Abstract
Introduction
Thirteen patients presented with patellofemoral instability out of 3212 knees treated with kinematically aligned total knee arthroplasty (KA TKA) during a nine year period. We determined the clinical characteristics and post-operative radiographic parameters associated with patellofemoral instability, and whether re-operation and patient reported outcome measures are different between patients with and without patellofemoral instability.
Methods
Patients with patellofemoral instability were matched 1:3 to a control cohort based on date of surgery (±3 months), age (±10 years), sex, pre-operative knee deformity (varus or valgus), and implant brand. We analyzed clinical characteristics and seven post-operative radiographic parameters.
Results
Patellofemoral instability presented atraumatically (12 of 13) at 5 ± 4.7 months for a 0.4 % incidence at a mean follow-up of 43 ± 36 months. No pre-operative clinical characteristics were associated with instability. Patients with patellofemoral instability had greater flexion of the femoral component (11° versus 5°; p = 0.0012), a trend toward greater external rotation of the tibial component (2° versus 0°; p = 0.2704), more reoperations (9 versus 0; p = 0.0026) and a lower Oxford Knee Score (36 versus 42; p = 0.0045) than controls.
Discussion
Patellofemoral instability after kinematically aligned TKA is infrequent, presents atraumatically, and is associated with greater flexion of the femoral component than the control group.
Conclusion
Minimizing flexion of the femoral component might reduce the risk of patellofemoral instability by promoting early engagement of the patella in the trochlear during knee flexion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patellofemoral instability results in subluxation and dislocation of the patella, causing pain and functional impairment in patients with native knees or after total knee arthroplasty (TKA) [1]. Patellofemoral complications including anterior knee pain, patellar crepitus, and less frequently patellar subluxation, dislocation, and fracture are causes of patient dissatisfaction and a reason for revision after mechanically aligned TKA [2–4]. The intended setting of the femoral component designed for mechanical alignment is 3° to 5° of external rotation relative to the posterior condylar axis or the transepicondylar axis [5, 6] (Fig. 1).
The composite of a three-dimensional model of the right distal femur shows the coronal (a and b) and axial (c and d) views of a femoral component designed for mechanical alignment set with mechanical alignment (MA) and with kinematic alignment (KA) in 0° of flexion [22]. The setting of the proximal point of the flange of the KA femoral component (orange dot) (b) is in less external rotation than the MA femoral component (blue dot) (a). Use of less external rotation causes a 4 mm increase in the distance between the femoral component and the lateral femur (transverse arrow pointing medial)
Femoral components are designed to maximize the lateral and proximal reach of the trochlea in order to promote early patella engagement during the initiation of knee flexion, restore normal patellar tracking, reduce anterior knee pain, and even the distribution of contact stress on the patella [7, 8]. Flexion of the femoral component is used to downsize the femoral component when the medial-lateral width of the component is wider than the femur and to assist in balancing the flexion gap [9]. Flexion of the femoral component reduces the proximal reach on the anterior surface of the femur [8]. Internal rotation of the femoral component reduces the lateral reach or distance between the lateral edge of the femur and trochlea of the femoral component (Fig. 2 ) [8]. Hence, flexion and internal rotation of the femoral component can compromise engagement of the patella in the trochlea.
The composite of a three-dimensional model of the right distal femur shows a simulation of the mechanically aligned (MA) and kinematically aligned (KA) femoral component set in 0° of flexion (a & b) and the 5 mm (c), 19 mm (d), and 13 mm (e) reductions in proximal reach (arrows pointing distal), and the reductions in femoral component size from flexing the kinematically aligned femoral component from 0° to 5°, 10°, and 15° of flexion [22]
Kinematically aligned TKA has gained interest because two randomized trials and a national multicentre study showed that patients treated with kinematic alignment reported significantly better pain relief, function, flexion, and a more normal feeling knee than patients treated with mechanical alignment [10–12]. Of concern is that kinematic alignment uses a femoral component designed for mechanical alignment and sets the femoral component tangent to the native distal and posterior joint lines that are different from mechanical alignment [13]. Kinematic alignment sets the femoral component in an average of 5° more flexion, 2° more valgus rotation, and 3° less external rotation than mechanical alignment according to one randomized trial [11] (Fig. 1). Although both the kinematically and mechanically aligned treatment groups in the randomized trial had the same 4.5 % incidence of patella-related complications requiring reoperation in the first 2 years, there is a concern that kinematically aligning a femoral component designed for mechanical alignment increases the risk of patellar-femoral instability [13].
