Abstract
Purpose
A cutting guide technique for patella resurfacing in total knee arthroplasty was expected to result in less patellofemoral syndromes. The aim of this study was to identify differences in the patellofemoral function, clinical outcomes, and radiographic parameters between the freehand and cutting guide patellar resection techniques in patients undergoing total knee arthroplasty.
Methods
A prospective randomized controlled trial was conducted. The study was registered in a public trials registry (International Standard Randomized Trial No. NCT02268097). One-hundred total knee arthroplasties in 100 patients were randomly allocated into one of the two groups, and their results were followed for a mean of 28 months (range, 18 to 38 months) in a double-blind (both patient and evaluator), prospective study. Evaluation was performed by an independent observer using patellofemoral functional capacity, the Knee Society clinical rating system, the Western Ontario and McMaster Universities Osteoarthritis Indices, and radiographic examination.
Results
In total, 14% of the patients were lost to follow-up. There was no difference in the incidence of anterior knee pain between the two groups. No patients received or required revisions. There was a significant difference in the outliers of lateral patellar tilt between the freehand and cutting guide groups (> 10°) (p = 0.036); however, the mean value of lateral patellar tilt did not differ significantly. There were no differences between groups with respect to the 30 seconds stair climbing test, complications, the Knee Society clinical rating system, the Western Ontario and McMaster Universities Osteoarthritis Indices, patient satisfaction, physical examination, hip-knee-ankle angle, lateral patellar displacement, or the Insall-Salvati ratio. Meanwhile, gender, age, weight, height, body mass index, pre-operative Knee Society scores, and pre-operative range of motion were not found to be related to the development of anterior knee pain.
Conclusions
Cutting guide technique group did not yield lower incidence of anterior knee pain. More outliers of lateral patellar tilt were observed in the freehand technique group. Overall, all patients in both groups had identical results in terms of patellofemoral functional capacity, clinical outcomes, and other radiographic results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is a successful surgical procedure. Long-term observational studies have indicated that more than 90% of modern primary TKA survive for at least 15 years [1]. In TKA cases, a controversy exists over whether to perform patellar resurfacing [2, 3]. Patients undergoing patellar replacement have a lower incidence of revision rate and anterior knee pain rate (AKP) than those without patellar replacement [4]. Therefore, it is common to perform patellar resurfacing when conducting TKA. In patellar resections, a number of principles should be considered including restoring patellar height, performing a symmetric resection, avoiding under-resection, and minimizing over-stuffing of the patellofemoral joint [5]. When resurfacing the patella, using a reasonable resection of the patella is more conducive to installing the patellar component; at the same time, a reasonable resection can reduce AKP, patellar fractures, and patella maltracking [6, 7]. Of the several patellar resection instruments provided by prothesis manufacturers, the cutting guide is one of the more common auxiliary patellar resection devices used. However, many surgeons still favor using the freehand technique with haptic feedback because they believe it achieves similar results [8, 9]. Previous nonrandomized cohort study has compared different patellar resection techniques with measurements made intra-operatively [10], and some have compared results using radiography [11, 12]. Few studies have directly compared the patellofemoral function and patellar alignment of different patellar resection techniques, which are important outcomes for surgeons [13].
Therefore, in this study, we sought to compare the patellofemoral function-related assessments, clinical outcomes, and radiographic outcomes between resections performed using the freehand technique and the cutting guide technique with a mean of 28 months of follow-up. The primary hypothesis is that using a cutting guide would yield lower incidence of AKP which is a main parameter of patellofemoral function [14]. To our knowledge, this study is the largest prospective randomized clinical trial to address the issue to date.
Materials and methods
The investigation was designed as a prospective randomized parallel controlled trial examining patients who underwent TKA at the Peking University Third Hospital between October 2014 and June 2016. The trial was registered in a public trial registry (International Standard Randomized Trial No. NCT02268097) and was approved by the institutional review board (IRB00006761-2011072). Informed consent was obtained from all enrolled patients. Patients were randomized to receive either the freehand technique or the cutting guide technique. Randomization was accomplished by opening a randomly selected envelope by circuiting nurses in the operating room after the capsule was opened. When a patient was to receive a bilateral patellar resurfacing, the first knee received the treatment indicated by the envelope.
