Abstract
Purpose
The purpose of our study was to compare the accuracy of the rotational position of the femoral component in total knee arthroplasty aligned with patient individualized jigs (PSJ) to a gap balancing technique (GBT).
Methods
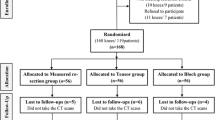
A consecutive series of 21 osteoarthritic patients were treated with 22 cruciate-retaining total knee prostheses. During surgery, the rotation of the femoral component pinholes was recorded for all knees using PSJ and GBT and transferred to computer tomograms (CT). The rotational differences between PSJ and GBT relative to the transepicondylar axis were analysed.
Results
The medium rotation of the femoral component pinholes was 1.3° ± 5.1° (min = −6.3°; max = 14.4°) for PSJ and 0.1 ± 1.4° (min = −1.6°; max = 3.4°) for GBT. Outliers of more than 3° were found more frequently with PSJ in 12 cases but only in one for GBT.
Conclusion
Based on our study, we would not recommend relying intra-operatively solely on the CT-based PSJ without the option to adjust or control femoral rotation.
Level of evidence
II.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary total knee arthroplasty (TKA) is one of the most successful orthopaedic procedures with reported 15-year implant survival beyond 90 % in cruciate-retaining TKA [1]. However, substantial numbers of patients are dissatisfied with their knee function and have painful or stiff knees [4]. Early revisions for pain, stiffness, instability and limited range of motion are increasingly common [6–8, 19, 25], and rotational alignment of the femoral component is crucial [2, 3, 8, 11, 31]. Currently, femoral rotation is determined intra-operatively relying on either anatomic landmarks, the transepicondylar axis (TEA) [16, 23, 27, 29], a fixed external rotation of 3° from the posterior condylar axis (PCA), or the anteroposterior trochlear axis [2, 3, 13]. Another option is the so-called gap balancing technique (GBT) described by John Insall in 1981 [17], where the posterior condyles are distracted in 90° flexion from the tibial cutting surface and the femoral component is rotated until medial and lateral flexion gaps are equal. It is clear from the literature that anatomic landmarks result in a highly variable femoral rotational prosthetic placement with the potential of its associated clinical complications [21, 32]. The GBT has the least variability and lowest amount of surgical outliers [13, 30, 36], and it has been shown that the restoration of the medial posterior condylar geometry results in improved knee kinematics [15].
Recent advancements of surgical techniques propose a pre-operative computer tomogram (CT) for improved femoral rotation of total knee implants. Using Berger’s et al. method [8], the CT-based transepicondylar axis (CTTEA) is determined on a pre-op CT scan, and the relative angle to the PCA is measured. This angle is used to determine femoral component rotation using the PCA and the measured angle on CT. Victor et al. and Michaut et al. [22, 33] have shown a high reliability of this technique, where 77 % of the components are placed within 2° of the actual CT-measured rotation. They felt that a pre-op CT scan is a more favourable method compared to techniques based on traditional intra-operative anatomic landmarks.
The aim of this study was to investigate whether the restoration of the posterior medial condyle in combination with a GBT, where less lateral posterior condyle is resected in order to place the femoral component in external rotation, would match the CT-based pre-operative CTTEA and PCA as described by Victor et al. [33] and Michaut et al. [22]. We further wanted to know how closely a CT-based patient-specific jig (PSJ), (Trumatch, Depuy, Warsaw, IN, USA) would place the femoral component relative to the CT-based pre-operative CTTEA and PCA. No study to our knowledge has so far evaluated the accuracy of femoral component rotation comparing GBT with PSJ in relation to CTTEA and PCA. This had a high clinical relevance for our routine, since the patient-specific jigs had no option to intra-operatively adjust or control femoral rotation.
The hypothesis was that there is no difference in the rotational position between GBT and PSJ. We asked specifically (1) how many degrees is our medial posterior condylar resection and GBT deviant from the CTTEA. (2) How many degrees is the PSJ rotational position deviant from the CTTEA and (3) how many degrees is the CTTEA deviant from the intra-operative surgical transepicondylar axis (STEA) and the PCA.
