Abstract
Purpose
The influence of cruciate-ligament-retaining (CR-TKA) and cruciate-ligament-substituting (CS-TKA) TKA on tibiofemoral kinematics was analysed in many investigations. However, the influence on patellar kinematics is unclear so far. The aim of this study was to compare patellar kinematics of the natural knee with those after CR- and CS-TKA.
Methods
Patellar kinematics of nine healthy whole-body cadaveric knees before and after CR- and CS-TKA was investigated using a commercial optical computer navigation system. Patellar kinematics of the healthy knee was compared with those after CR- and CS-TKA.
Results
No significant difference between the natural knee and the knee after TKA or between both types of TKA for patellar kinematics could be found. Interestingly, both types of TKA resulted in a more medial patellar shift and a contrary patellar tilt and rotation behaviour. CR- and CS-TKA resulted in smaller values for patellar epicondylar distance at all flexion angles.
Conclusions
Our study found no influence of prosthesis type on patellar kinematics. Factors like component alignment and prosthesis design seem to be more important in terms of adequate restoration of patellar kinematics in TKA than whether choosing CR- or CS-TKA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Post-operative anterior knee pain is one of the remaining major complications after total knee arthroplasty (TKA). Recent cadaveric and biomechanical investigations contribute anterior knee pain and patellar maltracking primarily to femoral and tibial component malalignment [1–9]. Moreover, frequency and severity of anterior knee pain after TKA is influenced by greater forces upon the patellofemoral joint caused by abnormal sagittal gait patterns [10, 11]. The influence of cruciate-ligament-retaining (CR-TKA) and cruciate-ligament-substituting (CS-TKA) TKA on tibiofemoral kinematics has been analysed in many recent investigations, and significant differences between both types of TKA have been demonstrated [12, 13]. CS-TKA showed a greater mean posterior displacement of tibiofemoral contact points, and forward displacement of the tibiofemoral contact areas could be found more frequent in CR- than in CS-TKAs. However, the influence of CR- and CS-TKA on patellofemoral kinematics is unclear. The aim of this investigation was to compare patellar kinematics in the natural knee and in knees with a CR- and CS-TKA. Based on the above-mentioned investigations, we hypothesised that altered tibiofemoral contact points due to the use of either a CR- or CS-TKA significantly changes patellofemoral kinematics compared with those of the natural knee.
Material and methods
Lower limbs of nine Thiel-embalmed whole-body cadavers were used for this investigation. All knees were free of gross arthritic deterioration, severe alignment deviation or dysplasia and had no history of surgery or injury. Patellar kinematics [mediolateral shift (mm): medial +, lateral −; axial tilt (°): medial −, lateral +; rotation (°): medial +, lateral −; epicondylar distance (mm): distance between patella and anatomical transepicondylar axis] were investigated using a commercial optical computer navigation system (Knee Patella Tracking Software, BrainLAB; Feldkirchen, Germany) before and after standard fixed-bearing CR- and CS-TKA.