The inclusion criteria for this study were as follows: a diagnosis of primary osteoarthritis of the knee with an Ahlback grade ≥ 2 (symptoms persisting after conservative treatment for at least 3 months); a varus of < 20° or valgus of < 15°; and a body mass index (BMI) of < 35. The exclusion criteria were inflammatory arthritis, restricted motion (flexion contracture of > 25°), patella alta (an Insall-Salvati ratio of < 0.6), a history of patellar fracture, a prior patellectomy, patellofemoral instability, or a history of previous knee surgery. We made 100 random sealed envelopes through computerized block randomization, and 100 patients were included in the study. During the enrollment period, 112 patients met the inclusion criteria. Of these, 100 patients agreed to participate, representing 89% of all eligible patients. Of the 100 patients, 14 patients were lost to follow-up: one died; one 83-year-old patient in the cutting guide group could not attend the clinic because he was unable to walk due to knee pain; and 12 of the patients enrolled in this study were lost to follow-up as we could not contact them or their kin. Eighty-six patients were thus included in the final study population. Patellofemoral functional capacity, clinical information, and radiographic assessments were made for each patient. The patients in the two treatment groups were similar with respect to their demographic variables and pre-operative status (Table 1), except for two valgus patients in the freehand group and one in the cutting guide group.
Surgical technique
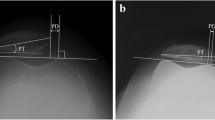
This study used Nexgen Legacy Posterior Stabilized-flex Prosthesis (Zimmer, Warsaw, Indiana, USA) components. All components were cemented. All surgery was performed by one senior surgeon (JKY) or his trainees while under his supervision. A similar technique was used for all surgeries that employed a uniform quadriceps-sparing (QS) approach and preserved the infrapatellar fat pad. For the QS approach, the knee of the patient was flexed to 30°, and a medial curvilinear skin incision was made and extended along the medial edge of the tibial tubercle. The quadriceps tendon was divided for a length of 2 cm. The vastus medialis obliquus muscle was divided if its insertion point was at the medial edge of the patellar. Minimally invasive QS instruments (Zimmer) were used. First, the native patellar thickness was measured using flat tipped calipers, and the target for post-resection thickness was noted in both groups [15]. The patella was resected using a freehand technique (Fig. 1a) with an oscillating saw, and the surgeon judged the symmetry based on haptic feedback and thickness by measuring the center of the patella. Repeating resection was performed as necessary until the desired thickness and symmetry were obtained. The cutting guide (Fig. 1b) was set to the desired resection depth and applied in a symmetric fashion using the articular surface and anterior surface. The guide was removed, but surgeons were permitted to reapply the guide to recut the patella if they felt that additional resection was required by haptic feedback. A cemented, three-peg, all-polyethylene, round patella was used to maximize bone coverage with medialization of the component, and restored thickness was measured. All loose synovium and osteophytes were removed to minimize peripatellar scar formation and subsequent crepitation or clunk. Optimal patellar tracking was ensured by appropriate soft-tissue balancing, and a lateral release was performed if the patella subluxated during passive range-of-motion testing [16]. A 7.5-mm patella component was used for 90% of the cases.
The post-operative rehabilitation protocol was identical in both the groups. Physical therapy was initiated on the day of surgery. Physical therapy included weight-bearing exercises using an assistive device on the first post-operative day and ROM exercises on the fourth day after surgery with increasing complexity as the patients’ tolerance progressed. The decision of whether patients were discharged from the hospital or were admitted to the inpatient rehabilitation unit was made by the physical therapist and the rehabilitation team, not by the operating surgeon.
Patellofemoral function and clinical assessment
The duration of follow-up ranged from 18 to 38 months after TKAs. All evaluations were conducted and reviewed by two investigators (FZY and ZWS) who were blinded to the type of treatment the patient received.
