Abstract
In the past 30 years there have been major improvements in the care of children with chronic kidney disease (CKD). The incidence and prevalence of CKD vary among published studies reflecting both epidemiological differences between countries and regions, differences in case definition and the lack of population-based studies on CKD in many part of the world, where CKD incidence is likely underestimated. Congenital disorders, including congenital anomalies of the kidney and urinary tract (CAKUT) and hereditary nephropathies, are responsible for about two thirds of all cases of CKD in developed countries while acquired causes predominate in developing countries. Most young children starting dialysis, begin on peritoneal dialysis, while older children start with hemodialysis. The predominant renal replacement modality among prevalent patients, particularly in high-income countries, is renal transplantation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Irreversible kidney damage or so-called chronic kidney disease (CKD) has become a major public health problem worldwide. The adult population has been the subject of extensive epidemiological research [1, 2] but fewer data are available about CKD in children [3]. Despite major scientific advances resulting in substantial improvement in the care of children with CKD, some will still progress and require kidney replacement therapy (KRT). ESKD is a devastating disorder causing substantial mortality and morbidity (most notably cardiovascular, cancer and infection), but this is compounded by specific problems which occur in children such as impaired growth and psychosocial adjustment [4], all of which severely impact upon quality of life [5]. Understanding of the epidemiology of CKD in children is required in order to make a precise and early diagnosis, identify preventable or reversible causes of progression, predict prognosis, and aid the counseling of children and their families.
Part I: CKD (Stages I–4)
Definition of CKD
Precise data on the epidemiology of CKD in children allowing the evaluation of the incidence and prevalence of CKD and the comparison between countries is lacking. This was in part due to the lack of a universal definition of CKD. For example, the ItalKid Project and North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS) defined CKD as having a glomerular filtration rate (GFR) of below 75 mL/min/1.73 m2 [6, 7]. Others based their definition on serum creatinine levels themselves or on other thresholds of GFR [8,9,10]. In 2002, the National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative (NKF-K/DOQI) published a classification of CKD applicable to children [11]. CKD was defined by the persistence for more than 3 months of morphological, histological or biological abnormalities of the kidneys and/or a glomerular filtration rate (GFR) below 90 mL/min/1.73 m2. This classification grades CKD in five stages from stage 1 with normal GFR to end-stage kidney disease (ESKD, stage 5). The K/DOQI classification was revised in 2012 by the KDIGO (Kidney Disease: Improving Global outcomes) to reflect the risk of progression to ESKD and is based on both GFR and albuminuria [12]. Of note, some pediatric specificities need to be considered when using this classification: a) the criteria for duration >3 months does not apply to newborns or infants <3 months of age, (b) the criteria of a GFR <90 mL/min/1.73 m2 does not apply to children <2 years of age as neonates are born with lower GFR, which increases to normal values in the first 2 years of life, (c) a urinary total protein or albumin excretion rate above the normal value for age may be substituted for albuminuria ≥30 mg/24 h. A similar classification based on the same GFR cut-offs and on the urine protein-creatinine ratio and specifically validated in two large pediatric cohorts (CKID in the USA and ESCAPE in Europe) has been developed recently (Fig. 54.1; Table 54.1) [13].
The new classification was widely adopted after its introduction; however, its limitations and possible modifications have been a matter of extensive discussions. Moreover, despite efforts to standardize creatinine measurement (by using enzymatic methods instead of colorimetric methods) and GFR estimation, there are still ongoing debates on which eGFR equation should be used in various clinical conditions particularly in early stages of kidney injury [14,15,16,17]. In 2009, the bedside Schwartz formula using height and serum creatinine and a unique k coefficient was developed and remains frequently used in clinical practice [18]. Since then many equations have been published using serum creatinine or cystatine C or a combination of both. Recently, papers focused on developing formulas that perform consistently over the whole range of GFR from infants to young adults (FAS [19], CKID U25 [20]).
Screening for CKD
CKD screening and surveillance in adults, either population-based or targeted at risk populations, has become widely advocated and implemented in many countries worldwide, in an attempt to prevent ESKD and the progression of CKD. However, the benefit of screening for early-stage CKD is uncertain [21]. The benefit of such programs in children is even more uncertain [22]. Tests used for CKD screening in children are usually limited to urinary dipstick protein instead of urine albumin/creatinine ratio or on creatinine-based calculation of estimated GFR as recommended for adults. There is also a large variation in the methods used and approaches taken by the different countries, and the findings have shown poor reproducibility [22].