Surgical procedure
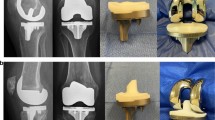
After performing a standard midline skin incision, a medial parapatellar approach was conducted. The joint capsule of each knee was marked at four defined locations with a waterproof pen (3-cm proximal to the superior patellar tip, at the medial proximal patellar edge, centrally at the medial patellar edge and at the medial distal patellar edge) to ensure subsequent anatomic closure. Reference arrays for the navigation system were attached to the proximal tibia and distal femur. The femoral array was attached through an additional 1-cm incision to avoid soft tissue tension while performing the motion cycle. After referencing the hip centre by circumduction, the standardised landmarks (femoral epicondyles, femoral entry point, medial and lateral malleolus, tibial plateau magnitude, eminentia intercondylaris) were acquired to define the femoral and tibial coordinate system. Afterwards, femorotibial kinematics were measured by using the navigation system. The line connecting the middle of the posterior cruciate ligament (PCL) to the medial edge of the patellar tendon onset (tibial tubercle) was defined as the tibial anteroposterior (AP) axis according to Akagi [1]. Subsequently, the patellar array (BrainLAB; Feldkirchen, Germany) was fixed onto the front of the patella with a small screw, as recommended by the manufacturer. The most medial, superior and inferior edge and the most prominent point at the posterior articular ridge of the patella were registered to define the patellar coordinate system. After anatomical closure of the joint capsule at the prior defined locations, the natural patellar kinematics and relative orientation between femur, tibia and patella was recorded. The lower extremity was placed free onto a continuous passive motion machine in a straight position without muscle load to simulate intraoperative conditions. Three motion cycles were performed while patellar kinematics were measured every 10° between 0° and 90° of flexion (Fig. 1). Subsequently, the measurement of patellar kinematics was repeated after implanting the trial CR and thereafter the CS prosthesis of the same geometry and same manufacturer (PFC Sigma, cruciate retaining/ cruciate substituting, fixed-bearing inlay; DePuy, Warsaw, IN, USA) in equal coronal, sagittal and axial alignment; in the frontal plane, cuts were performed perpendicular to the femoral and tibial mechanical axis. Femoral rotation was set to standardised 3° of external rotation related to the femoral posterior condylar line. Rotational alignment of the tibial tray was set to the above-mentioned Akagi line and was fixed using centrally placed screws. Rotational alignment of the tibial tray was the same in both CS- and CR-TKAs. No ligament release was necessary due to healthy knees, and the joint line could be restored in every knee using the navigation system. Thereafter, a bony resection of the patella was performed to resect 9 mm off the natural thickness using a calliper. Subsequently, patellar resurfacing was performed with a 9-mm inset oval dome component (PFC Sigma; DePuy). The dome component was placed centrally and the best-fitting dome patella was used; size 38 was used in six and 35 in four cases. Prior patellar kinematics were registered, and each time, accuracy of the desired position of the femoral and tibial component was verified using the navigation system and adapted if required.
Statistical analysis
In the figures, error bars represent one standard error (SE). Student’s t test for paired samples and Wilcoxon’s signed-rank test for not normally distributed data was used to determine statistical significance. A p value of <0.05 was considered to indicate statistical significance. Power analysis was done post hoc for paired samples using the standard deviation (SD) of the difference between compared groups. All values are reported for a power of 0.90. Analyses were performed using SPSS Statistics 21.0 (IBM, Chicago, IL, USA).
Results
Mean values of patellar kinematics were analysed relative to the femoral coordinate system before and consecutively after implantation of the CR and CS trial components. The study had the power to detect a difference of 0.7–1.5 mm and 1.5–4° between the natural knee and the TKAs and to detect a difference of 0.5–1.0 mm and 2.5–3.5° between the two types of TKAs.
Mediolateral shift
The natural knee and both types of TKA showed a constant increase in medial patellar shift from 20° to 90° of flexion. Interestingly, in early flexion angles, the natural knee and the CS-TKA showed an initial lateral patellar shift, while the CR-TKA showed a constant increase from the beginning. There was a tendency for the patella to be more medial relative to the femoral matrix in the presence of the TKA compared with the natural knee; however, this did not reach statistical significance. Although patella of the CS-TKA showed a more “natural” tracking behaviour, no significant difference between both types of TKAs could be detected (Fig. 2).
Epicondylar distance
Epicondylar distance in the natural knee and the knee after either CR- or CS-TKA showed a nearly linear decrease with flexion. Both types of TKA resulted in smaller values for patellar epicondylar distance at every flexion angle. No significant difference, whether between the natural knee and knee after TKA or between the CR- and CS-TKA could be detected (Fig. 3).
Rotation
In contrast to TKA patellas, that of the natural knee rotated more externally, from 40° to 90°, of flexion. Patellae of both types of TKA showed a similar rotation behaviour from 40° to 90° of flexion, whereas the CR-TKA resulted in a more externally rotated patella, from 0° to 40° of flexion, compared with the natural knee and the CS-TKA. However, no significant difference between TKAs and between TKAs and the natural knee were found (Fig. 4).