Materials and methods
In 2011, 25 consecutive knee arthroplasties had pre-operative CT scans, which were used to manufacture PSJ. PSJ were planned and manufactured using CTTEA. Three patients cancelled due to medical issues, and one patient delayed surgery and the jigs expired, which left a total of 22 knee arthroplasties for 21 osteoarthritic patients in our study. The average age of the patients was 67 ± 16 years. Ten women and 11 men were treated. All operations were performed without complications. Mean implant size was 3 (2.5–5) for the femur and 3 (2–4) for the tibia. All patients had a tissue-sparing trivector approach [14], receiving a cruciate-retaining knee implant, PFC® Sigma®, CR-TKA (DePuy Orthopedics Inc., Warsaw, IN, USA). All prostheses were implanted by the same surgeon (WF) using a surgical technique as described earlier [15] (Figs. 1, 2): the posterior medial condylar resection was equal to the implant thickness of 8 mm, and using a GBT, the lateral flexion gap was balanced with a slightly thicker spacer block for the looser lateral side (Fig. 1) which resulted in less posterior lateral condylar resection (Fig. 2). This ensured a femoral external rotation as described earlier [15]. Using this technique, the pivot point of the femoral rotation is changed: instead of rotating the femur through the centre of the femoral canal, the pivot point is on the surface of the posterior medial condyle in about 90° of flexion (Fig. 3).
In situ the lateral flexion gap is tensioned with a slightly thicker spacer block (most of the time 3 mm thicker than medial) and the femoral sizer (Brigham balancer) is constructed to resect implant thickness of the medial posterior condyle, but less than the implant thickness of the lateral posterior condyle resulting in a balanced flexion gap
Posterior medial condylar measured resection and gap balancing technique (GBT): this GBT resects the implant thickness of the posterior medial condyle and less than the implant thickness of the posterior lateral condyle. The lateral flexion gap is looser and is balanced with a thicker spacer block (most of the time 3 mm thicker compared to the medial flexion spacer block) resulting in femoral component external rotation
Patella resurfacing was performed in all procedures by subluxing the patella, and no medial or lateral releases were needed in any of the cases. The osteophytes at the medial and lateral tibial plateau and at the notch near the posterior cruciate ligament were aggressively removed. Intra-operatively the STEA was marked on the distal resected femur using the sulcus between the double peaks of the medial epicondyle and the lateral epicondyle. Using a posterior medial measured resection and lateral GBT, first these pinholes were drilled with a 2.6-mm drill. Secondly, the pinholes using the PSJ (TruMatch®, Depuy, Warsaw, IN, USA) were drilled (Fig. 4a′, b′). Twice each, two observers measured the distances to the STEA using a millimetre-scaled vernier calliper. Then, the distances to the PCA were measured after removing residual cartilage medially and laterally (Fig. 4c, d) to compute the relative position to the PCA. The measurements were done leaving the pins in place and subtracting half of the pin diameter to get the distance to the pinhole centre and increase accuracy to one decimal. This allowed us to bridge the intra-operative measurement to our pre-operative CT and its real femoral geometry [34]. Victor et al. demonstrated low intra- and inter-observer variability in the CT registration of PCA and CTTEA [34] using this technique. Intra-observer and inter-observer variability of the CT measurements in our study showed a correlation coefficient of 0.969 (p < 0.001) and 0.943 (p < 0.001), respectively.
Intra-operative pinhole marking and measurements, a position anterior to the surgical transepicondylar axis (STEA) was defined as positive distance a position dorsal as negative: a, b distance from STEA to the cutting blocks fixation pinholes with medial measured resection gap balancing technique (GBT). a′, b′ distance from STEA to the patient-specific cutting jigs fixation pinholes; c, d amount of bony resections medially and laterally from the posterior condylar axis
The angle between the connecting line of the pinholes for both techniques and the intra-operative STEA was calculated using the trigonometric tangent. The tangent of the angle was the ratio of the length of the opposite side, in our case the vertical distance of the pinholes in mm to the length of the adjacent side, in our case the horizontal distance between the cutting blocks fixation holes. The angle between the intra-operative STEA and CT-based CTTEA as well as the measured rotation of the PSJ and medial measured resection GBT were compared as described by Victor et al. [34] (Fig. 5). Deviation of more than 3° from the target in any plane was defined as an outlier.
IRB approval was obtained at the Brigham and Women’s Hospital in Boston, USA, with the Protocol No.: 2012P000882.