The main studies about screening for CKD in children are summarized in Table 54.2 [23,24,25,26,27,28,29,30,31,32,33,34]. Mass screening programs to detect CKD in children have been undertaken for many years in several Asian countries such as Japan, Taiwan and Korea [23,24,25]. Conversely, screening programs have not been adopted in Europe or Australia but screening using urine dipsticks have routinely been performed in healthy children for decades in the United States. In 2000, the recommendations from the American Academy of Pediatrics were to screen the urine of preschool children and adolescents [35]. This policy has been revised in 2007 and this practice is no longer recommended [36]. Although a decrease in the incidence of ESKD has been observed in Japan and Taiwan, there is only limited evidence that early detection of kidney injury in children may lead to effective interventions to slow progression of CKD and further reduce the risk of developing ESKD [22]. Furthermore, some studies suggest that a urine dipstick is not a cost-effective strategy for screening in children [37] given the high prevalence of transient proteinuria in this population. Although some population-based studies assessing CKD epidemiology by GFR estimation have been performed and indicate that a certain proportion of asymptomatic children have CKD, no systematic national screening program based on GFR assessment in children is currently ongoing.
Demographics of CKD
There is limited information on the epidemiology of early stages of CKD in children. As CKD is usually asymptomatic in its early stages, providing precise epidemiological data is difficult so CKD in children is likely to be underestimated and underreported. Although some pediatric CKD registries using the K/DOQI classification are beginning to emerge, only a few reports on the epidemiology of CKD stages 2–5 in children are available. Due to lack of resources and national renal registries, we know even less about the incidence and prevalence in low income countries. For these countries, data are mostly obtained from reports of major tertiary care referral centers, but the validity of this data is variable.
Europe
The largest population-based study in Europe on the epidemiology of pediatric CKD is the ItalKid project. This study in Italy has been collecting data since 1990 on the epidemiology of childhood CKD, describing the natural history of the disease, and identifying factors that influence its course [6]. So far, nearly 1198 patients have been registered. Other nation-wide European studies are the Serbian CKD registry [38], collecting data on over 336 patients since 2000, the Belgium CKD registry which started in 2001 and has over 143 patients [39], and the data from the Swedish Pediatric Nephrology Association [40]. Also regional studies have taken place in Spain [41], the South-East of the UK [42] and Lorraine in France [8].
Several pediatric nephrology societies from European countries have provided data on the early stages of CKD. Even though age categories and definition of CKD differed between countries, incidence in Europe was consistent, ranging from 8 to 14 per million age-related population (pmarp) for CKD stages 2–5, and being around 8 pmarp for CKD stage 4–5 (Fig. 54.1). The incidence was highest (17.5 pmarp) in a report from the United Kingdom but the study was hospital-based leading to potential referral filter bias and there may be some uncertainty about the covered geographical area [42].
While an increase in incidence since the 1970s was seen in France [8], this was not seen when comparing two time periods in Sweden [9, 40]. Two studies from Serbia and the UK also suggested an increase in incidence in the past 10 years [38, 42]. Prevalence ranged from about 55–60 to 90–95 pmarp in Spain, Italy, UK and Serbia, depending on the clinical definition of CKD that was used in each study.
In Turkey, the CREDIT study reported a prevalence of CKD stage 3–5 of 2600 pmarp in children aged 5–18 years old in 2007 [43].
North America
In Northern America most of the information on CKD in children derives from two large sources of information namely the North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS) [44] and the Chronic Kidney Disease in Children Prospective Cohort Study (CKiD) [45]. Both studies are collecting data on a voluntary basis and are not population based.
Population-based data are available in adolescents since the NHANES study investigated albuminuria and GFR in a nationally representative sample of the US population including 9225 adolescents aged 12–18 years over 3 study periods. They found a prevalence of 0.91% [95% CI 0.58–1.42%] for CKD stage 3–5 and a prevalence of persistent albuminuria of 3.29% [95% CI 1.94–4.63%] in the 2009–2014 survey [28].
Latin America and the Caribbean
In Chile, a national survey of pediatric nephrologists estimated an incidence of CKD (GFR <30 mL/min/1.73 m2) in children aged less than 18 years of 5.7 pmarp and a prevalence of 42.5 pmarp in 1996 [46]. Among these patients, half were on conservative treatment and the others were on KRT. Very similar results were found in Argentina, with an incidence of 6.5 pmarp, but with a lower prevalence (15.4 pmarp) [47]. Fifty-eight percent of this population had ESKD and started with dialysis. In Jamaica, the estimated incidence of CKD was 4.6 pmarp and 28% of them were already in ESKD, without having access to KRT [48].
A study on the epidemiology of CKD conducted in several Latin American countries (Argentina, Brazil, Chile, Colombia, Mexico, Uruguay, and Venezuela) has shown a wide variation in incidence that ranged from 2.8 to 15.8 new cases pmarp [49]. Also an indirect estimation of the incidence of CKD in Mexico suggested a very high incidence, between 24 and 39 per million inhabitants, for which the differences within Mexico were explained by the level of social deprivation [50].
