Abstract
Introduction
Optimal positioning of the patellar component is crucial for the success of a total knee arthroplasty (TKA). Usually, the patellar component is placed empirically over the presumed centre of the patellar cut. Medialization of the prosthetic patella has been recommended; however, no evidence-based guidelines have been reported.
Material and method
This anatomical study aims to quantify a pre-defined optimal location for positioning of the patellar component with regard to the centre of the patellar cut. Intra-operative measurements of the patellar cut of a series of 129 TKA were conducted in order to measure the distance between the optimal centre of prosthetic patella (OCPP) and the centre of the patellar cut, and that over the vertical (proximal-distal) axis and the horizontal axis (medial-lateral).
Results
Our results demonstrated that, (a) a significant morphological difference of the patellar cut exists between men and women (P < 0.0001), and (b) with reference to centre of the patellar cut, the OCPP lies superiorly and medially in 89%, inferiorly and medially in 9.4%, laterally and superiorly in 1.6%, and in no case laterally and inferiorly. No anterior pain, dislocation episode or patellar revision has been encountered during a follow-up of 4.5 years.
Conclusions
The placement of the patellar component during TKA differs from one patella to another. Thus, by defining the OCPP on a patient-by-patient basis, the surgeon should be able to reproduce the functional anatomy of the native patella.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In total knee arthroplasty, one of the main source of post-operative complications is the patella, with or without resurfacing [1]. Primary patellar resurfacing has been shown to yield significantly better clinical results than secondary patellar resurfacing in painful non-surfaced TKA [2]. Complications in relation to the patellar resurfacing such as anterior knee pain, maltracking, subluxation or dislocation, are usually due to the anatomy of the patient knee, the surgical technique or/and to the design of the patellar and/or trochlear component [3]. In addition to the above cited complications, a suboptimal surgical technique may cause an abnormal wear leading ultimately to the loosening of the polyethylene patellar component. Another technical issue which has been less researched is the positioning of the patellar component. Medialization of the patellar component relative to the centre of the patellar cut has been reported as beneficial [4, 5], while others discussed potential issues related to such medialization [6,7,8]. The few published papers recommending medialization reported vague and intuitive conclusions on the extent of such medialization. In addition, the placement of the patellar component in relation to the vertical axis of the patellar cut has been even less investigated. Two studies recommended a distal placement [8, 9] but again, empirically and with no clear guidelines.
To our knowledge, only one study acknowledged the anatomic prosthetic component positioning. Hofmann et al. [4] reported placing the centre of the patellar button over a point on the patellar cut projected from the highest point of the patellar sagittal ridge. The authors rightly stated that in order to reproduce proper knee kinematics, anatomy reproduced on the patellar side would also be reproduced on the trochlear side. However, the patellar button was either placed centrally or medially to the drilled hole with no description of the medialization calculus of the latter. More, the vertical location of the optimal centre with regard to the centre of the patellar cut was not conducted.
Wiberg’s [10] classification was helpful to understand not only the shape of the patellar facets but the high variability of the vertical ridge location as well [11]. Our hypothesis is based on the fact that the centre of the articular patellar surface moves with the location of the ridge. Therefore, the optimal centre of the prosthetic patella should be located in the same ridge plane to be as faithful as possible to the joint anatomy.
The aim of this study was to identify an optimal centre for the prosthetic patella and to relate it to patient gender in order to help surgeons position the patellar button in TKA. The surgical anatomy of the patellar cut has been revisited in order to (a) investigate gender size differences of the patellar cut, (b) define an optimal centre for the prosthetic patella, and (c) locate this optimal centre in relation to the centre of the patellar cut.
