Abstract
Background
The aim of this study was to identify, during total knee arthroplasty surgery, the effect on patellar kinematics of different patellar component designs in the same patients.
Methods
This study enrolled 84 patients with osteoarthritis. Intraoperative X-rays were used to measure internal rotation angle, flexion angle and lateral tilt were at different knee flexion angles with dome-type or anatomic-type patellar components (ATTUNE®, DePuy).
Results
Significant differences from baseline between the two types of components occurred at 120° of the knee flexion in the internal rotation angle, at 90° and 120° of the knee flexion in the flexion angle, and at 60° of the knee flexion in the lateral tilt.
Conclusion
This study revealed that the difference in patellar component design affects patellar kinematics. Therefore, the difference in patellar component design may affect patellar stability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patellofemoral complications after total knee arthroplasty (TKA) have become a major problem, increasing the risk for patellar instability, dislocation, loosening, wear and residual patellofemoral pain [1,2,3,4,5,6]. Patellofemoral complications following TKA are a common cause of patent dissatisfaction. We have been performing routine patellar surfacing, which is commonly recommended in TKA [7, 8].
Patellar motions from extension to flexion are influenced by the geometry of the femoral condyles, the femorotibial angle, the balance of the medial and lateral components of the quadriceps and the design of TKA components [9,10,11,12]. The component design and material choice for TKA appear to affect knee performance, survival rate of the components and potential complications. Dome, offset dome, modified dome and anatomic are commonly used types of patellar component design configurations. Medialization during installation of patellar component does not require lateral retinacular release [13]. In a previous review, an eccentrically shaped dome or an anatomic low contact stress device patellar component was preferred [14]. However, it is controversial which patellar component design is better for patellar kinematics when performing TKA with patellar resurfacing. In TKA, patellar tracking was often checked using trial patellar components. Evaluation of patellar kinematics is needed to confirm patellar tracking. We hypothesize that differences in patellar component designs influence patellar kinematics even when used with the same femoral and tibial components. Previous studies of patellar kinematics used cadavers or models of the patellofemoral joint for evaluation [11, 12]. The purpose of this study is to identify, during TKA surgery, the effect of different patellar component designs on patellar kinematics within the living body of the same patients.
Materials and methods
Patients
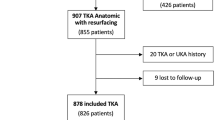
We prospectively enrolled 84 patients (84 knees) with osteoarthritis who underwent TKA by the same surgeon in our hospital. All patients provided written informed consent before enrollment in this trial. The inclusion criteria for this study included patients who were able to walk and fulfilled the criteria for knee osteoarthritis (OA) of the medial femorotibial joint. All patients had radiographic OA with Kellgren–Lawrence grade 2 to 4 evaluated by anteroposterior X-rays in the standing position [15]. The exclusion criteria included patients who had bilateral TKA or who had undergone joint arthroplasty in the hip and/or ankle joint.
We conducted this study following the principles of the Declaration of Helsinki. Informed consent was obtained from all patients. This research has been approved by the Institutional Review Board of the authors’ affiliated institutions.
Surgical technique
A standard TKA was performed using the ATTUNE® Total Knee Posterior Stabilized System® (DePuy Synthes, USA). All TKAs were performed using a medial parapatellar approach. Distal femoral resection uses anatomic landmarks and plane X-rays to match the degree of normal femoral external rotation. For anterior and posterior femoral resections, the degrees of external rotation were determined using the posterior condylar axis and the trans-epicondylar axis by preoperative magnetic resonance imaging. For proximal tibial resection, the landmarks were the posterolateral and medial tibial plateaus. Tibial rotation was determined to by inserting an implant to ensure a midline tibial articulation. The cutting thickness of the patella necessary to maintain patellar thickness after cutting was measured using a vernier caliper before cutting. The usual amount of bone resection was equal to the thickness of the patellar component to be used. The patellar thickness was checked using a vernier caliper after cutting.
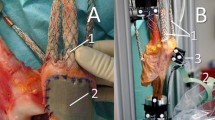
In the ATTUNE KNEE SYSTEM®, the patellar components have a medialized dome patella and medialized anatomic patella. The medialized dome type is offset by 3 mm medially (Fig. 1a, b). The medialized anatomic type is offset by 3 mm medially, a conforming lateral facet and a domed medial facet (Fig. 1c, d).
Intraoperative radiological data
After cutting femur, tibia and patella, the trial components and insert were installed. Subsequently, Kirschner wire was punctured into the patella and the capsule was sutured. The internal rotation angle, flexion angle and lateral tilt were measured intraoperatively during TKA surgery using offset dome-type and anatomic-type trial patellar components. We first measured the dome type of patellar trial component by intraoperative radiology. Then, the patellar trial component was changed to the anatomic type and measured in the same way. The knee flexion angles were measured using a goniometer.