The number of complications was determined by both the inpatient and outpatient medical records of each patient. The Knee Society clinical rating system (KSS) [17] was used in each evaluation to assess pain as well as the stability, function, and range of motion (ROM) in the knee. When measuring ROM, the goniometer was centered on lateral femoral condyle with one arm placed along the long axis of the femur pointing to the greater trochanter and the other arm placed along the long axis of the tibia pointing to the lateral malleolus [18]. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was also used as a patient-reported outcome score. Additionally, all patients answered a simplified satisfaction questionnaire that was developed by Barrack et al. [19] and Burnett et al. [20] regarding TKA. Patients were asked, “Are you satisfied with your general knee function?”, “Are you satisfied with your pain relief?”, and “Are you satisfied with returning to daily life?”. The answer was “Extremely” or “Very” or “Not”. Besides, questions regarding the severity of AKP in general and pain experienced when climbing stairs, rising from a chair, or exiting an automobile were also asked of all patients as a means of identifying symptoms related to the patellofemoral joint.
Several functional and physical examinations were conducted including a 30-second stair climbing test, a patellar glide test (medial and lateral translation), a grind test (isometric quadriceps contraction with the patella immobilized and the knee in extension, thus forcing the patella into the trochlear groove), and an assessment of patellar edge tenderness (isometric quadriceps contraction with the patella immobilized and the knee in extension, pressing sites around patella). In the 30-second stair climb test, patients were asked to ascend a set of steps, turn around, and descend the same steps, and then repeat this sequence in an empty stairwell that contained 20-cm high steps and 12 steps between platforms. Patients were instructed to complete as many steps as possible, with or without the rail, during the 30-second period.
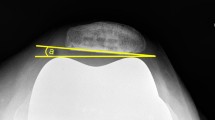
Radiographic assessment
Radiographs were taken before the operation and at the final follow-up examination. Full-length weight-bearing anteroposterior, supine posterior-anterior, and lateral conventional radiographs were taken of the knee that received the operation, and patellar skyline views were used as the basis for all assessments. In accordance with the principles stipulated by the knee society [21], radiographic measurements were made by two observers who were blinded to the patients’ treatment groups (FZY and HJW) by using computer-generated data derived from the digital radiographs. Lateral patellar tilt for patellar tilt (cutoff point ≥ 10°) and lateral patellar displacement (cutoff point ≥ 4 mm) were measured on sunrise radiographic views at 30° to 40° of flexion [22, 23] as well as for the hip-knee-ankle (HKA) angle in the full-length weight-bearing anteroposterior view. Patella baja was evaluated using the Insall-Salvati ratio [24].
Statistical analysis
Statistical analyses were conducted using the 2011 release of IBM SPSS Statistical Software for Windows, version 20.0 (IBM Corp., Armonk, NY, USA). Student t tests or the Mann-Whitney U tests were used to analyze differences in continuous variables between the two groups. Categorical variables and percentages of the outliers in different components were analyzed using chi-square tests and Fisher’s exact tests. Cox proportional hazards regression analysis was used to assess the associations between potential explanatory variables and postoperative AKP. Significance was set at a two-tailed p < 0.05.
A sample size was performed based on the primary outcome variable. The null hypothesis was that patellar resection using cutting guide had lower AKP incidence and the sample size is 76 based on an estimated 20% prevalence of AKP, an 18% confidence interval, and a significance of 5%. Considering the rate of loss of follow-up (15%), the final sample size should be 90. And our study enrolled 100 subjects and the final follow-up rate is 86%.
Results
Anterior knee pain and predictive factors for anterior knee pain
The results for 86 knees showed a similar presence of AKP in the two groups: 9.09% in knees repaired using the freehand technique and 7.14% in knees repaired with the cutting guide technique (p = 0.741). No significant relationship was found between the patellar resection technique and the patient’s postoperative presence of AKP when getting into and out of an automobile (p = 0.781), getting into and out of a chair (p = 0.501), or negotiating stairs (p = 0.945) (Fig. 2).