In our consecutive series of 3212 knees treated over a nine year period with kinematically aligned TKA, 13 patients presented with patellofemoral instability. Because the clinical and radiographic features of this type of failure has not been reported in the literature, we performed a case–control study and asked two questions: 1) What are the clinical characteristics and post-operative radiographic parameters associated with patellofemoral instability? and 2) Do patients with patellofemoral instability have a higher incidence of reoperation and lower patient reported outcome measures than a matched cohort of patients treated with kinematically aligned TKA without patellofemoral instability?
Methods
Between January 2006 and January 2015 we treated all patients requiring a primary TKA with kinematic alignment and prospectively followed them in our knee replacement registry. The indications for performing TKA were (1) disabling knee pain and functional loss unresolved with nonoperative treatment modalities; (2) radiographic evidence of Kellgren-Lawrence grade 3 or 4 arthritic change or osteonecrosis; (3) any severity of varus or valgus deformity; (4) and any severity of flexion contracture. Patients with prior femoral fracture, tibial fracture, and high tibial osteotomy were included.
With approval of our institutional review board (IRB 796385–1) we 1) identified the implant brand, dates of use, and surgical technique for all kinematically aligned TKAs performed between January 2006 and 2015, 2) identified all patients that presented with patellofemoral instability after TKA (N = 13) (Table 1), and 3) randomly selected a cohort of patients with stable patellofemoral joints and matched them 3:1 to patients with patellofemoral instability based on date of surgery (±3 months), age (±10 years) sex, knee deformity (varus or valgus), and implant brand (Table 2). During this time 3212 primary kinematically aligned TKAs were performed with posterior cruciate retaining implants. There were 837 knees treated with Vanguard CR (Zimmer Biomet, Warsaw, IN), 1391 with Triathlon CR (Stryker, Inc, Mahwah, NJ), 497 with Sigma CR (Depuy, Inc. Warsaw, IN), and 487 with Persona CR (Zimmer Biomet, Warsaw, IN).
Patient-specific instrumentation (PSI) was used in 995 knees (OtisMed Corporation, Alameda, CA, USA) until October 2009 and an evolving technique that used manual instruments was used in 2217 knees that has been previously described [11, 14]. Both surgical techniques used distal and posterior referencing to set varus-valgus and internal-external rotation of the femoral component tangent to the joint lines of the native knee. The patient-specific instrumentation technique used a femoral cutting guide to set the flexion of the femoral component based on three-dimensional pre-operative planning and machining the custom cutting guide. The manual instrument technique used a distal offset cutting block attached to either an extramedullary or a positioning rod inserted 8–10 cm through a hole drilled into the distal femur to set the flexion and varus-valgus of the femoral component (Fig. 4). One implant brand (Persona CR) used either a first or second generation distal offset cutting guide that had either short or long feet, respectively. The first generation guide used a starting hole for the positioning rod just anterior to the notch whereas the second generation guide used a starting hole midway between the top of the intercondylar notch and the anterior cortex. The use of the starting hole just anterior to the notch instead of midway enabled more flexion of the positioning rod and femoral component. The quality assurance step for intra-operatively verifying restoration of the distal and posterior native joint line of the femur was adjustment of the calipered thickness of the distal and posterior femoral resections until they equaled the thickness of the distal and posterior medial and lateral femoral condyles of the femoral component within ± 0.5 mm after compensating for cartilage wear and kerf [11, 15, 16]. Both surgical techniques set the internal-external rotation of the A-P axis of the tibial component parallel to the flexion-extension plane of the extended knee and set the varus-valgus and flexion-extension orientation of the tibial component to restore the native joint line [14, 16]. The manual instrument technique set internal-external rotation of the A-P axis of the tibial component parallel to the major axis of an ellipse drawn on the lateral tibial condyle [14–16]. The balance of the knee and patella tracking were determined qualitatively by manual and visual examination. Varus-valgus instability in full extension was corrected by adjusting the tibial bone resection without release of the collateral, posterior cruciate, or retinacular ligaments [11, 17]. Lateral release was only used in patients with chronic patella subluxation or dislocation prior to TKA. All components were cemented. On the day of discharge an anteroposterior, rotationally controlled, long-leg CT scanogram of the limb was obtained. Beginning in January 2010, axial CT scans of the knee were obtained with use of a previously described technique and were available for nine of 13 patients with patellofemoral instability and 25 of 39 patients in the control group [15, 16, 18].