Asia
The estimated prevalence of CKD stage 3–5 among Japanese children in 2010 was 29.8 pmarp [51]. This lower prevalence of pre-dialysis CKD in Japan than in Europe was consistent with the lower prevalence of pediatric ESKD in Japan. Two reports from Vietnam and one from Thailand have suggested an annual incidence of hospitalization for CKD around 5 pmarp, most of patients had already reached ESKD [52,53,54]. Very little is known about pediatric CKD epidemiology in India and China. A survey conducted in 91 Chinese hospitals found a total of 1658 children aged <15 years with CKD stage 3–5 between 1990 and 2002 which suggests a very low incidence of treated CKD <0.5 pmarp [55]. Patients were referred late with advanced CKD or ESKD in 80% and in-hospital mortality was as high as 72%. Similarly, in India 58% of children had ESKD at the time of CKD diagnosis suggesting that children with CKD are underdiagnosed and referred late [55].
Middle East
The referral center for pediatric kidney diseases in Kuwait provided data on children aged 0–15 years with a GFR <50 mL/min/1.73 m2 [10]. The mean incidence was found to be as high as 38 pmarp whereas the prevalence increased from 188 in 1996 to a rate as high as 329 pmarp in 2003. The marked difference in incidence between Kuwaiti children and non-Kuwaiti residents suggested the role of genetic factors. An incidence of 12 pmarp was found in a Turkish survey including children with a GFR <75 mL/min/1.73 m2 [56]. An incidence of 11 pmarp and a prevalence of 51 pmarp have been reported in Jordanian children [57].
Africa
Single center studies from sub-Saharan Africa showed very low incidence of CKD estimated at 1–4 pmarp in Nigeria, Sudan, and South Africa [58,59,60,61]. Another single center report from Nigeria, however, found an annual incidence of CKD stage 1–5 of 11 pmarp and a prevalence of 48 pmarp [62], which was much higher than the 1.7 pmarp reported in 2004 [63].
Causes of CKD
Type 2 diabetes and hypertension are the leading causes of CKD in adults. The distribution of the causes of CKD in children are very different with major variations between countries. Indeed, congenital abnormalities of the kidney and the urinary tracts (CAKUT) account for 50–60% of CKD cases in children in Europe [6, 38, 39, 42], Japan [51] and the USA [44]. In Turkey and in the Middle East, CAKUT remains the first cause of CKD with often a higher proportion of hereditary nephropathies related to higher rates of consanguinity [10, 56, 57, 64]. Higher proportions of glomerular diseases are found in developing countries such as India, Southeast Asia [52,53,54], Latin America [48, 49] and Sub-Saharan Africa [58]. The latter may be related to the high prevalence of bacterial, viral and fungal infections in these regions.
Whereas CAKUT predominates in younger patients, glomerulonephritis is the leading cause in children older than 12 years of age. Causes of CKD vary across races, for example, focal segmental glomerulosclerosis, the main cause of glomerular disease, is three times more common in blacks than in whites (19 compared with 6%) and especially among black adolescents (35%) [65].
In general, there is a predominance of male gender (male/female ratio ranging from 1.3 to 3.0). This partly reflects the higher incidence of CAKUT in boys than in girls, but has also been reported in the regions with a high rate of glomerulonephritis.
Part II: KRT (CKD Stage 5D and 5 T)
Epidemiological data on ESKD treated by dialysis or transplantation is more robust thanks to the development of several national and international registries. Unfortunately not every country has such a registry, not all children are reported to the relevant registry, and some countries with registries do not regularly publish reports. Also, as KRT is expensive not all countries are able to offer KRT to children with ESKD. Approximately 80% of the children on KRT live in Europe, Japan or the United States. Dialysis and transplant registries only collect data on treated ESKD; untreated children with ESKD are not captured. However, at least in the developed world, the proportion of children with ESKD who do not receive KRT is likely to be very low [1].
Incidence
The incidence of KRT in children varies greatly between countries but can be estimated between 5 and 10 pmarp [66,67,68,69,70] with extreme values ranging from 0 (Malta) to 17 pmarp (Kuwait) [71]. However, given that pediatric KRT is extremely rare, numbers in smaller countries are subject to random error. Moreover, variations in incidence may reflect variations in the incidence of CKD, differences in pre-ESKD care or differences in access to KRT. Among large countries with universal access to KRT, the US incidence is consistently high at around 12.9 per million population [72]. In Japan, incidence of pediatric KRT (4.0 pmarp) was consistently much lower than in other high income countries (Table 54.3).
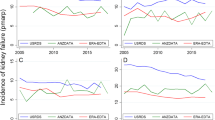
Among lower income countries the incidence is typically lower, as was shown for the Eastern European countries in the ESPN/ERA-EDTA registry [73]. In developing countries where KRT is unaffordable for all but the very wealthy, incidence rates are either not available or were extremely low (<1 pmarp in Bangladesh and Nepal). Some of the variation in incidence may be due to differences in the timing of KRT initiation. In Europe, KRT was generally started at a median GFR of 10.4 mL/min/1.73 m2 whereas mean GFR ranged from 11.3 to 13.6 mL/min/1.73 m2 in the United States [72, 74] (Fig. 54.2).