Statistical analysis: Data were presented descriptively as arithmetic mean, standard deviation and minimum and maximum of the evaluated values. We randomly excluded one limb of the patient with bilateral knees in the analysis to minimize the impact of bilateral knees. Statistical analysis was performed in several steps. First, a sample size calculation was done using the sixteen s-squared over d-squared estimation, a literature-based population standard deviation of 2.9° and a difference to be detected of 3° [20, 22]. This resulted in a minimum sample size of 15. The normal distribution of data was confirmed using Kolmogorov–Smirnov test. The effect of the implanting techniques was examined with a two-sample t test for the equality of means and with F test for equality of variances. The grade of agreement between the two methods variability was evaluated with the Bland–Altman plot. Intra-observer and inter-observer agreement were assessed by calculating Pearson’s correlation coefficient. All tests were two-sided, and a p value of 0.05 was considered significant. Statistical analyses were performed with PASW Statistics 18 (version 18.0.0, IBM Corporation, Chicago, IL, USA).
Results
There were no statistically significant differences for the average rotational component alignment relative to the STEA, but GBT showed more precise results with smaller variances (p = 0.01). The rotation was 0.1° ± 1.4° (−1.6° IR to 3.4° ER) for GBT and 1.3° ± 5.1° (−6.3° IR to 14.4° ER) for PSJ-based technique. The probability to get a rotational difference greater than ±3° was only 3.1 % for GBT but 58.7 % for the second technique using PSJ.
Medial posterior condylar resection and GBT
We saw a constant posterior condylar resection of 7.3 mm (5–10 ± 1.2 mm). The resection off the posterior lateral condyle was 4.1 mm (6–1 ± 1.3 mm). No posterior lateral condylar resection was larger than the used component thickness of 8 mm. The number of outliers with more than 3° is shown in Table 1. The mean difference of the rotational alignment in relation to the optimal value of 0° for the medial posterior condylar resection and GBT was 0.1° with 95 % limits of agreement between −2.9° and 2.6° in the Bland–Altman plots. This technique reflected the CT-based rotation very closely: mean rotation was 0.1° off (3.4° to −1.6° ± 1.4°). Ninety-five percentages were within 2°, and only one case was 3.4° ER (5 %).
Patient individualized jigs (PSJ)
The distribution was relatively uniform (Fig. 6). The number of outliers with more than 3° is shown in Table 1. The mean difference of the rotational alignment in relation to the optimal value of 0° was 0.9° for PSJ with 95 % limits of agreement between −11.8° and 10.1° in the Bland–Altman plots. The femoral rotation in our PSJ group compared to CT-based CTTEA had a mean rotation of 0.9° (14.4° to −8.8° ± 5.5°).
Intra-operative STEA and PCA
The CT-based CTTEA matched the surgical STEA. It was slightly internally rotated −0.4° ± 2.7°. However, the range was from −5.4° of IR to 4.4° ER. The average rotation of PCA relative to the STEA was −3.7° internal rotation (range −6.2° IR to 1.0° ER). The number of outliers with more than 3° can be found in Table 1.
Discussion
The most important finding of the present study was that the medial posterior condylar resection and gap balancing technique matched the CT-based CTTEA very closely, whereas patient-specific jigs showed an obviously greater variance. Patient-specific jigs have been recently added to the surgical armamentarium to improve implant alignment, decrease blood loss and reduce surgical time. Most studies looked at coronal implant alignment but not at femoral rotation [5, 24, 26]. The actual femoral rotation of two different surgical techniques was compared using pre-operative CT scans and bridging the intra-operative measurements using the PCA without the cartilage as described and validated by Michaut et al. [22] and Victor et al. [33]. More authors confirm that this is the most reliable method and even recommend the pre-op CT with this technique to place the femoral component [22, 35] as routine for each case. Michaut et al. showed that 77 % of all components are rotated within 2° of the CT-based CTTEA. We can confirm their findings. Restoration of the posterior medial condyle and rotating the femoral component by resecting less of the posterior lateral condyle resulted in no implant internal rotation of more than 1.6°. In fact, 20 of 21 patients had a rotation matching the CT-based CTTEA within 2° (95 %). Six of 21 patients (29 %) did not match the CT-based CTTEA within 3°. The PSJ did not reproduce the same results: 12 of 21 (57 %) implants would have been either internally rotated or externally rotated of more than 3°. Instead of reducing the anatomic variability, patient individualized jigs showed surprisingly a more than threefold greater variance of 1.3° ± 5.1° in our comparison.