Material and methods
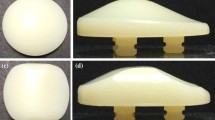
This is a cohort case series study that was conducted on 129 knees from 117 patients that underwent a total knee replacement surgery between 2010 and 2013 by the same surgeon. The indication for TKA was advanced osteoarthritis (OA) of the knee with primary OA in 90% and secondary OA (rheumatoid arthritis) in 10%. The institutional board of our institution approved the study and patient consent has been obtained in all cases prior to surgery. The primary outcome was to define the optimal centre for patellar positioning. Secondary outcomes were the clinical results in relation to the femoro-patellar joint. The same brand of total knee prosthesis was used: scarifying LCP with a rotating platform and a patellar dome-shaped component having three pegs for fixation. Rotation was controlled by the Whiteside line and 2° of external rotation for the femoral component while the tibial component was placed parallel to the posterior edge of the tibial plateau.
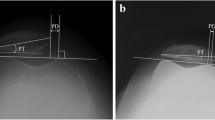
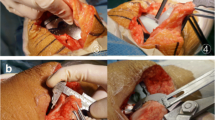
In order to reproduce the anatomical function of the patellar component, we chose the midline of the vertical ridge of the patellar cartilage as the optimal point for patellar positioning. A midline incision was the systematic approach in all patients followed by a medial parapatellar arthrotomy and a lateral dislocation of the patella. Lateral release was performed in none of the cases. The tibial and femoral cut were prepared first. The posterior aspect of the patella and the vertical ridge were then identified. A vertical line was drawn along the vertical ridge and measured. The midpoint of the vertical ridge was identified as the OCPP. A tunnel was perpendicularly drilled through the OCPP using a 1.2-mm drill bit to the anterior cortex of the patella without breaching it. The patellar cut was then done parallel to the anterior surface of the patella leaving usually a patellar bone thickness of 15 mm. The cartilage was removed and the pre-drilled hole identified. A cross was drawn with a marker pen on the patellar cut intersecting the horizontal and vertical axes where L1 and H1 represent the height and width of the patellar cut, respectively. The center of the patellar cut was defined as the intersecting point of L1 and H1. The location of the OCPP to the centre of the patellar cut was then quantified via two measurements; one on the horizontal axis (medial-lateral distance) and another on the vertical axis (proximal-distal distance) (Figs. 1, 2, 3, 4, 5).
The medial (L2), lateral (L3), inferior (H2), and superior (H3) lengths were measured and distances between the OCPP and the centre of the patellar cut were calculated in the horizontal plane [DL] and in the vertical plane [DH] (see figures). All values were reported in mm. The patellar button was then centred over the OCPP; the largest possible patellar component was used as long as it was centred over the OCPP without any overhanging medially and superiorly. The TKA procedure was then continued.
Statistical analysis
StatsDirect (Altrincham, UK) software served for statistical analysis. Student’s t test was used to look for gender difference of the height and width of the patellar cut. Simple linear regression and correlation test was used to correlate the optimal centre to the centre of the patellar cut.
Results
The sample of 117 patients consisted of 26 males and 91 females with a mean age of 72 ± 12.
Using the unpaired Student’s t test, results yielded the following: basic measurements of patellar height and width were significantly higher in men; P < 0.0001 for L1, L2, L3, H1 and H2, while P = 0.001 for H3. While no significance was found for medial displacement values between men and woman (P = 0.1), the distal location of the OPCC in relation to the centre of the patellar cut was significantly higher in men (P = 0.003). Mean (SD) values of patellar height and width along with the mean (SD) values of the difference between the OCPP and the presumed anatomical center are given in Table 1.
The OCPP points were plotted on a scatter-plot graph with reference point being the centre of the patellar cut (0,0) (Fig. 6). In 97.67% (126/129) of the patients, the OCPP was found to be medial to the centre of the patellar cut while in 91.47% (118/129) of the patients it was proximal to it. The correlation plot revealed the following: 89% of the patients’ OCPP were medial and superior, 9.4% were medial and inferior, 1.6% were lateral and superior, and 0% were lateral and inferior to the centre of the patellar cut.
