacement with the soft tissue balancing surgical technique maintain the natural joint line? Arch Orthop Trauma Surg 126(7):480–486
Peralta-Molero JV, Gladnick BP, Lee YY, Ferrer AV, Lyman S, Gonzalez Della Valle A (2014) Patellofemoral crepitation and clunk following modern, fixed-bearing total knee arthroplasty. J Arthroplasty 29(3):535–540
Springorum HR, Rath B, Baier C, Lechler P, Luring C, Grifka J (2011) Patellofemoral pain after total knee arthroplasty: clinical pathway and review of the literature. Orthopade 40(10):907–911, 914–916
Pongcharoen B, Yakampor T, Charoencholvanish K (2013) Patellar tracking and anterior knee pain are similar after medial parapatellar and midvastus approaches in minimally invasive TKA. Clin Orthop Relat Res 471(5):1654–1660
Matziolis G, Adam J, Perka C (2010) Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg 130(12):1487–1491
Barke S, Musanhu E, Busch C, Stafford G, Field R (2013) Patient-matched total knee arthroplasty: does it offer any clinical advantages? Acta Orthop Belg 79(3):307–311
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Preparation of this manuscript was supported by Smith & Nephew GmbH, Marl, Germany. Smith & Nephew had no involvement in the collection, analysis or interpretation of the data, in the writing of the report or in the decision to submit the results for publication.
Rights and permissions
About this article
Cite this article
Hommel, H., Perka, C. Gap-balancing technique combined with patient-specific instrumentation in TKA. Arch Orthop Trauma Surg 135, 1603–1608 (2015). https://doi.org/10.1007/s00402-015-2315-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2315-6