An answer to the question why the patient individualized jigs were so imprecise could not be found by our investigation. We had no issues with clearing of the anterior soft tissues on the femur or seating of the PSJ blocks. The best known algorithm to detect the epicondylar axis on CT scans, Berger’s technique, relies on the lateral epicondylar prominence and the medial sulcus of the medial epicondyle [8]. The posterior condylar angle, measured as the angle between the posterior condylar surfaces and the epicondylar axis, was 3.5° (± 1.2°) in Berger’s work which is similar to our results. A small change in this technique using the most prominent point on the medial epicondyle instead of the medial sulcus for the definition of the epicondylar axis resulted in an angle (condylar twist angle) of 4.7° (± 3.5°) [9]. We can only hypothesize that the computer algorithms or technician plans used for the production of patient individualized jigs were not able to define the medial sulcus of the medial epicondyle precisely enough and therefore added variability. Literature showed a need for significant changes in the technician plan to get an accurate pre-operative plan of patient-specific pin guides [28].
The following limitations of the study need to be discussed. They include a relatively small sample size and a single-surgeon experience. We have randomly excluded one limb of the patient with bilateral knees in the analysis to minimize its impact of bilateral knees which did not change statistical significance [10]. Another limitation was the intra-operative measurement procedure with pinhole marks and a millimetre-scaled calliper. Because of this, our values had to be rounded up or down to the next one-tenth millimetre. Even if this was done separately for each knee by two investigators with a small intra-observer and inter-observer variability, it remains a source of inaccuracy. The PCA and the bony resections from this line were used to transfer the intra-operative measurements on CT scans. These measurements were done with the same calliper and share the same limitations. All residual cartilage was cautiously removed to refer all measurements, operative and CT based, to the same subchondral line, which is the most accurate methodology to transfer CT-based information to intra-operative findings [34]. Another shortcoming of this study is that this is not a randomized controlled trial comparing the techniques based on pre-op and post-op CT scans. However, in our academic institution, we would not get IRB approval for an additional post-operative CT scan related to the additional radiation exposure. The design of this study comparing two techniques to the pre-operative CT-based CTTEA is its strength: the anatomic variability is the same for both techniques.
Despite these limitations and to the best of our knowledge, this study was the first that compared rotational alignment of patient individualized jigs and cutting blocks to conventional instruments restoring the posterior medial condyle GBT and moving the pivot point for femoral rotation from the centre of the intramedullary canal to the surface of the posterior medial condyle in 90° of flexion (Fig. 3). Recently, a more anatomic reconstruction of the posterior condyles using a kinematic alignment technique showed in a randomized controlled trial after a minimum of two years better pain relief, better function and range of movement compared to a traditional measured resection technique [12]. While the kinematic alignment technique did not show improvement in knee kinematics [18], we were able to demonstrate improved lateral rollback and tibial internal rotation using this restoring the posterior medial condyle GBT compared to a traditional GBT [15].
Conclusion
In clinical routine, care should be taken when relying on individualized jigs without the possibility to adjust intra-operatively for femoral rotation. Our study was able to show, as others, that anatomic landmarks during surgery are not as reliable as the CT-based CTTEA. The restoration of the posterior medial condyle GBT matched the CT-based CTTEA very closely. Further research is needed to use routine pre-operative CT for femoral rotation planning, but our technique moving the pivot point for femoral rotation from the intramedullary canal to the surface of the posterior condyle in 90° flexion may have the potential to improve femoral rotation without the use of pre-operative CT scans.