The types of patellar component designs for measuring patellar kinematics have been described previously [16]. The internal rotation angle (Fig. 2a) was measured on frontal view X-rays with the knee in extension (baseline) and with 30°, 60°, 90° and 120° of knee flexion. The rotation angle is the angle between the box line in the femoral component and the Kirschner wire. The flexion angle (Fig. 2b) is measured on lateral view X-rays with the knee in extension (baseline) and with 30°, 60°, 90° and 120° of knee flexion. The flexion angle is the angle between the cutting surface of the patella and anterior cutting surface of the femur. Lateral tilt (Fig. 2c) was measured on skyline view X-rays in 30° (baseline) of knee flexion and with 60°, 90° and 120° of knee flexion. The lateral tilt is the angle between the cutting surface of the patella and a bi-condylar line across the femoral component.
Statistical analysis
The outcome measures were changes in internal rotation angle, flexion angle and lateral tilt from baseline at each angle of knee flexion. Comparisons of the changes in these measures between the dome-type group and anatomic-type components were made using paired t-tests. Statistical analyses were performed using the R software package (http://www.r-project.org/). p < 0.05 was considered to be statistically significant.
Results
The population included 12 men and 72 women, aged 74.1 ± 8.4 years. The valgus angle and external rotation angle of the femoral component were 6.3 ± 0.7° and 4.1 ± 0.9°, respectively.
Changes from baseline in the internal rotation angle of the dome and anatomic types were 0.38 ± 3.24 and − 0.07 ± 3.86° at 30° of knee flexion (p = 0.410), − 0.10 ± 4.60 and 0.03 ± 5.16° at 60° of the knee flexion (p = 0.871), 0.03 ± 6.85 and 0.12 ± 6.11° at 90° of knee flexion (p = 0.925) and 1.71 ± 6.82 and − 0.33 ± 6.09° at 120° of knee flexion (p = 0.042), respectively (Fig. 3a). Changes from baseline in the flexion angle of the dome and anatomic types were 15.2 ± 11.5 and 13.8 ± 12.1° at 30° of knee flexion (p = 0.429), 27.9 ± 12.2 and 25.7 ± 14.6° at 60° of knee flexion (p = 0.296), 40.4 ± 14.9 and 34.9 ± 16.8° at 90° of knee flexion (p = 0.026) and 53.4 ± 16.9 and 44.8 ± 19.8° at 120° of knee flexion (p = 0.003), respectively (Fig. 3b). The changes from baseline in the lateral tilt of the dome and anatomic types were 3.02 ± 6.16 and 0.80 ± 3.69° at 60° of knee flexion (p = 0.009), 3.66 ± 8.47 and 1.77 ± 4.97° at 90° of knee flexion (p = 0.104) and 4.60 ± 8.75 and 2.50 ± 5.26° at 120° of knee flexion (p = 0.082), respectively (Fig. 3c).
Discussion
This clinical study examined the influence on the patellar kinematics of two different patellar component designs in the same patients during surgery. The change of internal rotation angles from baseline nearly reached a plateau at 30°, 60° and 90° of knee flexion for both types of components. However, at 120° of knee flexion, the change of the internal rotation angle with the dome type was much greater than for the anatomic type. The flexion angles of the patella increase as the knee flexes when using either the dome-type or anatomic-type design. However, the change of flexion angles from baseline was significantly less with the anatomic-type component than with the dome type at 90° and 120° of knee flexion. The lateral tilt of the patella with the dome-type component was unstable, but lateral tilt was stable with the anatomic-type component. Therefore, differences in patellar component design affect patellar kinematics.
Patellar kinematics is also affected by various factors such as position of the femoral, tibial and patellar components, the joint line and quadriceps force. Specifically, patellar resurfacing and thickness may influence patellar kinematics. In a cadaver study using middle-aged donors, the influence of patellar thickness on patellar rotation and patellar flexion was not significant when 8–12 mm of the patella was resected. On the other hand, in the intact cadaver knee, patellar internal rotation was increased through 0°–75° of knee flexion and plateaued through 75°–105° of flexion. Patellar flexion increased through 0°–105° of knee flexion. Patellar medial tilt increased though 0°–15° of knee flexion, decreased to about baseline at 15°–45° of knee flexion and plateaued near baseline from 45°–105° of knee flexion [16]. In cadaveric knees, the lateral translation of the patella increased when knee flexion exceeded 30° [17]. This result was similar to the results with both types of component used in this study. However, lateral tilt of the dome type was large compared with that of the anatomic type of component. This result demonstrates that the dome type had larger medial and lateral contact area than the anatomic type of component [18]. Based on our results in the patient knee, patellar rotation with the anatomic-type component is more similar to the intact cadaver knee than the dome-type component. Patellar flexion in both types of component is similar to the intact cadaver knee, whereas patellar tilt deviates from the intact cadaver knee for both types of components.
The anatomic type of patellar component is square and thick from proximal to distal and has a conforming lateral facet and a domed medial facet. We hypothesize that the lateral facet is related to medial–lateral stability, and the thickness from proximal to distal is related to flexion stability. In previous reports using a dynamic finite element model of the patellofemoral joint [18, 19], the kinematics of the patella in rotation and flexion were similar to our results for both dome and anatomic types of component. However, there were slight differences in lateral tilt reported previously and in this study for each angle of knee flexion. We assume that the difference in muscle tension between the living body and the assumptions made in the dynamic finite element model is responsible for the difference in the results.