For each patient with post-operative patellofemoral instability, we recorded the history and clinical presentation, physical examination findings, and non-surgical treatment and operative management from the patient record. A summary of each patient’s instability onset, age, sex, type of instability (dislocation/subluxation), mechanism of onset, implant type, reoperation, clinical outcome, Oxford Knee score (48 is best, 0 is worst), and Forgotten Joint score (100 is best, 0 is worst) are listed in Table 1.
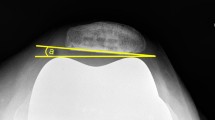
We used the matched cohort of patients to determine the clinical and post-operative radiographic characteristics associated with patellofemoral instability. Eight pre-operative clinical characteristics were compared including age, sex, body mass index (kg/m2), extension, flexion, varus-valgus deformity, Oxford Knee score, Knee Society score (100 is best, 0 is worst), months from date of surgery to follow-up, and incidence of re-operation (Table 2). Seven post-operative radiographic characteristics were compared including flexion-extension of the femoral component, varus-valgus angle of the femoral component to the mechanical and anatomic axis of the femur, hip-knee-ankle angle of the limb, varus-valgus angle of the tibial component to the mechanical axis of the tibia, Insall-Salvati ratio, and internal-external rotation of the tibial component on the femoral component using previously described techniques (Fig. 3) [15–17, 19, 20]. One author (AJN) blinded to the patient group measured each radiographic parameter using previously described and validated techniques with use of image-analysis software (OsiriX Imaging Software, http://www.osirix-viewer.com) [18] (Fig. 3). Two post-operative patient reported outcome measures, (i.e., Oxford Knee score and Forgotten Joint score) obtained at final (Fig. 4).
Composite shows the measurement methods for determining seven radiographic parameters from computer tomographic scanograms and axial views which are: flexion-extension of the femoral component (a), varus-valgus angle of the femoral component to the anatomic and mechanical axis of the femur (b & c), hip-knee-ankle angle of the limb (d), varus-valgus angle of the tibial component to the mechanical axis of the tibia (e), Insall-Salvati ratio (f), and internal-external rotation of the tibial component on the femoral component (g)
Schematic shows the second generation method for minimizing the flexion of the femoral component with use of a distal offset reference guide inserted into the cutting block and passed over a positioning rod for one implant brand (Persona CR). The longer feet of the second generation guide enabled more anterior placement of the starting hole for the positioning rod midway between the top of the intercondylar notch and the anterior cortex rather than at the top of the notch which was used for the first generation with shorter feet. The rod is inserted 8–10 cm through a hole drilled into the metaphysis of the distal femur and set parallel to the anterior femoral shaft and perpendicular to the distal femoral articular surface
Statistical analysis
To quantify reproducibility, two observers (one co-author (AJN) and a senior orthopaedic resident (LH)) independently measured the seven radiographic measurements on ten randomly selected imaging studies. The intraclass correlation coefficient (ICC) was computed for each measurement with use of a two-factor analysis of variance (ANOVA) with mixed effects. The first factor was the observer with two levels (observer 1 and observer 2) and was the fixed effect. The second factor was the scanogram of each of the ten patients with ten levels and was the random effect. An ICC value of > 0.9 indicated excellent agreement, 0.75 - 0.90 indicated good agreement, and 0.5–0.75 indicated moderate agreement [21]. The ICC ranged from 0.89 to 0.97, which indicates good to excellent agreement between the seven radiographic measurements made by two observers independently of the treating physician.
Continuous variables were reported as mean ± standard deviation (SD) or median (range), and discrete variables were reported as number (percentage). To determine whether a clinical and radiographic characteristic was associated with patellofemoral instability we assessed the significance of the difference of each characteristic between the patellofemoral instability and matched cohort groups with either a Student’s T-test for continuous and discrete variables, or a Chi-square test for categorical variables (JMP, 12.1, http://www.jmp.com). Significance was p < 0.05.