Within-country variations occur by racial group. For example African American in the US, arboriginal children in Australia and New Zealand or children from South Asian origin in the UK [72, 75, 76] have a significantly higher incidence of ESKD than their white counterparts, although differences in the prevalence of other ESKD risk factors such as obesity or disparities in access to medical care may account for at least part of these differences. There are also large differences between age groups. The incidence has a typical U-shape distribution, with the highest incidence in the preschool children and in adolescents. Therefore, registries that include patients up to 20 years of age report higher incidence and prevalence data compared with registries excluding those over the age of 15.
Around 20% of patients receive a pre-emptive kidney transplant. In patients starting on dialysis, dialysis modality is strongly dependent on age; while peritoneal dialysis is the treatment of choice in the majority of young children, this pattern decreases with age, with typically higher rates of HD from the age of 10 onwards [75]. Finally, the relative proportion of HD and PD is quite variable between countries and between centers presumably reflecting differences in clinician preference and funding models [77].
Prevalence
The prevalence of treated ESKD is completely dependent on access to KRT in each country. In countries with available data on KRT, the IPNA global registry reports prevalences ranging from less than 1% in some African and Asian countries to 98.7 pmarp in the United States [72, 78]. Indeed, 80% of prevalent ESKD patients live in Europe, North America and Japan, while the prevalence of treated ESKD remains very low in many countries with the highest CKD burden [79]. Within Europe, there are also large differences, with high income countries reporting prevalence rates over 55 pmarp similar to Australia/New Zealand with 56.7 cases per million population [69], while middle income European countries report prevalences around 40 pmarp (Fig. 54.3).
In many countries the prevalence is rising due to the combination of a fairly steady incidence and improved patient survival on KRT. In the United States, the adjusted annual incidence of ESKD in the pediatric population rose slowly during the 1980s then increased marginally from 14 to 15 pmarp between 1990 and 2011 [80]. In contrast, the adjusted prevalence increased from 60 to 85 in between 1990 and 2011. Similar trends were observed in Australia and New Zealand, where the incidence has remained constant at about 8 pmarp over the past 25 years, while the prevalence of KRT increased from approximately 30–50 pmarp [69]. A report from the ERA-EDTA registry on patients aged 0–19 years starting KRT between 1980 and 2000 in 12 Western European countries showed that the incidence of KRT rose from 7 pmarp in 1980–1984 to 10 pmarp in 1985–1989 and remained stable thereafter [81], while the prevalence increased from 22.9 pmarp in 1980 to 62 pmarp in 2000. The increases in prevalence were explained by improved survival and treatment of younger children, while the prevalence was relatively constant for the pubertal age groups.
In developing countries, a lower prevalence of children with ESKD is explained by a low access to KRT [78] and by lower patient survival. Figure 54.4 presents the death rates per country caused by CKD in children aged 5–14 years old in 2019. As expected, this map perfectly matches maps reporting access to KRT by countries [82].
CKD-related death rates in children aged 5–14 years (Global Burden of Disease [83])
Transplantation is by far the most common treatment modality in most countries, accounting for 60–80% of patients receiving KRT (Table 54.3). Here again, differences among countries are substantial. For example, fewer than 10% of children on KRT are maintained with a kidney transplant in Belarus, compared with over 90% in Japan and Finland [84]. Recent data show that differences among countries were explained by factors such as the deceased donor rate, the pediatric priority from deceased donor programs, the living donation rate, and healthcare funding models [85]. Compared to adults, children are much more likely to be treated by transplantation due to a combination of fewer comorbidities, higher availability of living donors and, in some cases, preferential allocation of deceased donor kidneys.
Causes of ESKD
the distribution of primary kidney diseases in children reaching ESKD is different than the distribution in children with CKD. Although CAKUT is the most prevalent cause also in children with ESKD, a relatively higher proportion of ESKD cases is caused by glomerular diseases reflecting the faster progression and higher risk of ESKD of this disease group. However, a recent large cohort study from Israel demonstrated that young adults (16–25 years old) with a medical history of kidney disease in childhood but with normal serum creatinine, blood pressure and no proteinuria presented a four-fold increased risk of ESKD over a 30 year follow-up [86]. This underlines the impact of kidney diseases in childhood on ESKD in adulthood and supports long-term follow up of these patients.
There are also very specific local factors. For example, congenital nephrotic syndrome of the Finnish type, explains the very high prevalence of childhood KRT in Finland. Finally, the difference in the distribution of the causes of ESKD in children vs. adults and especially the absence of diabetes or hypertension induced ESKD explains the moderate increase in the prevalence of ESKD in children (+16.6%) in contrast with the major growth experienced by the entire ESKD population (+77%) between 2000 and 2017 in the US [72].