This study has some limitations. First, the sample size is small, so larger samples are needed to evaluate a more exact relationship between patellar kinematics and the differences in patellar component design. The differences of groove design in the femoral component and patellar component design both affect stress distribution [20]. Therefore, in the future, clinical outcomes will be necessary for improved evaluations of patellar component design. Second, intraoperative radiological measurements were performed with the patient under general anesthesia. Therefore, the results of this study are not necessarily the same as those that might occur during daily activity. Despite these limitations, our study is the first to evaluate intraoperatively the relationship between patellar kinematics and differences in patellar component design in the same patient.
In conclusion, this study revealed that differences in patellar component design affect patellar kinematics. Therefore, different patellar component designs may affect patellar stability. We believe that the ideal design of the patellofemoral articulation still is not known. We hope these results clarify the pathomechanics of the patellofemoral joint after TKA and will inform the choice of patellar component used in TKA.
References
Merkow RL, Soudry M, Insall JN (1985) Patellar dislocation following total knee replacement. J Bone Jt Surg Am 67:1321–1327
Roffman M, Hirsh DM, Mendes DG (1980) Fracture of the resurfaced patella in total knee replacement. Clin Orthop Relat Res 148:112–116
Clayton ML, Thirupathi R (1982) Patellar complications after total condylar arthroplasty. Clin Orthop Relat Res 170:152–155
Healy WL, Wasilewski SA, Takei R, Oberlander M (1995) Patellofemoral complications following total knee arthroplasty. Correlation with implant design and patient risk factors. J Arthroplasty 10:197–201
Figgie HE 3rd, Goldberg VM, Heiple KG, Moller HS 3rd, Gordon NH (1986) The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Jt Surg Am 68:1035–1040
Aglietti P, Buzzi R, Gaudenzi A (1988) Patellofemoral functional results and complications with the posterior stabilized total condylar knee prosthesis. J Arthroplasty 3:17–25
Boyd AD Jr, Ewald FC, Thomas WH, Poss R, Sledge CB (1993) Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Jt Surg Am 75:674–681
Dalury DF, Dennis DA (2003) Extensor mechanism problems following total knee replacement. J Knee Surg 16:118–122
Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M (2001) Early failures in total knee arthroplasty. Clin Orthop Relat Res 392:315–318
Abraham W, Buchanan JR, Daubert H, Greer RB 3rd, Keefer J (1998) Should the patella be resurfaced in total knee arthroplasty? Efficacy of patellar resurfacing. Clin Orthop Relat Res 236:128–134
Ewald FC, Jacobs MA, Miegel RE, Walker PS, Poss R, Sledge CB (1984) Kinematic total knee replacement. J Bone Jt Surg Am 66:1032–1040
Saffarini M, Zaffagnini S, Bignozzi S, Colle F, Marcacci M, Dejour D (2015) Does patellofemoral geometry in TKA affect patellar position in mid-flexion? Knee Surg Sports Traumatol Arthrosc 23:1799–1807
Brilhault J, Ries MD (2010) Measuring patellar height using the lateral active flexion radiograph: effect of total knee implant design. Knee 17:148–151
Yoshii I, Whiteside LA, Anouchi YS (1992) The effect of patellar button placement and femoral component design on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 275:211–219
Chew JT, Stewart NJ, Hanssen AD, Luo ZP, Rand JA, An KN (1997) Differences in patellar tracking and knee kinematics among three different total knee designs. Clin Orthop Relat Res 345:87–98
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Hsu HC, Luo ZP, Rand JA, An KN (1996) Influence of patellar thickness on patellar tracking and patellofemoral contact characteristics after total knee arthroplasty. J Arthroplasty 11:69–80
Fitzpatrick CK, Baldwin MA, Clary CW, Wright A, Laz PJ, Rullkoetter PJ (2012) Identifying alignment parameters affecting implanted patellofemoral mechanics. J Orthop Res 30:1167–1175
Abo-Alhol TR, Fitzpatrick CK, Clary CW, Cyr AJ, Maletsky LP, Laz PJ et al (2014) Patellar mechanics during simulated kneeling in the natural and implanted knee. J Biomech 47:1045–1051
Huang CH, Hsu LI, Chang TK, Chuang TY, Shih SL, Lu YC et al (2017) Stress distribution of the patellofemoral joint in the anatomic V-shape and curved dome-shape femoral component: a comparison of resurfaced and unresurfaced patellae. Knee Surg Sports Traumatol Arthrosc 25:263–271
Author information
Authors and Affiliations
Contributions
TM, KI and KO designed the research. TM and RH participated in the operations and data collection. KY performed the statistical analysis. KI and KO participated in the editing and submission of the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mochizuki, T., Yano, K., Ikari, K. et al. Effect on patellar kinematics of the different patellar component designs in total knee arthroplasty: intraoperative measurement of dome type versus anatomic type. Eur J Orthop Surg Traumatol 30, 419–424 (2020). https://doi.org/10.1007/s00590-019-02586-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02586-1