Results
Intra-operative assessment of patella tracking at the time of primary kinematically aligned TKA did not detect patellofemoral instability (Table 1). The post-operative onset of patellofemoral instability was atraumatic and occurred at an average of five months. Nine patients had lateral subluxation of the patella that spontaneously reduced after 15–30° of active flexion and did not occur with passive motion. Instability symptoms were most pronounced during stair descent. Three patients had patella dislocation. Nine of 13 patients (70 %) had a patella stabilizing procedure at an average of three months (range, 2–13 months) after the onset of patellofemoral instability, and four were treated with observation. The treatments were open lateral release and medial reefing in six, arthroscopic lateral release in two, and revision of the patellar component with medial reefing in one. The periphery of the patella button was partially covered with soft tissue overgrowth. The ratio of patients with patellofemoral instability per total patients treated with each implant brand was four of 837 Vanguard, one of 1391 Triathlon, one of 497 Sigma, seven of 487 Persona (p = 0.007). The level of patient satisfaction, Oxford Knee score, and Forgotten Joint score varied widely. One patient was deceased and one was lost-to follow-up.
The comparison of the eight preoperative clinical characteristics and incidence of re-operation between the patients with patellofemoral instability and the matched cohort are listed in Table 2. The mean follow-up was 43 months. The only difference was a greater incidence of re-operation in the patients with patellofemoral instability (N = 9) than the patients in the matched cohort (N = 0) (p = 0.0026).
The comparison of the seven post-operative radiographic characteristics and two patient reported outcome scores between the patients with patellofemoral instability and the matched cohort are listed in Table 3. Patients with patellofemoral instability had 2° greater external rotation of the tibial component on the femoral component (mean 2° ± 5.4°, p = 0.2704) that was not significantly different from controls. The only two significant differences were that patients with patellofemoral instability had 6° greater flexion of the femoral component (11° ± 6.2°, p = 0.0012), and a 6 point lower Oxford Knee score (mean 36 ± 7.5, p = 0.0045) than the matched cohort.
Discussion
We performed this case control study to better understand the clinical characteristics and post-operative radiographic parameters associated with patellofemoral instability after kinematically aligned TKA. The most important findings were that patellofemoral instability is infrequent (0.4 %), is associated with flexion of the femoral component averaging 11°, is not associated with internal-external malrotation of the tibial component on the femoral component, presents atraumatically at an average of five months post-operatively, is often treated with a patella stabilizing reoperation, and the final Oxford Knee score averages six points lower than the control cohort.
Three limitations should be discussed that might affect the generalization of the findings. First, the computation of the incidence of patellofemoral instability represents those patients that returned for evaluation and did not include any patients that were treated elsewhere or lost to follow-up. Therefore, our incidence of 0.4 % might be higher. We are unable to compare our 0.4 % incidence to other studies of patients with patellofemoral instability after kinematically or mechanically aligned TKA with a comparative research design because to the best of our knowledge they have not been published. Secondly, it is unknown whether an average of 11° of flexion of the femoral component is associated with patellofemoral instability observed in mechanically aligned TKA. From a geometric perspective, such an association could occur because the reduction in proximal reach caused by flexing the femoral component is similar for kinematic or mechanical alignment [22]. A third limitation was whether the power, based on sample sizes of nine with patellofemoral instability and 25 controls, was adequate to conclude that the 2° greater external rotation of the tibial component in the patellofemoral instability group was not a clinically important difference relative to the control group. The recommended direction for placing the tibial component to minimize the risk of patellofemoral instability is in external rotation rather than internal rotation [23]. A power analysis was performed using a conservative minimal clinically important difference of −7° internal rotation. This difference was chosen based on a report that patients with pain had −6° more internal rotation of the tibial component with no significant difference in the degree of radiographic patellar tilt or patellar subluxation relative to pain-free patients [23]. The 0.9 power computed in the present study using the minimal clinically important difference of −7° internal rotation, sample sizes of 9 and 25, standard deviation of 5.4°, and an alpha of 0.05 was adequate. Paradoxically, the 2° greater external rotation of the tibial component relative to the control group should have decreased the instability risk in the patellofemoral instability group as it was 9° more externally rotated than the minimal clinically important difference of −7° internal rotation. Based on this analysis, the 2° greater external rotation of the tibial component on the femoral component was unlikely the cause of patellofemoral instability.
The analysis of the presentation of patellofemoral instability after kinematically aligned TKA and treatment provide insights and guidelines for understanding and managing this uncommon and challenging complication. Intra-operative assessment of patellofemoral tracking at the time of kinematically aligned TKA and at the time of re-operation often failed to detect the instability. The average onset at five months, the initiation of the instability by an atraumatic mechanism, and the instability caused by active and not passive flexion suggests that a change in the congruency of the patellofemoral joint rather than with a change in the peripatellar muscle balance might be a factor associated with the instability. The development and maturation of soft-tissue overgrowth on the periphery of the patella button might be such a mechanism. Unfortunately, treatment with observation or re-operation with a lateral release with or without medial reefing did not always eliminate the instability. Although the instability may persist, reoperation mitigated the symptoms as a mean Oxford Knee score of 36 was self-reported by the 11 patients available for follow-up, which is comparable to scores of 34 and 37 reported for mechanically aligned TKA at two years by registries in the United Kingdom and New Zealand, respectively [24, 25].