Conclusion
CKD and ESKD in children is a significant public health burden worldwide. Despite significant effort to collect data on children with CKD, the incidence and prevalence of CKD are underestimated in many parts of the world and further studies aiming at improving early CKD diagnosis and at developing effective strategies to slow down CKD progression are needed. For children reaching ESKD, the main challenge is the access to KRT and especially transplantation that remain unavailable to the majority of children with ESKD worldwide.
References
Remuzzi G, Benigni A, Finkelstein FO, Grunfeld J-P, Joly D, Katz I, et al. Kidney failure: aims for the next 10 years and barriers to success. Lancet. 2013;382(9889):353–62.
Eckardt K-U, Coresh J, Devuyst O, Johnson RJ, Köttgen A, Levey AS, et al. Evolving importance of kidney disease: from subspecialty to global health burden. Lancet. 2013;382(9887):158–69.
Harambat J, van Stralen KJ, Kim JJ, Tizard EJ. Epidemiology of chronic kidney disease in children. Pediatr Nephrol. 2012;27(3):363–73.
Shroff R, Weaver DJ, Mitsnefes MM. Cardiovascular complications in children with chronic kidney disease. Nat Rev Nephrol. 2011;7(11):642–9.
Al-Uzri A, Matheson M, Gipson DS, Mendley SR, Hooper SR, Yadin O, et al. The impact of short stature on health-related quality of life in children with chronic kidney disease. J Pediatr. 2013;163(3):736–41. e1
Ardissino G, Daccò V, Testa S, Bonaudo R, Claris-Appiani A, Taioli E, et al. Epidemiology of chronic renal failure in children: data from the ItalKid project. Pediatrics. 2003;111(4 Pt 1):e382–7.
Fivush BA, Jabs K, Neu AM, Sullivan EK, Feld L, Kohaut E, et al. Chronic renal insufficiency in children and adolescents: the 1996 annual report of NAPRTCS. North American Pediatric Renal Transplant Cooperative Study. Pediatr Nephrol. 1998;12(4):328–37.
Deleau J, Andre JL, Briancon S, Musse JP. Chronic renal failure in children: an epidemiological survey in Lorraine (France) 1975–1990. Pediatr Nephrol. 1994;8(4):472–6.
Esbjörner E, Aronson S, Berg U, Jodal U, Linne T. Children with chronic renal failure in Sweden 1978–1985. Pediatr Nephrol. 1990;4(3):249–52. discussion 253-254
Al-Eisa A, Naseef M, Al-Hamad N, Pinto R, Al-Shimeri N, Tahmaz M. Chronic renal failure in Kuwaiti children: an eight-year experience. Pediatr Nephrol. 2005;20(12):1781–5.
Hogg RJ, Furth S, Lemley KV, Portman R, Schwartz GJ, Coresh J, et al. National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative clinical practice guidelines for chronic kidney disease in children and adolescents: evaluation, classification, and stratification. Pediatrics. 2003;111(6 Pt 1):1416–21.
Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;(3):1–150.
Furth SL, Pierce C, Hui WF, White CA, Wong CS, Schaefer F, et al. Estimating time to ESRD in children with CKD. Am J Kidney Dis. 2018;71(6):783–92.
Pottel H, Hoste L, Martens F. A simple height-independent equation for estimating glomerular filtration rate in children. Pediatr Nephrol. 2012;27(6):973–9.
Schwartz GJ, Schneider MF, Maier PS, Moxey-Mims M, Dharnidharka VR, Warady BA, et al. Improved equations estimating GFR in children with chronic kidney disease using an immunonephelometric determination of cystatin C. Kidney Int. 2012;82(4):445–53.
Sharma AP, Yasin A, Garg AX, Filler G. Diagnostic accuracy of cystatin C-based eGFR equations at different GFR levels in children. Clin J Am Soc Nephrol. 2011;6(7):1599–608.
Björk J, Nyman U, Berg U, Delanaye P, Dubourg L, Goffin K, et al. Validation of standardized creatinine and cystatin C GFR estimating equations in a large multicentre European cohort of children. Pediatr Nephrol. 2019;34(6):1087–98.
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009;20(3):629–37.
Pottel H, Hoste L, Dubourg L, Ebert N, Schaeffner E, Eriksen BO, et al. An estimated glomerular filtration rate equation for the full age spectrum. Nephrol Dial Transplant. 2016;31(5):798–806.
Pierce CB, Muñoz A, Ng DK, Warady BA, Furth SL, Schwartz GJ. Age- and sex-dependent clinical equations to estimate glomerular filtration rates in children and young adults with chronic kidney disease. Kidney Int. 2021;99(4):948–56.
Qaseem A, Hopkins RH, Sweet DE, Starkey M, Shekelle P, Clinical Guidelines Committee of the American College of Physicians. Screening, monitoring, and treatment of stage 1–3 chronic kidney disease: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2013;159(12):835–47.