On the last follow-up (mean = 4.5 years), there were no reports of anterior pain or patellar snapping, maltracking or subluxation. No episodes of dislocation were noted by the patients and no TKA revision has been planned or performed for any patellar problem.
Discussion
Our findings can be summarized as follows: (a) there is a significant gender difference in the size of the patellar cut, and (b) the pre-defined optimal centre could be located in three areas with regard to the centre of the patellar cut: superiorly and medially in 89%, inferiorly and medially in 9.4%, laterally and superiorly in 1.6%.
The patella functions to increase the lever arm of the extensor mechanism making knee flexion more effective [12]. It articulates with trochlear groove via its vertical ridge that divides the patella into medial and lateral facets [12]. This study described an attempt to recreate the centre of the patella-femoral joint based on the variability of the position of the cartilage ridge as reported by the original Wiberg’s classification [10]. The implication of Wiberg’s classification is crucial; when the morphology of the patella changes, so does the position of the vertical articular ridge. This means that every patellar type has a different centre point, an important parameter during patellar component positioning when preforming a TKA. Furthermore, the significant size difference of the patellar cut found between males and females should incite manufacturers to take that difference into account when designing patellar components.
Since the patellar ridge constitutes the vertical axis of the patella-femoral joint, we chose the midline of this axis as the reference in positioning the centre of the native patella in order to be as faithful as possible to the factual anatomy of patello-femoral joint. Thus, the vertical axis and centre of the patellar button would be lying in the same plane of the vertical crest of the native patella. In doing so, the centre of the prosthetic patella would be located depending on the patellar morphology via an anatomical patient-based positioning. Instead of proposing a single solution for all patients, an individualized approach for an optimal location would be offered as an alternative. It is of importance to note that choosing the midline axis of the patellar cartilage as the reference has no impact on patellar height; thus, the modified Caton-Deschamps index, which was developed to measure patellar height before/after TKA, would not be affected [19]. The simplicity of the method would likely infer high repeatability and reproducibility. Further prospective studies evaluating intra- and inter-observer reliability are already planned.
Though a resurfaced patella has been linked to a lesser cumulative percent of TKA revision over five years [20], revisions related to the femoro-patellar joint were estimated at 1.8% and post-operative anterior knee pain at 11.1% for the same year range [21]. While loosening [22] and patella-femoral instability [23] are found to be rare complications, patellar component malpositioning may give rise to patellar maltracking that causes tilting or subluxation and, to a lesser degree, a dislocation [1]. Proper positioning of the patellar component is advocated in order to decrease the risk of maltracking post-operatively [1]. Medialization of the patellar component is considered by many as beneficial [4, 5] with less need for lateral retinacular release, and significant decrease in shear forces component [5]. On the other hand, an excessive medialization may cause a higher tendency for lateral tilting of the patella relative to the femur [7, 8, 24] and an increased contact pressure over the medial prosthetic facet [8]. However, while many authors advocate medialization of the patellar component and that for all patients (Table 2), their approach was often empirical such as not exceeding 2.5 mm [6] or lacking quantification such as recommending a button placement on the medial two thirds of the patella [5]. Our results do not support such recommendations; 1.6% of the studied population needed a lateralization, and for the remaining patients, medialization ranged from 0.85 mm to 4.51 mm. The results of this study are not in line with those found by Hofmann et al. [4] who reported an optimal centre being medial to the centre of the patellar cut in every case. Additionally, the location range from the centre of the patellar cut was much wider at 0.54 to 11.6 mm.
Placement of the patellar component in relation to the vertical axis of the patellar cut has been even less investigated. Two studies concluded that a distal placement of the patellar component should lead to decreased loading at higher knee flexion angles [8, 9]. Our results rather suggest a more proximal placement of the prosthetic patella in 90.6% of the cases with only 9.4% having their native centre located more distally.