The analysis of eight preoperative clinical characteristics, and seven post-operative radiographic characteristics identified flexion of the femoral component averaging 11° as a controllable variable associated with patellofemoral instability after kinematically aligned TKA. Flexion of the femoral component occurred in patients treated with patient-specific and manual instrumentation. The incidence of patellofemoral instability was greater in patients with one (Persona CR) implant brand that relied on manual instruments. We attribute this to the use of the first generation distal offset referencing guide with short feet that required a starting hole for the positioning rod just anterior to the intercondylar notch whereas the second generation guide used a starting hole midway between the top of the intercondylar notch and the anterior cortex. The use of the starting hole anterior to the notch instead of midway enabled more flexion of the femoral component. Hence, the higher incidence of patellofemoral instability with one implant brand (Persona CR) was more likely associated with the use of the first generation of manual instrumentation enabling greater flexion of the femoral component than implant design. Accordingly, we have used the starting hole midway between the top of the intercondylar notch and the anterior cortex and the distal referencing guide with long feet to reduce the risk of flexion of the femoral component in 715 consecutive patients treated with the Persona implant in addition to the cohort of 487 patients in the present study. None of these 715 patients have presented to our clinic with patellofemoral instability after performing kinematically aligned TKA.
Malrotation of the femoral or tibial components from the intended targets is another cause of patellofemoral instability. The rotational target for the femoral component in kinematic alignment is tangent to the native posterior joint line. The use of the quality assurance step of adjusting the calipered thickness of the distal and posterior femoral resections until they equaled the thickness of the distal and posterior medial and lateral femoral condyles of the femoral component within ± 0.5 mm after compensating for cartilage wear and kerf reliably sets rotation [11, 15, 16]. The reported range of malrotation of the kinematically aligned femoral component is small from −3° internal to 2° external from tangent to the native joint line, which is four to five times narrower than the range of malrotation of mechanical alignment of the femoral component of −11° internal to 16° external rotation to the transepicondylar axis, −12° internal to 15° external rotation to the A-P axis of the trochlear groove, and −10° internal to 12° external rotation to the line 3° externally rotated from the posterior condylar line [6, 16]. The rotational target for the tibial component in kinematic alignment is parallel to the flexion-extension plane of the knee [11, 15, 16]. Since kinematic alignment reliably sets the rotation of the femoral component tangent to the native posterior joint line, and since the present study showed that the rotation of the tibial component on the femoral component was not different between the nine of 13 patients in the patellofemoral instability group and the 25 of 39 patients in the control groups that had axial CT scans, malrotation of the femoral and tibial components was not a likely cause of patellofemoral instability.
In summary, limiting flexion of the femoral component might lower the risk of patellofemoral instability, lower the incidence of reoperation, and improve the mean Oxford Knee score after kinematically aligned TKA.