Hogg RJ. Screening for CKD in children: a global controversy. Clin J Am Soc Nephrol. 2009;4(2):509–15.
Murakami M, Hayakawa M, Yanagihara T, Hukunaga Y. Proteinuria screening for children. Kidney Int Suppl. 2005;94:S23–7.
Lin CY, Sheng CC, Chen CH, Lin CC, Chou P. The prevalence of heavy proteinuria and progression risk factors in children undergoing urinary screening. Pediatr Nephrol. 2000;14(10–11):953–9.
Cho B-S, Kim S-D. School urinalysis screening in Korea. Nephrology (Carlton). 2007;12(Suppl. 3):S3–7.
Kim S, Macaskill P, Hodson EM, Daylight J, Williams R, Kearns R, et al. Beginning the trajectory to ESKD in adult life: albuminuria in Australian aboriginal children and adolescents. Pediatr Nephrol. 2017;32(1):119–29.
Chaudhury AR, Reddy TV, Divyaveer SS, Patil K, Bennikal M, Karmakar K, et al. A cross-sectional prospective study of asymptomatic urinary abnormalities, blood pressure, and body mass index in healthy school children. Kidney Int Rep. 2017;2(6):1169–75.
Saydah SH, Xie H, Imperatore G, Burrows NR, Pavkov ME. Trends in albuminuria and GFR among adolescents in the United States, 1988–2014. Am J Kidney Dis. 2018;72(5):644–52.
Ramirez SP, Hsu SI, McClellan W. Low body weight is a risk factor for proteinuria in multiracial Southeast Asian pediatric population. Am J Kidney Dis. 2001;38(5):1045–54.
Zhai Y-H, Xu H, Zhu G-H, Wei M-J, Hua B-C, Shen Q, et al. Efficacy of urine screening at school: experience in Shanghai, China. Pediatr Nephrol. 2007;22(12):2073–9.
Vehaskari VM, Rapola J. Isolated proteinuria: analysis of a school-age population. J Pediatr. 1982;101(5):661–8.
Shajari A, Shajari H, Zade MHF, Kamali K, Kadivar MR, Nourani F. Benefit of urinalysis. Indian J Pediatr. 2009;76(6):639–41.
Koshy SM, Garcia-Garcia G, Pamplona JS, Renoirte-Lopez K, Perez-Cortes G, Gutierrez MLS, et al. Screening for kidney disease in children on World Kidney Day in Jalisco. Mexico Pediatr Nephrol. 2009;24(6):1219–25.
Meadow SR, White RH, Johnston NM. Prevalence of symptomless urinary tract disease in Birmingham schoolchildren. I. Pyuria and bacteriuria. Br Med J. 1969;3(5662):81–4.
Committee on Practice and Ambulatory Medicine. Recommendations for preventive pediatric health care. Pediatrics. 2000;105(3):645–6.
Committee on Practice and Ambulatory Medicine, Bright Futures Steering Committee. Recommendations for preventive pediatric health care. Pediatrics. 2007;120(6):1376.
Sekhar DL, Wang L, Hollenbeak CS, Widome MD, Paul IM. A cost-effectiveness analysis of screening urine dipsticks in well-child care. Pediatrics. 2010;125(4):660–3.
Peco-Antic A, Bogdanovic R, Paripovic D, Paripovic A, Kocev N, Golubovic E, et al. Epidemiology of chronic kidney disease in children in Serbia. Nephrol Dial Transplant. 2012;27(5):1978–84.
Mong Hiep TT, Ismaili K, Collart F, Van Damme-Lombaerts R, Godefroid N, Ghuysen M-S, et al. Clinical characteristics and outcomes of children with stage 3–5 chronic kidney disease. Pediatr Nephrol. 2010;25(5):935–40.
Esbjörner E, Berg U, Hansson S. Epidemiology of chronic renal failure in children: a report from Sweden 1986–1994. Swedish Pediatr Nephrol Assoc Pediatr Nephrol. 1997;11(4):438–42.
Areses Trapote R, Sanahuja Ibáñez MJ, Navarro M. Investigadores Centros Participantes en el REPIR II. [Epidemiology of chronic kidney disease in Spanish pediatric population. REPIR II Project]. Nefrologia. 2010;30(5):508–17.
Kim JJ, Booth CJ, Waller S, Rasmussen P, Reid CJD, Sinha MD. The demographic characteristics of children with chronic kidney disease stages 3–5 in South East England over a 5-year period. Arch Dis Child. 2013;98(3):189–94.
Soylemezoglu O, Duzova A, Yalçinkaya F, Arinsoy T, Süleymanlar G. Chronic renal disease in children aged 5–18 years: a population-based survey in Turkey, the CREDIT-C study. Nephrol Dial Transplant. 2012;27(Suppl. 3):146–51.