References
Abdel MP, Morrey ME, Jensen MR, Morrey BF (2011) Increased long-term survival of posterior cruciate-retaining versus posterior cruciate-stabilizing total knee replacements. J Bone Joint Surg Am 93(22):2072–2078
Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT (1993) The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res 287:170–177
Arima J, Whiteside LA, McCarthy DS, White SE (1995) Femoral rotational alignment, based on the anteroposterior axis, in total knee arthroplasty in a valgus knee. A technical note. J Bone Joint Surg Am 77(9):1331–1334
Baker PN, van der Meulen JH, Lewsey J, Gregg PJ (2007) The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J Bone Joint Surg Br 89(7):893–900
Bali K, Walker P, Bruce W (2012) Custom-fit total knee arthroplasty: our initial experience in 32 knees. J Arthroplasty 27(6):1149–1154
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 392:46–55
Bedard M, Vince KG, Redfern J, Collen SR (2011) Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res 469(8):2346–2355
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Bryant D, Havey TC, Roberts R, Guyatt G (2006) How many patients? How many limbs? Analysis of patients or limbs in the orthopaedic literature: a systematic review. J Bone Joint Surg Am 88(1):41–45
Churchill DL, Incavo SJ, Johnson CC, Beynnon BD (1998) The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res 356:111–118
Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG (2012) Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics 35(2):e160–e169
Feinstein WK, Noble PC, Kamaric E, Tullos HS (1996) Anatomic alignment of the patellar groove. Clin Orthop Relat Res 331:64–73
Fisher DA, Trimble SM, Breedlove K (1998) The medial trivector approach in total knee arthroplasty. Orthopedics 21(1):53–56
Fitz W, Sodha S, Reichmann W, Minas T (2012) Does a modified gap-balancing technique result in medial-pivot knee kinematics in cruciate-retaining total knee arthroplasty? A pilot study. Clin Orthop Relat Res 470(1):91–98
Griffin FM, Insall JN, Scuderi GR (2000) Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty 15(8):970–973
Hood RW, Vanni M, Insall JN (1981) The correction of knee alignment in 225 consecutive total condylar knee replacements. Clin Orthop Relat Res 160:94–105
Howell SM, Kuznik K, Hull ML, Siston RA (2008) Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics 31(9):857–863
Incavo SJ, Wild JJ, Coughlin KM, Beynnon BD (2007) Early revision for component malrotation in total knee arthroplasty. Clin Orthop Relat Res 458:131–136
Lehr R (1992) Sixteen S-squared over D-squared: a relation for crude sample size estimates. Stat Med 11(8):1099–1102
Mahfouz MR, ElHak Abdel Fatah E, Bowers L, Scuderi G (2015) A new method for calculating femoral anterior cortex point location and its effect on component sizing and placement. Clin Orthop Relat Res 473(1):126–132
Michaut M, Beaufils P, Galaud B, Abadie P, Boisrenoult P, Fallet L (2008) Rotational alignment of femoral component with computed-assisted surgery (CAS) during total knee arthroplasty. Rev Chir Orthop Reparatrice Appar Mot 94(6):580–584
Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE (2001) Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res 392:38–45
Nam D, Maher PA, Rebolledo BJ, Nawabi DH, McLawhorn AS, Pearle AD (2013) Patient specific cutting guides versus an imageless, computer-assisted surgery system in total knee arthroplasty. Knee 20(4):263–267
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br 92(9):1238–1244
Nunley RM, Ellison BS, Zhu J, Ruh EL, Howell SM, Barrack RL (2012) Do patient-specific guides improve coronal alignment in total knee arthroplasty? Clin Orthop Relat Res 470(3):895–902
Olcott CW, Scott RD (1999) The Ranawat Award. Femoral component rotation during total knee arthroplasty. Clin Orthop Relat Res 367:39–42
Pietsch M, Djahani O, Hochegger M, Plattner F, Hofmann S (2013) Patient-specific total knee arthroplasty: the importance of planning by the surgeon. Knee Surg Sports Traumatol Arthrosc 21(10):2220–2226
Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE (1996) Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res 331:35–46
Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ (2005) The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am 87(10):2276–2280
Stiehl JB, Cherveny PM (1996) Femoral rotational alignment using the tibial shaft axis in total knee arthroplasty. Clin Orthop Relat Res 331:47–55
Thienpont E, Schwab PE, Paternostre F, Koch P (2014) Rotational alignment of the distal femur: anthropometric measurements with CT-based patient-specific instruments planning show high variability of the posterior condylar angle. Knee Surg Sports Traumatol Arthrosc 22(12):2995–3002
Victor J (2009) Rotational alignment of the distal femur: a literature review. Orthop Traumatol Surg Res 95(5):365–372
Victor J, Van Doninck D, Labey L, Innocenti B, Parizel PM, Bellemans J (2009) How precise can bony landmarks be determined on a CT scan of the knee? Knee 16(5):358–365
Victor J, Van Doninck D, Labey L, Van Glabbeek F, Parizel P, Bellemans J (2009) A common reference frame for describing rotation of the distal femur: a ct-based kinematic study using cadavers. J Bone Joint Surg Br 91(5):683–690
Yau WP, Chiu KY, Tang WM (2007) How precise is the determination of rotational alignment of the femoral prosthesis in total knee arthroplasty: an in vivo study. J Arthroplasty 22(7):1042–1048
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fitz, W., Jäger, S., Rieger, J.S. et al. Femoral rotation in total knee arthroplasty: a comparison of patient individualized jigs with gap balancing in relation to anatomic landmarks. Knee Surg Sports Traumatol Arthrosc 25, 1712–1719 (2017). https://doi.org/10.1007/s00167-015-3836-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3836-9