Tilt
The natural preoperative knee showed a nearly linear increase in lateral patellar tilt throughout flexion. The CR-TKA showed a more lateral tilt at every flexion compared with the natural knee, with a relative increase from 10° to 40°, and a decrease from 40° to 90° of flexion. Interestingly, the CS-TKA resulted in a more medial patellar tilt during the entire motion cycle. Again, no significant differences between groups was found (Fig. 5).
Discussion
Most importantly, this study demonstrates that there is no significant difference in patellofemoral kinematics between CR-TKA and CS-TKA. Furthermore, compared with both types of TKA, a more lateral patellar shift during the flexion cycle was noticeable in the natural knee, even though this effect did not result in significant values. This could be ascribed to either a more medially placed femoral component or to the centralised trochlea groove of the femoral component, which differ from the natural trochlea groove. No significant difference for patellar epicondylar distance and patellar rotation between both types of TKA and the natural knee was found. CR-TKA and CS-TKA showed similar results for these two patellar kinematic parameters. Patellar epicondylar distance decreased after both types of TKA, which might reflect a difference in trochlea shield compared with the natural knee. Interestingly, compared with the CS-TKA, which showed a similar patellar rotational behaviour, the CR-TKA showed a more externally rotated patella, from 0° to 40° of flexion. This effect also might indicate an increased femoral anterior shift in the CR-TKA compared with the CS-TKA in early flexion angles. However, this possible effect could not be demonstrated with statistical significance. So far, there is no literature to support these findings. For patellar tilt, the CR-TKA showed mean values more similar to the natural knee compared with the CS-TKA but again without statistical significance. Interestingly, CR-TKAs showed a contrary tilt behaviour with a decrease in lateral patellar tilt in higher flexion angles. This might have occurred due to an increased anterior femoral shift compared with the CS-TKA. To the authors’ knowledge, there is no other study in literature investigating a possible influence of CS-TKA and CR-TKA on patellofemoral kinematics. We found only a few studies dealing with the effect of sagittal knee joint loading on patellar kinematics and the incidence of anterior knee pain after TKA. Smith et al. [10] state in their clinical investigation that frequency and severity of anterior knee pain after TKA correlates with higher sagittal forces on the patellofemoral joint. In a fluoroscopic investigation, Stiehl et al. [14] found a more superior patellofemoral contact and higher sagittal patellar tilt angles in TKA patellae compared with normal knees. Takeuchi et al. [15] studied the patellofemoral contact in six cadavers, each with a different type of TKAs, and found different superior and inferior sagittal patellofemoral contact areas. Patellar ligament rotation, which describes the angle between the patellar tendon and the longitudinal axis of the tibia, was lower in TKAs than in natural knees, which may reflect anterior translation of the femur in TKAs at higher flexion angles. Li et al. [16] demonstrated that an increase in posterior tibial translation is accompanied by an increase in contact pressure in the patellofemoral joint. Furthermore, Waslewski et al. [17] found an improvement in pain, effusion and stability after revision to a CS implant in patients with CR-TKA and deficiency of the PCL. A greater and more consistent posterior displacement of the tibiofemoral contact areas (rollback) was seen in the CS compared with the CR TKAs in a prospective study conducted by Victor et al. [13], which explains the higher mean flexion in CS-TKA [12]. Although the above-mentioned results of recent studies indicate a more anterior shift of the tibiofemoral contact areas in CR-TKAs compared with CS-TKAs, which suggests an impact on patellar kinematics, our study found no significant difference in patellar kinematics between both types of TKA.
Our study has some limitations. First, patellar kinematics were measured without muscle force using passive range of motion on a passive motion machine. However, data were collected using healthy cadaveric knees still attached to the torso. Moreover, Masri and Mc Cormack [18] reported that patellar kinematics are not strongly influenced by quadriceps contractions compared with passive motion. The PCL in this study was intact; the influence of TKAs with a deficient PCL on patellofemoral kinematics would have been desirable but could not be realised in this study. In the natural knee, reference points on the patella need to be registered after arthrotomy. Hence, patellar tracking of the natural knee was measured after anatomical closure of the capsule. However, defined marks were set to achieve similar tensionless anatomical closure for patellar tracking before and after TKA, and measurements were performed under similar conditions. Closure and reopening of the arthrotomy and motion cycle on the passive motion machine was conducted with great care due to possible deterioration of the capsule. Furthermore, using CR- and CS-TKA components from one manufacturer might have produced unique patellar kinematics that would not be transferable to knees resurfaced with other implants.