Seikaly MG, Ho PL, Emmett L, Fine RN, Tejani A. Chronic renal insufficiency in children: the 2001 Annual Report of the NAPRTCS. Pediatr Nephrol. 2003;18(8):796–804.
Furth SL, Cole SR, Moxey-Mims M, Kaskel F, Mak R, Schwartz G, et al. Design and methods of the Chronic Kidney Disease in Children (CKiD) prospective cohort study. Clin J Am Soc Nephrol. 2006;1(5):1006–15.
Lagomarsimo E, Valenzuela A, Cavagnaro F, Solar E. Chronic renal failure in pediatrics 1996. Chilean survey. Pediatr Nephrol. 1999;13(4):288–91.
Grimoldi IA, Briones LM, Ferraris JR, Rodríguez Rilo L, Sojo E, Turconi A, et al. Chronic renal failure, dialysis and transplant: multicentric study: 1996–2003. Arch Argent Pediatr. 2008;106(6):552–9.
Miller MEY, Williams JA. Chronic renal failure in Jamaican children—an update (2001–2006). West Indian Med J 2009;58(3):231–234.
Orta-Sibu N, Lopez M, Moriyon JC, Chavez JB. Renal diseases in children in Venezuela, South America. Pediatr Nephrol. 2002;17(7):566–9.
Franco-Marina F, Tirado-Gómez LL, Estrada AV, Moreno-López JA, Pacheco-Domínguez RL, Durán-Arenas L, et al. An indirect estimation of current and future inequalities in the frequency of end stage renal disease in Mexico. Salud Publica Mex. 2011;53(Suppl. 4):506–15.
Ishikura K, Uemura O, Ito S, Wada N, Hattori M, Ohashi Y, et al. Pre-dialysis chronic kidney disease in children: results of a nationwide survey in Japan. Nephrol Dial Transplant. 2013;28(9):2345–55.
Huong NTQ, Long TD, Bouissou F, Liem NT, Truong DM, Nga DK, et al. Chronic kidney disease in children: the National Paediatric Hospital experience in Hanoi, Vietnam. Nephrology (Carlton). 2009;14(8):722–7.
Mong Hiep TT, Janssen F, Ismaili K, Khai Minh D, Vuong Kiet D, Robert A. Etiology and outcome of chronic renal failure in hospitalized children in Ho Chi Minh City, Vietnam. Pediatr Nephrol. 2008;23(6):965–70.
Vachvanichsanong P, Dissaneewate P, McNeil E. Childhood chronic kidney disease in a developing country. Pediatr Nephrol. 2008;23(7):1143–7.
Gulati S, Mittal S, Sharma RK, Gupta A. Etiology and outcome of chronic renal failure in Indian children. Pediatr Nephrol. 1999;13(7):594–6.
Bek K, Akman S, Bilge I, Topaloğlu R, Calişkan S, Peru H, et al. Chronic kidney disease in children in Turkey. Pediatr Nephrol. 2009;24(4):797–806.
Hamed RMA. The spectrum of chronic renal failure among Jordanian children. J Nephrol. 2002;15(2):130–5.
Odetunde OI, Okafor HU, Uwaezuoke SN, Ezeonwu BU, Adiele KD, Ukoha OM. Chronic kidney disease in children as seen in a tertiary hospital in Enugu, South-East, Nigeria. Niger J Clin Pract. 2014;17(2):196–200.
Anochie I, Eke F. Chronic renal failure in children: a report from Port Harcourt, Nigeria (1985–2000). Pediatr Nephrol. 2003;18(7):692–5.
Bhimma R, Adhikari M, Asharam K, Connolly C. The spectrum of chronic kidney disease (stages 2–5) in KwaZulu-Natal, South Africa. Pediatr Nephrol. 2008;23(10):1841–6.
Ali E-TMA, Abdelraheem MB, Mohamed RM, Hassan EG, Watson AR. Chronic renal failure in Sudanese children: aetiology and outcomes. Pediatr Nephrol. 2009;24(2):349–53.
Olowu WA, Adefehinti O, Aladekomo TA. Epidemiology and clinicopathologic outcome of pediatric chronic kidney disease in Nigeria, a single center study. Arab J Nephrol Transplant. 2013;6(2):105–13.
Michael IO, Gabreil OE. Chronic renal failure in children of Benin, Nigeria. Saudi J Kidney Dis Transpl. 2004;15(1):79–83.
Madani K, Otoukesh H, Rastegar A, Van Why S. Chronic renal failure in Iranian children. Pediatr Nephrol. 2001;16(2):140–4.
Registry Reports | NAPRTCS [Internet]. [cited 2020 Apr 24]. Available from: https://naprtcs.org/registries/annual-report
Hattori M. Current trend of pediatric renal replacement therapy in Japan. Contrib Nephrol. 2018;196:223–8.