Revisions and other complications
Two complications occurred in the freehand group, while one occurred in the cutting guide group. Thus, there were no significant differences in the number of complications between the groups (p = 1.00), based on a continuity correction chi-square test. One patient who was enrolled in the freehand technique group developed deep vein thrombosis after surgery. The condition was suspected based on the presenting symptoms and was confirmed using venous ultrasound. The condition improved after treatment with anticoagulation medication; however, temporary peroneal nerve palsy occurred but resolved four months after the operation. The complication in the cutting guide group was temporary peroneal nerve palsy. No complications occurred in other patients, and no revisions or complications related to the patellofemoral joint were required or observed.
Knee Society clinical rating system scores and the Western Ontario and McMaster Universities Osteoarthritis Index
Table 2 shows the WOMAC score and the KSS sub-scores for pain, total knee, total function scores, and ROM for pre-operative and post-operative patients. There were significant improvements in both groups after TKA with respect to the pain score, total knee score, total function score, ROM, and WOMAC score (p < 0.001). There were no significant differences between the freehand group and cutting guide group with respect to the pain sub-scores (p = 0.37), total knee score (p = 0.78), total functional score (p = 0.58), ROM (p = 0.89), or WOMAC score (p = 0.35) at the most recent follow-up examination (Fig. 3).
Patient satisfaction
No significant differences were found between the freehand and cutting guide groups for patient satisfaction with pain relief (continuity correction chi-square, p = 1.00), return to daily activities (Pearson chi-square, p = 0.431), or general function (Pearson chi-square, p = 0.431). However, there was a minor trend indicating higher satisfaction among patients in the cutting guide group (Fig. 4).
Predictors of anterior knee pain
We analyzed several patient factors to determine if they could predict the development of AKP in the groups. According to a Cox regression analysis, sex, age, weight, height, body mass index (BMI), pre-operative KSS, and pre-operative range of motion were not related to the development of anterior knee pain (p > 0.05).
Functional capacity outcome measures
The post-operative functional capacity outcome measures are summarized in Table 3. Patellar glide, the grind test, and patellar edge tenderness were examined at the final follow-up visit. Four of the 44 knees in the freehand group had AKP during the patellar glide test, and three of the 42 knees had pain in the cutting guide group. There were no significant differences in patellar glide pain based on the patellar resection technique used (p = 0.741). Five out of 44 knees and three out of 42 knees in the freehand and cutting guide groups, respectively, had pain during the patellar grind test. Again, there was no relationship between patellar grind pain and the patellar resection technique used (p = 0.501). No significant difference was found between patellar edge tenderness and the patellar resection technique used (p = 0.953).
A 30-seconds stair climb test was conducted to assess patient’s functional capacity. Patients in the freehand technique group climbed a mean 32.7 ± 8.0 stairs, compared with 32.5 ± 9.1 stairs in the cutting guide group (p = 0.901). One patient in the cutting guide group was unable to climb stairs at the 33-month follow-up visit because of severe bilateral pain knee.
Radiographic data
The post-operative radiological data are summarized in Table 4. Lateral patellar tilt (LPT) averaged 3.90° in the freehand group and 3.00° in the cutting guide group (p = 0.358). Using a standard to define radiographic outliers clinically for LPT (> 10°) [22], a significant difference was observed in the number of outliers in the freehand group (ten of 44 knees) and the cutting guide group (two of 42 knees) (p = 0.036). The mean amounts of lateral patellar displacement (LPD) were − 1.93 ± 3.54 mm and − 1.78 ± 4.50 mm in the freehand and cutting guide groups, respectively, and this difference was not significant (p = 0.869). There were no significant differences in the frequency of outliers (displacement of > 4 mm) [22] between the two groups; three of the 44 knees in the freehand group were outliers, compared with two of the 42 knees in the cutting guide group (p = 1.000). The mean Insall-Salvati index (IS) was 1.02 in the freehand group and 1.05 in the cutting guide group (p = 0.455). Using a standard of < 0.8 or > 1.2, there were no significantly different numbers of radiographic outliers of IS between the groups (p = 0.885). There were 10 outliers in the freehand group and 9 outliers in the cutting guide group.