During the follow-up period, no clinical dysfunction or anterior pain was encountered in all patients. Such promising results incited the authors to continue using this method in patella resurfacing. Further investigations over longer periods of time would better elucidate the clinical outcome of the resurfaced patellar joint and TKA revision rate. The lack of radiological analysis might constitute a potential limitation; however, the absence of post-operative symptoms, signs and episodes of instability are excellent indicators when assessing the femoro-patellar joint. In addition, we did not classify patellar tracking preoperatively because the purpose of our study was to locate the centre of the patellar button depending on the individual anatomical centre of the native patella. In case of patellar mal-tracking, other procedures such as a lateral retinacular release or adequate positioning of the femoral implant could be performed to adjust patellar tracking.
Though we have used the same brand for all cases, and the same medial approach, we believe that the described new method for patellar positioning would be suitable for any brand and for other approaches like the Keblish lateral approach. For instance, it has been demonstrated that no influence of prosthesis type, whether a cruciate-ligament-retaining TKA or a cruciate-ligament-substituting TKA, was found on patellar kinematics [25]. In fact, since the method is focused only over the optimal positioning of the prosthetic patella in relation to the patellar cartilage shape, the component shape (e.g. the dome) or whether the component is embedded or not, are not to be considered as possible factors which could affect the rationale or the suitability of the method in locating the optimal centre.
In conclusion, taking into account the patellar morphology and vertical axis, we were able to reproduce the position of the anatomical patellar centre and to quantify its horizontal and vertical distances to the centre of the patellar cut. Hence, a patient-based approach relative to the native patellar morphology is proposed as an alternative to empirical patellar positioning.
References
Gasparini G, Familiari F, Ranuccio F (2013) Patellar malalignment treatment in total knee arthroplasty. Joints 1(1):10–17
Leta TH, Lygre SH, Skredderstuen A, Hallan G, Gjertsen JE, Rokne B, Furnes O (2016) Secondary patella resurfacing in painful non-resurfaced total knee arthroplasties: a study of survival and clinical outcome from the Norwegian arthroplasty register (1994-2011). Int Orthop 40:715–722
Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, Myers L (2001) Patellar resurfacing in total knee arthroplasty. A prospective, randomized, double-blind study with five to seven years of follow-up. J Bone Joint Surg Am 83-A(9):1376–1381
Hofmann AA, Tkach TK, Evanich CJ, Camargo MP, Zhang Y (1997) Patellar component medialization in Total knee arthroplasty. J Arthroplast 12(2):155–160
Lewonowski K, Dorr LD, McPherson EJ, Huber G, Wan Z (1997) Medialization of the patella in Total knee arthroplasty. J Arthroplast 12(2):161–167
Anglin C, Brimacombe JM, Wilson DR, Masri BA, Greidanus NV, Tonetti J, Hodgson AJ (2010) Biomechanical consequences of patellar component medialization in Total knee arthroplasty. J Arthroplast 25(5):793–802
Doerr TE, Eckhoff DG (1995) Lateral patellar burnishing in Total knee arthroplasty following medialization of the patellar button. J Arthroplast 10(4):540–542
Lee TQ, Budoff JE, Glaser FE (1999) Patellar component positioning in Total knee arthroplasty. Clin Orthop Relat Res 366:274–281
Reithmeier E, Plitz W (1990) A theoretical and numerical approach to optimal positioning of the patellar surface replacement in a total knee endoprosthesis. J Biomech 23(9):883–892