ESPN/ERA-EDTA Registry—Annual reports [Internet]. [cited 2020 Nov 27]. Available from: https://www.espn-reg.org/index.jsp?p=pua
Information (CIHI) CI for H. CORR Annual Statistics [Internet]. [cited 2020 Nov 28]. Available from: https://secure.cihi.ca/estore/productSeries.htm?pc=PCC24
ANZDATA 42nd Annual Report 2019 (Data to 2018) [Internet]. ANZDATA 42nd Annual Report 2019 (Data to 2018)—ANZDATA. [cited 2020 Jun 12]. Available from: https://www.anzdata.org.au/report/anzdata-42nd-annual-report-2019/
Hattori M, Sako M, Kaneko T, Ashida A, Matsunaga A, Igarashi T, et al. End-stage renal disease in Japanese children: a nationwide survey during 2006–2011. Clin Exp Nephrol. 2015;19(5):933–8.
Al-Eisa AA, Samhan M, Naseef M. End-stage renal disease in Kuwaiti children: an 8-year experience. Transplant Proc. 2004;36(6):1788–91.
USRDS. United States Renal Data System, 2018 Annual Data Report: An overview of the epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018.
Chesnaye N, Bonthuis M, Schaefer F, Groothoff JW, Verrina E, Heaf JG, et al. Demographics of paediatric renal replacement therapy in Europe: a report of the ESPN/ERA-EDTA registry. Pediatr Nephrol. 2014;29(12):2403–10.
van Stralen KJ, Tizard EJ, Jager KJ, Schaefer F, Vondrak K, Groothoff JW, et al. Determinants of eGFR at start of renal replacement therapy in paediatric patients. Nephrol Dial Transplant. 2010;25(10):3325–32.
White A, Wong W, Sureshkumur P, Singh G. The burden of kidney disease in indigenous children of Australia and New Zealand, epidemiology, antecedent factors and progression to chronic kidney disease. J Paediatr Child Health. 2010;46(9):504–9.
Lewis MA, Shaw J, Sinha MD, Adalat S, Hussain F, Castledine C, et al. UK Renal Registry 12th Annual Report (December 2009): chapter 14: demography of the UK paediatric renal replacement therapy population in 2008. Nephron Clin Pract. 2010;115(Suppl. 1):c279–88.
Hogan J, Ranchin B, Fila M, Harambat J, Krid S, Vrillon I, et al. Effect of center practices on the choice of the first dialysis modality for children and young adults. Pediatr Nephrol. 2017;32(4):659–67.
IPNA. IPNA Global Registry annual report. 2018. Available from: https://ipna-registry.org/fileadmin/reports/IPNA_Registry_Annual_Report_2018.pdf
Harambat J, Ekulu PM. Inequalities in access to pediatric ESRD care: a global health challenge. Pediatr Nephrol. 2016;31(3):353–8.
Jafar TH, Stark PC, Schmid CH, Landa M, Maschio G, de Jong PE, et al. Progression of chronic kidney disease: the role of blood pressure control, proteinuria, and angiotensin-converting enzyme inhibition: a patient-level meta-analysis. Ann Intern Med. 2003;139(4):244–52.
van der Heijden BJ, van Dijk PCW, Verrier-Jones K, Jager KJ, Briggs JD. Renal replacement therapy in children: data from 12 registries in Europe. Pediatr Nephrol. 2004;19(2):213–21.
Liyanage T, Ninomiya T, Jha V, Neal B, Patrice HM, Okpechi I, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385(9981):1975–82.
Global Burden of Disease. Global Burden of Disease [Internet]Available from: www.healthdata.org/gbd/2019.
Harambat J, van Stralen KJ, Schaefer F, Grenda R, Jankauskiene A, Kostic M, et al. Disparities in policies, practices and rates of pediatric kidney transplantation in Europe. Am J Transplant. 2013;13(8):2066–74.
Harambat J, van Stralen KJ, Verrina E, Groothoff JW, Schaefer F, Jager KJ, et al. Likelihood of children with end-stage kidney disease in Europe to live with a functioning kidney transplant is mainly explained by nonmedical factors. Pediatr Nephrol. 2014;29(3):453–9.
Calderon-Margalit R, Golan E, Twig G, Leiba A, Tzur D, Afek A, et al. History of childhood kidney disease and risk of adult end-stage renal disease. N Engl J Med. 2018;378(5):428–38.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hogan, J., van Stralen, K.J. (2023). Demographics of CKD and ESRD in Children. In: Schaefer, F., Greenbaum, L.A. (eds) Pediatric Kidney Disease. Springer, Cham. https://doi.org/10.1007/978-3-031-11665-0_54
Download citation
DOI: https://doi.org/10.1007/978-3-031-11665-0_54
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-11664-3
Online ISBN: 978-3-031-11665-0
eBook Packages: MedicineMedicine (R0)