The post-operative hip-knee-ankle angles measured in the coronal plane were 2.62° ± 1.55° and 2.32° ± 1.47° in the freehand and cutting guide groups, respectively (p = 0.328). There were no significant differences between the freehand and cutting guide groups in terms of the frequency of outliers in radiographic lower limb alignment (< 87° or > 93° on the anteroposterior radiograph) (p = 0.548).
Discussion
This study reported patellofemoral function, clinical outcomes, and radiographic results in freehand and cutting guide patellar resection techniques. As for the hypothesis, relevant results show that no statistically significant difference was observed in the incidence of AKP between the two groups in our prospective randomized controlled trial.
Neither patellar resection technique could guarantee a painless patellofemoral joint. AKP, which reflects the function of patellofemoral joint, was objectively assessed in all patients who performed the radiographic test. The results at a mean of 28 months showed a similar presence of AKP between the groups: 9.09% of knees in the freehand group and 7.14% of knees in the cutting guide group (p = 0.741). To further assess the impact of the AKP, we inquired about the AKP during activities of daily living (climbing stairs, getting out of a chair, and getting into and out of an automobile); there were no significant differences in these measures between groups and there was no relationship between body mass index and the development of pain. Meanwhile, there were no significant differences between groups for any of the patellofemoral examinations that were conducted (patellar glide test, grind test, and patellar edges tenderness, all p > 0.05). Additionally, the incidence of pain in the patellofemoral examinations was similar to that for AKP, and both conditions appeared in most of the same patients. This finding suggests that patellofemoral examination (patellar glide test, grind test, and patellar edges tenderness) parallels the incidence of AKP to some extent. The exact pathogenesis of AKP is probably multifactorial including the type of prosthesis [25] and femoral component design [26] which are the same in our study. Wolf Petersen et al. [27] states that the incidence of AKP is related to factors such as thigh muscles and the hip and trunk stabilizing muscles which may influence on the movement pattern of the knee. Thus, in our future follow-up, we believe that those factors mentioned above by Wolf Petersen et al. [27] need to be considered and studied.
Radiographic assessments were conducted in which we found that there was difference between the two groups for the outliers of LPT (> 10°) (p = 0.036); however, the mean LPT value did not differ significantly. This indicates that, to a certain degree, the cutting guide technique may be superior for patellar resection. And we observed that different incidence of LPT outliers did not produce differences in the patellofemoral examinations or differences in the incidence of AKP which is consistent with previous studies [28, 29]. Besides, we did not find any significant differences between the two groups for the mean values or outliers of HKA, LPD, and IS. None of the cemented patellar components had loosened at the time of the most recent radiographs.
As of this writing, no patient had received or required revision. There were no significant differences in complications at follow-up (continuity correction chi-square, p = 1.00) between the groups. Three patients who suffered deep vein thrombosis and temporary peroneal nerve palsy all came to the clinic for follow-up and were all satisfied with the results of TKA. When we examined the KSS and the WOMAC score, we found significant post-operative improvements at a mean of 28 months in both groups; however, there were no significant differences between the freehand and cutting guide patellar resection techniques with respect to Knee Society pain (p = 0.37), knee (p = 0.78), function (p = 0.58) scores, ROM (p = 0.89), or the WOMAC score (p = 0.35). We observed that patients with lower KSS or higher WOMAC scores generally had compounding medical conditions, bilateral knee pain, and knees that had poor flexion and extension. In other studies, we have found that whether the patella is resurfaced in TKA has no significant differences in the KSS or the WOMAC score [2, 30, 31]. Other studies that examined the effects of using different surgical techniques as well as their use of various instruments and prostheses also reported that these factors had no relationship with these scores [32,33,34]. Therefore, we believe that better knee function may be more relevant to basic principles including excellent lower limb alignment, proper prothesis position, integrated ligaments, and greater lower limb strength.