Conclusion
No difference in patellar kinematics between CR- and CS-TKA could be found in our investigation. Results suggest that femoral and tibial component alignment and trochlea shape are more important for adequate restoration of patellar kinematics than whether to use CR- or CS-TKA.
References
Barrack RL, Schrader T, Bertot AJ et al (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop 392:46–55
Belvedere C, Catani F, Ensini A et al (2007) Patellar tracking during total knee arthroplasty: an in vitro feasibility study. Knee Surg Sports Traumatol Arthrosc 15:985–993
Hefzy MS, Jackson WT, Saddemi SR, Hsieh Y-F (1992) Effects of tibial rotations on patellar tracking and patello-femoral contact areas. J Biomed Eng 14:329–343
Kessler O, Patil S, Colwell CW Jr, D’Lima DD (2008) The effect of femoral component malrotation on patellar biomechanics. J Biomech 41:3332–3339
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg (Br) 92-B:1238–1244
Schiavone Panni A, Cerciello S, Del Regno C et al (2014) Patellar resurfacing complications in total knee arthroplasty. Int Orthop 38:313–317
Petersen W, Rembitzki I, Brüggemann G-P et al (2014) Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop 38:319–328
Chinzei N, Ishida K, Matsumoto T et al (2014) Evaluation of patellofemoral joint in advance® medial-pivot total knee arthroplasty. Int Orthop 38:509–515
Howell S, Papadopoulos S, Kuznik K et al (2015) Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop
Smith AJ, Lloyd DG, Wood DJ (2004) Pre-surgery knee joint loading patterns during walking predict the presence and severity of anterior knee pain after total knee arthroplasty. J Orthop Res 22:260–266
Bracey D, Brown M, Beard H et al (2015) Effects of patellofemoral overstuffing on knee flexion and patellar kinematics following total knee arthroplasty: a cadaveric study. Int Orthop
Hirsch HS, Lotke PA, Morrison LD (1994) The Posterior Cruciate Ligament in Total Knee Surgery: Save, Sacrifice, or Substitute? Clin Orthop 309. Symposium
Victor J, Banks S, Bellemans J (2005) Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: a prospective randomised outcome study. J Bone Joint Surg (Br) 87-B:646–655
Stiehl JB, Komistek RD, Dennis DA, Keblish PA (2001) Kinematics of the patellofemoral joint in total knee arthroplasty. J Arthroplasty 16:706–714
Takeuchi T, Lathi VK, Khan AM, Hayes WC (1995) Patellofemoral contact pressures exceed the compressive yield strength of UHMWPE in total knee arthroplasties. J Arthroplasty 10:363–368
Li G, DeFrate LE, Zayontz S et al (2004) The effect of tibiofemoral joint kinematics on patellofemoral contact pressures under simulated muscle loads. J Orthop Res 22:801–806
Waslewski GL, Marson BM, Benjamin JB (1998) Early, incapacitating instability of posterior cruciate ligament-retaining total knee arthroplasty. J Arthroplasty 13:763–767
Masri BA, McCormack RG (1995) The Effect of Knee Flexion and Quadriceps Contraction on the Axial View of the Patella. Clin J. Sport Med 5(1)
Acknowledgments
We to thank DePuy, Germany and Brainlab, Germany for technical and logistical support for this study. Furthermore, we thank the Institute of Anatomy at the Medical University of Graz/Austria, for providing the specimen for this investigation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Additional information
This work was performed at the Department of Orthopedic Surgery at the Medical University of Regensbur/Germany.
Rights and permissions
About this article
Cite this article
Keshmiri, A., Maderbacher, G., Benditz, A. et al. No difference in patellar kinematics between fixed-bearing cruciate-retaining and cruciate-substituting total knee arthroplasty: a cadaveric investigation. International Orthopaedics (SICOT) 40, 731–735 (2016). https://doi.org/10.1007/s00264-015-3041-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3041-y