References
de Oliveira V, de Souza V, Cury R, Camargo OP, Avanzi O, Severino N, Fucs P (2014) Medial patellofemoral ligament anatomy: is it a predisposing factor for lateral patellar dislocation? Int Orthop 38(8):1633–1639. doi:10.1007/s00264-014-2357-3
Aglietti P, Buzzi R, Gaudenzi A (1988) Patellofemoral functional results and complications with the posterior stabilized total condylar knee prosthesis. J Arthroplasty 3(1):17–25
Patel J, Ries MD, Bozic KJ (2008) Extensor mechanism complications after total knee arthroplasty. Instr Course Lect 57:283–294
Petersen W, Rembitzki IV, Bruggemann GP, Ellermann A, Best R, Koppenburg AG, Liebau C (2014) Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop 38(2):319–328. doi:10.1007/s00264-013-2081-4
Mahfouz MR, ElHak Abdel Fatah E, Bowers L, Scuderi G (2015) A new method for calculating femoral anterior cortex point location and its effect on component sizing and placement. Clin Orthop Relat Res 473(1):126–132. doi:10.1007/s11999-014-3930-1
Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ (2005) The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am 87(10):2276–2280. doi:10.2106/JBJS.D.02945
Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT (1993) The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res 287:170–177
Brar AS, Howell SM, Hull ML (2016) What are the bias, imprecision, and limits of agreement for finding the flexion-extension plane of the knee with five tibial reference lines? Knee 23(3):406–411. doi:10.1016/j.knee.2016.01.005
Tsukeoka T, Lee TH (2012) Sagittal flexion of the femoral component affects flexion gap and sizing in total knee arthroplasty. J Arthroplasty 27(6):1094–1099. doi:10.1016/j.arth.2011.10.015
Calliess T, Bauer K, Stukenborg-Colsman C, Windhagen H, Budde S, Ettinger M (2016) PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study. Knee Surg, Sports Traumatol, Arthrosc: Off J ESSKA. doi:10.1007/s00167-016-4136-8
Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG (2014) A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J 96-B(7):907–913. doi:10.1302/0301-620X.96B7.32812
Nam D, Nunley RM, Barrack RL (2014) Patient dissatisfaction following total knee replacement: a growing concern? Bone Joint J 96-B(11 Supple A):96–100. doi:10.1302/0301-620X.96B11.34152
Ishikawa M, Kuriyama S, Ito H, Furu M, Nakamura S, Matsuda S (2015) Kinematic alignment produces near-normal knee motion but increases contact stress after total knee arthroplasty: a case study on a single implant design. Knee 22(3):206–212. doi:10.1016/j.knee.2015.02.019
Howell SM, Papadopoulos S, Kuznik KT, Hull ML (2013) Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg, Sports Traumatol, Arthrosc: Off J ESSKA 21(10):2271–2280. doi:10.1007/s00167-013-2621-x
Nedopil AJ, Howell SM, Rudert M, Roth J, Hull ML (2013) How frequent is rotational mismatch within 0 degrees +/−10 degrees in kinematically aligned total knee arthroplasty? Orthopedics 36(12):e1515–e1520
Nedopil AJ, Howell SM, Hull ML (2016) Does malrotation of the tibial and femoral components compromise function in kinematically aligned total knee arthroplasty? Orthop Clin North Am 47(1):41–50. doi:10.1016/j.ocl.2015.08.006
Howell SM, Papadopoulos S, Kuznik K, Ghaly LR, Hull ML (2015) Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop 39(11):2117–2124. doi:10.1007/s00264-015-2743-5
Howell SM, Kuznik K, Hull ML, Siston RA (2010) Longitudinal shapes of the tibia and femur are unrelated and variable. Clin Orthop Relat Res 468(4):1142–1148. doi:10.1007/s11999-009-0984-6
Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG (2012) Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics 35(2):e160–e169. doi:10.3928/01477447-20120123-04
Nelitz M, Dreyhaupt J, Williams SR, Dornacher D (2015) Combined supracondylar femoral derotation osteotomy and patellofemoral ligament reconstruction for recurrent patellar dislocation and severe femoral anteversion syndrome: surgical technique and clinical outcome. Int Orthop 39(12):2355–2362. doi:10.1007/s00264-015-2859-7
Indrayan A (2013) Methods of Clinical Epidemiology. In: SARDaGMW (ed) Springer series on epidemiology and public health. Springer, Berlin, p 24. doi:10.1007/978-3-642-37131-8_2
Brar AS, Howell SM, Hull ML, Mahfouz MR (2016) Does kinematic alignment and flexion of a femoral component designed for mechanical alignment reduce the proximal and lateral reach of the trochlea? J Arthroplasty. doi:10.1016/j.arth.2016.01.040
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 392:46–55
The New Zealand Joint Registry (2013) The New Zealand Joint Registry 14 year report: January 1999 to December 2012
Williams DP, Blakey CM, Hadfield SG, Murray DW, Price AJ, Field RE (2013) Long-term trends in the Oxford knee score following total knee replacement. Bone Joint J 95-B(1):45–51. doi:10.1302/0301-620X.95B1.28573
Acknowledgments
We wish to thank Lukas Haug, MD for measuring the radiographic measurements used to compute the intraclass correlation coefficients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Funding
There is no funding source.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors (institutional review board (IRB 796385–1)).
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Nedopil, A.J., Howell, S.M. & Hull, M.L. What clinical characteristics and radiographic parameters are associated with patellofemoral instability after kinematically aligned total knee arthroplasty?. International Orthopaedics (SICOT) 41, 283–291 (2017). https://doi.org/10.1007/s00264-016-3287-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3287-z