General patient satisfaction and two other satisfaction questions (pain relief and return to activities of daily living) in regard to TKA were evaluated using the questionnaire developed by Barrack et al. [19] and Burnett et al. [20]; these results were very similar to the previously reported findings [13].
Meanwhile, 30-second stair climb test was repeated in all patients as a functional measure at the follow-up visit. There was no significant difference between the freehand and cutting guide technique groups. Two patients who were over 80 years of age could not easily ascend and descend the stairs because of bilateral knee pain and heart disease. Another two patients, who were both over 70 years of age, could only climb approximately ten stairs in 30 seconds because they had either less than 90 degrees of knee flexion or poor muscle strength. These findings suggest that the use of a 30-second stair climb test may be limited in the elderly population and in those with compounding medical conditions that affect the ability to climb stairs.
The present study has limitations and the conclusions drawn from it should be interpreted with caution. The number of patients studied is an important consideration. At the follow-up, 14% of the original study participants were lost to follow-up. The sample size in this study was too small to provide adequate power to detect all of the differences between the groups, which is an important consideration. Additionally, many lost-to-follow-up patients refused to come because they claimed to be “very good” or because they “could not walk because of bilateral knee pain” which could have affected the results. We did not conduct pre-operative 30-second stair climb tests, which weakens the validity of evaluating patellofemoral joint function to a certain extent. We noticed that, especially in patients with low KSS, the strength of the quadriceps was generally weak. In this study, we did not collect objective indicators of quadriceps strength such as an extension torque and flexion torque test.
The strengths of this prospective randomized controlled trial include the use of independent evaluators, patellofemoral function-related examinations, clinical outcomes, and radiographic results. The results of the present study may be specific to the implant and the surgical techniques that were utilized. Until now, a reference point for patellar resections has not been unified [9,10,11, 13, 35,36,37]. However, a number of principles in patellar resection should be considered including in determining such a reference: restoring patellar height, performing a symmetric resection, avoiding under-resection, and minimizing over-stuffing of the patellofemoral joint [6, 10]. In our study, the surgeons were high-volume arthroplasty surgeons who had done more than 500 TKAs. The surgeons generally believed that the freehand technique for patellar resection is more efficient without compromising patellofemoral functional capacity. Based on the results of this study, we are cautiously optimistic about the freehand technique though less outliers of LPT.
References
Ranawat CS, Flynn WJ, Saddler S, Hansraj KK, Maynard MJ (1993) Long-term results of the total condylar knee arthroplasty. A 15-year survivorship study. Clin Orthop Relat Res 94–102
Breeman S, Campbell M, Dakin H, Fiddian N, Fitzpatrick R, Grant A, Gray A, Johnston L, Maclennan G, Morris R, Murray D (2011) Patellar resurfacing in total knee replacement: five-year clinical and economic results of a large randomized controlled trial. J Bone Joint Surg Am 93:1473–1481. https://doi.org/10.2106/JBJS.J.00725
Longo UG, Ciuffreda M, Mannering N, D’Andrea V, Cimmino M, Denaro V (2017) Patellar resurfacing in total knee arthroplasty: systematic review and meta-analysis. J Arthroplast. https://doi.org/10.1016/j.arth.2017.08.041