Wiberg G (1941) Roentgenographs and anatomic studies on the femoropatellar joint: with special reference to chondromalacia patellae. Acta Orthop Scand 12.1(4):319–410
Tecklenburg K, Dejour D, Hoser C, Fink C (2006) Bony and cartilaginous anatomy of the patellofemoral joint. Knee Surg Sports Traumatol Arthrosc 14(3):235–240
Fox AJ, Wanivenhaus F, Rodeo SA (2012) The basic science of the patella: structure, composition, and function. J Knee Surg 25(2):127–142
Yoshi I, Whiteside LA, Anouchi YS (1992) The effect of patellar button placement and femoral component design on patellar tracking in total knee arthroplasty. Clin Orthop 275:211–219
Lewonowski K, Dorr LD, McPherson EJ, Huber G, Wan Z (1997) Medialization of the patella in total knee arthroplasty. J Arthroplast 12(2):161–167
Lee TQ, Budoff JE, Glaser FE (1999) Patellar component positioning in total knee arthroplasty. Clin Orthop Relat Res 366:274–281
Kawano T, Miura H, Nagamine R, Urabe K, Matsuda S, Mawatari T, Moro-Oka T, Iwamoto Y (2002) Factors affecting patellar tracking after total knee arthroplasty. J Arthroplasty 17:942–947
McPherson EJ (2006) Patellar tracking in primary total knee arthroplasty. Instr Course Lect 55:439–448
Anglin C, Brimacombe JM, Wilson DR, Masri BA, Greidanus NV, Tonetti J, Hodgson AJ (2010) Biomechanical consequences of patellar component medialization in total knee arthroplasty. J Arthroplast 25:793–802
Caton JH, Prudhon JL, Aslanian T, Verdier R (2016) Patellar height assessment in total knee arthroplasty: a new method. Int Orthop 40:2527–2531
Clements WJ, Miller L, Whitehouse SL, Graves SE, Ryan P, Crawford RW (2010) Early outcomes of patella resurfacing in total knee arthroplasty. Acta Orthop 81:108–113
Li S, Chen Y, Su W, Zhao J, He S, Luo X (2011) Systematic review of patellar resurfacing in total knee arthroplasty. Int Orthop 35:305–316
Witvoet J (1994) Etat Actuel des Prostheses Femoropatellaires. In Chasiers d’enseignement de la Sofcot. Expansion Sci Francaise 46:79–92
Nedopil AJ, Howell SM, Hull ML (2017) What clinical characteristics and radiographic parameters are associated with patellofemoral instability after kinematically aligned total knee arthroplasty? Int Orthop 41:283–291
Nelissen RG, Weidenheim L, Mikhail WE (1995) The influence of the position of the patellar component on tracking in Total knee arthroplasty. Int Orthop 19(4):224–228
Keshmiri A, Maderbacher G, Benditz A, Müller W, Grifka J, Craiovan B (2016) No difference in patellar kinematics between fixed-bearing cruciate-retaining and cruciate-substituting total knee arthroplasty: a cadaveric investigation. Int Orthop 40:731–735
Yoshi I, Whiteside LA, Anouchi YS (1992) The effect of patellar button placement and femoral component design on patellar tracking in total knee arthroplasty. Clin Orthop 275:211-219
Tsutomu K, Hiromasa M, Ryuji Nagamine, Ken U, Shuichi M, Taro M, Takaaki M, Yukihide I, (2002) Factors affecting patellar tracking after total knee arthroplasty. J Arthroplasty 17 (7):942-947
McPherson EJ (2006) Patellar tracking in primary total knee arthroplasty. Instr Course Lect 55:439-48
Anglin C, Brimacombe JM, Wilson DR, Masri BA, Greidanus NV, Tonetti J, Hodgson AJ (2010) Biomechanical Consequences of Patellar Component Medialization in Total Knee Arthroplasty. J Arthroplasty 25 (5):793-802
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Funding
There is no funding source.
Ethical approval
The study was approved by the ethical board of our institution.
Informed consent
An informed consent was obtained from each participant included in the study.
Rights and permissions
About this article
Cite this article
Assi, C., Kheir, N., Samaha, C. et al. Optimizing patellar positioning during total knee arthroplasty: an anatomical and clinical study. International Orthopaedics (SICOT) 41, 2509–2515 (2017). https://doi.org/10.1007/s00264-017-3557-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3557-4