Grassi A, Compagnoni R, Ferrua P, Zaffagnini S, Berruto M, Samuelsson K, Svantesson E, Randelli P (2018) Patellar resurfacing versus patellar retention in primary total knee arthroplasty: a systematic review of overlapping meta-analyses. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-4831-8
Rand JA (1990) Patellar resurfacing in total knee arthroplasty. Clin Orthop Relat Res 110–117
Pagnano MW, Trousdale RT (2000) Asymmetric patella resurfacing in total knee arthroplasty. Am J Knee Surg 13:228–233
Fu C, Wai J, Lee E, Myden C, Batuyong E, Hutchison CR, Anglin C (2012) Computer-assisted patellar resection for total knee arthroplasty. Comput Aided Surg 17:21–28. https://doi.org/10.3109/10929088.2011.638399
Assiotis A, Ng MSS, Mordecai S, Hollingdale J (2015) A novel freehand method for patellar resurfacing in total knee replacement. Acta Orthop Belg 81:340–343
Lombardi AJ, Mallory TH, Maitino PD, Herrington SM, Kefauver CA (1998) Freehand resection of the patella in total knee arthroplasty referencing the attachments of the quadriceps tendon and patellar tendon. J Arthroplast 13:788–792
Camp CL, Martin JR, Krych AJ, Taunton MJ, Spencer-Gardner L, Trousdale RT (2015) Resection technique does affect resection symmetry and thickness of the patella during total knee arthroplasty: a prospective randomized trial. J Arthroplast 30:2110–2115. https://doi.org/10.1016/j.arth.2015.05.038
Anglin C, Fu C, Hodgson AJ, Helmy N, Greidanus NV, Masri BA (2009) Finding and defining the ideal patellar resection plane in total knee arthroplasty. J Biomech 42:2307–2312. https://doi.org/10.1016/j.jbiomech.2009.06.021
Camp CL, Bryan AJ, Walker JA, Trousdale RT (2013) Surgical technique for symmetric patellar resurfacing during total knee arthroplasty. J Knee Surg 26:281–284. https://doi.org/10.1055/s-0032-1330056
Stryker LS, Odum SM, Springer BD, Fehring TK (2017) Role of patellofemoral offset in total knee arthroplasty: a randomized trial. Orthop Clin North Am 48:1–7. https://doi.org/10.1016/j.ocl.2016.08.001
Meftah M, Jhurani A, Bhat JA, Ranawat AS, Ranawat CS (2012) The effect of patellar replacement technique on patellofemoral complications and anterior knee pain. J Arthroplast 27:1075–1080. https://doi.org/10.1016/j.arth.2011.10.006
Barrack RL, Wolfe MW, Waldman DA, Milicic M, Bertot AJ, Myers L (1997) Resurfacing of the patella in total knee arthroplasty. A prospective, randomized, double-blind study. J Bone Joint Surg Am 79:1121–1131
Benjamin J, Chilvers M (2006) Correcting lateral patellar tilt at the time of total knee arthroplasty can result in overuse of lateral release. J Arthroplast 21:121–126. https://doi.org/10.1016/j.arth.2006.05.001
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 13–14
Brosseau L, Balmer S, Tousignant M, O’Sullivan JP, Goudreault C, Goudreault M, Gringras S (2001) Intra- and intertester reliability and criterion validity of the parallelogram and universal goniometers for measuring maximum active knee flexion and extension of patients with knee restrictions. Arch Phys Med Rehabil 82:396–402. https://doi.org/10.1053/apmr.2001.19250
Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, Myers L (2001) Patellar resurfacing in total knee arthroplasty - a prospective, randomized, double-blind study with five to seven years of follow-up. J Bone Joint Surg Am 83A:1376–1381
Burnett RS, Haydon CM, Rorabeck CH, Bourne RB (2004) Patella resurfacing versus nonresurfacing in total knee arthroplasty - results of a randomized controlled clinical trial at a minimum of 10 years’ followup. Clin Orthop Relat Res 12–25. https://doi.org/10.1097/01.blo.0000148594.05443.a3
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Heesterbeek PJ, Beumers MP, Jacobs WC, Havinga ME, Wymenga AB (2007) A comparison of reproducibility of measurement techniques for patella position on axial radiographs after total knee arthroplasty. Knee 14:411–416. https://doi.org/10.1016/j.knee.2007.06.006
Chonko DJ, Lombardi AJ, Berend KR (2004) Patella baja and total knee arthroplasty (TKA): etiology, diagnosis, and management. Surg Technol Int 12:231–238
Insall J, Salvati E (1971) Patella position in the normal knee joint. Radiology 101:101–104. https://doi.org/10.1148/101.1.101
Biau D, Mullins MM, Judet T, Piriou P (2006) Mobile versus fixed-bearing total knee arthroplasty: mid-term comparative clinical results of 216 prostheses. Knee Surg Sports Traumatol Arthrosc 14:927–933. https://doi.org/10.1007/s00167-006-0070-5
Saffarini M, Ntagiopoulos PG, Demey G, Le Negaret B, Dejour DH (2014) Evidence of trochlear dysplasia in patellofemoral arthroplasty designs. Knee Surg Sports Traumatol Arthrosc 22:2574–2581. https://doi.org/10.1007/s00167-014-2967-8
Petersen W, Rembitzki IV, Bruggemann GP, Ellermann A, Best R, Koppenburg AG, Liebau C (2014) Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop 38:319–328. https://doi.org/10.1007/s00264-013-2081-4
van Jonbergen HP, Reuver JM, Mutsaerts EL, Poolman RW (2014) Determinants of anterior knee pain following total knee replacement: a systematic review. Knee Surg Sports Traumatol Arthrosc 22:478–499. https://doi.org/10.1007/s00167-012-2294-x
van Houten AH, Heesterbeek PJ, Wymenga AB (2016) Patella position is not a determinant for anterior knee pain 10 years after balanced gap total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:2656–2662. https://doi.org/10.1007/s00167-015-3930-z
He JY, Jiang LS, Dai LY (2011) Is patellar resurfacing superior than nonresurfacing in total knee arthroplasty? A meta-analysis of randomized trials. Knee 18:137–144. https://doi.org/10.1016/j.knee.2010.04.004
Smith AJ, Wood DJ, Li MG (2008) Total knee replacement with and without patellar resurfacing - a prospective, randomised trial using the profix total knee system. J Bone Joint Surg Br 90B:43–49. https://doi.org/10.1302/0301-620X.90B1.18986
Shin YS, Kim HJ, Ko YR, Yoon JR (2016) Minimally invasive navigation-assisted versus conventional total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-016-4016-2
Unwin O, Hassaballa M, Murray J, Harries W, Porteous A (2017) Minimally invasive surgery (MIS) for total knee replacement; medium term results with minimum five year follow-up. Knee 24:454–459. https://doi.org/10.1016/j.knee.2017.01.010
Stolarczyk A, Nagraba L, Mitek T, Stolarczyk M, Deszczynski JM, Jakucinski M (2018) Does patient-specific instrumentation improve femoral and tibial component alignment in total knee arthroplasty? A prospective randomized study. Adv Exp Med Biol. https://doi.org/10.1007/5584_2018_193
Park DY, Ji HM, Kwak KS, Nair SG, Won YY (2012) Three dimensional CT-based virtual patellar resection in female patients undergoing total knee replacement: a comparison between tendon and subchondral method. Clin Orthop Surg 4:193–199. https://doi.org/10.4055/cios.2012.4.3.193
Fu CK, Wai J, Lee E, Hutchison C, Myden C, Batuyong E, Anglin C (2012) Computer-assisted patellar resection system: development and insights. J Orthop Res 30:535–540. https://doi.org/10.1002/jor.21567
Ledger M, Shakespeare D, Scaddan M (2005) Accuracy of patellar resection in total knee replacement. A study using the medial pivot knee. Knee 12:13–19. https://doi.org/10.1016/j.knee.2003.11.007
Funding
This study was funded by the National Key R&D Program of China (No. 2017YFB1303000).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The trial was registered in a public trial registry (International Standard Randomized Trial No. NCT02268097) and was approved by the institutional review board (IRB00006761-2011072). Informed consent was obtained from all enrolled patients.
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Yuan, F., Sun, Z., Wang, H. et al. Clinical and radiologic outcomes of two patellar resection techniques during total knee arthroplasty: a prospective randomized controlled study. International Orthopaedics (SICOT) 43, 2293–2301 (2019). https://doi.org/10.1007/s00264-018-4264-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4264-5